بسم الله الرحمن الرحيم
Introduction to nephrologyGross anatomy
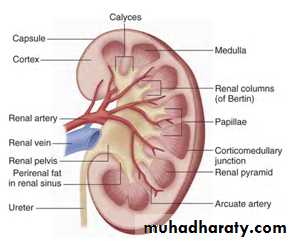
located in the retroperitoneal spaceextend from the 12th thoracic vertebra to the 3rd lumbar vertebra.
the medulla is divided into 8 to 18 striated, conical masses called pyramids.
the apex of the pyramids extends toward the renal pelvis and forms a papilla
On the tip of each papilla are numerous small openings ( the collecting ducts of Bellini).
between the pyramids are portions of cortex, the
septa of Bertin.
The renal pelvis is the saclike dilation of the upper ureter.
the calyces extend from the pelvis and divide into the minor calyces that surround individual papillae.
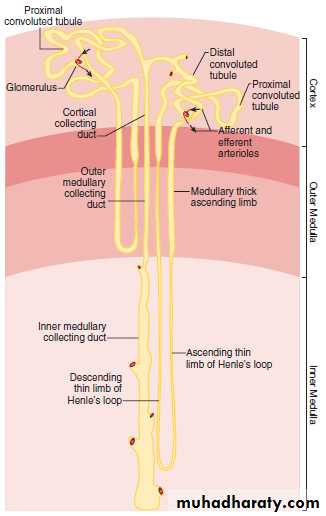
NEPHRON
Each kidney contains about 0.8 to 1.2 × 106 nephrons—the functional units of the kidneyA nephron consists of
• the glomerulus or renal corpuscle,
• the proximal tubule,
• the thin limbs of Henle, and
• the distal tubule
Anatomy of glomerulus
Anatomy of glomerulus
Anatomy of glomerulus
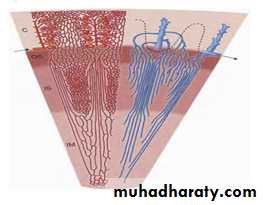
VASCULATUREhas extensive vasculature that accommodates 20 to 25% of the cardiac output.
The main renal A →→ anterior and posterior A→→ into five segmental A.
The segmental arteries →→ interlobar A.
At the corticomedullary junction, the interlobar A→→ arcuate A,
The arcuate A →→ interlobular A, which ascend in the cortex.
The afferent A ←← interlobular A and each →→single glomerulus .
The efferent A exit the glomeruli →→ intricate peritubular microcirculation.
VASCULATURE
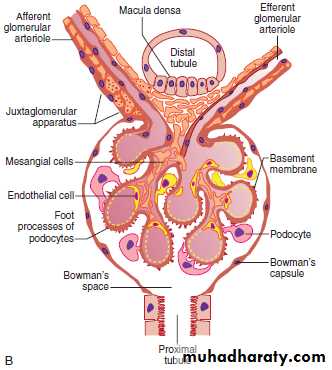
GLOMERULUS ( RENAL CORPUSCLE)
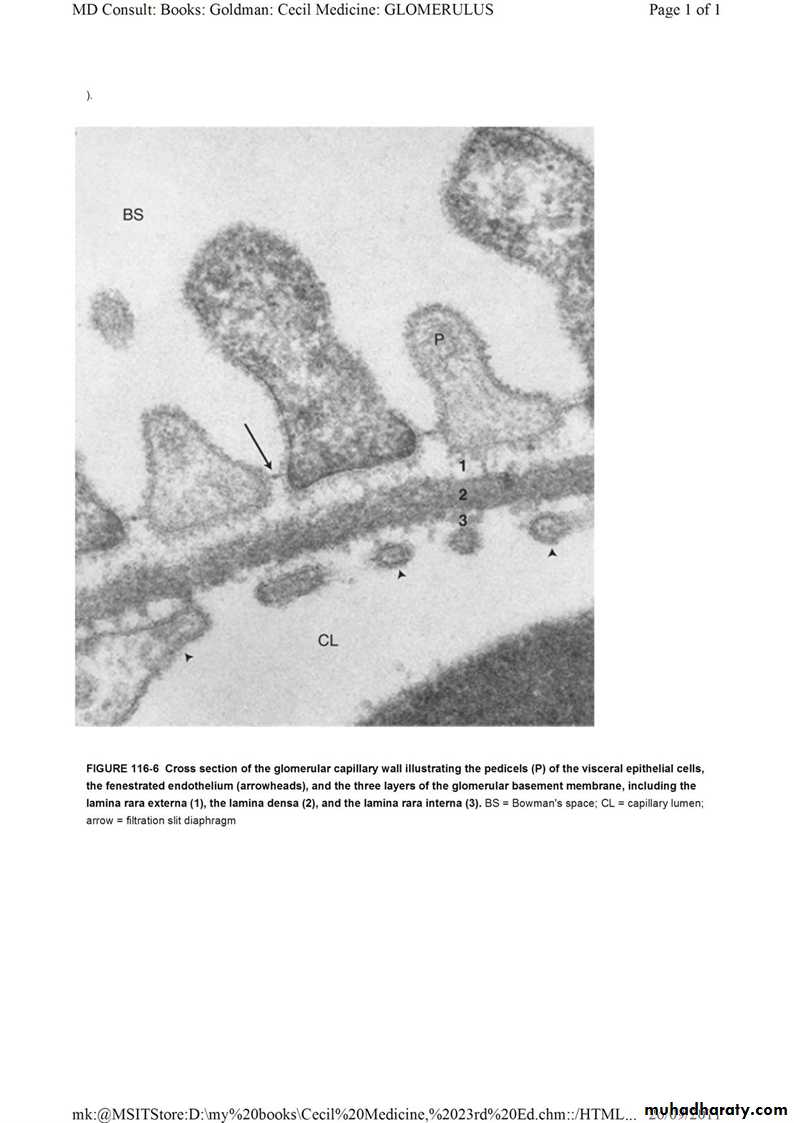
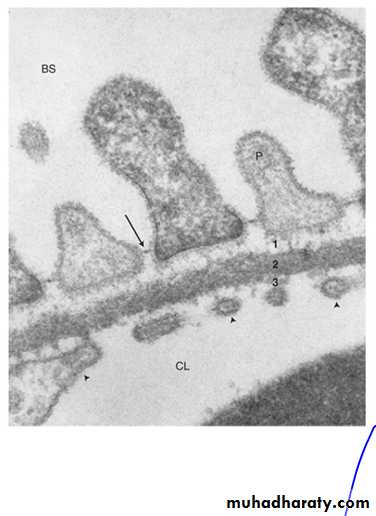
The glomerulus ( glomerular tuft and Bowman's capsule) .The glomerular tuft ( three specialized cells, a basement membrane, and the mesangium).
The specialized cells include
• endothelial cells lining the lumens of the capillaries,
• mesangial cells located in the centrilobular region of the glomerular tuft,
• and the visceral epithelial cells situated on the outer surfaces of the capillaries .
A fourth cell type, the parietal epithelial cell,
GLOMERULUS ( RENAL CORPUSCLE)
• fenestrated endothelium lining the capillary loops,
• the peripheral glomerular basement membrane (GBM), and
• the overlying visceral epithelial cell
Function
In a 70-kg person, the kidney forms 180 L of glomerular filtrate each day through a process termed ultrafiltration.The driving force to move fluid from the glomerular capillaries across the glomerular capillary wall to the urinary space (Bowman's space) is derived from hydraulic pressure
The rate of filtration is proportional to the net ultrafiltration pressure (PUF) that is present across the glomerular capillary wall and is determined by the balance of hydraulic (P) and oncotic (Π) pressures (Starling's forces) that are operative between the glomerular capillary lumen and Bowman's space.
The intrinsic water permeability of the capillary wall (k) and the surface area (A), which together define the ultrafiltration coefficient (Kf), are also important determinants of ultrafiltration.
Function
Because in normal circumstances there is virtually no protein in the ultrafiltrate, the oncotic pressure in the urinary space (ΠT) approaches 0 and does not affect ultrafiltration.Increasing the oncotic pressure in the glomerular capillary (as in multiple myeloma with its characteristic hyperproteinemia), increasing the hydraulic pressure in Bowman's space (via ureteral obstruction), and lowering glomerular capillary hydraulic pressure (as in hypotension) all reduce the SNGFR.
GLOMERULAR BASEMENT MEMBRANE ( GBM )
The GBM is a hydrated gel containing cross-linked molecules that form a complex, three-dimensional lattice-like network .
The GBM is both synthesized and maintained by podocytes and endothelial cells.
Biochemical and immunocytochemical studies have revealed that the GBM is composed of type IV and type V collagens, laminin, heparan sulfate proteoglycans, nidogen, entactin, and other components.
GBM FUNCTION
Physiologic and ultrastructural studies have established that the GBM is a size-selective and a charge-selective barrier to the passage of macromolecules.JUXTAGLOMERULAR APPARATUS
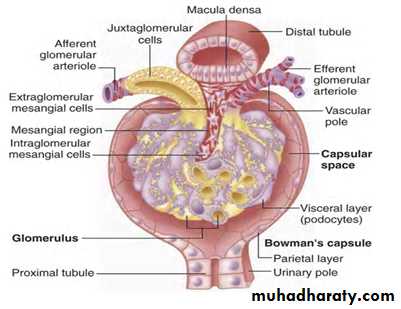
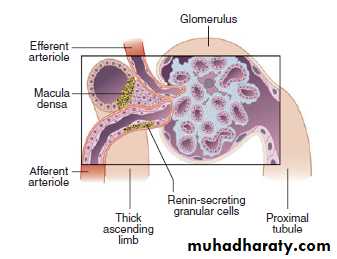
StructureThe juxtaglomerular apparatus is formed by four structures: ( the macula densa, the afferent and efferent arterioles, and the extraglomerular mesangium ).
In the wall of the afferent arteriole are modified smooth muscle cells, the so-called granular cells, which secrete renin.
The macula densa is a plaquelike configuration of specialized cells within the cortical thick ascending limb (TAL) of Henle that is in contact with the extraglomerular mesangium .
Function
The juxtaglomerular apparatus is believed to be responsible for tubuloglomerular feedback
Anatomy of glomerulus
JUXTAGLOMERULAR APPARATUS
StructureThe juxtaglomerular apparatus is formed by four structures: ( the macula densa, the afferent and efferent arterioles, and the extraglomerular mesangium ).
The macula densa is a plaquelike configuration of specialized cells within the cortical thick ascending limb (TAL) of Henle that is in contact with the extraglomerular mesangium .
In the wall of the afferent arteriole are modified smooth muscle cells, the so-called granular cells, which secrete renin.
Function
The juxtaglomerular apparatus is believed to be responsible for tubuloglomerular feedback
PROXIMAL CONVOLUTED TUBUL
Structure
the pars convoluta
the pars recta
The cells contain a well-developed endocytic-lysosomal apparatus that has an important role in the absorption and degradation of macromolecules, such as albumin from the glomerular filtrate. transport
Localization of Na+,K+-ATPase (the sodium pump) in the basolateral membranes explains the active transport of sodium characteristic of this tubule segment.
Numerous elongated mitochondria provide a source of the cellular energy required for active
Proximal convoluted tubule
FunctionThrough iso-osmotic fluid reabsorption, fluid volume is reduced by 60% or more under normal conditions.
The principal driving force for the reabsorption of solutes is the Na+,K+-ATPase .
Sodium is pumped out of the cell actively at the basolateral surface via Na+,K+-ATPase. This process also creates a slight osmotic( AND ELECTROCHEMICAL) gradient that facilitates the reabsorption of fluid.
Water permeability of the proximal tubule is due largely to the presence of a transmembrane protein
Proximal convoluted tubul function
Several hormones lead to RETENTION OF SODIUM by acting at the tubular level (e.g., growth hormone, cortisol, insulin, and estrogen).Parathyroid hormone (PTH), progesterone, and glycogen inhibit the tubular reabsorption of sodium.
Atrial natriuretic peptide— enhances sodium excretion, in part by inhibiting sodium reabsorption by the collecting duct.
Reabsorption of glucose, amino acids, citrate, lactate, acetate, and phosphate also occurs early in the proximal tubule by sodium-coupled active transport processes.
The proximal tubule is also an important site for ammoniagenesis, in which glutamine serves as the substrate.
Ammonia combines with protons to form the ammonium ion (NH4+), which is secreted into the tubule lumen.( metabolic acidosis and hypokalemia).
Thin limb of henle,s loop
play an important role in urine concentration and dilution.
The thin descending limb in the inner medulla has high osmotic water permeability (Lp) because of the presence of the transmembrane protein AQP-1, but low permeability to solutes (PS).This facilitates transfer of water from the tubule lumen to the surrounding hypertonic medullary interstitium and raises the concentration of NaCl and urea in the tubule fluid
Thick ascending limb of henle,s
The TAL actively reabsorbs NaCl, which is mediated by a Na+-K+-2Cl- cotransport mechanism in the apical plasma membrane .The TAL also reabsorbs about 15% of the filtered load of calcium (Ca2+) from the tubular fluid.
Calcium transport is enhanced in the cortical TAL by PTH and cyclic adenosine monophosphate (AMP) and in the medullary TAL by calcitonin and cyclic AMP.
Thick ascending limb of henle,s
Bicarbonate transport is present along the entire TAL through a sodium-coupled HCO3- transport mechanism .The cortical TAL is a major site for reabsorbing magnesium.
Conecting tubule
FunctionPTH affects calcium transport in this segment,
This segment is responsible for reabsorbing sodium and secreting potassium.
The connecting segment is also involved in proton and bicarbonate transport
THANK YOU