Lecturer: Ass.Prof. Dr. Luay Farhood
Class: 5
TH
Class
Time: 1Hour
By the end of this lecture the student should be
able to:
1.
Define the concept of neonatal asphyxia
2.
Clarify the causes of neonatal asphyxia
3.
Identify investigations of neonatal asphyxia
4.
Outline the treatment of neonatal asphyxia
5.
Mention the main birth injuries and it's
mechanisms
Birth asphyxia
Anoxia: indicate the consequences of complete lack
of oxygen as a result of a number of primary causes.
Hypoxia: decreased arterial concentration of oxygen.
Ischemia: insufficient blood flow to cells or organs to
maintain their normal function.
Birth asphyxia is characterised by a critical reduction in
oxygen delivery to the fetus antenatally, during labour
and/or delivery sufficient to produce a lactic acidosis and
render the infant in poor condition at birth with delayed
respiration. It remains an important cause of brain
damage resulting in disability or death.
Asphyxia
APGAR score at 1 minute < 7
Interruption in oxygen delivery to the fetus
• Hypoxia
• Hypercapnia
Neonatal Evaluation and
Resuscitation
APGAR Scoring
A
Appearance
P
Pulse
G
Grimace
A
Activity
R
Respirations
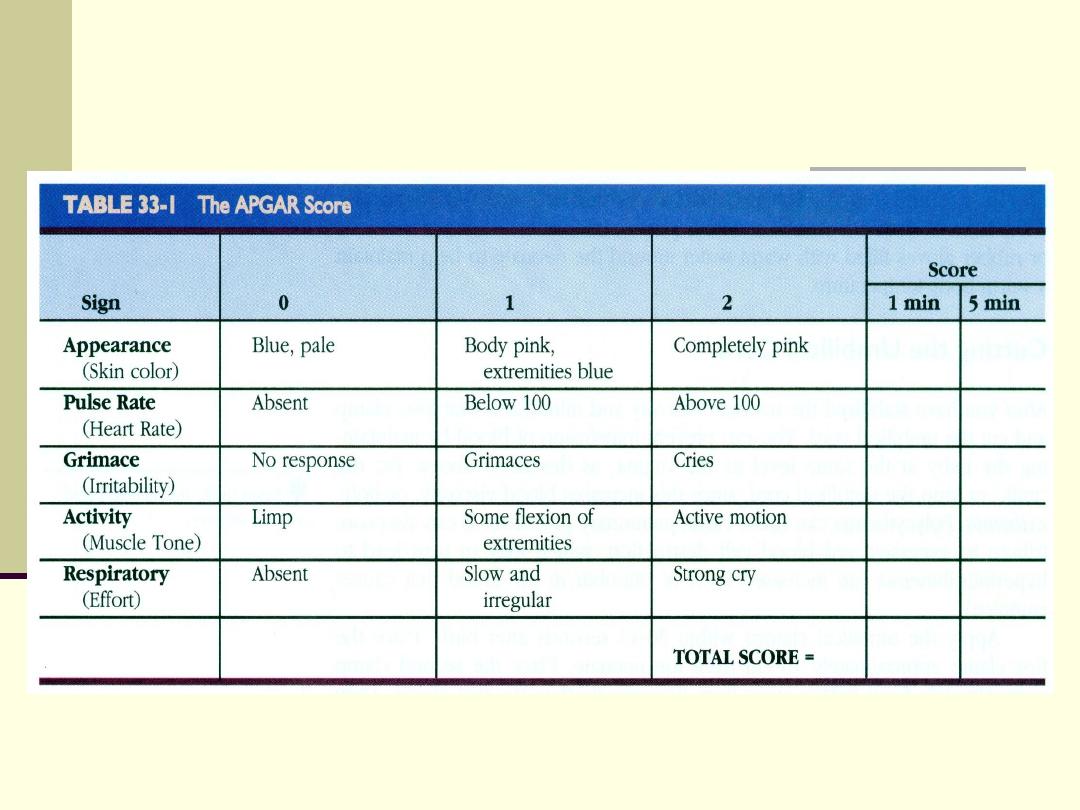
APGAR Score
Apgar Score
Total Score = 10
score 7-10
normal
score 5-6
mild birth asphyxia
score 3-4
moderate birth asphyxia
score 0-2
severe birth asphyxia
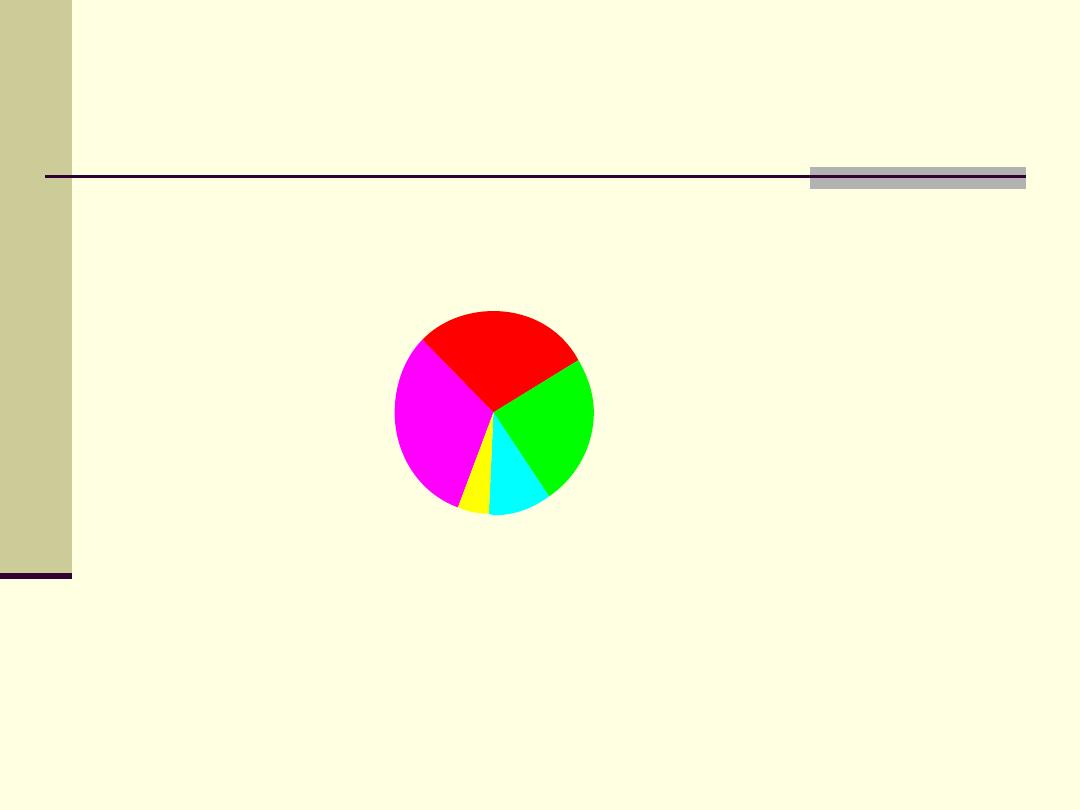
Causes of Neonatal Mortality
Infection
32%
Other
5%
Congenital
Anomalies
10%
Birth Asphyxia
29%
Complications
of Prematurity
24%
Source: WHO 2001 estimates (based on data collected around 1999)
Etiology
Birth asphyxia in undeveloped countries
10% of newborns suffer mild to moderate birth
asphyxia
1% of newborns suffer severe birth asphyxia
Risk factors
Antepartum :
Maternal diabetes
post-term gestation
Pregnancy induced hypertension
multiple gestation
Chronic hypertension
Previous Rh sensitization
maternal drug abuse
Previous stillbirth
maternal age >35 or<16
Bleeding in second or third trimester
no prenatal care
Maternal infection
Polyhydramnios or oligohydramnios
Risk factors
Intrapartum :
Elective or emergency c/s
Precipitous labour, prolonged labour
Prolonged second stage of labour
Premature labour
Abnormal presentation
Rupture of membranes > 24 hours
Foul-smelling amniotic fluid
Non reassuring fetal heart rate patterns
Use of general anesthesia
Prolapsed cord
Assessment
Fetal heart rate slows
Electronic fetal monitoring
• persistent late deceleration of any
magnitude
• persistent severe variable deceleration
• prolonged bradycardia
• decreased or absent beat-to-beat variability
Thick meconium-stained amniotic fluid
Fetal scalp blood analysis show pH less than 7.2
Effects of Asphyxia
Central nervous system
• infarction, intracranial hemorrhage,
cerebral edema, seizure, hypoxic-
ischemic encephalopathy
Cardiovascular
• bradycardia, ventricular hypertrophy,
arrhythmia, hypotension, myocardial
ischemia
Effects of Asphyxia
Respiratory system
• apnea, respiratory distress syndrome
cyanosis
KUB
• acute tubular necrosis, bladder paralysis
Gastrointestinal tract
• necrotizing enterocolitis , stress ulcer
Effects of Asphyxia
Hematology
• Disseminated intravascular coagulation
Metabolic
• hypoglycemia, hyperglycemia,
hypocalcemia, hyponatremia
Integument
• subcutaneous fat necrosis
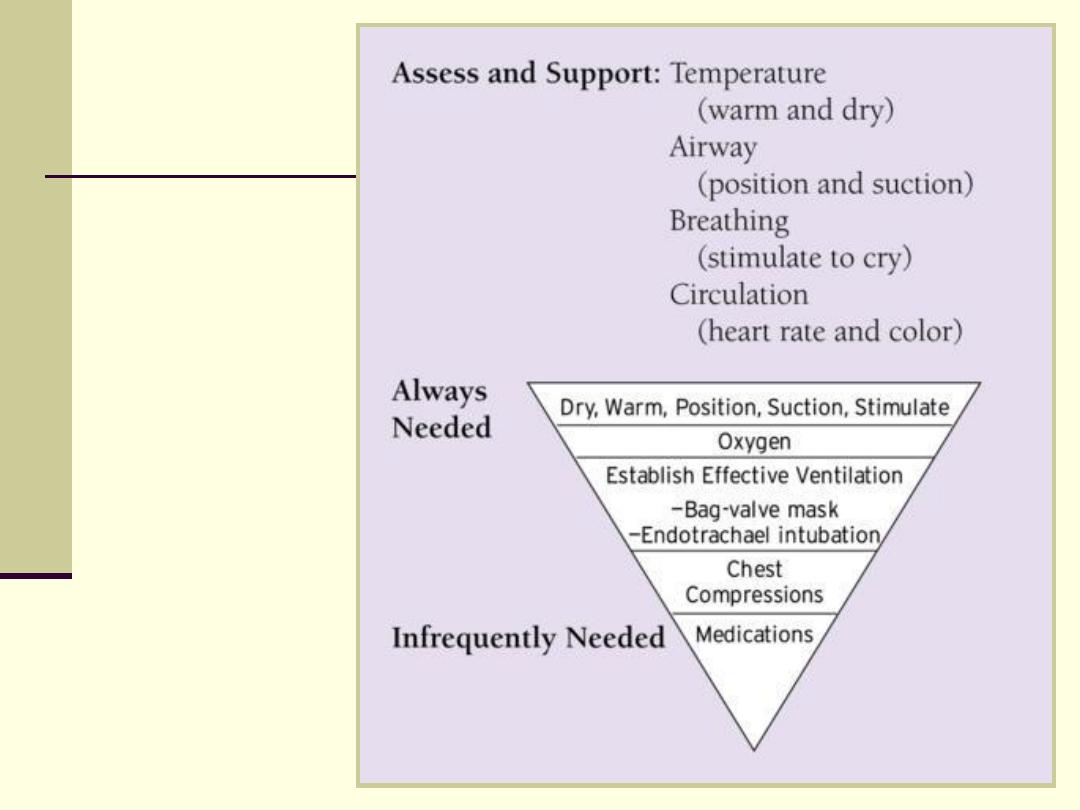
Neonatal
Resuscitation
Newborn Resuscitation
Guidelines
Meconium -stained amniotic fluid: endotracheal
suctioning of the depressed - not the vigorous child
Hyperthermia should be avoided
100% oxygen is still recommended, however if
supplemental oxygen is unavailable room air should be
used
Chest compression: Initiated if heart rate is absent or
remains < 60 bpm despite adequate ventilation for 30
sec
Medications: Epinephrine 0.01-0.03 mg/kg if heart rate
< 60 bpm in spite of 30 seconds adequate ventilation
and chest compression
Volume: Isotonic crystalloid solution
Prognosis
Apgar score < 5 at 10 minutes : nearly 50
death or disability
No spontaneous respiration after 20 min : 60
% disability in survivors
No spontaneous respiration after 30 minutes :
nearly 100 % disability in survivors

Facts About Newborn Resuscitation
The most important is to get air into the lungs
Hypoxic-ischemic encephalopathy(HIE)
is the terminology used in the term infant to describe
the clinical manifestation of brain injury starting
immediately or up to 48 hours after asphyxia,
whether antenatal, intrapartum or postnatal.
Hypoxic-ischemic encephalopathy is an important
cause of permanent damage to central nervous
system cells, which may result in
- neonatal death
- manifest later as cerebral palsy or mental
deficiency
It can be graded as:
mild - the infant is irritable, responds excessively to
stimulation, may have staring of the eyes and
hyperventilation and has impaired feeding
moderate - the infant shows marked abnormalities of
tone and movement, cannot feed and may have
seizures
severe
-
there
are
no
normal
spontaneous
movements or response to pain; tone in the limbs
may fluctuate between hypotonia and hypertonia;
seizures are prolonged and often refractory to
treatment; multi-organ failure is present.
Essential criteria:
1. Metabolic acidosis on cord blood or very early (1 hour) neonatal
blood (pH 7.0 or base deficit > 12 mmol/l.)
2. Early onset of severe or moderate neonatal encephalopathy in
infants of > 34 weeks gestation.
3. Cerebral palsy of the spastic quadriplegic or
dyskinetic type.
4.evidence of hypoxia antenatally (e.g. antepartum haemorrhage) or
during labour (e.g. cord prolapse or markedly abnormal CTG trace)
or at delivery (e.g. shoulder dystocia)
5.resuscitation needed at birth
6.evidence of hypoxic damage to other organs such as liver, kidney,
or heart
7.no other prenatal or postnatal cause identified
8.characteristic findings on neuroimaging.
SECOND PART
BIRTH INJURIES
Birth injuries
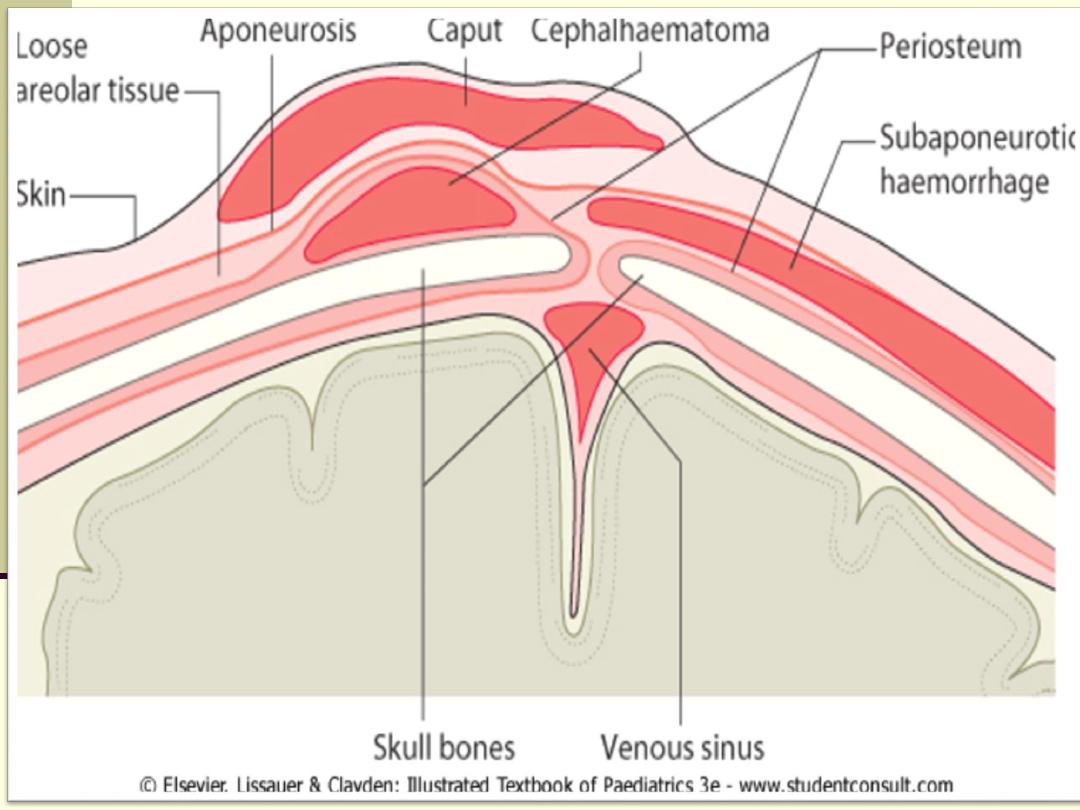
Soft tissue injuries:
caput succedaneum, cephalhaematoma,
chignon, bruises and abrasions
subaponeurotic haemorrhage
Nerve palsies:
brachial plexus - Erb's, Klumpke's
facial nerve
Fractures:
clavicle, humerus, femur
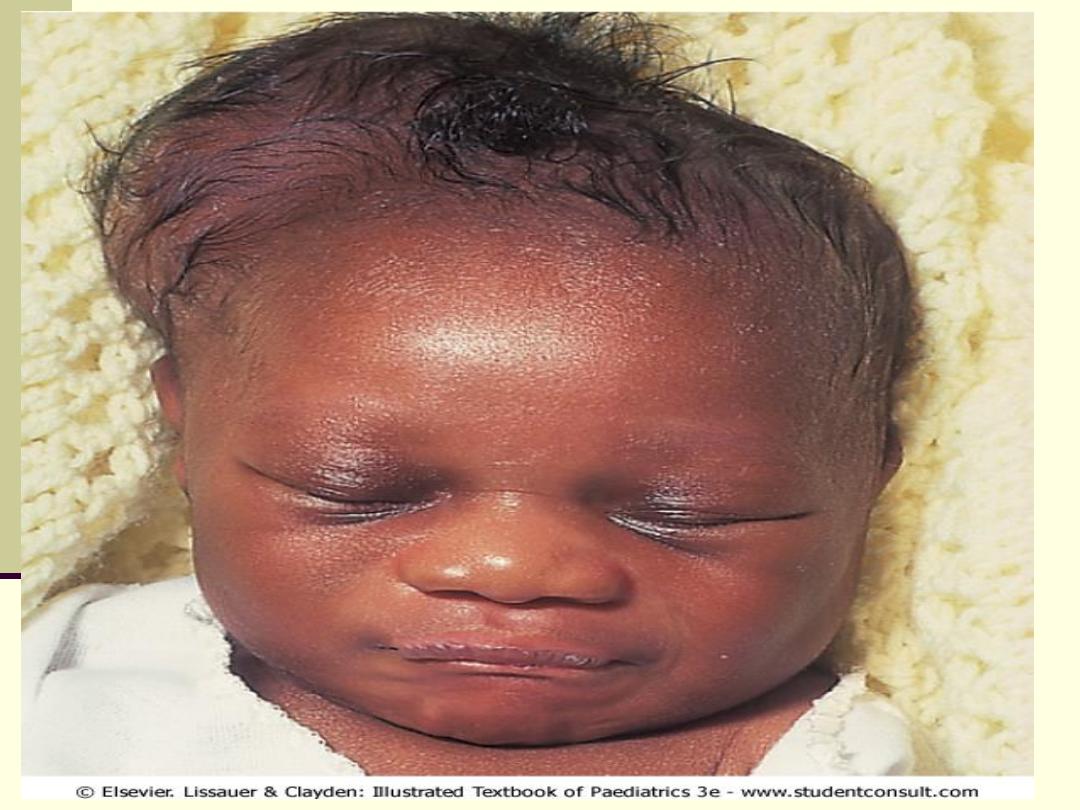
Soft tissue injuries
Caput succedaneum
- bruising and oedema of the presenting part
extending beyond the margins of the skull bones; resolves in a few
days.
Cephalhaematoma
- haematoma from bleeding below the
periosteum, confined within the margins of the skull sutures. It
usually involves the parietal bone. The centre of the haematoma
feels soft. It resolves over several weeks. It is occasionally
accompanied by a linear skull fracture.
Chignon
- oedema and bruising from Ventouse delivery.
Bruising
-to the face after a face presentation and to the genitalia
and buttocks after breech delivery. Preterm infants bruise readily
from even mild trauma.
Abrasions
to the skin from scalp electrodes applied during labour or
from accidental scalpel incision at caesarean section.
Forceps marks
to face from pressure of blades - transient.
Subaponeurotic haemorrhage
(very uncommon) - diffuse, boggy
swelling of scalp, may be accompanied by serious blood loss
leading to hypovolaemic shock.
Nerve palsies
Brachial nerve palsy: results from traction to the brachial plexus nerve
roots. They may occur at breech deliveries or with shoulder dystocia.
Erb's palsy:
Upper nerve root (C5 and C6) injury. The affected arm lies
straight, limp and with the hand pronated and the fingers flexed (waiter's
tip position). It may be accompanied by phrenic nerve palsy causing an
elevated diaphragm.
Klumpke's
palsy: the lower roots are injured, resulting in weakness of
the wrist extensors and intrinsic muscles of the hand.
Most palsies resolve completely, but should be referred to an orthopaedic
surgeon if not resolved by 6 weeks. Ninety per cent recover by 2 years.
facial nerve palsy: compression of the facial nerve by forceps blades or
against the mother's ischial spine. It is unilateral, and there is facial
weakness on crying but the eye remains open.

Fractures
Clavicle:
Usually from shoulder dystocia. A snap may be heard at delivery or
the infant may have reduced arm movement on the affected side,
or a lump from callus formation may be noticed over the clavicle at
several days of age. The prognosis is excellent.
Humerus/femur:
Usually mid-shaft, occurring at breech deliveries, or fracture of the
humerus at shoulder dystocia. There is deformity, reduced
movement of the limb and pain on movement. They heal rapidly
with immobilization.
