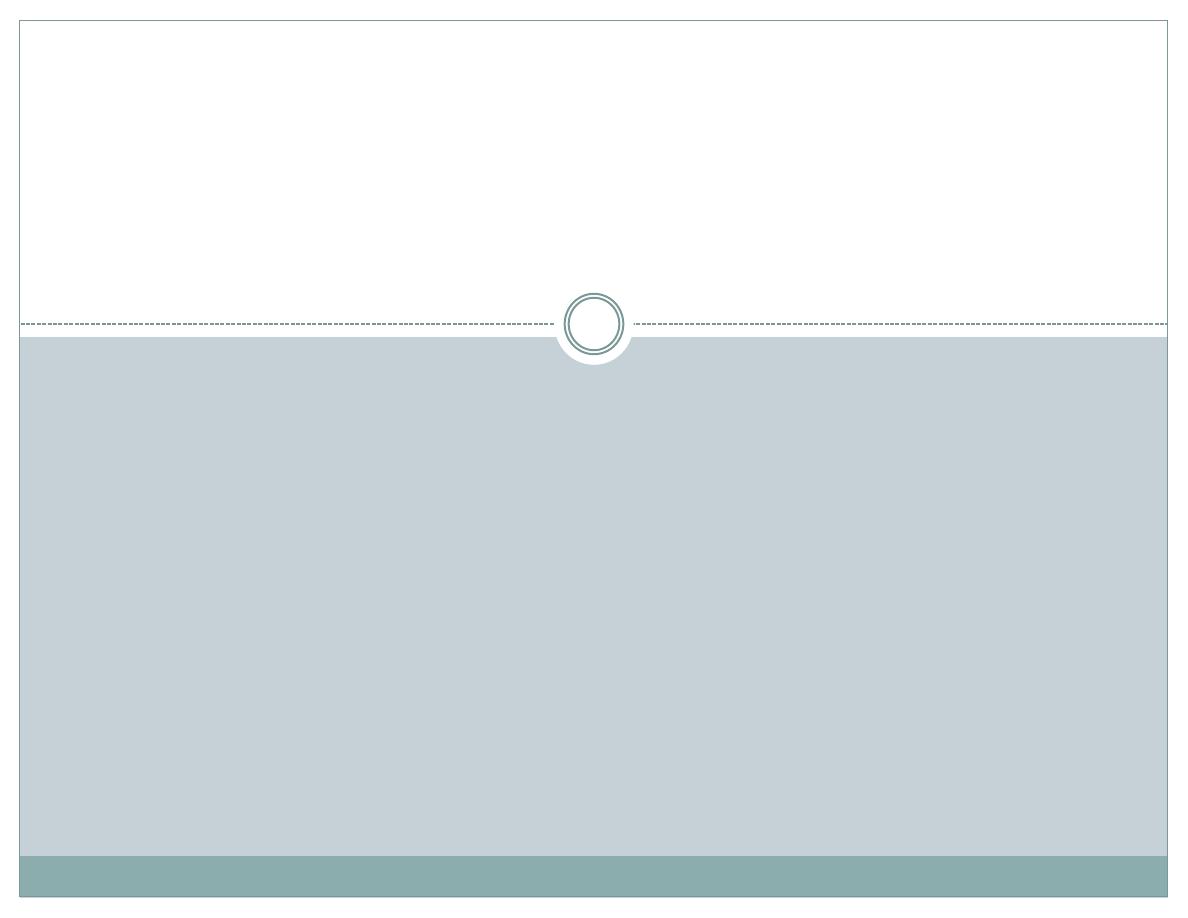
PROF. DR. MOHAMMED A.
YOUNIS
T IK R IT U N IVE R S IT Y
C OLLE G E OF M E D IC IN E
P E D IA T R IC S D E P A R T M E N T
Fever and Sore Throat
Learning Objectives
Determine the aetiology of fever and sore throat
Define the concept, causes, and clinical
manifestations of diphtheria
Outline management of diphtheria
Define the concept ,causes ,and clinical
manifestations of infectious mononucleosis
Outline management of infectious mononucleosis
Diphtheria
Diphtheria
Greek diphthera (leather hide)
Caused by Aerobic Gram +ve rods
Cornyebacterium diphtheriae
Exotoxin production only if infected by
virus phage infected carrying toxin gene
6
Epidemiology
Sources of infection
Patients and asymptomatic carriers
Patients: Transmission time is variable, usually
persist 12 days or less, and seldom more than 4
weeks, without antibiotics.
Etiology
There are three biotypes — gravis,
intermedius, and mitis. The most severe
clinical type of this disease is associated
with the gravis biotype, but any strain may
produce toxin.
Epidemiology
Susceptibility
The susceptibility are influenced by
widespread immunization in childhood and
immunity obtained after infection.
Children of 2-10 years old before widespread
immunization.
the unimmunized or inadequately immunized
adults after widespread immunization.
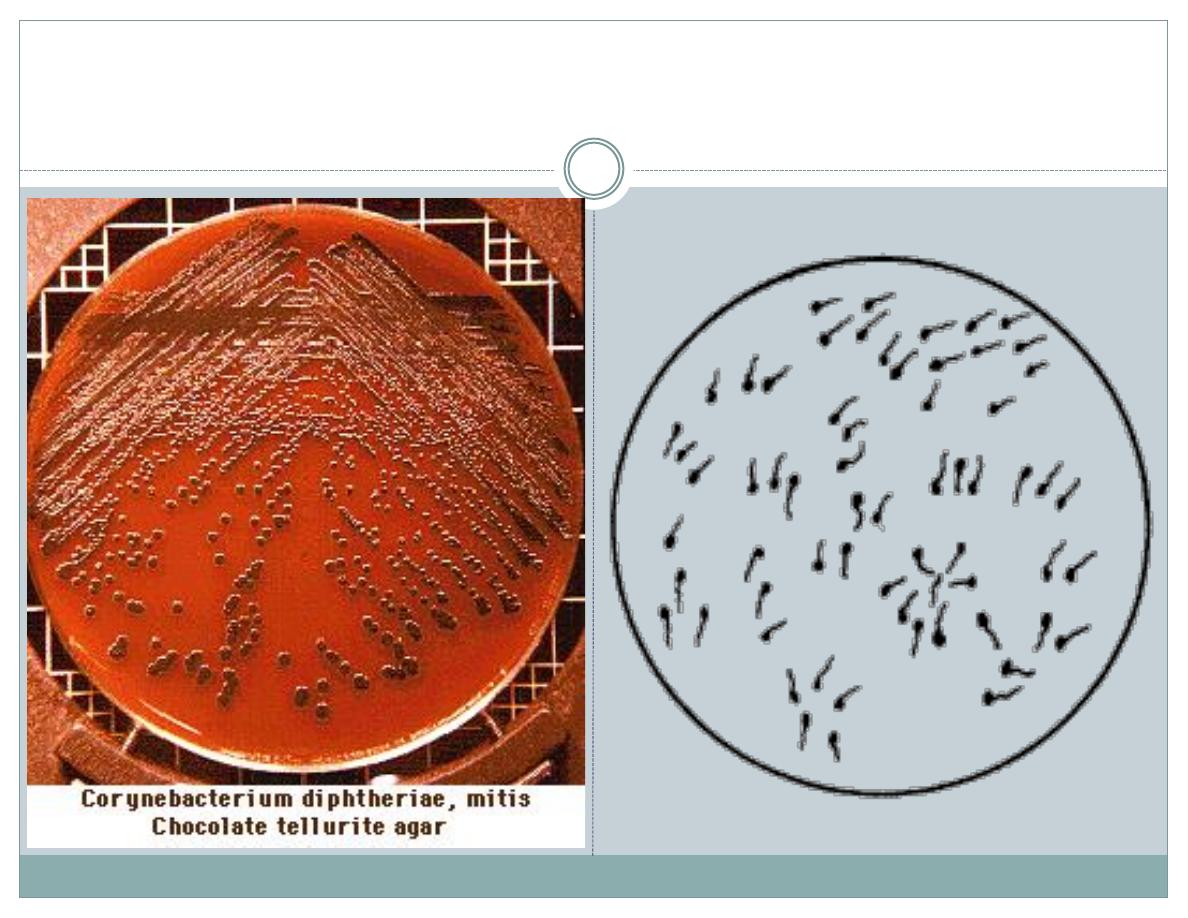
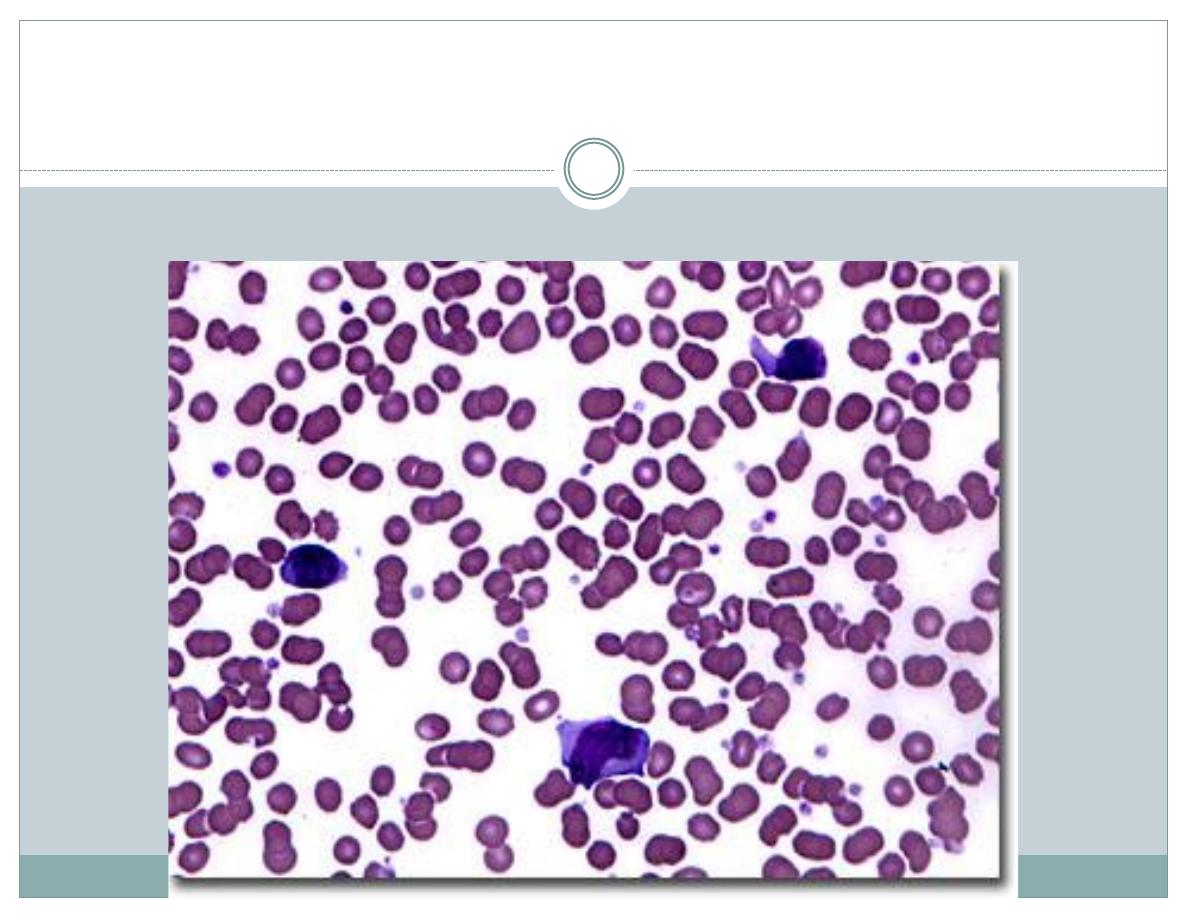
Gram +ve Bacilli and Colonies

Diphtheria Epidemiology
Reservoir
Human carriers
Usually asymptomatic
Transmission
Respiratory
Skin and fomites rarely
Temporal pattern
Winter and spring
Communicability
Up to several weeks
without antibiotics
11
Pathogenesis and pathology
The organism produces a toxin that
inhibits cellular protein synthesis and is
responsible for local tissue destruction and
pseudomembrane formation.
12
Pathogenesis and pathology
The pseudomembrane consists of
coagulated fibrin, inflammatory cells,
destructed mucous tissues and bacteria.
the pseudomembrane in larynx, trachea or
bronchia may have the potential for airway
obstruction.
13
Pathogenesis and pathology
The toxin produced at the site of the
pseudomembrane is absorbed into the
bloodstream and then distributed to the
tissues of the body.
14
Pathogenesis and pathology
The toxin is responsible for the major
complications of myocarditis and neuritis,
and can also cause low platelet counts
(thrombocytopenia) and protein in the
urine (proteinuria).
15
Pathogenesis and pathology
The rapidity of onset, the severity of
disease, and the ultimate outcome are
determined by the site of infection, the
virulence of the strain and the status of
host immunization, in actual, by the site
and magnitude of the local lesions
(pseudomembrane).

Diphtheria Clinical Features
Incubation period 2-5 days
(range, 1-10 days)
May involve any mucous membrane
Classified based on site of infection
anterior nasal
pharyngeal and tonsillar
laryngeal
cutaneous
ocular
genital

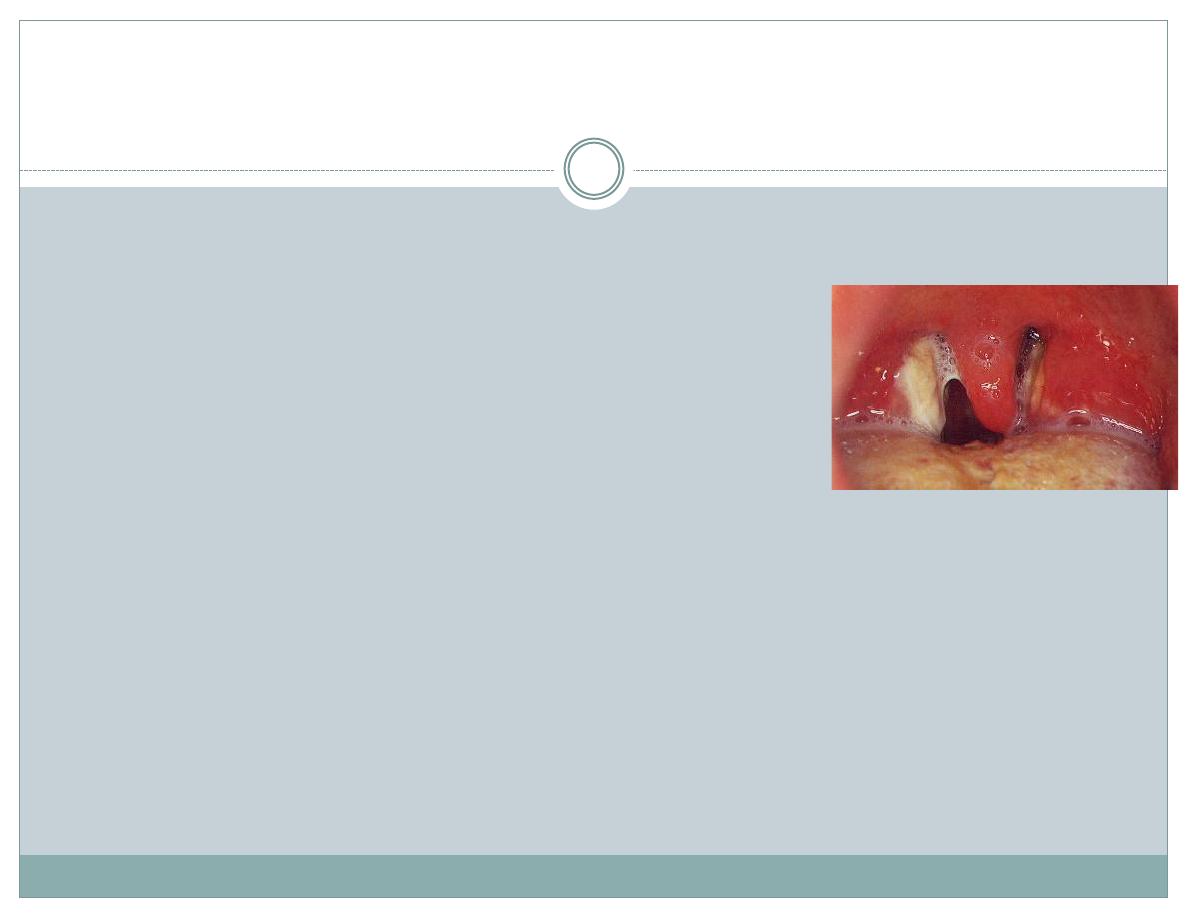
Pharyngeal and Tonsillar Diphtheria
Insidious onset of exudative pharyngitis
Exudate spreads within 2-3 days and may form
adherent pseudo membrane
Membrane may cause respiratory obstruction
Fever usually not high but patient appears toxic

Thick Membrane
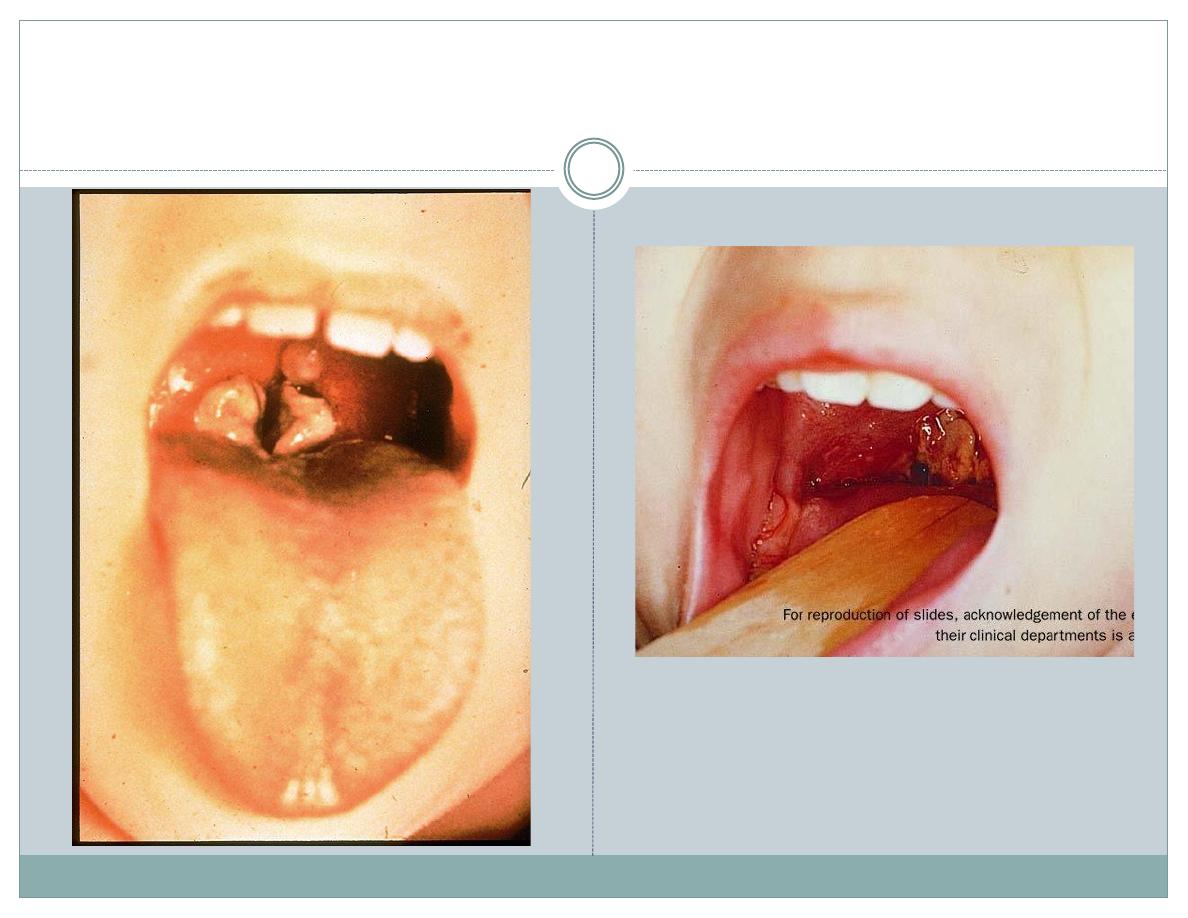
Pseudo membrane
‘Bull Neck’
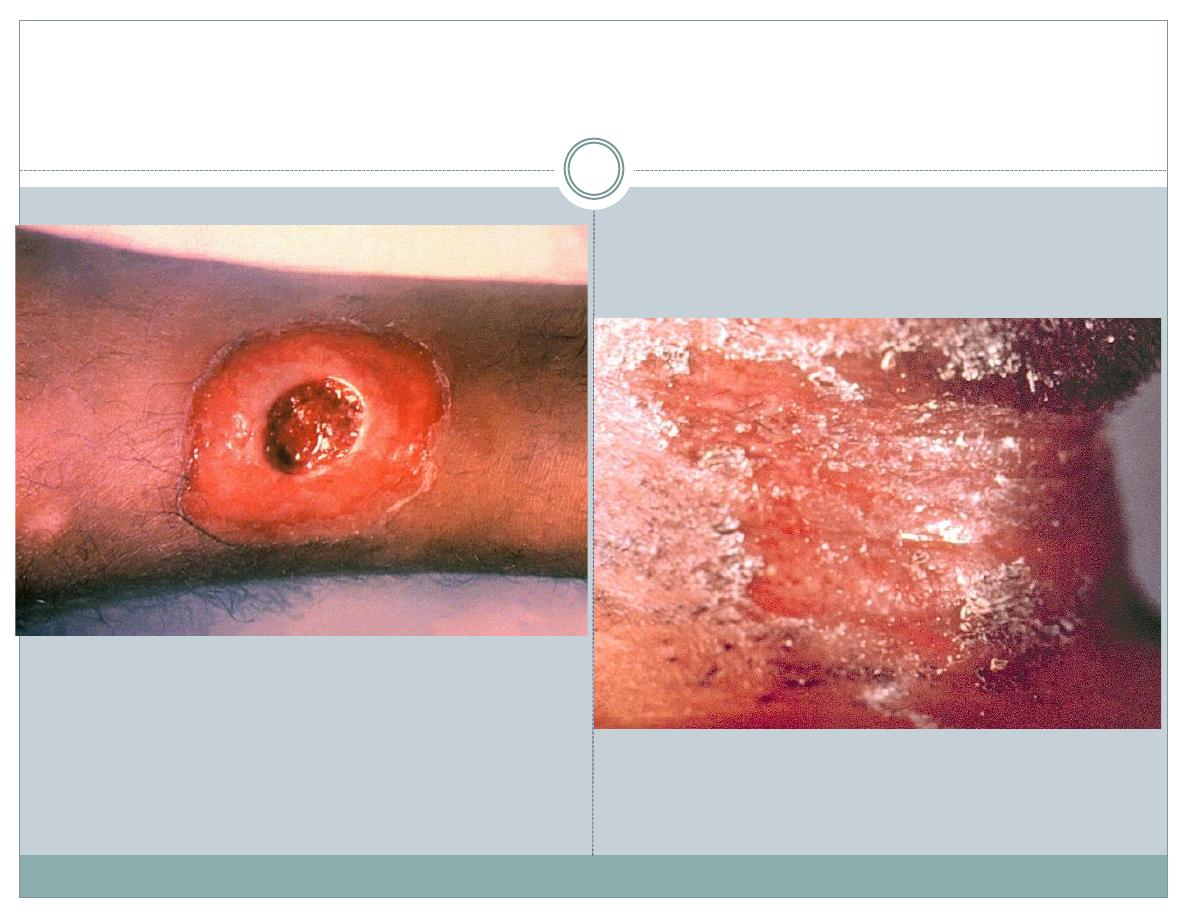
Skin Lesions
Laboratory findings
Routine examination
Leukocytosis, 10~20 G/L, neutrophil is
dominant.
Low platelet count (thrombocytopenia), rise
profiles of the serum enzyme tests and
proteinuria were found in serious cases.
23
Laboratory findings
Bacteriological examinations
Smear and gram stain can found C. diphtheriae, but
can not identify from the diphtheroids.
Laboratory findings
Bacteriological examinations
Fluorescent antibody-stain can found toxigenic C.
diphtheriae, favourable for early diagnosis, but
definitive diagnosis (false positive).

Diphtheria Complications
Mostly attributable to toxin
Severity generally related to extent of local disease
Most common complications are myocarditis and
toxic neuritis with palsy
Death occurs in 5%-10% for respiratory disease
Diphtheria Antitoxin (DAT)
Produced in horses
First used in the U.S. in 1891
Used only for treatment of diphtheria
Neutralizes only unbound toxin
Treatments
Strict isolation
Use antitoxin and antibiotics for
neutralization of free toxin, elimination of
further toxin production and to control
local infection.
Use supportive interventions during
disintoxication.
28
Treatments
General measures
Relax on bed for more than 3 weeks, 4-6 weeks for
patients with myocarditis.
Provide adequate energy and nutriments
29
Treatments
Diphtheria antitoxin
Diphtheria antitoxin, produced in horses.
It will not neutralize toxin that is already fixed
to tissues, but will neutralize circulating toxin.
Early use will prevent progression of disease.
The earlier, the better.
30
Treatments
Diphtheria antitoxin
Diphtheria antitoxin, produced in horses.
It will not neutralize toxin that is already fixed
to tissues, but will neutralize circulating toxin.
Early use will prevent progression of disease.
The earlier, the better.
Treatments
Antibiotics
Procaine penicillin G daily, intramuscularly
(300,000 U/day for those weighing 10 kg or less and
600,000 U/day for those weighing more than 10 kg)
for 7-10 days.
Erythromycin orally or by injection (40-50
mg/kg/day; maximum, 2 gm/day) for 14 days.
Preventions
Protect the susceptibles by vaccination
The effective measure
Primary series (DTP, multivalent vaccine) given at
age of 3, 5, 6 months.
Boosters (DTP) given at 15 months and 4-6 years
old, and booster (DT) every 10 years after then.
DTaP, DT, and Td
DTaP, DT
Td, Tdap
(adult)
Diphtheria
7-8 Lf units
2-2.5 Lf units
Tetanus
5-12.5 Lf units
5 Lf units
Prognosis
The overall case-fatality rate for diphtheria
is about 5%, with higher death rates (up to
20%) in persons <5 and >40 years of age.

Infectious Mononucleosis
Virology
Epstein Barr Virus (EBV)
Herpes Family – (linear DNA virus HHV4)
Surrounded by nucleocapsid and glycoprotein
envelope
Also associated w/ nasopharyngeal carcinoma,
Burkitts lymphoma,
Hodgkins Disease,
B cell lymphoma.
Epidemiology
Worldwide Prevalence of EBV
Infections peak in early childhood and late
adolescence/young adulthood.
By adulthood , 90% of individuals have been
infected and have antibodies to the virus.

Pathogenesis
EBV infects the epithelium of the oropharynx and
salivary glands.
Lymphocytes in the tonsilar crypts are directly
infected -> BLOODSTREAM.
Infected B cells and activated T cells proliferate and
expand.
Polyclonal B cells produce antibodies to host and
viral proteins.
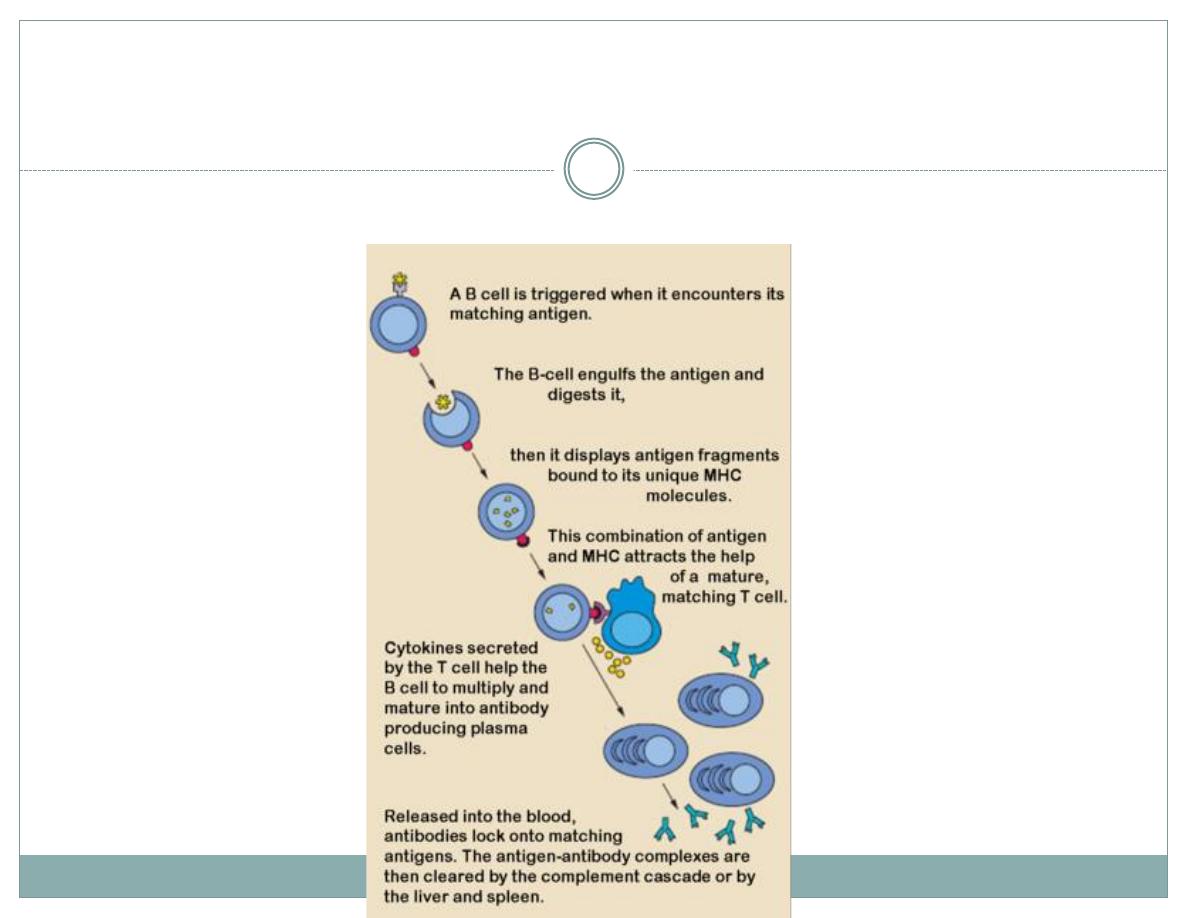
Infectious Mononucleosis
Pathogenesis
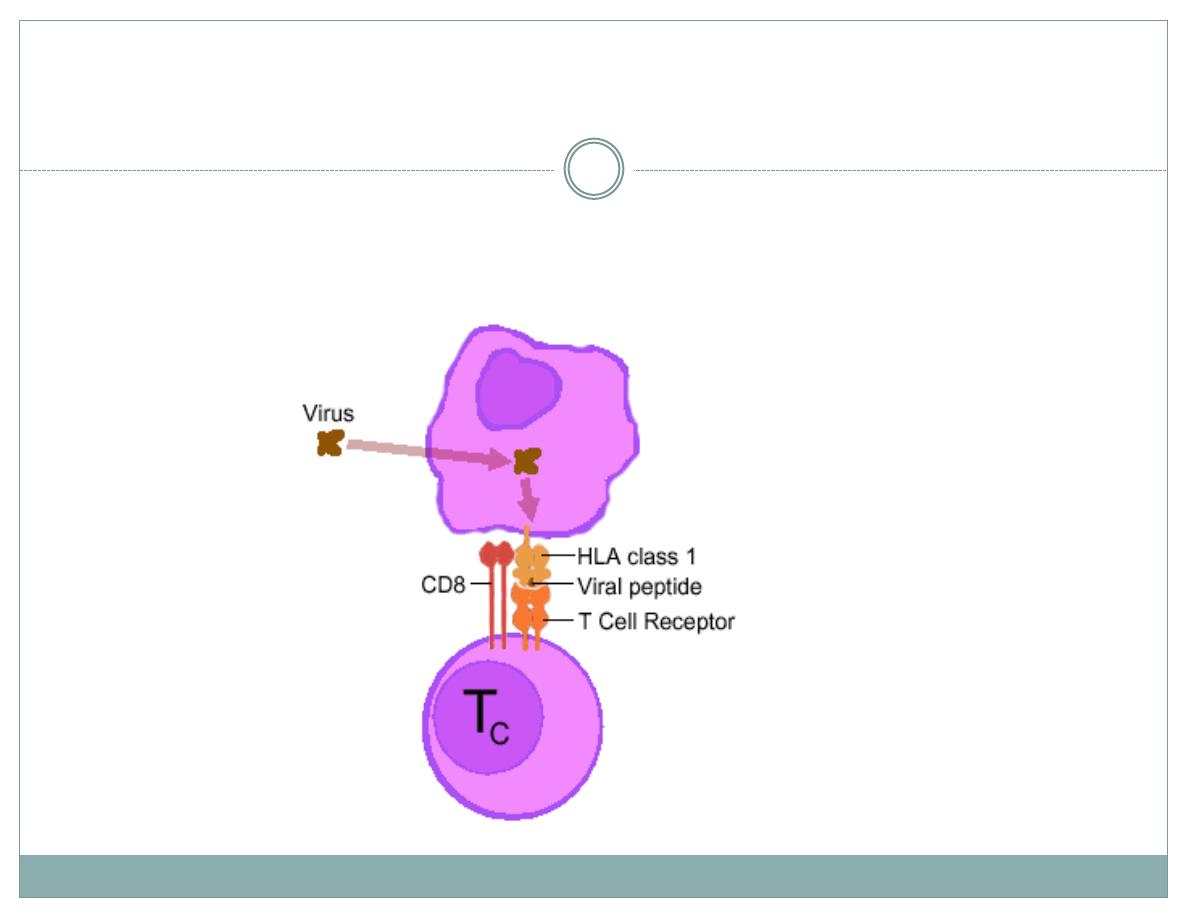
Infectious Mononucleosis
Pathogenesis
Memory B cells (not epithelial cells) are reservoir for
EBV.
EBV receptor is CD21 (found on B cell surface)
Cellular immunity (suppressor T cells, NK cells,
cytotoxic T cells) more important than humoral
immunity in controlling infection
Pathogenesis
Signs & Symptoms
Incubation 4-6 wks
Prodrome (1-2 weeks before illness)
Fatigue, Malaise, Myalgias
Symptoms
Sore throat, Malaise, Headache, Abdominal Pain,
Nausea/Vomiting, Chills
Signs
Lymphadenopathy, Fever, Pharyngitis, Splenomegay,
Hepatomegaly, Rash, Periorbital Edema, Palatal
Enanthem, Jaundice.
Diagnosis
Lymphocytosis (>50% Lymphs)
Atypical Lymphocytes (>10%, mostly CD8+ T
cells)
+Heterophile Antibodies (human serum
agglutinates the erythrocytes of non-human
species) (75% sens, 90% spec) (FP = lymphoma,
CTD, viral hepatitis, malaria)
Monospot -rapid agglutination assay – lower sens
Confirm dx w/ antibodies to viral capsid antigen
(VCA), early antigens (EA) and EBNA
LFTs abnormal in 90%
Diagnosis
Treatment
Rest
Analgesics
Avoid excessive physical activity (risk for splenic
rupture).
Prednisone for severe airway obstruction, hemolytic
anemia, or thrombocytopenia.
No role for acyclovir
Prognosis
Most cases are self limited
Complications include
Meningitis/Encephalitis (<1%)
Splenic rupture (0.1-0.2%)
Upper airway obstruction (<1%)
Bacterial superinfection
Autoimmune hemolytic anemia (3%) (Coombs +, Cold
Agglutnins)
THANK YOU
