Pulmonary Edema
Clinical & Radiological
Rapid Review
Chest Series
Tikrit University
College of Medicine
Department of Radiology
Cardiogenic
left heart failure
mitral regurgitation
Non Cardiogenic
(mnemonic: NOTCARDIAC)
•
N: near drowning
•
O: O
2
therapy/post intubation pulmonary oedema
•
T: trauma/transfusion (TRALI: transfusion-related acute lung injury)
•
C: CNS: neurogenic pulmonary oedema
•
A: allergic alveolitis
•
R: renal failure
•
D: drugs
•
I: inhaled (toxins)
•
A: altitude: high altitude pulmonary oedema (HAPE), ARDS
•
C: contusion
Cardiogenic
Pulmonary Edema
Fluid backs up into the veins of the lungs.
Increased pressure in these veins forces
fluid out of the vein and into the air spaces
(alveoli). This interferes with the exchange
of oxygen and carbon dioxide in the
alveoli.
Extreme shortness of breath (severe difficult breathing)
Feeling of "air hunger"
"Grunting" sounds with breathing
Inability to lie down
Wheezing
Anxiety
Cough
Excessive sweating
Pale skin
Nasal flaring
Coughing up blood
Listening to the chest with a stethoscope
(auscultation) may show crackles in the
lungs or abnormal heart sounds.
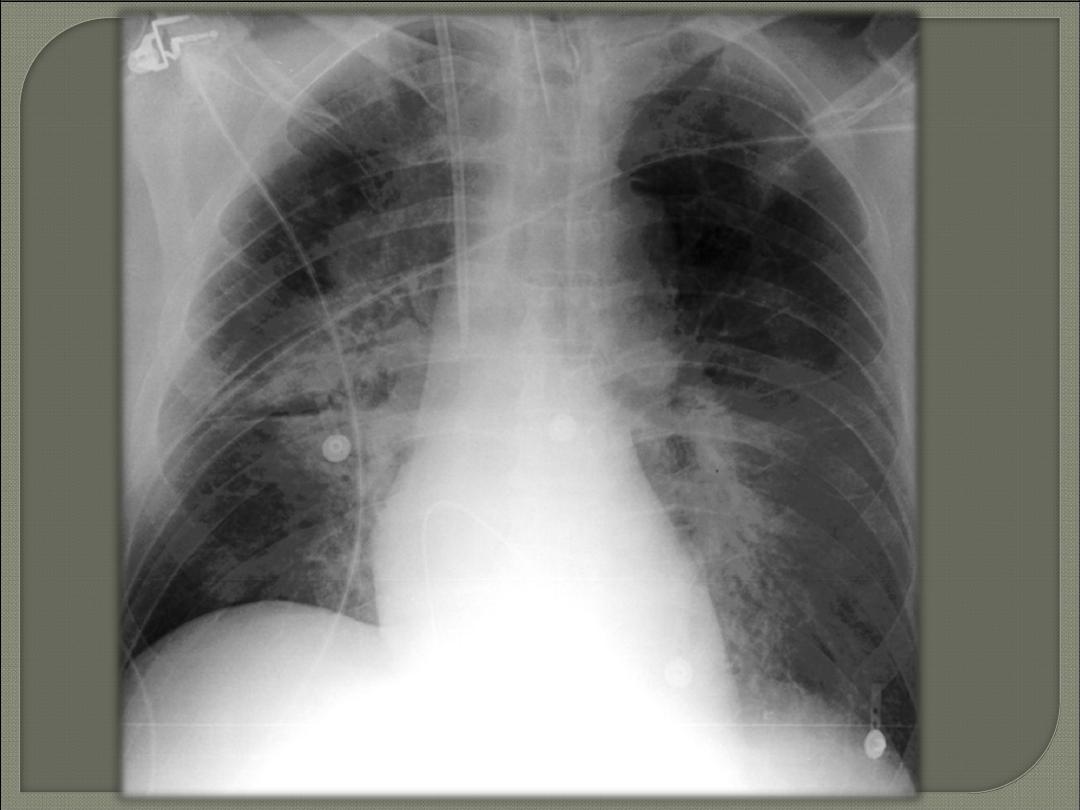
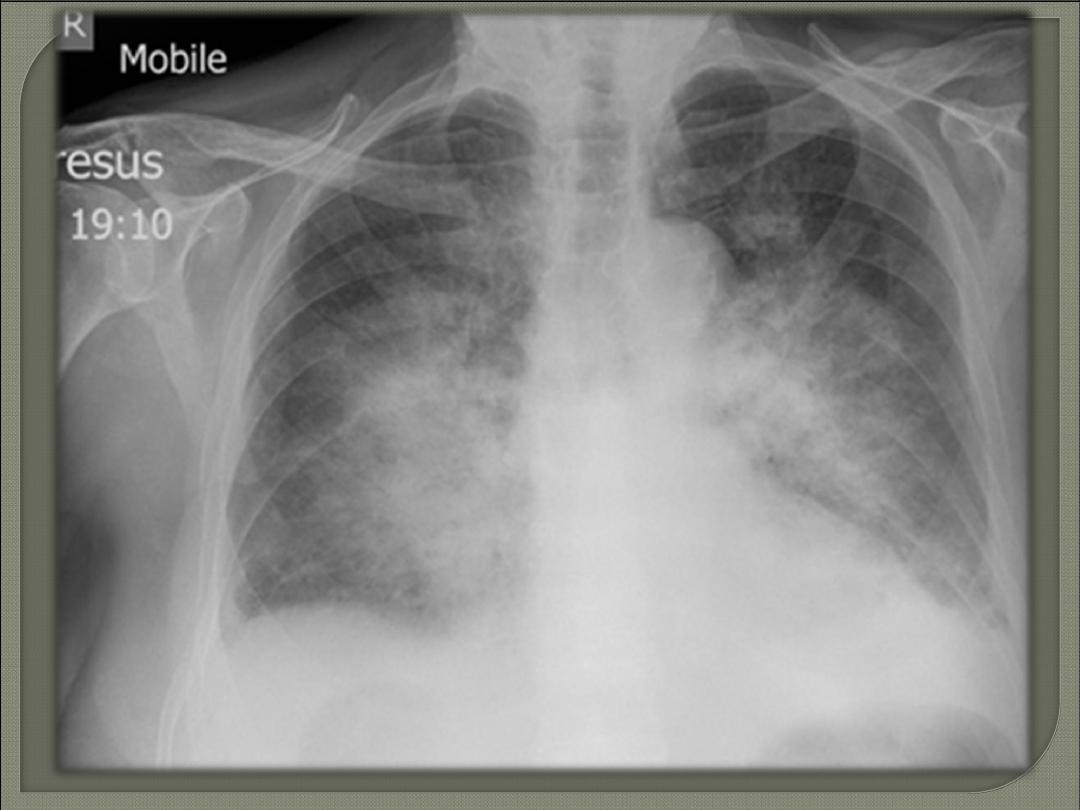
A
chest x-ray
may show fluid in the lung
space.
An echocardiogram may be performed in
addition to (or instead of) a chest x-ray.
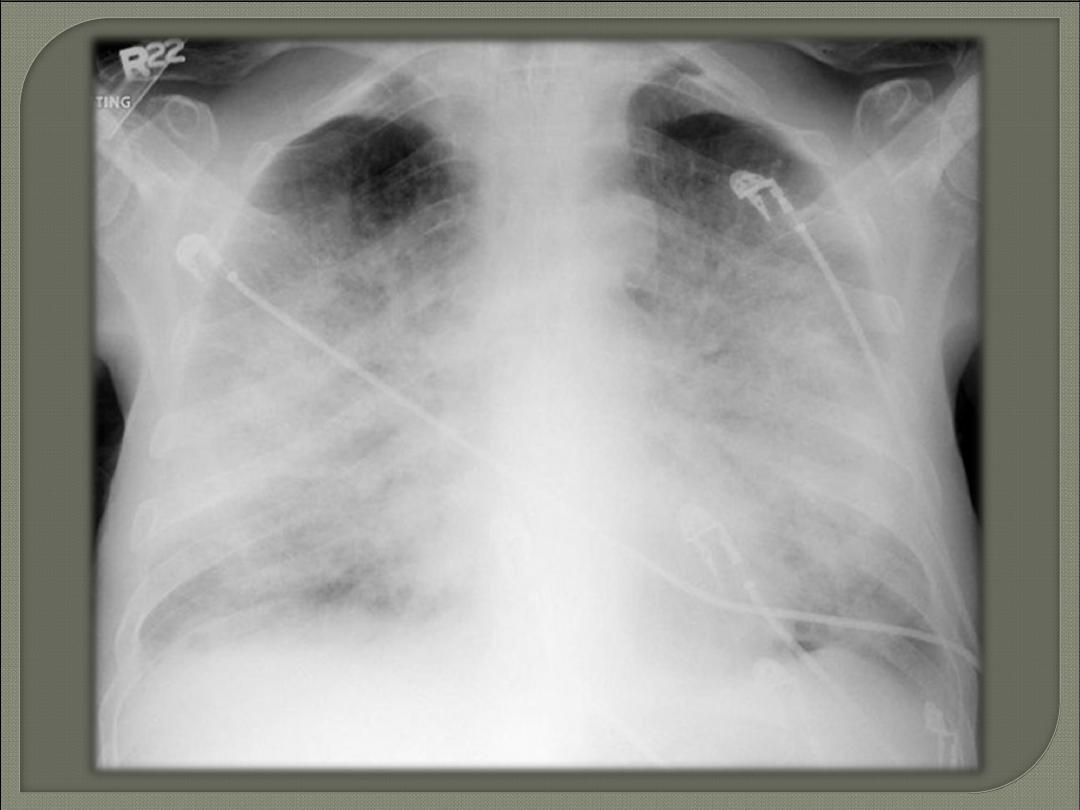
Plain film: chest radiograph
The chest radiograph still remains the
most practical and useful method of
radiologically assessing and quantifying
pulmonary edema.
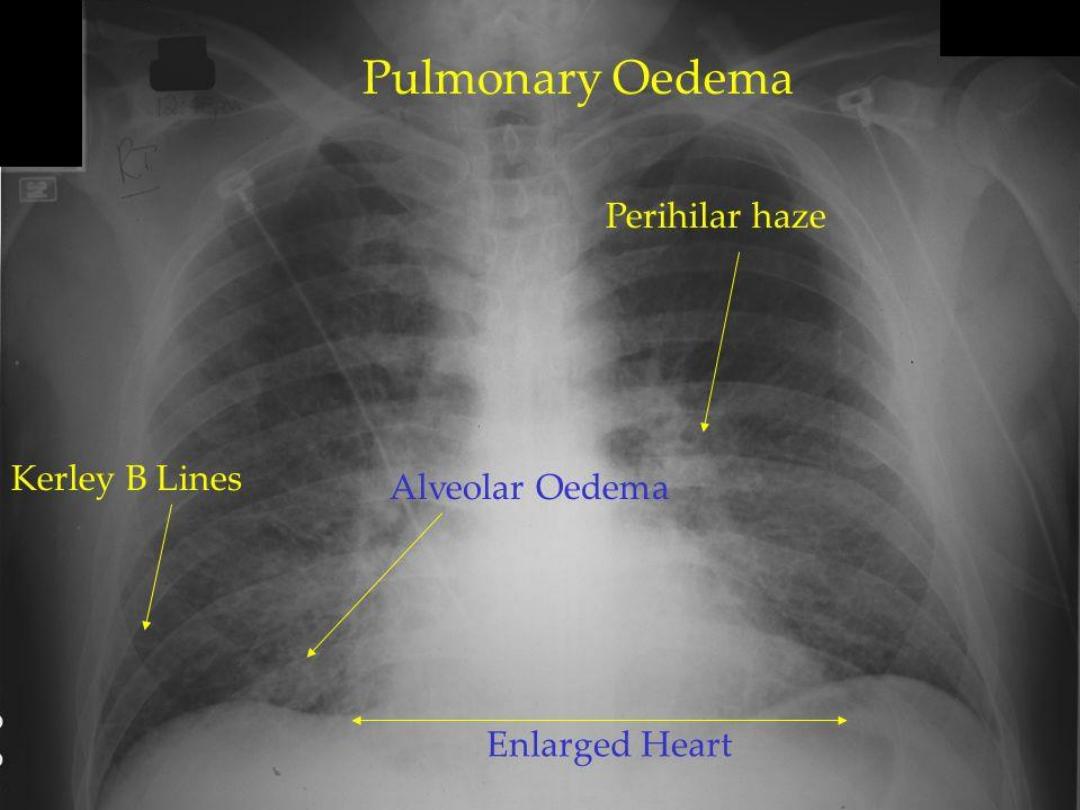
Radiological Features of pulmonary oedema
on a plain radiograph include:
1. Cardiac size enlarged / ⇧Cardio-thoracic ratio
2. Bat wing pulmonary opacities
3. Peri-bronchial cuffing
4. Septal lines: Kerley lines
5. Pleural effusions
6. Pulmonary venous engorgement/pulmonary
blood flow distribution/upper lobe pulmonary
venous diversion
Some of these features can vary dependent on the cause &
severity.
Septal lines, also known as Kerley lines,
are seen when the interlobular septa in the
pulmonary interstitium become
prominent.
This may be because of
lymphatic
engorgement or
oedema
of the connective
tissues of the interlobular septa.
They usually occur when pulmonary
capillary wedge pressures reach 20-25
mmHg.
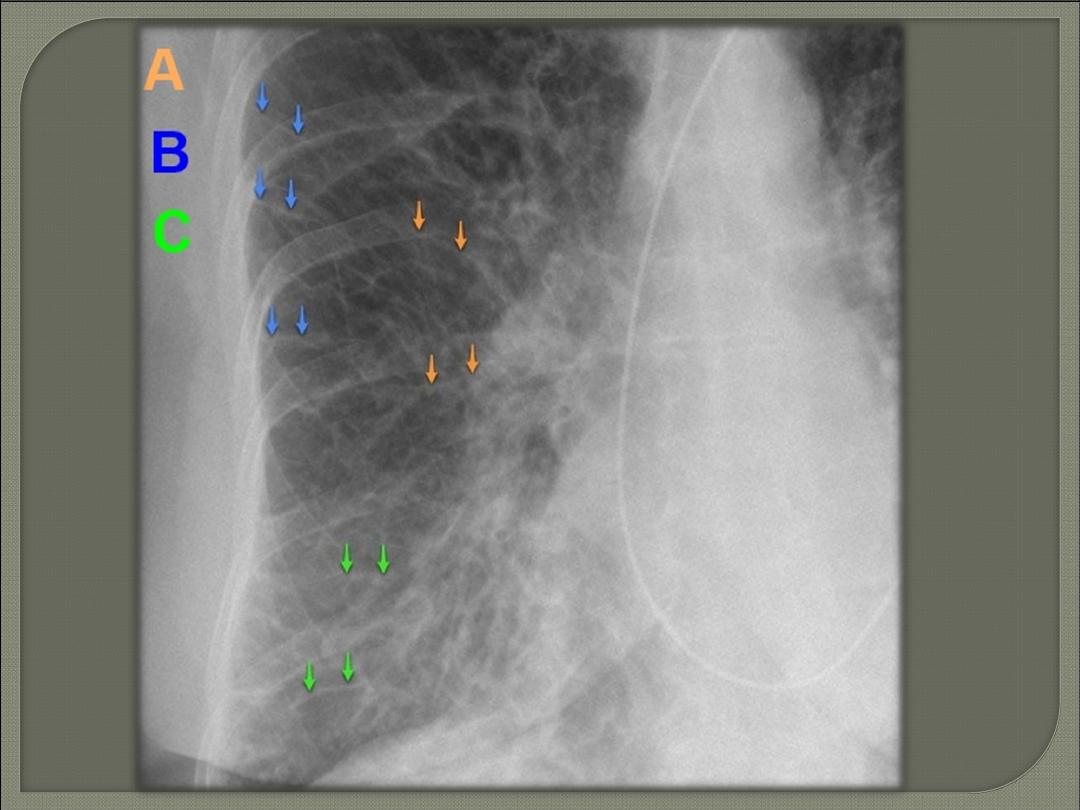
Kerley A lines
These are 2-6 cm long oblique lines that are <1 mm thick and
course towards the hila.
On chest radiographs they are seen to cross normal vascular
markings and extend radially from the hilum to the upper
lobes.
HRCT is the best modality for demonstration of Kerley A lines.
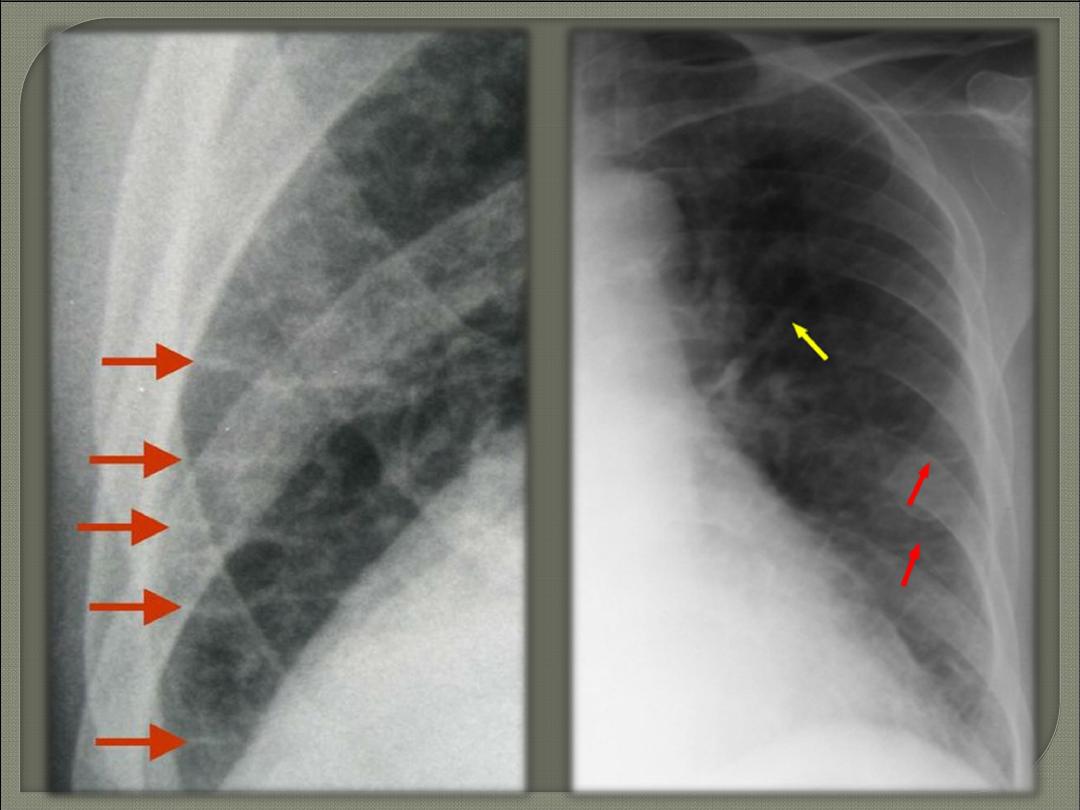
Kerley B lines
These are 1-2 cm thin lines in the peripheries of the lung.
Usually seen at the lung bases.
They are
perpendicular
on pleural surface.
Kerley C lines
Kerley C lines are short lines which:
do not reach the pleura (i.e. not B or D lines)
do not course radially away from the hila (i.e. not A lines).