1
Tikrit University/ College of Medicine
Community Medicine Department
د
.
ﺣ
ﯾ
د
ر
ﺳ
ﻌ
د
ا
ﻟ
ﻌ
ﯾﺑ
د
ي
Control of Diarrheal Diseases (CDD)
• Diarrhea is a condition in which stools are passed more frequently and/or looser than
usual per day. [Three or more loose stools in a day is considered diarrhea.]
• Children with diarrhea lose copious amounts of water and electrolytes, resulting in
dehydration.
• It's the most common between 6 months and 3 years of age, and also common under 6
months among bottle fed infants.
• Rotavirus account for >50% of cases.
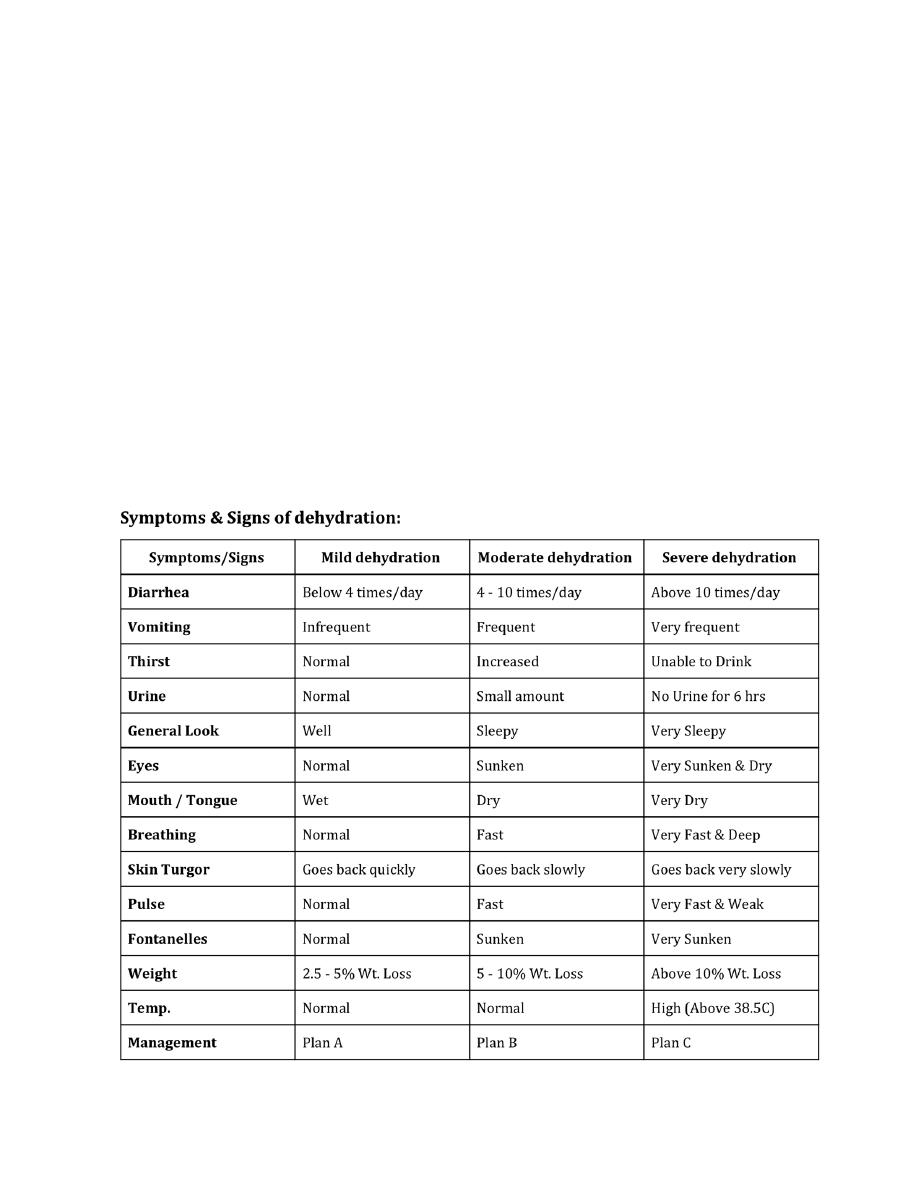
Assessment of dehydration

2
Treatment of dehydration
Plan A: aims to prevent dehydration
● Give extra fluids (e.g. ORS).
● Continue feeding.
● Teach the mother:
o How to prepare & give ORT.
o How to detect dehydration and what to do then.
Plan B: aims to correct dehydration
● Give ORS in the PHC Center. [Wight (Kg) x 75mL = Volume given over 4 hours]; Assess the
condition every hour.
● Continue Breastfeeding.
● Teach the mother:
o How to prepare & give ORT.
o How to detect dehydration and what to do then.
o If the child vomits the ORT, wait for 10 min and restart giving the solution slowly.
●Reassess the condition:
o If dehydration is decreasing; go back to Plan A.
o If dehydration is the same; continue Plan B.
o If dehydration is increasing; go to Plan C.
Plan C: aims to correct dehydration urgently.
● Give Rehydration Therapy through IV or NG tube in the hospital.
● Give ringer's lactate solution if not available use normal saline: [Weight (Kg) x 100 mL over a
period of]:
o Age less than one year: 30 mL/Kg/hour then continue 70 mL/Kg/for 5-6 hours.
o More than one year: 30 mL/Kg/30 minutes then continue 70 mL/Kg over 2.5 to 3 hours.
● Reassess the condition every hour.
3
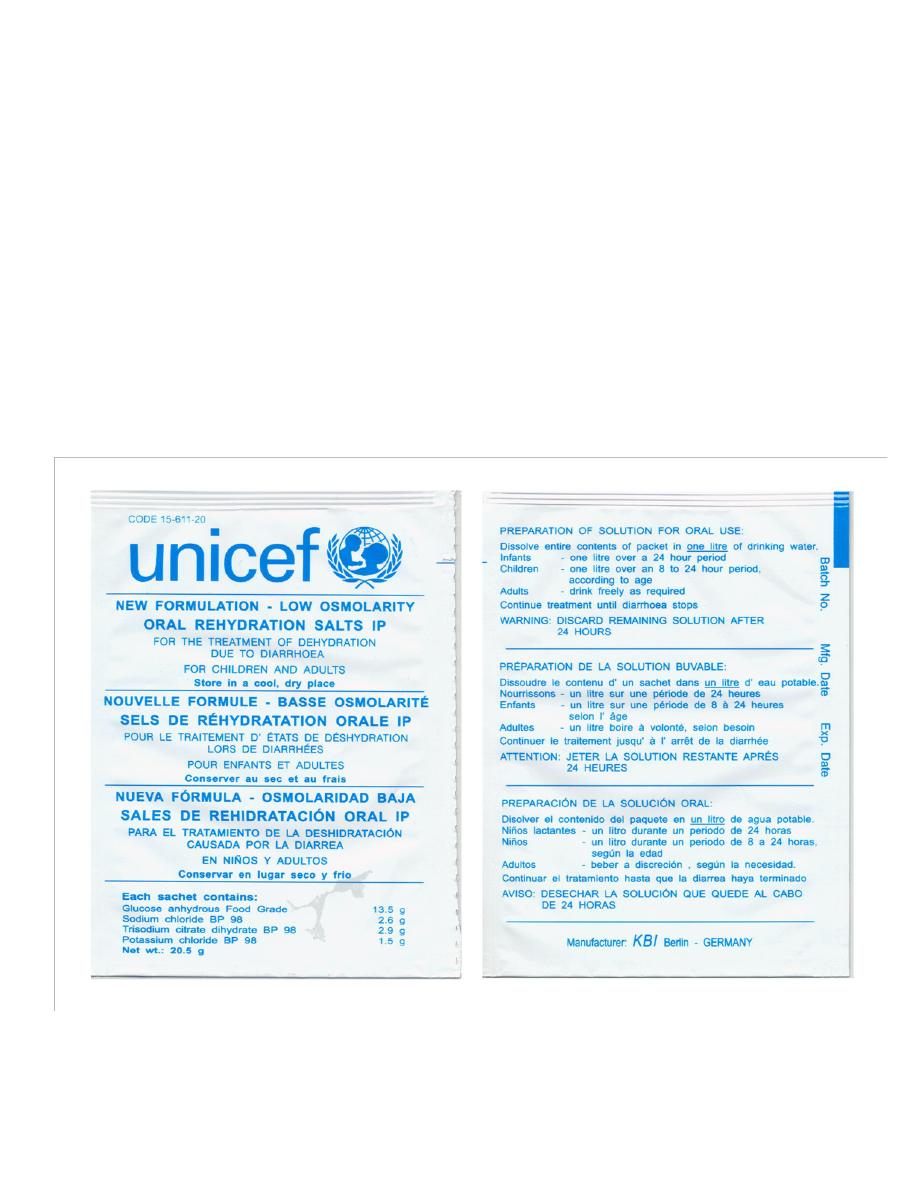
Oral Rehydration Solution (ORS)
• ORS is balanced glucose-electrolyte mixture, first used in 1969 and approved,
recommended, and distributed by UNICEF and WHO as a drug for the treatment of
clinical dehydration throughout the world.
• ORS use has been associated with dramatic global reduction in mortality from diarrheal
disease by 93%.
Composition and MOA
• Glucose: facilitates the absorption of
sodium (and hence water) on a 1:1
molar basis in the small intestine.
• Sodium and potassium: to replace the
body losses of these essential ions
during diarrhea (and vomiting).
• Citrate: corrects the acidosis that
occurs as a result of diarrhea and
dehydration.
Indications
• ORS is used to prevent or treat dehydration from diarrhea irrespective of the cause or
age group affected.
Contraindications
• Excessive vomiting
• Ileus
• Worsening of dehydration despite using ORS
• Patient with shock
Preparation and administration
• Dissolve one sachet of ORS in one liter of clean water. It should not be used for >24 hr.
• Newborn may be given ORS with a dropper or a syringe. Infants under two may be given
a teaspoon of ORS fluid every one to two minutes. Older children and adults should take
frequent sips from a cup.
4
Types of ORS
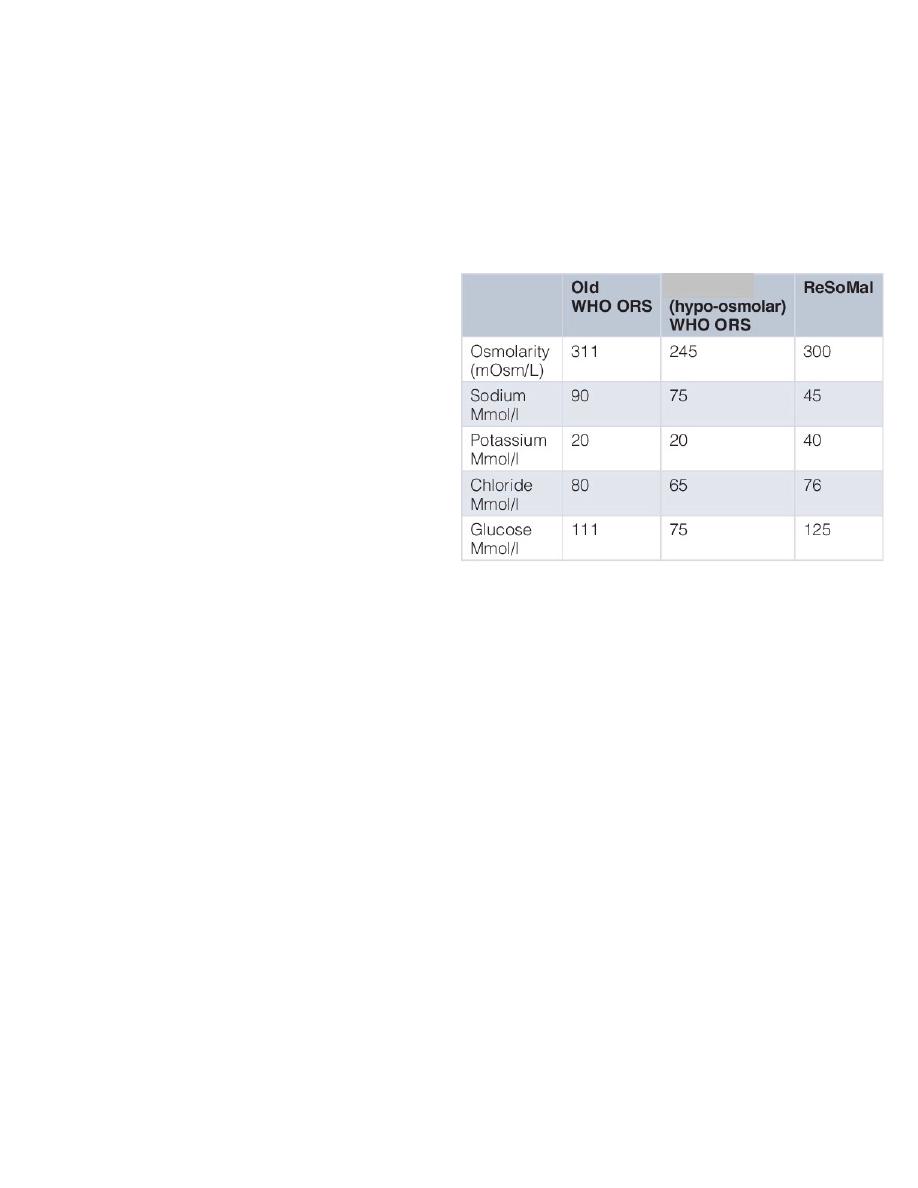
1. Reduced osmolarity ORS
• Recommended currently by WHO/UNICEF
Advantages or reduced osmolarity ORS
• As effective as standard ORS
• 33% reduced need for IV rehydration
• 25% Reduce stool output
• Reduce vomiting
2. Standard ORS
• 90 mmol/l sodium and 90 mmol/l glucose, total osmolarity 311 mmol/l).
• Previous version of ORS recommended by WHO before 2003.

5
3. ReSoMal (Rehydration Solution for
Malnutrition)
• The original ORS (90 mmol sodium/L) and
the current standard reduced-osmolarity
ORS (75 mmol sodium/L) both contain too
much sodium and too little potassium for
severely malnourished children with
dehydration due to diarrhea. ReSoMal is
recommended for such children. It contains
less sodium (45 mmol/l) and more
potassium (40 mmol/l) than reduced
osmolarity ORS.
• Children with severe acute malnutrition and
who have some or severe dehydration but
no shock should receive 5 mL/kg ReSoMal
every 30 min for the first 2 h. Then, if the
child is still dehydrated, 5–10 mL/kg/h
ReSoMal should be given in alternate hours,
up to a maximum of 10 h
• Children with severe acute malnutrition and signs of shock or severe dehydration and
who cannot be rehydrated orally or by nasogastric tube should be treated with
intravenous fluids.
4. Home prepared ORS
• A WHO publication for physicians recommends a homemade ORS consisting of one liter
water with one teaspoon salt (3 grams) and two tablespoons sugar (18 grams) added.
Additive therapies
As a part of oral rehydration therapy, the WHO recommends supplemental zinc (10 to 20 mg
daily) for ten to fourteen days, to reduce the severity and duration of the illness and make
recurrent illness in the following two to three months less likely. Preparations are available as a
zinc sulfate solution for adults, a modified solution for children and in tablet form.
