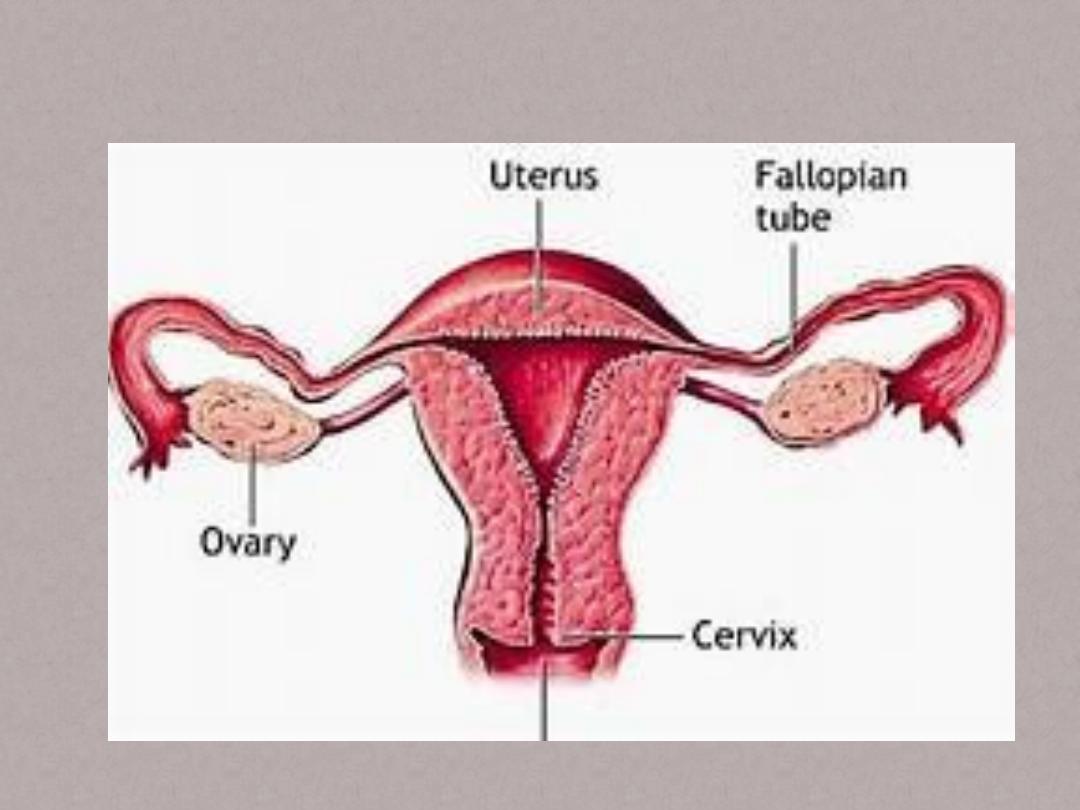
Gynaecology of the uterus
• Anatomy the uterus:
• The uterus is approximately the size & shape
of a pear with a central cavity & thick
muscular walls.The serosal surface is the
closely applied peritoneum , beneath which is
the myometrium which is a smooth muscle
supported by connective tissue.
• The myom. Is made up 3 layers of muscle ,
external,intermediate & internal layers.The 3
layers run in complimentary directions which
encourage vascular occlusion during
contraction, an important aspect of menstrual
blood loss & postpartum haemostasis.
• The mucous membrane overlying the myom.
To line the cavity is the endometrium.Glands
of the endom. Pierce the myom. & a single
layer of columnar epithelium on the surface
changes cyclically in response to the mensrual
cycle.
• The uterus consists of a fundus superiorly, a
body , an isthmus(internal os) & inferiorly the
cervix (external os).The uterus is supported by
the muscles of the pelvic floor together with 3
supporting condensations of connective
tissue:
• 1. The pubocervical ligaments run from the
cervix anteriorly to the pubis.
• 2.The cardinal ligaments pass laterally from
the cervix & upper vagina to the lateral pelvic
side walls.
• 3.The uterosacral ligaments from the cervix &
upper vagina to the sacrum.
• The uterus blood supply is derived mainly
from the uterine artery , a branch of the
anterior division of the internal iliac artery.
• Benign diseases of the uterus:
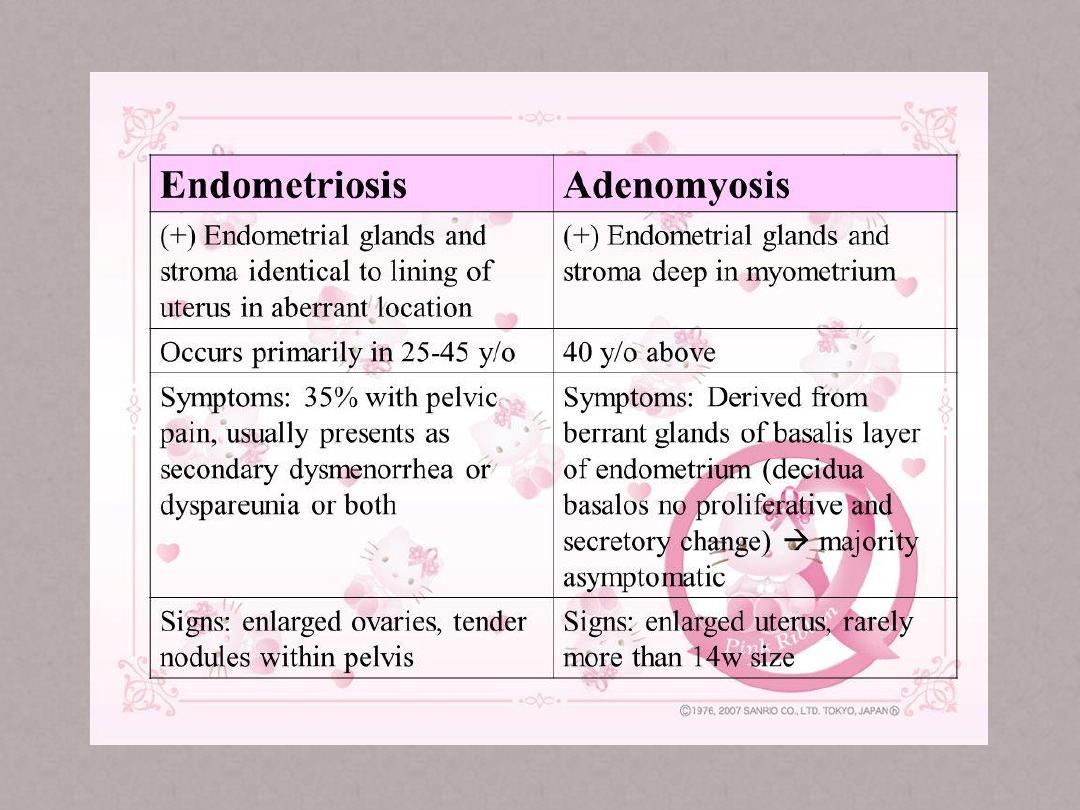
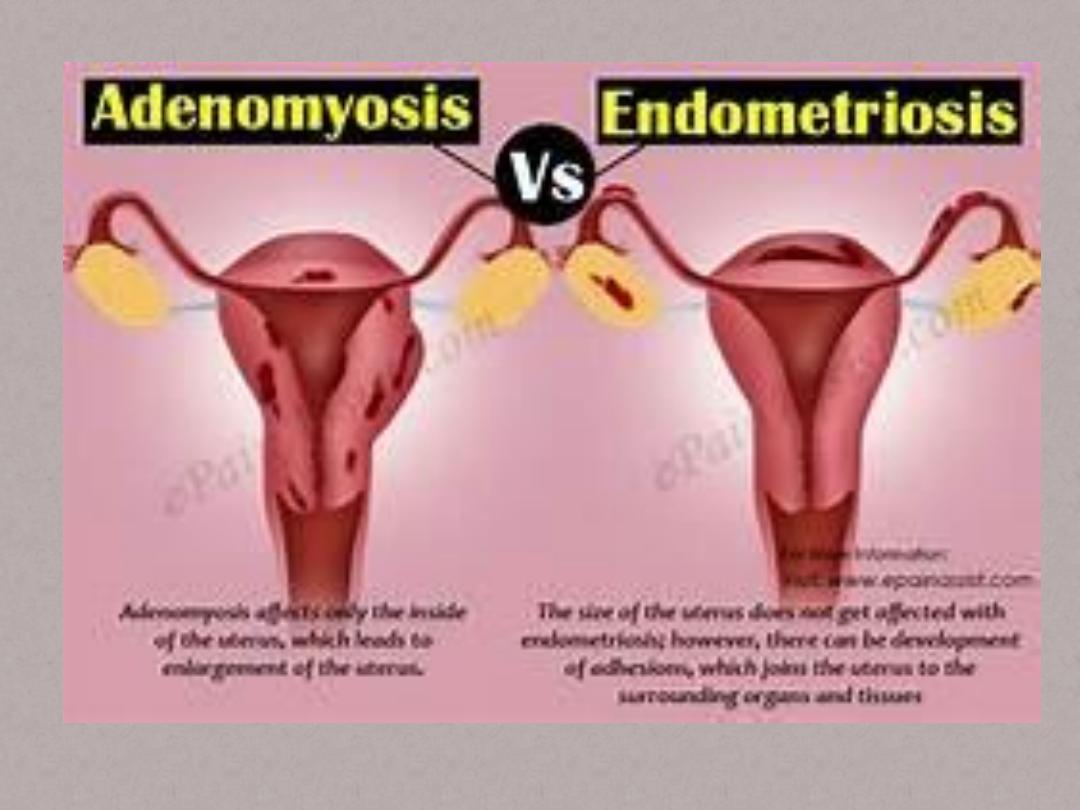
• Endometriosis :
• It is defined as the presence of endometrial
like tissue that is, glands & stroma, outside the
uterus.The most commonly affected sites are
the pelvic organs & peritoneum although
other parts of the body such as the lungs are
occasionally affected.
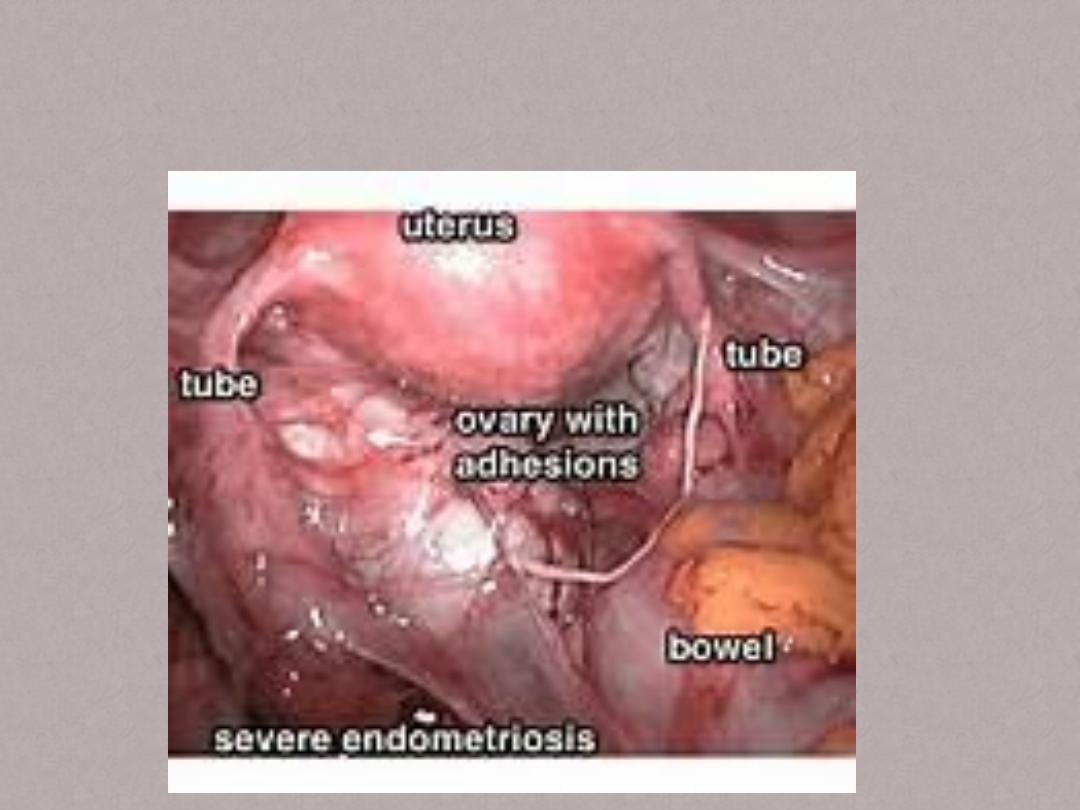
• The varies from a few , small lesions on
otherwise normal pelvic organs to solid,
infiltrating masses & ovarian endometriotic
cysts(endometiomas) often with extensive
fibrosis & adhesion formation causing marked
distortion of pelvic anatomy.
• Prevalence :
• Is 8-10% in reproductive years , although the
precise rate is not known because the pelvis
has to be inspected at surgery to make a
definitive diagnosis.
• Aetiology:
• Implantation of viable endometrial cells &
metaplasia of one tissue type into another are
both reasonable explanations for the
occurrence of endometriosis.
• Risk factors:
• 1.age
• 2.increased peripheral body fat
• 3.greater exposure to menstruation (i.e.short
cycles,long duration of flow & reduced parity).
Where as smoking,exercise & oral
contraceptive use (current & recent) may be
protective.
• Genetic predisposition is likely as endom.
Occurs 6-9 times more in the 1
st
degree
relatives of affected women than in controls.
• Presentation:
• 1.sever dysmenorrhea
• 2.deep dyspareunia
• 3.chronic pelvic pain
• 4.cyclical or perimenstrual symptoms often
bowel or bladder related causing dyschezia or
dysuria with or without abnormal bleeding &
chronic fatigue.
• 5.many affected women are asymptomatic.
• 6.infertility due to sever anatomical distortion
which interfer with oocyte pick up.
• Numerous mechanisms have been proposed
including abnormal folliculogenesis,
anovulation,luteal insufficiency, luteinized
unruptuted follicle syndrome,recurrent
miscarriage , decreased sperm survival
,altered immunity , intraperitonel inflamation
& endom. Dysfunction.
• Diagnosis:
• Making dx on the basis of symptoms is
difficult as the presentation is variable.finding
pelvic tenderness , a fixed retroverted uterus,
tender uterosacral ligaments or enlarged
ovaries on exam. is suggestive of
endometriosis.
• Non – invasive tests: TVS is a useful tool to dx
& exclude ovarian endomeriomas, but it has
no value for peritoneal disease.
• Laproscopy: it is the gold standard for dx ,
histological confirmation of at least one
peritoneal lesion is ideal.The best practise is to
remove / ablate endometriosis at the same
time.
• Treatment:
• Factors influencing choice of Rx:
• 1. woman’s age
• 2. fertility status
• 3. nature of symptoms
• 4.severity of disease
• 5. previous Rx
• 6. priorities & attitudes
• 7. resource implications
• 8. costs+ side-effect profile
• 9. risks of Rx
• 10. other subfertility factors
• 11. intended duration of Rx
• 12.best available evidence
• Non hormonal Rx for pain relief:
• 1.herbal remedies
• 2.dietary manipulation
• 3.acupuncture
• 4.vitamine or mineral supplements
• Hormonal Rx:
• They are attempted to mimic pregnancy or
menopause , based upon that the disease
regresses during these physiological states.
• The currently available:
• COCPs ,progestagens,danazol,gestrinone &
GnRH agonists.
• Despite different modes of action, they all
appear to induce atrophy & decidualization of
peritoneal deposits by suppressing ovarian
function.
• Peritoneal lesions decrease in size during
therapy but reappear rapidly on stopping.
• Endomeriomas rarely decrease in size &
adhesions will be unaffected.
• Side effects & complications of danazol &
GnRH agonists:
• Danazol side effects : weight gain,bloating,
increased body hair, acne & oily skin, deep
voice(irreversible), decreased breast size,
muscle cramps, headaches,hot flushes,limb
tingling,decreased libido,menstrual spotting.
• Complications:liver tumors(long-term
use),adverse effect on lipids.
• GnHR agonists side effects: hot flushes, night
sweats, headaches, vaginal dryness, irritability,
insomnia, decreased libido, palpitations, joint
stiffness.
• Complications: bone loss
• The duration of GnRH agonists use is limited
by the associated loss in bone density, up to
6% in the 1
st
6 months,although the loss is
restored almost completely 2 years after
stopping Rx. The hypoestrogenic symptoms
can be alleviated & bone loss prevented ,
without loss of efficacy, by using add-back
therapy in the form of oestrogens,
progestagens or tibolone.
• Surgical Rx:
• The goal of surgery is to eliminate all visible
peritoneal lesions, endomeriomas & associated
adhesions & to restore normal anatomy. Excision
is done for endometriomas.
• Laproscopy should be used as it decrease
morbidity & duration of hospitalization &
therefore cost, compared to laparatomy.
• Lesions can be removed by surgical excision with
scissors ,laser CO2 or potassium titanyl
phosphate (KTP).
• Laoroscopic cystectomy for endometriomas is
preferable to coagulation or laser
vaporization.
• Some general priciples apply ,for ex , a woman
in her late 40s with deblitating pain & sever
disease who has completed her family can be
offered a TAH+BSO provided that all the
endometriotic tissue is removed at the same
time.
• On the other hand , a young nulliparous
woman with a similar presentation will want
as much normal tissue as possible conserved if
she opt for surgery.
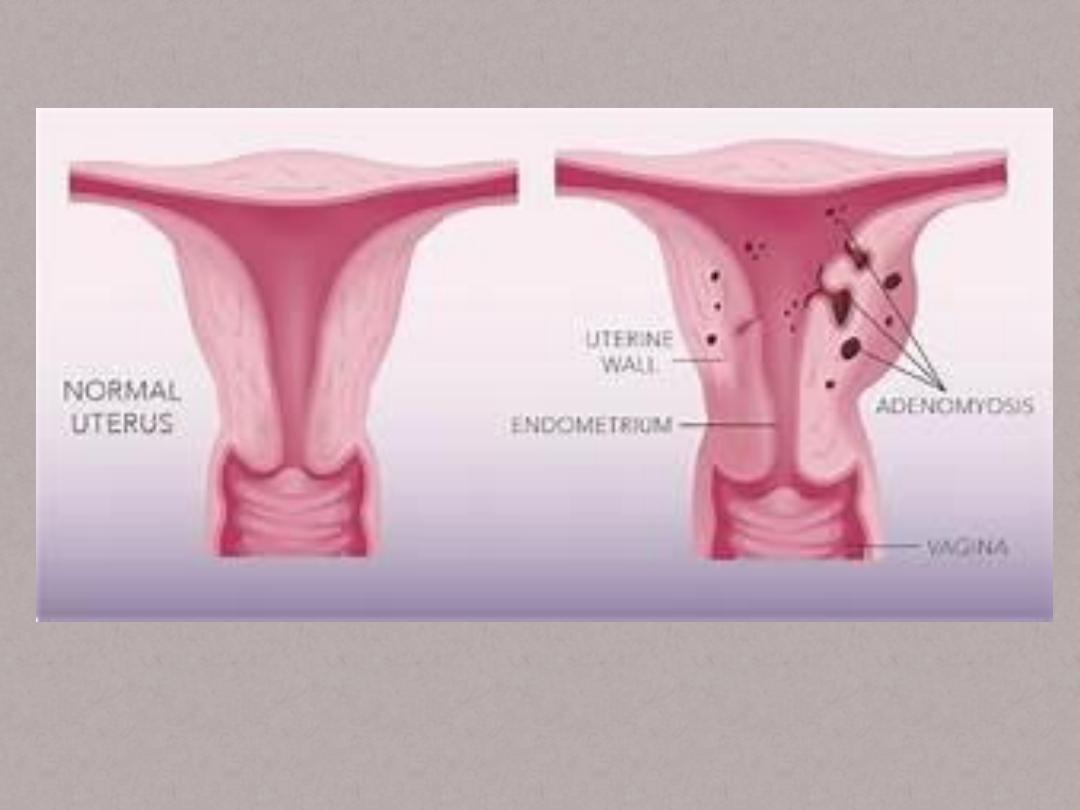
• Adenomyosis:
• Is the benign invasion of endometrium into the
myometrium.
• Both endom glands & stroma must be present
the result is enlarged uterus in which the
adenomyosis may be either diffuse or present as
focal deposits or adenomyomas.
• Incidence varies because it is a post-hystrectomy
Dx , the preoperative Dx is less than 10%.
• Presentation:
• The commonest is that of heavy menstrual
bleeding associated with worsening
dysmenorrhea , the later being worse in deep
infiltrating disease.
• The condition is characteristic of the 5
th
decade with the age of 45 being the
commonest age of presentation & is very rare
in nulliparous women.

Aetiology:
The ectopic endometrium is resposive to steroid
hormones , therefore bleeding will occur each
month & it is possible that this contributes to
dysmenorrea.
In addition there is abnormal PG production &
this could contribute to both pain& heavy
bleeding.
• Dx.:
• The dx is by hitological exam. of the uterus
after hysterectomy.However , MRI is more
accurate than US in dx.
• Rx.:hysterectomy is the only cure of the
problem , it is possible that modalities such as
levonorgestrel rleasing intrauterine system or
uterine artery embolization may be useful .

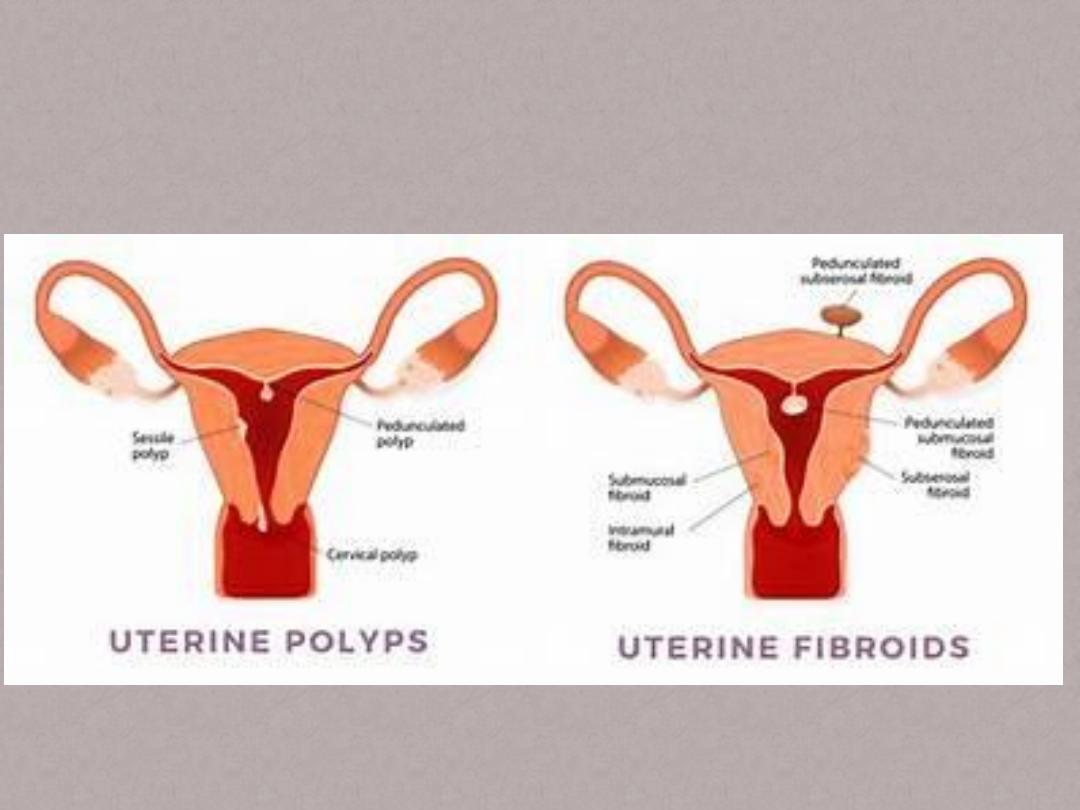
• Endometrial [polyps:
• Are discreat outgrowths of the endom that
contain a variable amount of gland stroma &
blood vessels.
• They may be pedunculated or sessile ,single or
multiple & different sizes.
• They are relatively insensitive to cyclical
hormonal changes & so are not shed at the
time of menstruation.
• Epidemiology:
• The presence is increasingly recognised since
the wide spread adoption of TVS & out patient
hysteroscopy.It is possible that they are
present in 25% of women with abnormal
vaginal bleeding although at least 10% of
asymptomatic women are likely to have
polyps, they are practically common in women
taking preparations such as Tamoxifen.
• Presentation:
• Unscheduled vaginal bleeding or spotting is
the commonest presentation.
• Dx.: TVS can identify them singly or as part of
abnormally thickening endom , intrauterine
injection of saline can markedly increase the
diagnostic performance of TVS.

• Hysteroscopy is the best method of dx & can
be treated at the same time.Biopsy should be
carried out to confirm dx.
• Rx.: is by removal of the whole lesion intact or
cut up into small pieces.
• Uterine leiomyomata(fibroids):
• They are clinically apparent in 20% of women
in reproductive age , there incidence is
increased in women of Afro Caribbean origin
& decreased with prolonged use of OCP as
well as with increasing number of term
pregnancies.
• Symptoms:
• 1.menstrual problems mainly heavy menses &
it is not confined to those with submucos
types , but also can be associated with
subserosal lesions.
• 2.symptoms related to the size of the fibroid
like abdominal swelling & discomfort ,or
pressure effects on urinary system causing
frequency & retention,or bowel problems.
• 3.subfertility:difficulty in conceiving,
pregnancy loss.
• Dx.:uterus is enlarged on abdominal exam ,
however it may be difficult to distinguish
between an enlarged uterus & an ovarian
mass , so imaging is mandatory.
• US is very useful as 1
st
line, also MRI can give
excellent visualization of uterus & ovaries.
• Rx.: medical & surgical
• Medical Rxs do not cure the problem but are
designed to bring symptom relief.
• 1.The most established medical option is
adminstration of the GnRH agonists,these drugs
lead to down regulation of pituitary receptors
that results initially in stimulation of
gonadotrophin release but within 2-3 weeks of Rx
, gonadotrophin output decreases &
consequently that of ovarian steroids.
• The decreased output of ovarian steroids
continues while Rx is ongoing.This is usually
given by monthly depot injections although
other methods of adminstration such as the
nasal spray are available.Fibroid shrinkage
ocurrs rapidly in the 1
st
3 months but then
tends to slow down with little further
decrease.
• The principle disadvantage of these agents are
that fibroids grow again when Rx has stopped
& also they are associated with
postmenopausal type side effects ,these
consist of hot flushing & vaginal dryness but
the most important it can lead to significant
bone loss.
• It is possible to counteract these side effects
by adminstration of low dose HRT
• This is an option available if a woman is
unsuitable for surgery due either to multiple
previous abdominal operations , medical
problems or morbid obesity.
• There adminstration results in amenorrhea&
this increases Hb.
• 2.progestrone receptor modulators
• 3.levonorgestrel –secreting intrauterine system:
• This device has revolutionized the Rx of DUB & it
may be one of the reasons why hysterectomy rate
has declined over recent years.However there
use in fibroids is not widely used partly because it
may be expelled during heavy menstruation
because of the presence of a very distorted cavity
as found in fibroids.
• 4.other drugs are those that cause
amenorrhea such as progestagens, OCP ,
danazol & gestrinone.
• Surgical Rx:
• The commonest option is hystrectomy ,many
women do not wish to lose their uterus ,
either to maintain fertility or feel that not
appropriate.

• Myomectomy involves removing the fibroids
only ,this can be carried out as an open ,
laproscopic or as a hysteroscopic procedures.
• Bleeding can be heavy during myomectomy &
this may lead in a small number of cases to
hysterectomy.
• Uterine artery embolization:
• This procedure leads to shrinkage of the
fibroids that ,unlike with GnRH agonists,
continues in some cases for as long as follow
up has occurred.Also there is a significant
beneficial effect on menstrual blood loss.
• Complications:
• 1.sepsis
• 2.vaginal discharge
• 3.groin injury
• 4.amenorrhea:premature ovarian failure, endom
atrophy,intrauterine adhesions
• 5.post embolization syndrome
• 6.non-target embolization:ovary,bowel or bladder
• 7.Rx failure
• Other radiological techniques:
• Laser ablation of fibroids can carried out at
surgery either using a hysteroscope or
laproscope depending on the position of the
fibroids . Laser can also be used with MRI or
US guidance.
• Endometrial ablation:may be performed with
or without myomectomy & is associated with
a high rate of amenorrhea.
• Cancer of uterus:
• Includes endom cancers , the commonest &
accounts for 95% , carcinosarcomas &
sarcomas. It is the 2
nd
in incidence among
gyneco cancers in the European union.
• Aetiology: There is an association with
hyperoestrogenism , also obesity & related co-
morbidity such as diabetes & HT.
• The obese woman experiences increased
circulating estrogens from conversion of
androgens in peripheral fat.
• Conditions such as PCO syndrome & granulosa
cell tumors , both produce hyperestrog, are
associated with endom hyperplasia.
• Unopposed estrogen replacement therapy
increases rates of endom cancer.
• Another factor involved in the rising incidence
of endom cancer & probably also
carcinosarcomas is Tamoxifen because it
exerts proestrogenic effect on the endom.
• There are groups of women who are
genetically predisposed to endom cancer ,
particularly those with hereditary non-
polyposis colon cancer(HNPCC).
• FIGO staging: from book
• Presentation:
• 75-80% of women will present with
postmenopausal bleeding, however a
postmenopausal discharge particularly a blood
stained discharge may be associted with
carcinoma.In the premenopausal period,most
women will present with intermenstrual bleeding
although one-third will present with heavy
periods only.
• Investigations & dx:
• US is a useful 1
st
screen capable of demonstrating
a likely tumor & myometrium invasion , other
radiological is MRI scan , which although not
superior to CT scanning at identifying nodal
involvement , is superior at assessing both
myometrial invasion & cervical involvement &
direct extension of tumor outside the uterus.
• The defenitive dx requires a biopsy which is
obtained by an outpatient procedure using
devices such as Endocell or pipelle or curettage.
• Pre-anasthesia assessment:
• Many of these women are elderly & obese
with high prevalence of IHD ,HT & chronic
obstructive airway disease , full
heamatological & biochemical screening is
essential together with ECG & CXR , which is
also required to exclude pulmonary
metastases.
• Rx: the principle Rx for endom cancer is
surgery & because it usually presents when
the disease is confined to the uterus , surgical
excision is curative in the majority of cases .
• In high risk cases, adjuvant therapy is
employed & in a minority of cases ,either
advanced or presence of extreme comorbidity,
non-surgical Rx needs to be considered.
• Low risk tumors can be managed by TAH+BSO,
a thorough palpation of the of the contents of
the peritoneal cavity should be made
including the pelvic & para-aortic nodes.
• The omentum should be visualized & any
suspicious mass should be sampled.
• A staging laparotomy is often performed for
high risk tumors.
• Stage 1:TAH+BSO , radiotherapy is necessary if
invasion of the myometrium has occurred to
more than the inner half.
• Stage 2: if surgically fit patient , a radical
hysterectomy & bilateral lymphadenectomy
with para-aortic node sampling is performed.
• If surgically unfit then radiotherapy may be
used.
• Stage 3: if the node suggests spread of the
disease then adjuvant radiotherapy is
necessary with surgery.
• Stage 4: surgery is not usually the 1
st
line of
Rx, radiotherapy is performed & then
occasionally residual disease may be involved
by surgical intervention.
• Sarcomas & mixed mesodermal tumors:
• Leiomyosarcomas: may arise in the uterine
muscle , very rarely such a tumor may arise by
transformation of a previously benign
fibromyoma , this occurs in less than 0.2% of
fibromyomata.
• Sarcoma botryoides ( embryonal
rhabdomyosarcoma) is seen in infants &
young children.
