Conversional disorders
Conversion disorder is characterized by the occurrence of certain signs
or symptoms that are clearly inconsistent with what is known about
anatomy and pathophysiology. The lifetime prevalence of conversion
disorder is not known with certainty, and estimates range from 0.01% to
0.5% of the general population; it is more common in females, with
female to male ratios ranging from 2:1 up to 10:1.
ONSET
Although conversion disorder may appear at any time from early
childhood up to old age, most patients experience their first symptoms
during adolescence or early adult years. In most cases the actual onset
of symptoms is abrupt and typically follows a major stress in the patient's
life.
ETIOLOGY
Conversion symptoms are more common among the uneducated and
unsophisticated; the actual conversion symptom itself is generally a
reflection or extension of symptoms that the patient has seen in another
or has personally experienced.
In most instances, consequent upon the appearance of the:
conversion symptom there is a reduction in the patient s level of
anxiety.
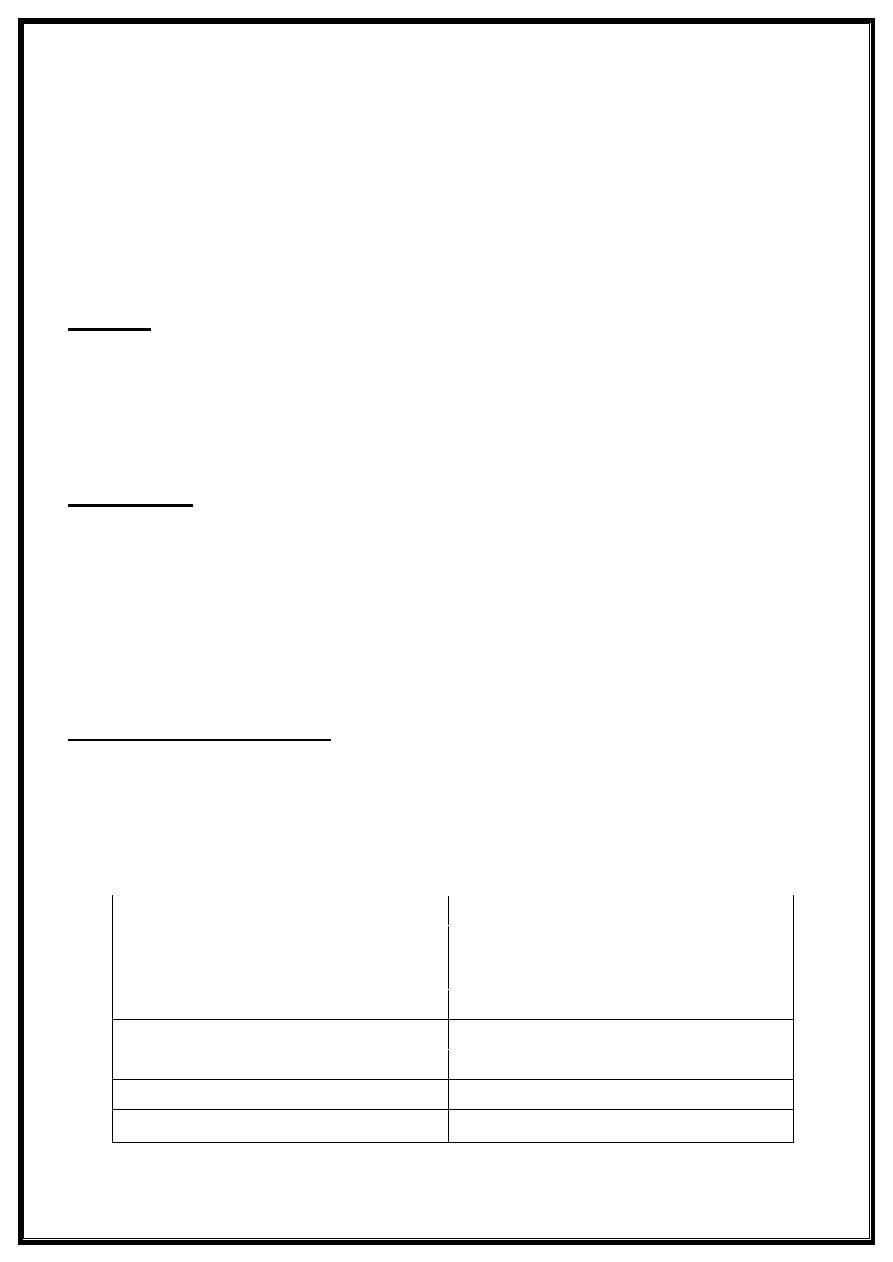
CLINICAL FEATURES
In general, at any given time most patients with conversion disorder have
only one symptom. Some of the more common ones are listed in the box
below, and most of these are described in detail below.
Common Conversion Symptoms
Anesthesia
Parkinsonism
Paralysis
Syncope
Ataxia
Coma
Tremor
Nystagmus
Tonic-clonic Pseudoseizures
Convergencespasm
Deafness
Facial weakness
Blindness
Globus hystericus
Aphonia
Anosmia
Conversion anesthesia
may occur anywhere, but it is most common on the extremities. One
may see a typical "glove and stocking" distribution; however, unlike the
"glove and stocking" distribution that may occur in a polyneuropathy, the
areas of conversion anesthesia have a very precise and sharp
boundary, often located at a joint. The Same non physiologic sharp
boundary may be seen in conversion hemianesthesia, wherein the
boundary precisely bisects the body on a sagittal plane.
In conversion hemiplegia
other abnormalities may be seen; for example, though weak for
many months the affected arm may hang limply at the side, rather
than displaying the typical physiologic flexion posture .Patients with
conversion hemiplegia may also display the "wrong-way tongue"
sign wherein the protruded tongue, instead of deviating toward the
hemiplegic side, as in "true" hemiplegia, deviates instead toward the
normal side. Furthermore, on observation of gait one finds that the
weakened leg is dragged, rather than circumducted. In conversion
paraplegia, one finds normal, rather than increased, deep tendon
reflexes, and the Babinski sign is absent; in doubtful cases the
issue may be resolved by demonstrating normal motor evoked
potentials.
In conversion ataxia
(or, as it has been classically called,astasia- abasia)
a patient, upon attempting to stand or walk, lurches and staggers
forward, arms flinging and trunk swaying, always barely making it to
the safety of bed or chair. Yet when examined in bed, one finds no
limb or truncal ataxia.
Conversion tremor
tends to be coarse and irregular and generally disappears when
the patient is distracted.
Conversion seizures
also known as "hysterical fits" or "non-epileptic seizures/' may
mimic either grand mal or complex partial seizures.
In conversion deafness
the blink reflex to a loud and unexpected sound is present, thus
demonstrating the intactness of the brain stem. Should one suspect
the vanishingly rare bilateral cortical deafness, a brain stem auditory
evoked potential will resolve the issue.
Bilateral conversion blindness
may be suspected when the patient, though complaining of recent
onset of blindness, neither sustains. injury while maneuvering
around the officenor displays any of the expected bruises or
scrapes. The pupillary reflex is present, avisual evoked potential will
resolve the question.
In cases of monocular conversion blindness
one need only demonstrate two things to make the correct
diagnosis: first ,that the peripheral fields are full in the unaffected
eye; and second, that the pupillary response is normal in both eyes.
Conversion aphonia
may be suspected when the patient is asked to cough, for example,
during auscultation of the lungs. ln contrast with other aphonias, the
cough is normally full and loud. A synonym for"globus hystericus"
might be conversion dysphagia; however, this term fails to convey
the essence of the patient's chief complaint, which is a most
distressing sense of having a lump in one's throat. Finding that the
patient can swallow solid food with little difficulty or even that
swallowing liquid may ease the discomfort argues strongly for a
diagnosis of globus.
Diagnosis
The diagnosis is determined after ruling out organic components or other
psychogenic diagnosis. This may involve brain scans such as MRI or CT
scanning as well as blood tests. Electrophysiological studies
(electroencephalography, sensory and motor evoked potentials,
urodynamics) are usually normal. There are no pathological findings in
laboratory tests, supporting CD. On the other hand, however,
pathological findings will not necessarily rule out CD3. Conversion
reactions need to be distinguished from malingering. With malingering,
the patient has a conscious secondary gain in mind.
Treatment
1-Aggressive therapy of comorbid psychiatric illness.
2-Pharmacotherapy Anxiolytic or antidepressant medications.
3-Psychotherapy.
Dr.Hassan M. Al jumaily
Neurologist
