Dr. Nabila Kamil
Department of obstetric Gynecology
Tikrit University College Of Medicine
(TUCOM)
Definition
Infertility
is the inability of a couple to
become pregnant ( regardless of cause) after
1 year of unprotected sexual intercourse
( using no birth control method).
@
Infertility affect men and women
equally.
@
85-90 % of infertility cases are
treated with medication or surgery.
@
Advanced technologies include IVF,
ICSI and other similar procedures
improve fertility rate in general.
Types of infertility:
Primary infertility
: A couple that has
never able to conceive a pregnancy, after at
least 1 year of unprotected intercourse.
Secondary infertility
: A couple who have
previously been pregnant at least once, but
have not been able to achieve another
pregnancy.
-
Infertility affects 10-15 % of couples at
reproductive age.
-
Female factors has prevalence of 40-55 %.-
-
Tubal factor 30-40%
-
14% of all infertility cases are related to tubal
factor.
Causes in either sex
(Both male and female).
1-Genitic causes
:
Any abnormal translocation.
2-General factors:
*
D.M.
*
Thyroid diseases.
*
Adrenal diseases.
3-Hypothalamic- pituitary causes:
*
Kallmann syndrome.
*
Hyperprolactinemia.
*
Hypopituitarism.
Female infertility
Causes:
1-General factors:
Significant liver, kidney disease,
thrombophilia.
2-Hypothalamic- pituitary factors:
Hypothalamic
dysfunction.
3-Ovarian factors:
*
PCOS.
*
Anovulation.
*
Diminish ovarian reserve.
*
Premature menopause.
*
Menopause.
*
Luteal dysfunction.
*
Gonadal dysgenesis (turner syndrome).
*
Ovarian cancer.
4-Tubal and peritoneal factors
*
Endometriosis
*
Pelvic adhesion.
*
PID (chlamydia).
*
Tubal occlusion.
*
Tubal dysfunction.
5-Uterine factors:
*
Uterine malformation.
*
Uterine fibroids.
*
Asherman
’s syndrome.
Female infertility
6-Cervical factors:
*
Anti sperm antibodies.
*
Cervical stenosis.
*
Insufficient cervical mucus for travel and survival of
sperm.
7-Vaginal factors:
*
Vaginismus.
*
Vaginal obstruction.
8-Genetic factors:
Intersexed conditions (androgen
insensitivity syndrome).
Female infertility
Male infertility
Causes:
1-Pretesticular causes:
Hypogonadism due to drugs, alcohol
,
smoking.
2-Testicular causes:
*
Bad semen quality.
*
Abnormal sperm morphology.
*
Azoospermia (complete lack of sperm in semen).
*
Y- chromosome microdeletions.
*
Kline Felter syndrome.
*
Neoplasm (seminoma).
*
Idiopathic failure.
*
Varicocele.
*
Hydrocele.
*
Mumps and malaria.
*
Testicular dysgenesis syndrome.
3-Post testicular causes:
*
Vas deference obstruction.
*
Lack of vas deference.
*
Infection (prostitis).
*
Retrograde ejaculation.
*
Impotence.
*
Acrosomal defect (egg penetration defect).
4-Immunological causes:
*
Anti sperm antibody.
Male infertility
@
Combined infertility: Both male and female
are infertile.
@
Unexplained infertility in 15% of cases.
@
Joint infertility problems: Frequency of
intercourse not appropriate.
@
Sperm can live about 48 hours in woman
’s
reproductive tract.
@
Medical history in infertility is very important.
Clinical evidence of ovulation
*
Basal body temperature.
*
Observation of the cervical mucus.
*
Exfoliative vaginal cytology.
*
Transvaginal sonography (ovarian follicle).
*
Pituitary and ovarian hormone assays.
*
Laproscopy and direct observation of the
ovaries.
Clinical evidence of normality of
internal genetic tract
*
HSG.
*
Transvaginal sonography.
*
Hysteroscopy.
*
Laproscopy.
Post coital test
Involve sampling of your cervical mucus between 4-
10 hours after intercourse to determine whether
the mucus in your cervix is hostile to sperm.
Note
: Don
’t use any lubricants, douche or bathe.
Conclusions of the test:
*
Ferning.
*
Amount of cervical mucus production increase.
*
Clarity (watery).
*
Cellularity (should few cells other than sperm).
*
Spinn barkiet: Stretchiness of mucus should be elastic and
stretch 10 cm or more.
Poor test due to:
1-
Infection.
2-
Poor timing.
3-
Prior freezing or laser to cervix.
4-
Medications (clomiphene).
It
’s used since 1860.
Abnormal test mean that other treatments will be
needed to help you conceive like
IVF and IUI.
Post coital test
Routine laboratory tests
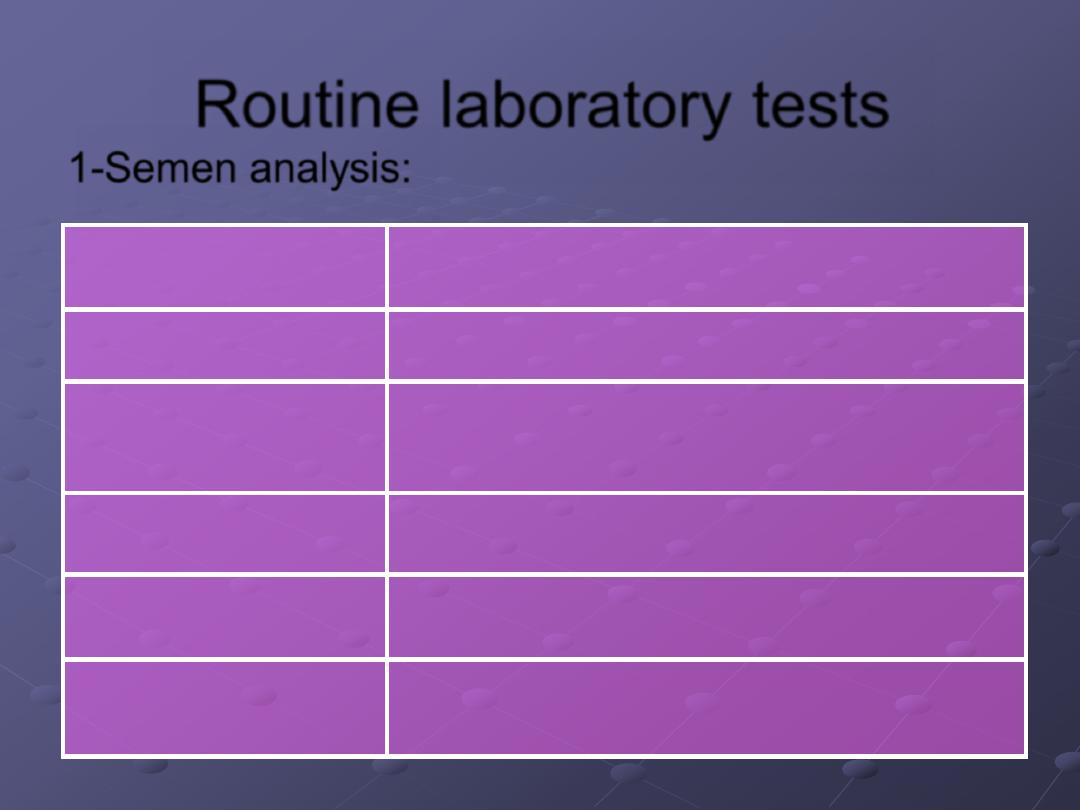
1-
Semen analysis:
2 or more than 2 ml
Volume
7.2-7.8
PH
More than 20x10
6
ml(40million/ml
in ejaculate).
Concentration
More than 50 %
Motility
More than 30%
Morphology
Less than 1x10
6
/ml
WBC
@
At least 25% of spermatozoa should be
swimming with rapid forward movement.
@
At least 50% of the spermatozoa should be
swimming forward, even if only sluggishly.
Routine laboratory tests
1-
Semen analysis:
2-
Basic laboratory tests:
*
LH, FSH, testosterone
*
Serum prolactine.
*
ACTH, TSH, Growth hormone in patients with
hypogonadotrophic hypogonadism.
Routine laboratory tests
A-
Quantitation of the leukocyte in semen
:
By monoclonal antibody technology.
Pyospermia indicate infection.
Anderson has shown that infertile men have
higher WBC counts in their ejaculate than
normal men.
Routine laboratory tests
3-
Additional laboratory tests:
Routine laboratory tests
3-
Additional laboratory tests:
B-
Anti sperm antibody testing (ASA):
Indication
: IF their history of :
1-
Genital infection.
2-
Testicular trauma or biopsy.
3-
Heat- induced testicular damage.
4-
Genital tract obstruction.
5-
If there is clumping or agglutination or SFA
sampling.
6-
Poor post coital test.
4-
Transrectal ultrasound (TRUS):
Indications:
*
Low volume sperm.
*
Acidic azoospermic semen specimens (incomplete
ejaculatory duct obstruction and absence of seminal
vesicle fluid).
Dilated seminal vesicles: Ejaculatory duct
obstruction due to transurethral resection of the
ejaculatory duct (TURED).
*
As guidance during needle aspiration of the seminal
vesicle to determine ejaculatory duct obstruction.
Routine laboratory tests
5-
Vasography:
Can be perform at time of testicular biopsy by
transverse micro incision in the vas., detect
distal and proximal obstruction of vas.
Routine laboratory tests
6-
Testis biopsy (open biopsy):
Reports by Charnny in 1940 about it
’s important in
male infertility.
Indications especially in:
*
Azoospermic patient to differentiating obstruction
from non-obstructive testicular pathology.
*
Severe unexplained oligospermia.
*
Asymmetrical testicular lesion.
*
For mopping of the tests for later sperm aspiration for
ICSI.
Testicular needle biopsy: Little pain and morbidity.
Routine laboratory tests
7-
Assessment of sperm morphology
by fixation of
spermatozoa with Papanicolaou stain.
Criteria of normal spermatozoa:
*
Smooth, oval sperm head.
*
Head measure 3-5 micrometers in length and 2-3
micrometers in width.
*
No neck defect, mid piece and tail.
*
Acrosome comprise 40-70% of sperm head
Any abnormality in morphology of sperms called
teratozoospermia.
Routine laboratory tests
8-
(CASA):
Used since 1980, it
’s costy.
9-
Hypo-osmotic swelling test:
Based up on the
principle that living spermatozoon can maintain an
osmotic gradient where
’s dead cells can’t.
Normally more than 60% of spermatozoa react.
No swelling----very poor IVF results
Routine laboratory tests
10-
Viability stain assay:
Determine if spermatozoa
are alive and plasma membrane intact.
*Live cells exclude dye.
*Damaged dead cells can
’t.
11-
Cervical mucus/ sperm interaction assay.
Routine laboratory tests
12-
Genetic evaluation: Specially in cystic fibrosis
when there is gene mutation:
*
Congenital absence of vas.
*
Y-chromosome micro deletions leading to
spermatogenic impairment and karyotype
abnormalities.
*
Deletion in Y-chromosome lead to oligospermia
and azoospermia.
If sperm density less than 10 million /ml do Y-
chromosome analysis in peripheral blood.
Routine laboratory tests
Treatment of infertility
A-
Fertility drugs:
(forms of hormone therapy).
B-
IUI:
Washed, concentrated sperm from seminal plasma,
placed into uterus through special catheter.
C-
IVF:
Meet egg and sperm invetro and the resulting
embryo implanted into the uterus.
Indication:
*
absence or damaged sperm.
*
ovarian failure.
*
male factors.
*
resistant PCOS.
*
sever endometriosis.
*
unexplained infertility.
Steps of IVF:
1-
Ovarian stimulation.
2-
Egg retrieval.
3-
Fertilization.
4-
Embryo transfer.
GIFT---High pregnancy rate and luteal support.
Treatment of infertility
ART:
Is term that describe several different
methods used to help infertile couples.
Success rate depend on:
1
-Age of the partner.
2
-Reason for infertility.
3
-Clinic.
4
-Type of ART.
5
-If the egg is fresh or frozen.
6
-If the embryo is fresh or frozen.
Treatment of infertility
Assisted Reproductive Technology (ART)
Results of pregnancy:
*
37.3% in women under 35 years.
*
30.2% in women aged 35-37 years.
*
20.2% in women aged 37-40 years.
*
11.0% in women aged 41-42 years.
Treatment of infertility
Assisted Reproductive Technology (ART)
Types:
1-IVF.
2-ZIFT:
Freshly fertilized eggs (zygotes) are placed into tubes
during laproscopy after they have reduced the embryo stage.
3-GIFT:
Transferring eggs and sperm into the woman
’s
fallopian tube. So fertilization occur in the woman
’s body.
4-ICSI:
Specially in sever sperm disorders, older couples and
failed IVF, single sperm injected into mature egg then the
embryo is transferred to the uterus or fallopian tube.
@
Donor egg (women can
’t produce egg).
@
Donor sperm.
Both can be used for women or man has a genetic disease than
can be passed on to the baby.
Treatment of infertility
Assisted Reproductive Technology (ART)
5-Donor insemination.
6-SUZI.
7-TESA:
In non-obstructive azoospermia.
8-PESA:
In obstructed azoospermia.
9-MESA:
In obstructed azoospermia.
Treatment of infertility
Assisted Reproductive Technology (ART)
Classical treatment of infertility
1
-Stop toxic factors.
2
-Treatment of systemic diseases.
3
-Treatment of endocrinopathies.
4
-Treatment of prostatitis and anti sperm antibodies
(systemic steroid).
5
-Treatment of sexual dysfunction.
6
-Non-specific drug treatments.
7
-Treatment of infection by appropriate antibiotics.
8
-Anti oxidant like Vitamin E and Vitamin C.
9
-Varicocele ligation in symptomatic cases but
improvement in fertility is not confirmed.