Tikrit Medical College, Urology, Fifth year
1
.أ
د
.
دمحم محسن عبد العزيز
I
I
n
n
g
g
u
u
i
i
n
n
o
o
s
s
c
c
r
r
o
o
t
t
a
a
l
l
C
C
o
o
n
n
d
d
i
i
t
t
i
i
o
o
n
n
s
s
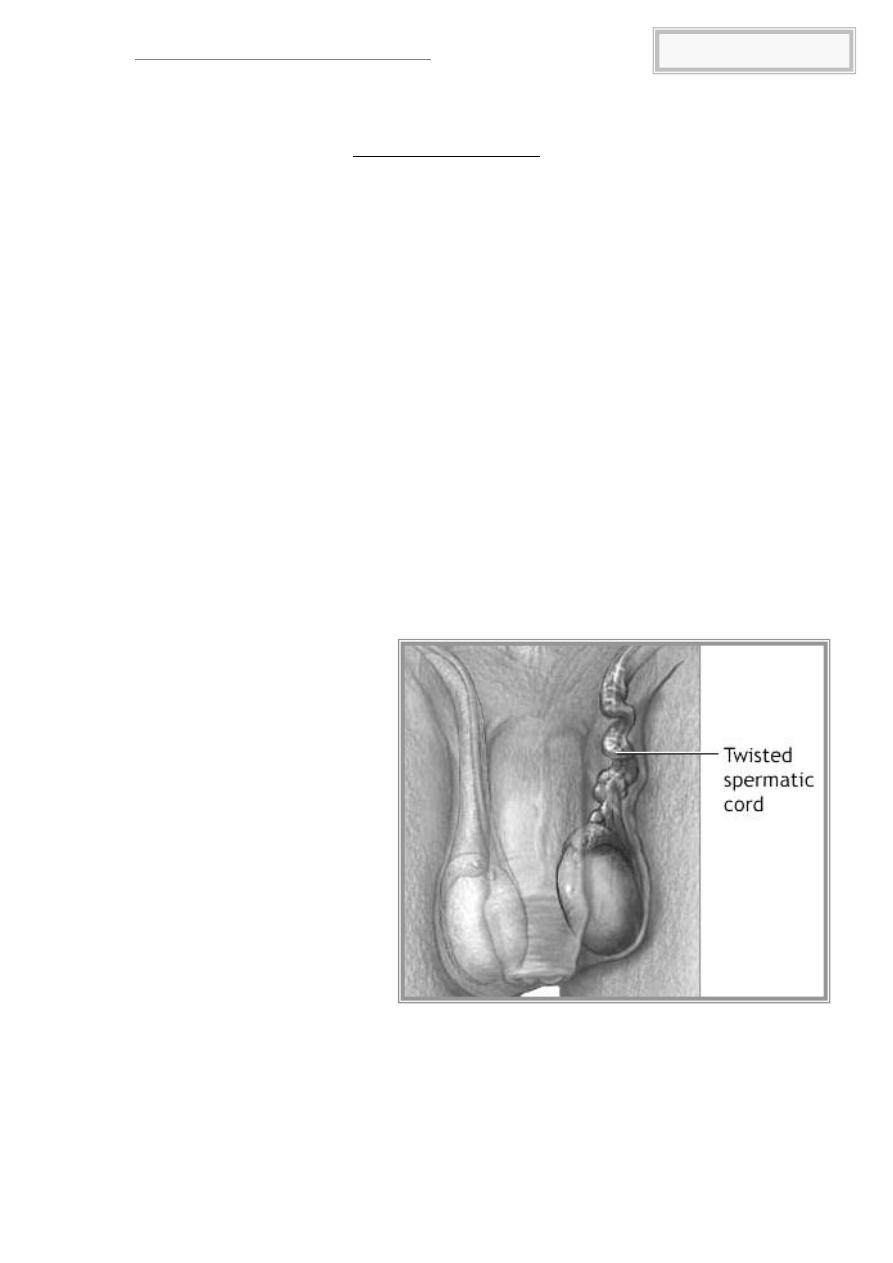
Testicular Torsion
Torsion refers to a twisting of the testis and spermatic cord around a
vertical axis, resulting in venous obstruction, progressive swelling, arterial
compromise, and eventually testicular infarction. Torsion must be considered
in the initial diagnosis of any scrotal pathology because without immediate
detorsion, the testis will be lost. This condition can occur at any age but is
most common among adolescents. It is the result of an abnormally narrowed
testicular mesentery, with the tunica vaginalis almost completely surrounding
the entire testis and epididymis. This narrowed mesentery facilitates twisting
of the testis within the tunica vaginalis about its vascular pedicle and gives an
appearance termed the bell-clapper deformity.
Diagnosis
The typical patient presents with sudden onset of pain and swelling,
occasionally associated with some minor trauma. The testis will be tender, is
often high in the scrotum because of shortening by the twisted cord, and
may have a transverse lie or an anteriorly positioned epididymis.
Urinalysis is usually negative. Elevation of the scrotum will not relieve the
pain (negative Prehn's sign). Color-flow Doppler ultrasonography should be
obtained without hesitation and has become the test of choice. A radionuclide
testicular scan may be useful in equivocal cases if performed early after the
onset of symptoms and before significant reactive hyperemia of the scrotal
skin occurs. Surgical exploration is the best diagnostic test and should not be
delayed if this diagnosis is seriously considered.
Treatment
Treatment
consists
of
immediate
detorsion.
Correction within 4-6 hours of
onset of pain usually results in
a normal testis. Delay for more
than 12 hours results in poor
testicular
salvage
(~20%).
Manual detorsion can be
attempted by either lifting the
scrotum or rotating the testis
about its vascular pedicle.
Successful manual detorsion
must still be followed by
surgical
orchiopexy.
An
unsuccessful
attempt
at
manual detorsion requires
immediate
surgical
exploration.
The
clearly
infarcted testis should be removed; however, if viability is in doubt, it should
be left in situ because Leydig cell function may be preserved. After detorsion,
the testis should be fixed to the scrotal wall. The contralateral testis must also
be fixed because of the high incidence of its subsequent torsion.
Tikrit Medical College, Urology, Fifth year
2
.أ
د
.
دمحم محسن عبد العزيز
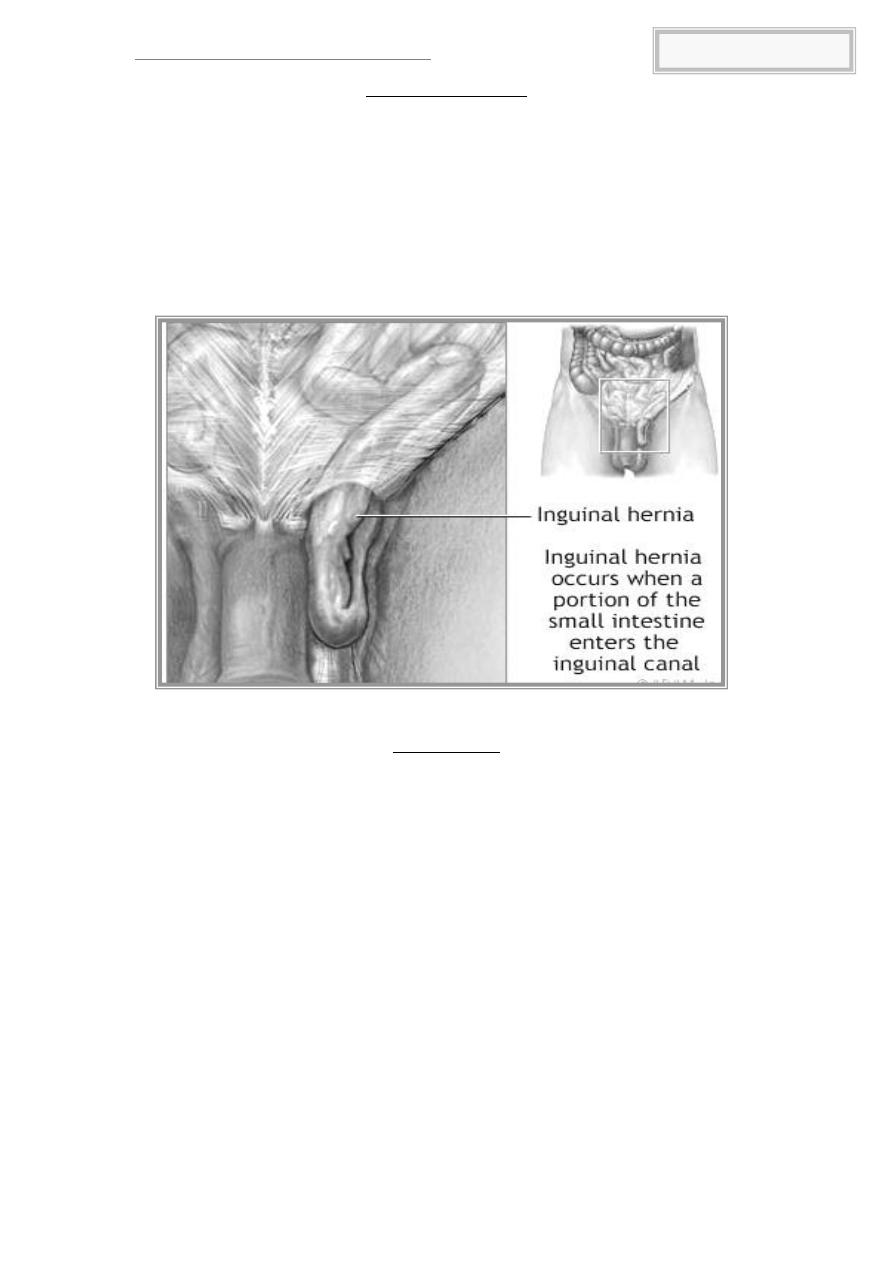
Inguinal Hernia
An inguinal hernia often is first seen as a scrotal mass secondary to
loops of bowel within the scrotum. Indirect inguinal hernias may be secondary
to a patent processus vaginalis or protrusion of a new peritoneal process
following the same path along the cord into the scrotum. Direct inguinal
hernias result from weakness of the transversalis fascia at Hesselbach's
triangle, with peritoneal outpouching into the area of the external ring only,
rarely descending into the scrotum. An inguinal hernia that cannot be reduced
is said to be incarcerated. If the vascular supply of the herniated organ
(usually bowel) is compromised, it is said to be strangulated surgical
emergency. Treatment is usually surgical.
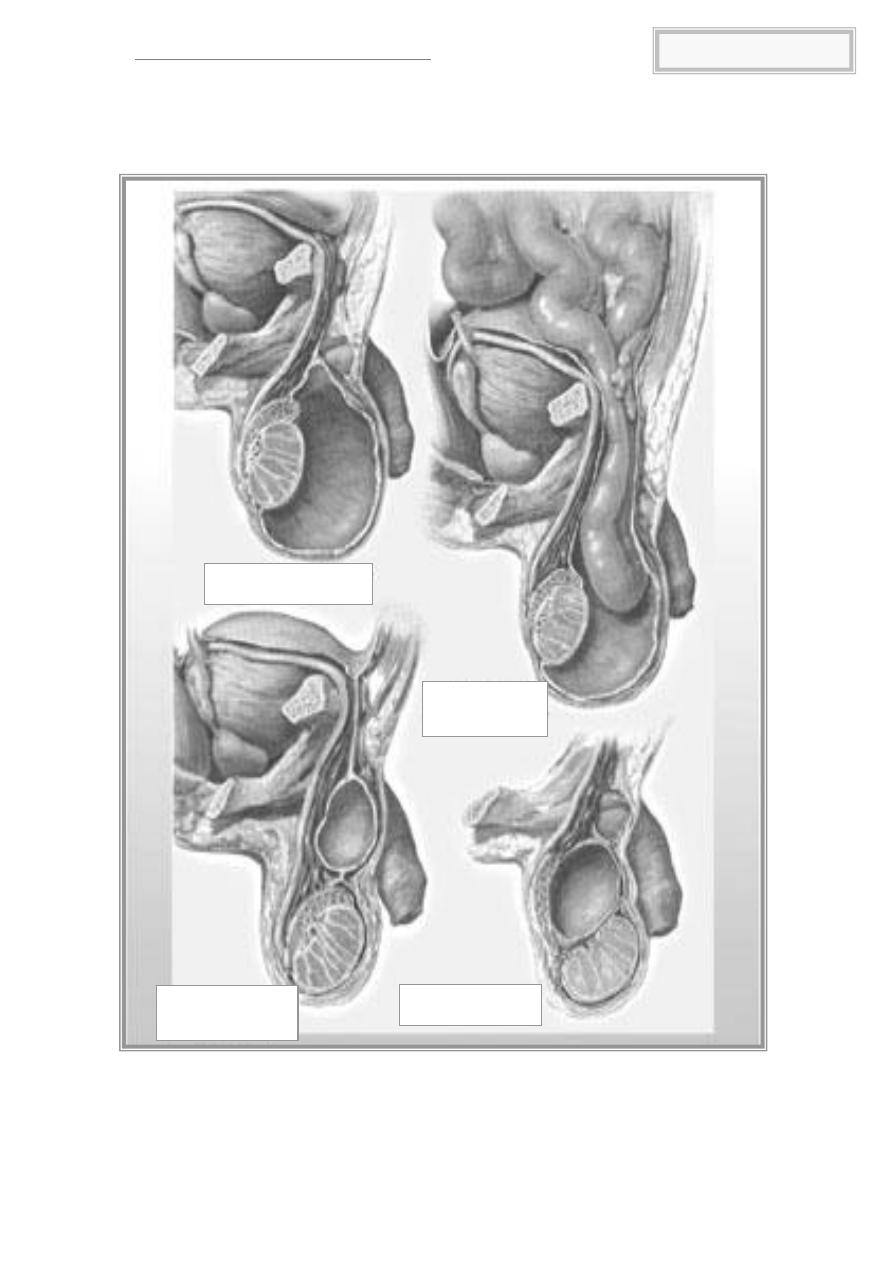
Hydrocele
A hydrocele is a fluid collection within the tunica vaginalis surrounding
the testis or the processus vaginalis ( hydrocele of the cord) . It presents as a
painless swelling of the scrotum that transilluminates. It often makes
testicular palpation difficult and can conceal an underlying testicular tumor.
Congenital or Infant Hydroceles
Congenital or infant hydroceles are usually the result of peritoneal fluid
accumulation within the scrotum via a patent processus vaginalis and occur in
6% of full-term boys. Their size often changes from day to day or with
recumbency. Treatment should be delayed during the first year of life because
normal spontaneous closure of the processus vaginalis may occur. After 1 year,
surgical ligation of the processus vaginalis should be undertaken.
Acquired or Adult Hydroceles
Acquired or adult hydroceles are usually idiopathic but may be
secondary to tumor, infection, trauma or systemic disease. An imbalance in
fluid secretion and absorption by the tunica vaginalis has been suggested as a
possible cause. Treatment is generally indicated to allow easy palpation of the
testis or because of symptomatic discomfort or disfigurement. Definitive
therapy is surgical drainage and excision of tunica vaginalis.
Tikrit Medical College, Urology, Fifth year
3
.أ
د
.
دمحم محسن عبد العزيز
Simple Hydrocele
Hydrocele
with Hernia
Hydrocele of the
Cord
Spermatocele
Tikrit Medical College, Urology, Fifth year
4
.أ
د
.
دمحم محسن عبد العزيز
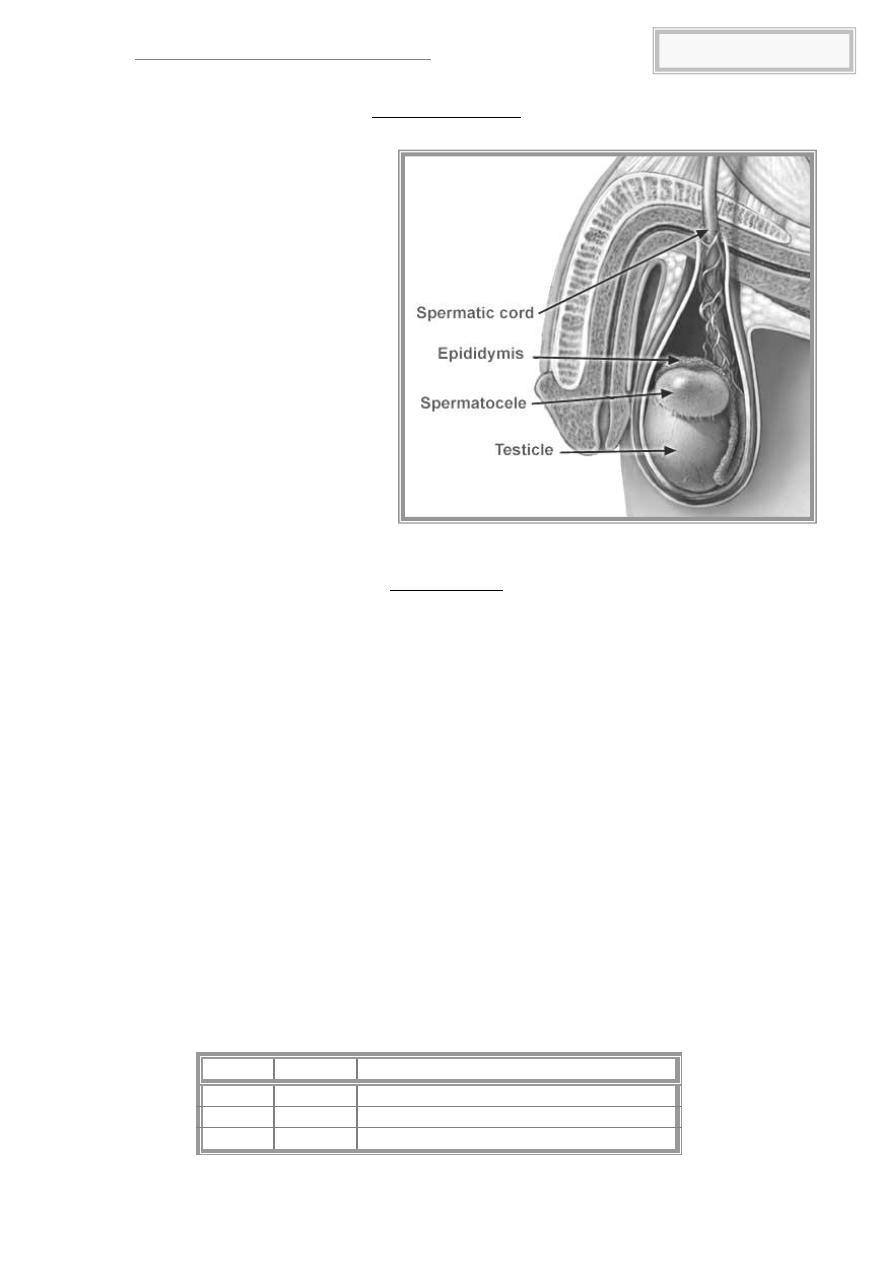
Spermatocele
A spermatocele is an
epididymal cyst that arises
from the efferent ductules and
holds a cloudy fluid containing
spermatozoa. It presents as
a painless, cystic mass that lies
above and anterior to the
testis. Ultrasound can confirm
the diagnosis if doubt exists.
Treatment
consists
of
spermatocelectomy
for
extensive
involvement.
Therapy should be avoided in
young male patients concerned
with fertility.
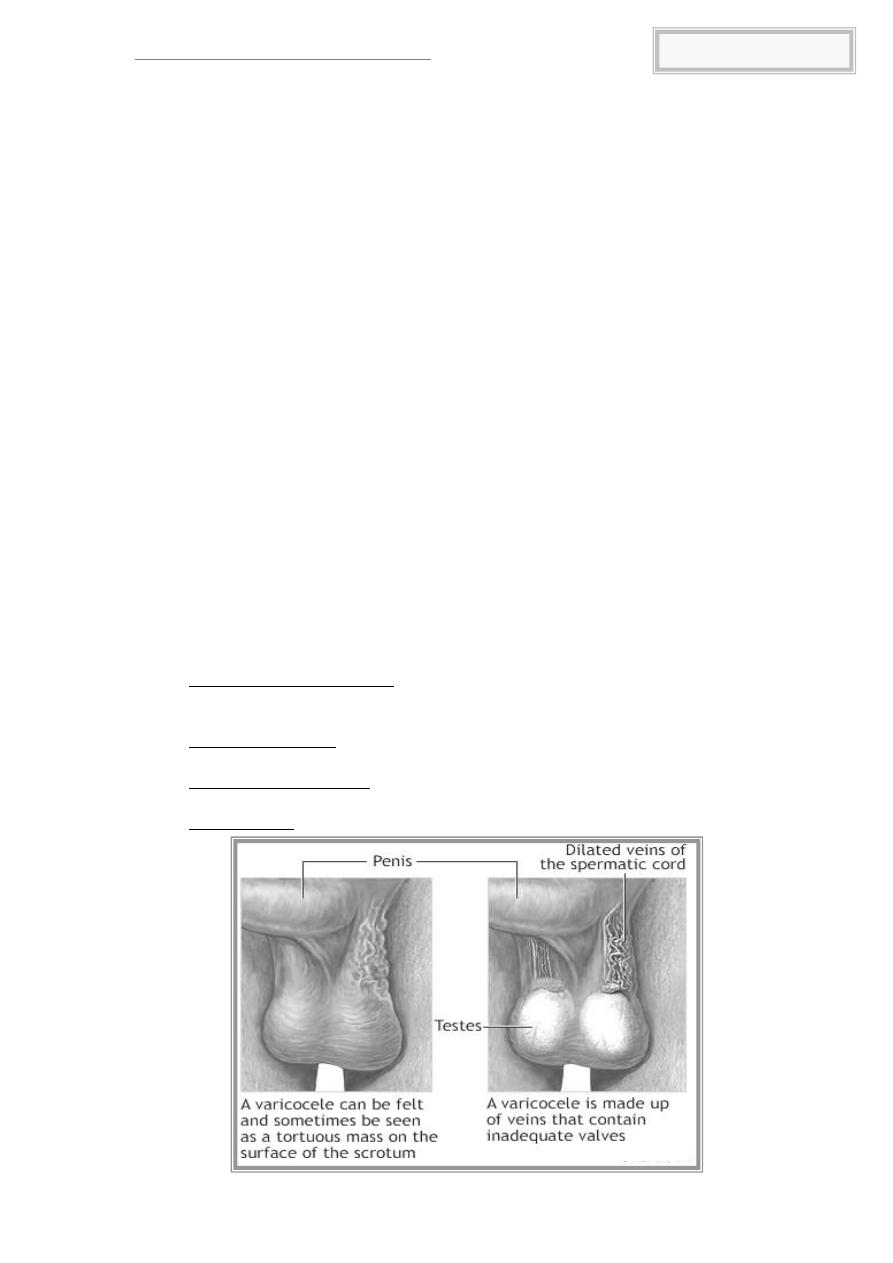
Varicocele
Definition
Dilatation and tortuosity of the veins of the pampiniform plexus of the
spermatic cord.
Prevalence
Found in 15% of men in the general population and 40% of males
presenting with infertility. Bilateral or unilateral (left side affected in 90%).
Aetiology
Incompetent values in the internal spermatic veins lead to retrograde
blood flow, vessel dilatation, and tortuosity of the pampiniform plexus. The
left internal spermatic vein enters the renal vein at right angles, and is under a
higher pressure than the right vein, which enters the vena cava obliquely at a
lower level. As a consequence, the left side is more likely to develop a
varicocele.
Pathophysiology
Testicular venous drainage is via the pampiniform plexus, a meshwork
of veins encircling the testicular arteries. This arrangement normally provides
a counter-current heat exchange mechanism which cools arterial blood as it
reaches the testis. Varicoceles adversely affect this mechanism, resulting in
elevated scrotal temperatures and consequent deleterious effects on
spermatogenesis (± loss of testicular volume).
Varicocele grading system
Grade
Size
Definition
1
Small Palpable only with Valsalva manoeuvre
2
Moderate
Palpable in a standing position
3
Large
Visible through the scrotal skin
Tikrit Medical College, Urology, Fifth year
5
.أ
د
.
دمحم محسن عبد العزيز
Presentation
The majority of varicoceles are asymptomatic, although large
varicoceles may cause pain or a heavy feeling in the scrotal area. Examine
both lying and standing, and ask patient to perform Valsalva manoeuvre
(strain down). A varicocele is identified as a mass of dilated and tortuous veins
above the testicle (described as feeling like a bag of worms), which
decompress on lying supine. Examine for testicular atrophy.
Investigation
Scrotal Doppler ultrasound scan is diagnostic.
Semen analysis: varicoceles are associated with low or absent sperm
counts, reduced sperm motility, and abnormal morphology, either
alone or in combination (oligoasthenoteratospermia (OAT) syndrome).
Management
The significance of a varicocele is its association with infertility.
Indications for varicocelectomy include oligospermia, decreased sperm
motility, and a painful symptomatic varicocele.
Embolization
Interventional radiological technique where the femoral vein used to
access the spermatic vein for venography and embolization (with coils or other
sclerosing agents).
Surgical ligation
Retroperitoneal approach: a muscle-splitting incision is made near the
anterior superior iliac spine, and the spermatic vessels are ligated at
that level.
Inguinal approach: the inguinal canal is incised to access the spermatic
cord, and the veins are tied off as they exit the internal ring.
Subinguinal approach: veins are accessed and ligated via a small
transverse incision below the external ring.
Laparoscopic: veins are occluded high in the retroperitoneum.

Tikrit Medical College, Urology, Fifth year
6
.أ
د
.
دمحم محسن عبد العزيز
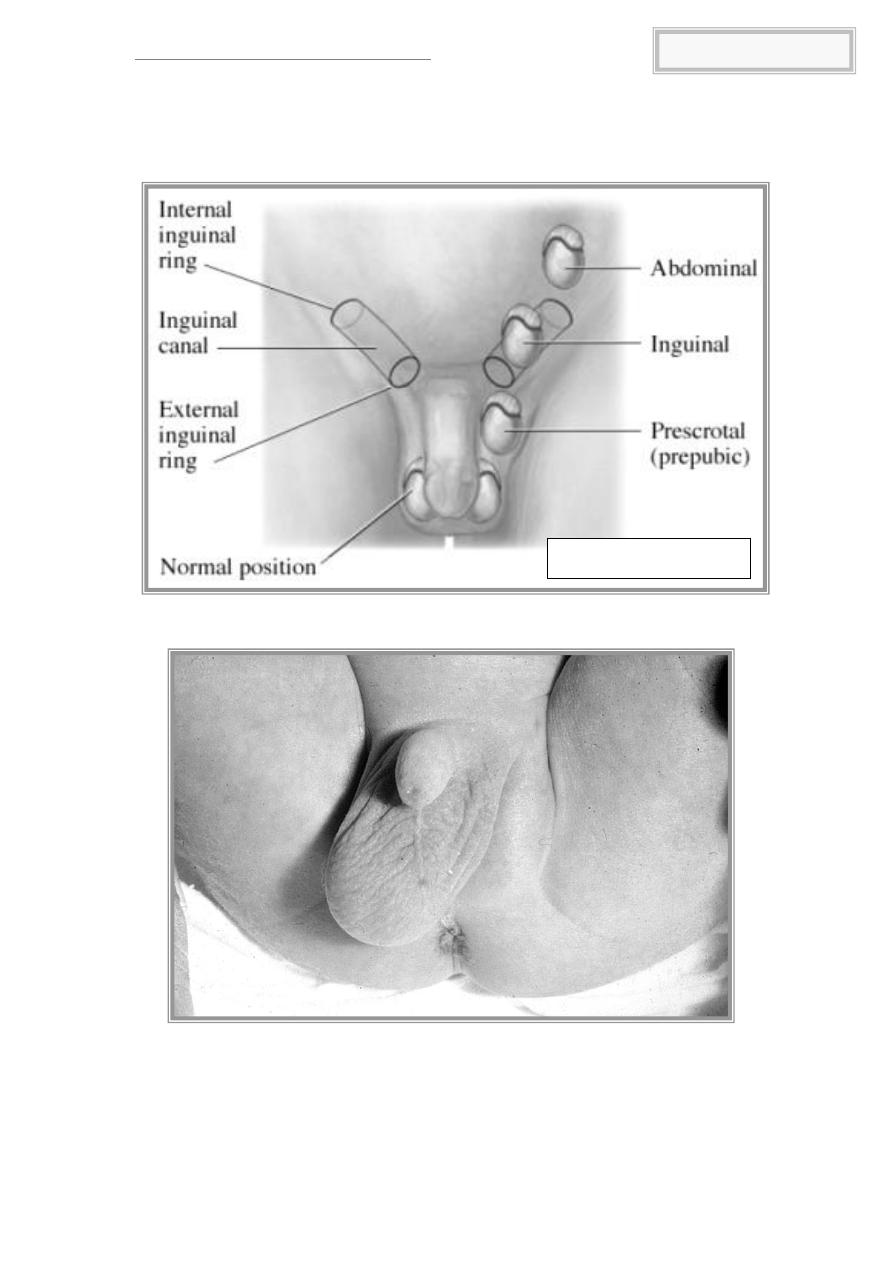
Undescended testes
The testes descend into the scrotum in the 3rd trimester (passing
through the inguinal canal at 24-28 weeks). Failure of testicular descent
results in cryptorchidism (or undescended testes).
Incidence
3% at birth (unilateral > bilateral). ~75% will spontaneously descend by
3 months. The incidence at 1 year is 1%.
Classification
testis may be intra-abdominal, intra-inguinal, or pre-scrotal.
Risk factors
Pre-term infants; low birth weight; small for gestational age; twins.
Aetiology
Abnormal testis or gubernaculum (tissue which guides the testis into
the scrotum during development); endocrine abnormalities (low level of
androgens, human chorionic gonadotrophin (HCG), luteinizing hormone
(LH)); decreased intra-abdominal pressure (prune-belly syndrome).
Pathology
Degeneration of Sertoli cells; loss of Leydig cells; atrophy and abnormal
spermatogenesis.
Long-term complications
Relative risk of cancer is 40-fold higher in the undescended testis.
Majority are seminomas; carcinoma in situ represents a small
percentage (~2%). There is a slightly increased risk of cancer in the
contralateral, normally descended testis.
Reduced fertility.
Increased risk of testicular torsion.
Increased risk of direct inguinal hernias (due to a patent processus
vaginalis).
Management
Full examination to elucidate if testis is palpable and to identify
location. Assess for associated congenital defects. If neither testis is palpable,
consider chromosome analysis (to exclude an androgenized female), and
hormone testing (high LH and FSH with a low testosterone indicates
anorchia).
Treatment should be performed within the first year. Hormone therapy
(HCG, LHRH) stimulates testosterone production. Surgery consists of
inguinal exploration, mobilization of spermatic cord, ligation of processus
vaginalis, and securing the testis into a dartos pouch in the scrotal wall
(orchidopexy). Laparoscopy can be used in planning surgery and for
treatment. Intra-abdominal testes may require division of spermatic vessels to
provide extra length (relying on collateral blood flow from vas), 2-stage
procedures, or microvascular autotransplantation.
Tikrit Medical College, Urology, Fifth year
7
.أ
د
.
دمحم محسن عبد العزيز
Undescended testes
