
Dermatology
Skin
Anatomy:
It weighs about 4.5 kgs.
It's surface area is 2 m
2
.
Skin is composed of epidermis and dermis.
The line separating between the 2 layers of the skin is called the dermo-epidermal junction.
Epidermis
The basal cell layer (stratum basale) comes from the DEJ. These cells grow upward and form
another layer called and then another layer (Granulosum and Malpegian) above it and then
the last layer, the stratified squamous cell layer (keratinocyte)the cells in BCL divide and
undergo differentiation and form keratohyaline granules and then begin to lose organelles,
leading to the formation of dead cells containing keratin only Then this keratin undergoes
shedding. This process is programmed and it takes about 28 days (from the BCL to the
shedding phase). Normally the shedding of keratin is insensible, if it is sensible, disease is
suspected.
With each 10 keratinocytes, there is an umbrella-like cellMelanocyteIt is the cells
responsible for pigmentation (melanin production). The number of melanocytes is the same
in all individuals. It is present in hair, skin, eye (retina), substantia nigra, etc.
Melanocytes produce melaninit's (melanin) function is to protect the skin and the
underlying structures from the sun (UV light) by reflecting or absorbing the UV light (type
B& C) within the cell itself preventing it from passing towards the underlying structures.
UV lightType A
Type B
Type C (Doesn’t pass through the Ozone layer)It is carcinogenic.
Dermis
It contains:
1) Vasculature.
2) Fibroblastsproducing fibers (elastic & collagen)Function: recoiling of skin. With
aging, UV light damages the fibroblasts and fibersElastic and collagen fibers decrease
in the skin aging process (wrinkles).
3) Sebaceous glandsproducing sebum.
4) Sweat glandsApocrine sweat glands are located mostly in the axilla and groin.
5) Hair follicles and arrector pili muscles. (hair is composed of keratin)
6) Nerve endings.
7)

Nail
It consists of:
1) Nail plate is composed of keratin.
2) Cuticle: The white area of the nail that is regarded as the nail matrix.
3) Nail folds.
4) Nail bed.
Function:
1. Protection.
2. Thermal regulation.
3. Appearance (organ of beauty).
4. Vitamin D synthesis.
5. Indicator of disease. (mirror of internal organs).
6. Immunity, etc.
Language Of Dermatology
In Dermatology, we do physical examination and then take history (ask questions related the
findings of the physical examination).
Erythema Redness.
MaculeAlteration in the skin's texture or color <0.5 cm.
Patch Alteration in the skin's texture or color >0.5 cm.
Papule Elevation in the skin <0.5 cm.
Pluque Elevation in the skin >0.5 cm.
Vesicle Papule containing clear fluid.
Pustule Papule containing turbid fluid.
Bullae Enlarged vesicle. If contains blood Haemorrhagic bullae.
Fissure Loss of continuity of the skin.
Crust Dry exudate.
Scale ???? (Like the shedding of the keratin).

Acne
Types
Acne vulgaris.
Rosacia.
Acne vulgaris
Definition:
It’s a self-limiting disease affecting the young age (from
puberty to 30 years),
occurring in the seborreic areas (face, chest, shoulder, upper back, gluteal region).
Etiology:
1) Genetic predisposition.
2) Environmental factors.
3) There 3 theories:
a. Internists noticed that the disease occurs in the young age (during puberty), there is
an increase in the levels of sex hormones (androgen)act on the sebaceous
glandsIncrease sebum secretion.
b. Microbiologists have noticed the presence of a pustule in the lesionprobyno
bacterium acnis which is a normal florathey noticed that this NF numbers are
increased in the lesion.
c. Pathologists have noticed that there is a narrowing in the opening of the sebaceous
glands in the lesionsebum exits with difficultyhyperkeratosis of the pilo-
sebaceous orifice.
Clinical features & Complications:
Hyper secretion of sebum (seborrhea) + hyperkeratization blocking the pilo-sebaceous
orifice
Sebum contains cholesterol, FFA, etc
when this sebum accumulates in this
site (there is no way out, because the pilo-sebaceous duct is blocked)Papule will be
formed (due to the accumulation of sebum). This papule is called comedon (black or
white. If the accumulation of sebum is deep
white head {comedon}, but if it is
superficial
black head)
with further accumulation of sebum
it will rupture releasing
the contents inside the skin including FFA which will cause irritation and will provoke
an inflammatory reaction
ErythemapapulepustulecystScar
1) Erythema.
2) Papule (comedon).
3) Pustule.
4) Cyst.
5) Scarpitting scar (in acne), atrophic, hypertrophic, keloid.
6) PigmentationHyper or hypo.
7) Depression (mental scar).

Types
:
1) Acne vulgaris
2) Neonatal acneAndrogen H. from the mother through the placentastimulating the
sebaceous glands of the neonateAcne. (sebum acts in the 1
st
year of life due the maternal
androgen)
3) Childhood acneEarly puberty.
4) Acne medicamentosa Due to certain drugs (like steroids, CCP).
5) Post depilation acne Due to mechanical removal of the hair (sugar solution, waxing,
etc).
6) Oil acneOccur in car mechanicsoil causes obstruction of the pilo-sebaceous orifices.
7) Rosacea
Treatment:
1) Includes topical & systemic.
2) Antibiotics 1
st
line of treatment.
3) Increased androgen levelAnti-androgen (like cemitidine, spirolactone, fenisteride, etc).
4) Heperkeratosiskeratolytic (salicylic acid, retinoid, etc).
5) Scar: PittingFiller.
Hypertrophickeratolytic.
Keloidresection & application of steroid (to prevent re-formation of keloid).
Hypopigmentationgive drugs that increase the pigmentation.
Hyperpigmentationgive drugs that decrease the pigmentation.
Psoriasis
Definition:
It is a chronic disease, occurring in old age, occurring in both genders, remission and
relapse and it is regarded as an autoimmune disease.
Etiology:
1) Genetic factors.
2) Environmental factorsstress, D.M, infection, drugs (like beta blockers, gold, lithium),
sunlight, etc.
Clinical features:
1) Thickening of skin.
2) Fissuring.
3) Scaling.
4) Papule & plaque.
5) VasodilationhyperemiaErythema.
6) Itching.

Types:
1) Localized or generalized (emergency condition).
2) Psoriasis capitis.
3) Frictural psoriasis.
4) Pustular psoriasis.
5) Palmer or planter psoriasis.
6) Psoriasis of the nail.
7) Gutet psoriasis. (caused by streptococcal infection)
8) Etc.
Treatment:
1) Thickening of skinkeratolytic agents (topical & systemic).
2) FissuringOintment (emollients).
3) ErythemaSteroids (topical & systemic).
4) InfectionAntibiotics.
5) ItchingAntihistamines.
6) Analgesia.
7) Cytotoxic drug (methotrexate).
8) Vit. A (acetritinenhance proliferation & differentiation)
When psoriasis is cured, it leads to post-inflamatory hypopigmentation, while lichen
planus leads to post-inflamatory hyperpigmentation.
Lichen planus
Types: Generalized or localized.
Same etiological factors.
Same mechanism but here only papule and plaque are formed (no thickening and
fissuring).
Both skin and mucous membranes are involved.
The lesion is violate (no erythema)
Pyteriasis rosea
It is an infection by Herpes virus type A
Pigmentary disorders
Each 10 keratinocytes, there is 1 melanocyte.
The number of melanocytes is fixed in all individuals.
FunctionMelanin productionresponsible for pigmentation, absorption and reflection of UV
light type A & B (to prevent its passage into underlying structures. If it passesDamage to
fibroblasts (producing elasticresponsible for elasticity and collagenActs as a
cushion)Aging process. If it reaches the BCL may cause damage and lead to tumor
formation).
Melanin is located in vesiclescalled melanosomes.
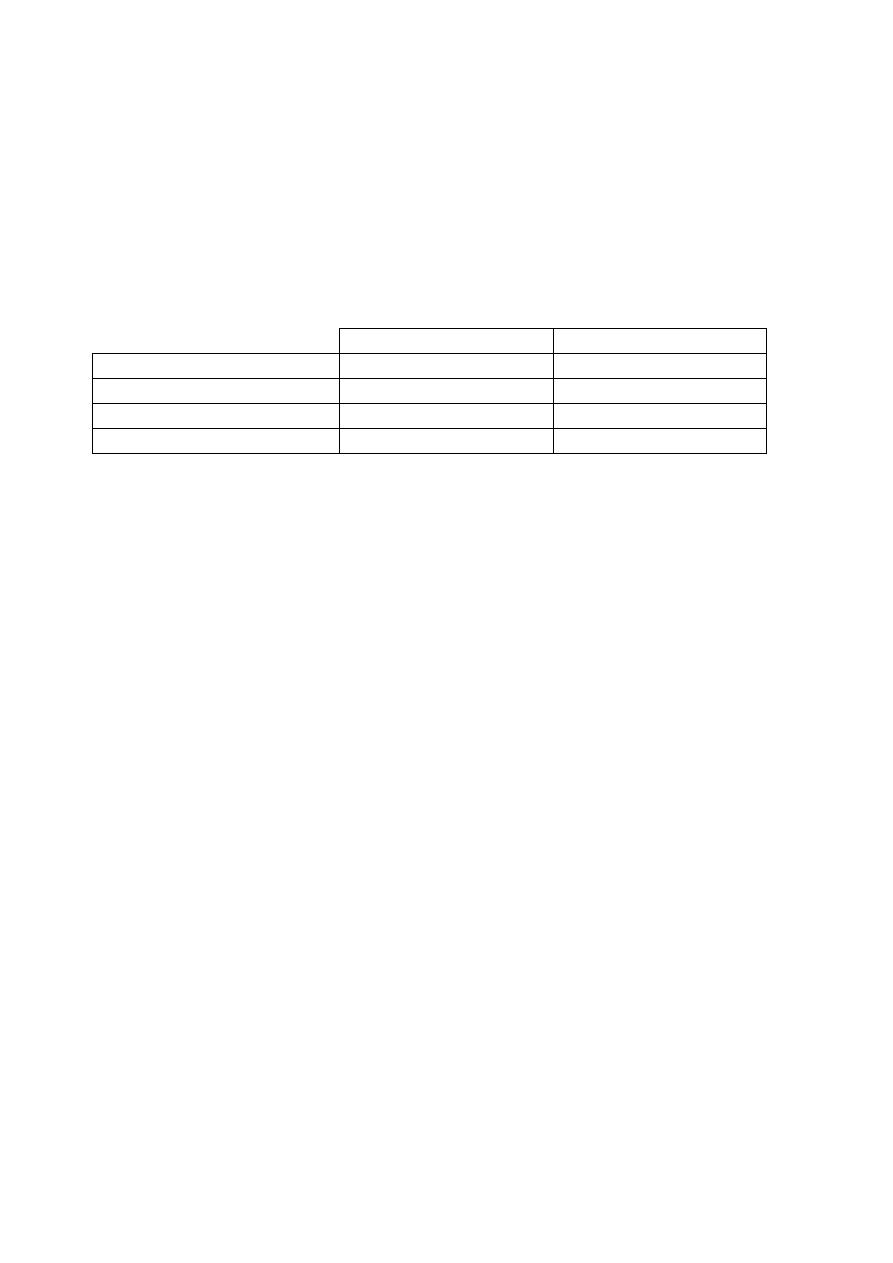
White
Black
Number of melanocytes
Same
Same
Number of melanosomes
Less
More
Size of melanosomes
Smaller
Larger
Oxidation of melanin
Less
More
Melanocytes are located in the skin, hair, retina, substantia nigra.
Melanocytes activity decreases with age.
Increased pigmentationHyperpigmentation.
Decreased pigmentation Hypopigmentation.
No pigmentationDepigmentation.
Hypopigmentation
Vitiligo
Definition:
It is an autoimmune disorder. Remission and relapse.
Etiology:
1. Genetic factors.
2. Environmental factors. (i.e. stressful condition, infection, etc these factors stimulate
antibodies against the melanocytes)
Clinical features:
1. Hypopigmentation or depigmentation.
2. Macule or patch.
3. Mostly occurs at sites of friction (fingers, elbows, knees, eyes, ano-genital area, etc).
Types:
1. Generalized or localized vitiligo.
2. Xosteriform vitiligo.
3. Halo naevus vitiligo.
4. Vitiligo of the hair.
Complications:
1. Depression.

2. Early aging process.
3. Burning.
4. Tanning.
5. Tumor.
Treatment:
1. Genetic counseling.
2. Immune modulationsteroids (topical & sysyemic), zinc sulphate, antioxidants.
3. Psoralen and UV light exposure.
4. Plastic surgery.
5. Camouflage (dye or henna). (can be detected by Wood's light, the lesions will look
ivory in color).
6. If a pt. with 80% of his body is white and only some spots are blackDepigmentation
(bleaching agent).
After being cured could lead to Post-inflammatory hypo-pigmentation.
Hyperpigmentation
Melasma
Definition:????
It is seen in the face.
Etiology:
1. Genetic factors.
2. Environmental factors: Occupational (sun exposure), pregnancy (melanocyte
stimulating hormone), CCP, Post-inflammatory hyperpigmentation, drugs
Types:
1. Localized or generalized.
2. Butterfly melasma.
Treatment:
1. Sun exposure sun screen.
2. CCP avoid it and use other type of contraception.
3. Bleaching agent (i.e. glutathione, etc). could be given topical, injection.
4. Laser.
5. Dermoabrasion.
6. Peeling.
7. Antioxidants, vitamins.
Complications:
1. Depression.
By: Muthana Harith
