
Control of Diarrheal Disease
Dr. Hayder Saad Al Aubaidi
Definition of diarrhea
• Diarrhea is a condition in which stools are passed more frequently and/or
looser than usual per day. [Three or more loose stools in a day is considered
diarrhea.]
• Children with diarrhea lose copious amounts of water and electrolytes,
resulting in dehydration.
• It’s the most common between 6 months and 3 years of age, and also
common under 6 months among bottle fed infants.
• Rotavirus
account for >50% of cases.
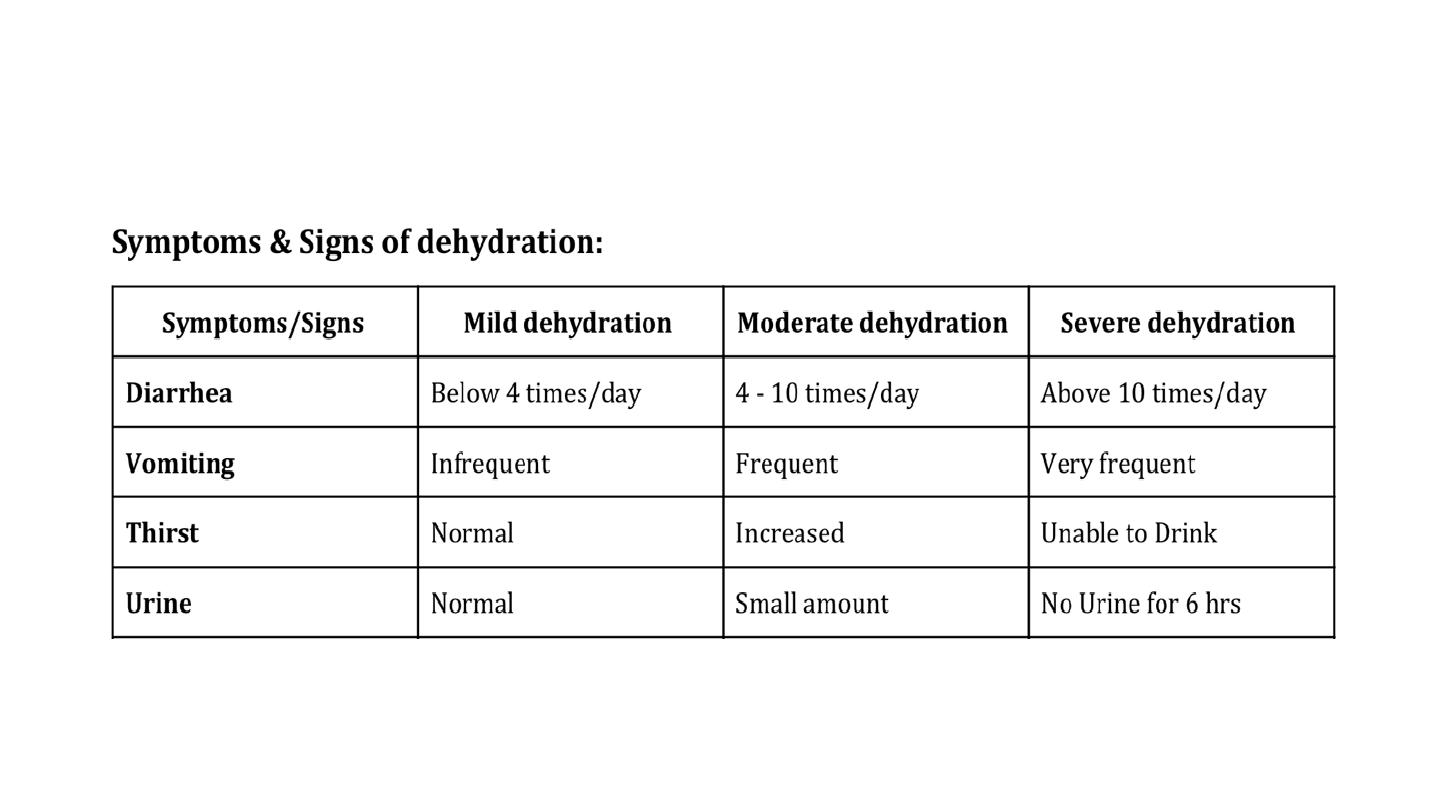
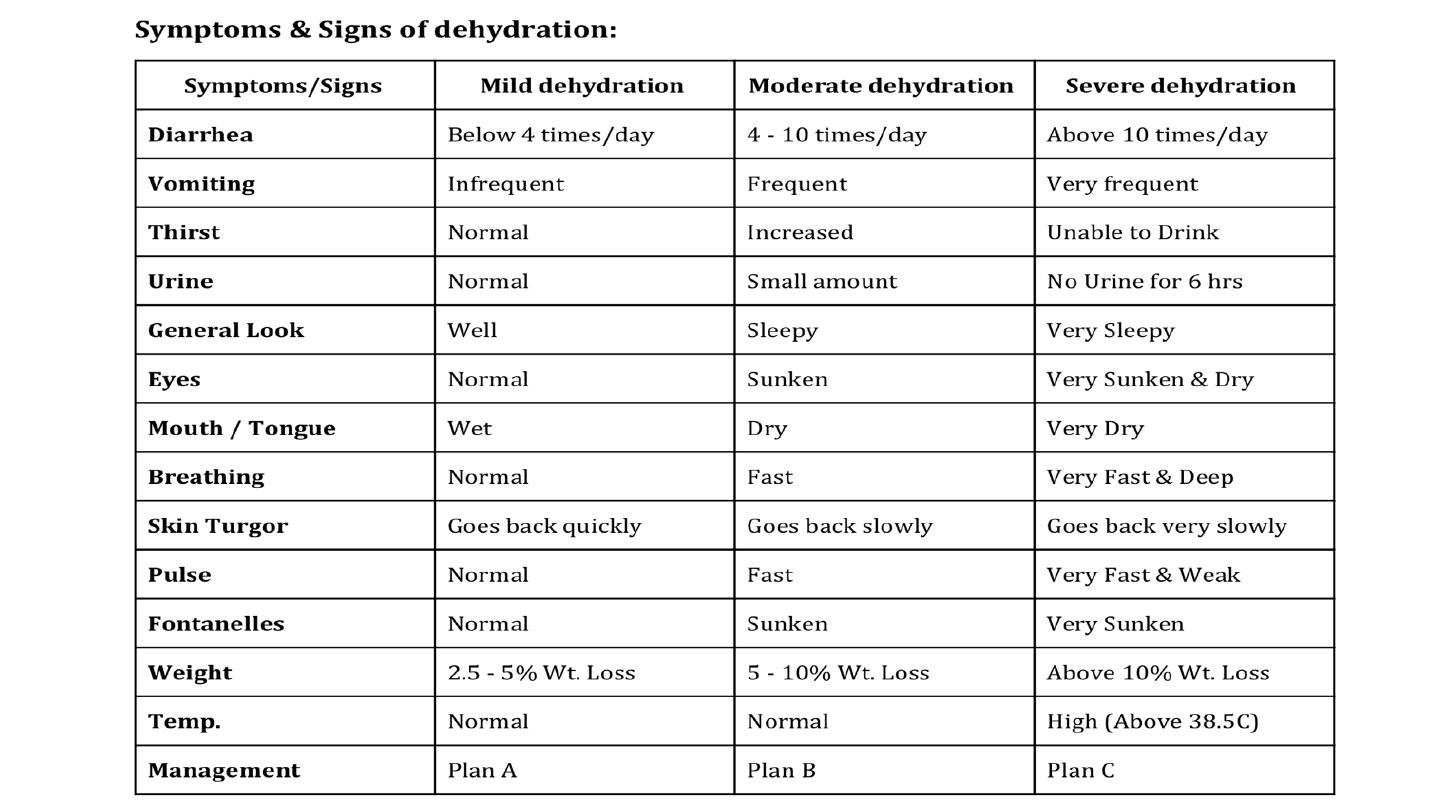
Assessment of dehydration
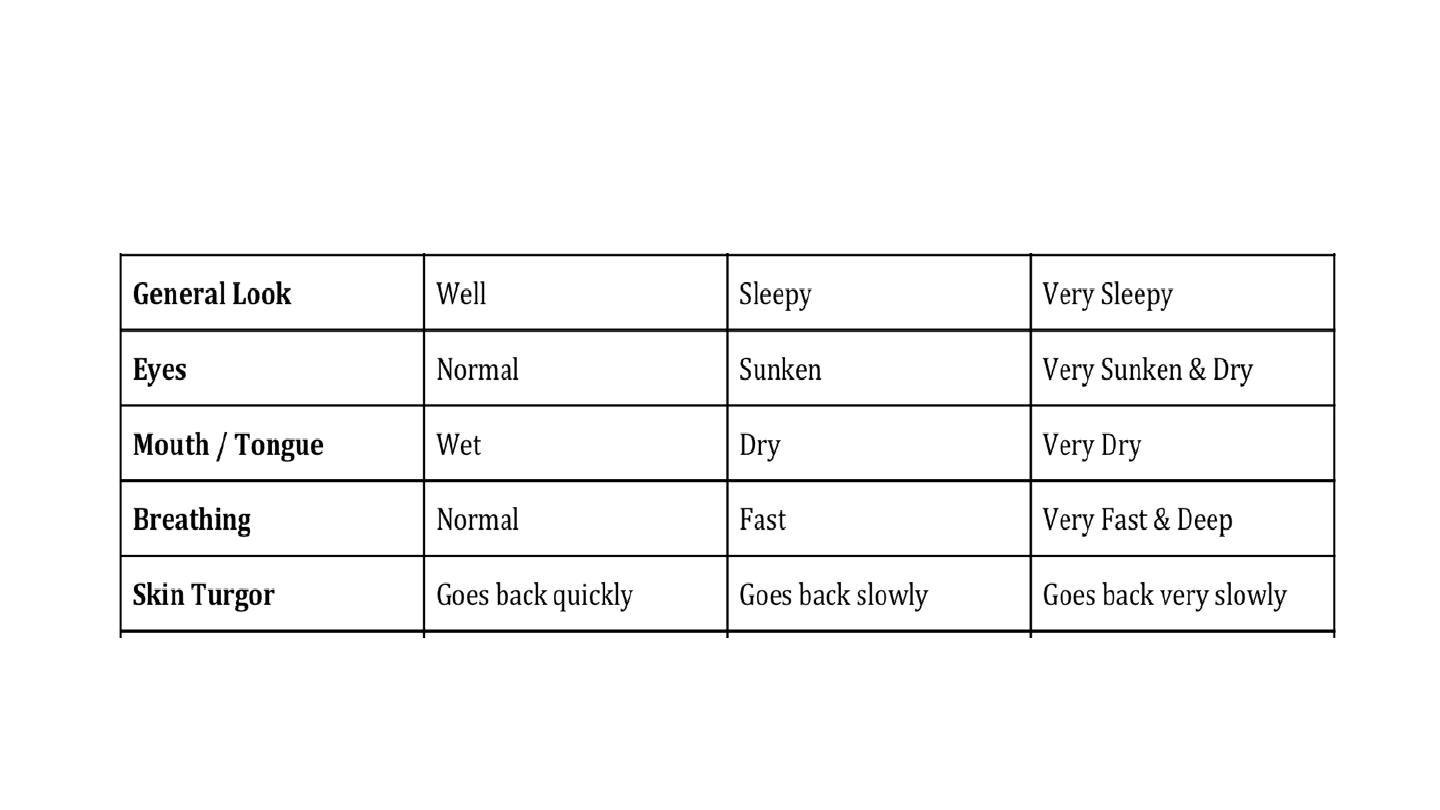
Assessment of dehydration
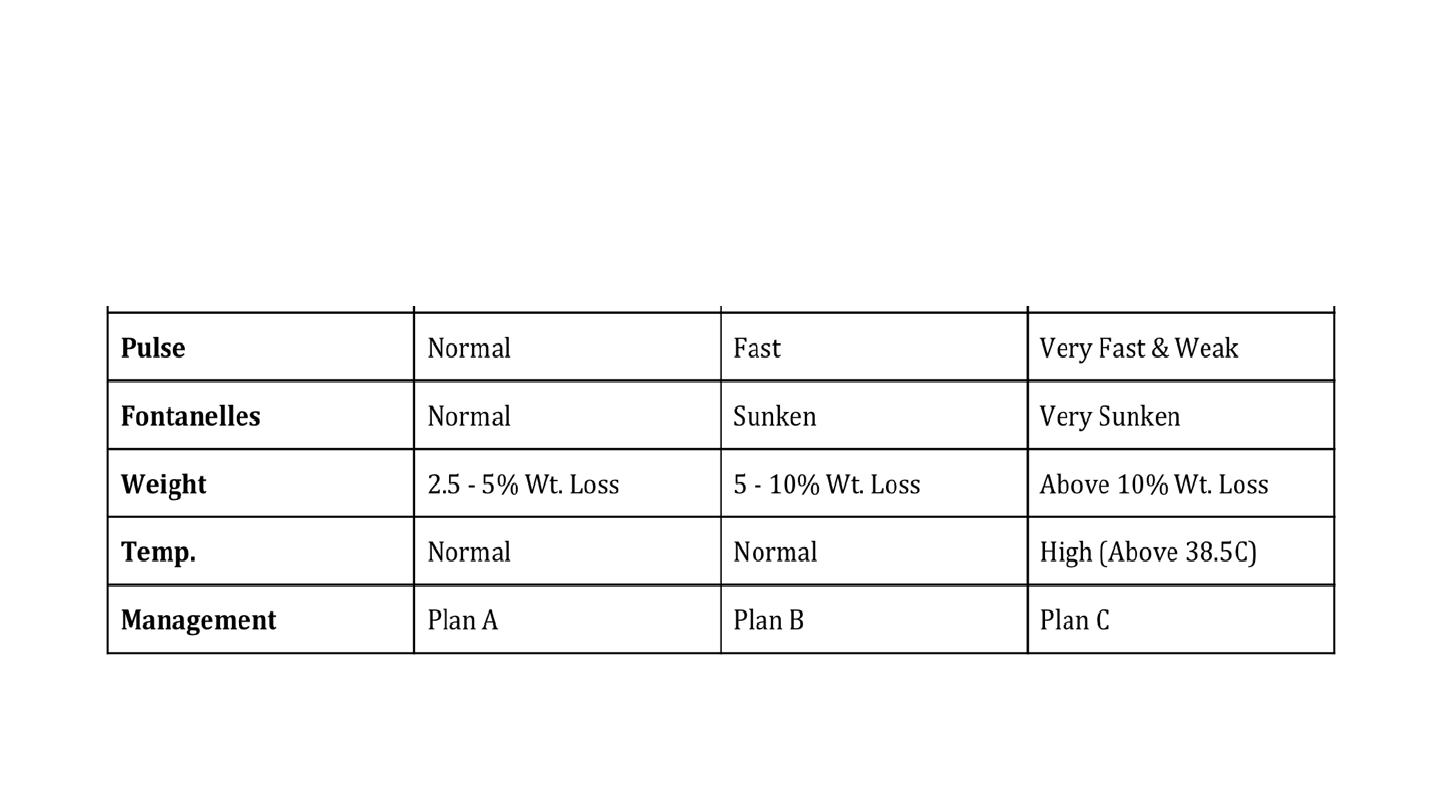
Assessment of dehydration

Treatment of dehydration
Plan A: aims to prevent dehydration
• Give extra fluids (e.g. ORS).
• Continue feeding.
Teach the mother:
➢How to prepare & give ORT.
➢How to detect dehydration and what to do then.

Plan B: aims to correct dehydration
• Give ORS
in the PHC Center
. [Wight (Kg) x
75mL
= Volume given over 4 hours]; Assess the
condition every hour.
• Continue Breastfeeding.
Teach the mother:
➢How to prepare & give ORT.
➢How to detect dehydration and what to do then.
➢If the child vomits the ORT, wait for 10 min and restart giving the solution slowly.
Reassess the condition:
• If dehydration is decreasing; go back to Plan A.
• If dehydration is the same; continue Plan B.
• If dehydration is increasing; go to Plan C
.
Plan C: aims to correct dehydration urgently.
• Give Rehydration Therapy through
IV or NG tube
in the
hospital
.
• Give
ringer's lactate
solution if not available use
normal saline
: [Weight (Kg) x
100 mL over a period of]:
➢Age less than one year: 30 mL/Kg/hour then continue 70 mL/Kg/for 5-6 hours.
➢More than one year: 30 mL/Kg/30 minutes then continue 70 mL/Kg over 2.5 to 3
hours.
• Reassess the condition every hour
.

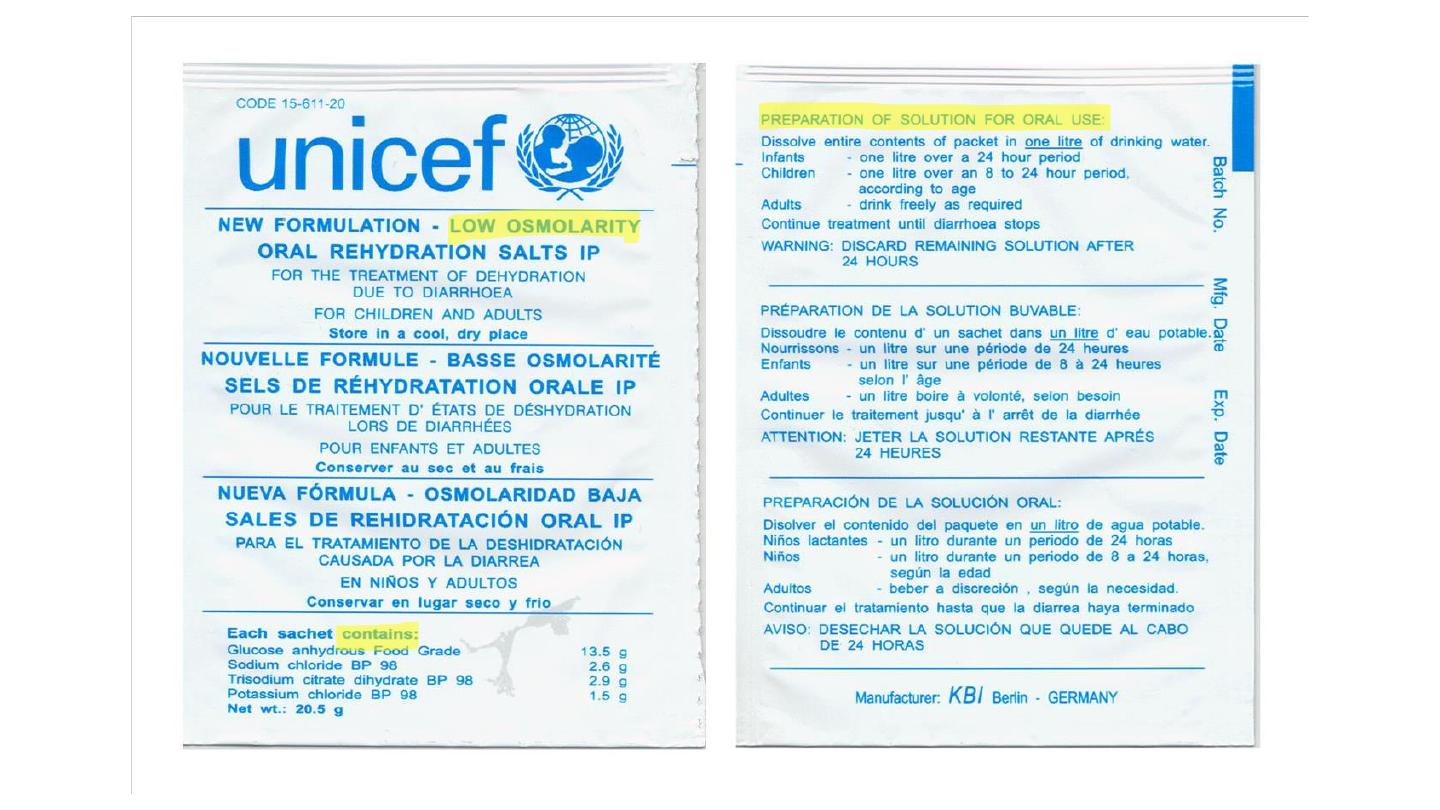
ORS
• ORS is balanced glucose-electrolyte mixture, first used in 1969 and approved,
recommended, and distributed by UNICEF and WHO as a
drug
for the treatment
of clinical dehydration throughout the world.
• ORS use has been associated with dramatic global reduction in mortality from
diarrheal disease by
93%.

Composition and MOA
Composition and MOA
• Glucose
: facilitates the absorption of sodium (and hence water) on a
1:1 molar basis in the small intestine.
• Sodium and potassium
: to replace the body losses of these essential
ions during diarrhea (and vomiting).
• Citrate
: corrects the acidosis that occurs as a result of diarrhea and
dehydration.
Indications and contraindications of ORS
Indications
• ORS is used to
prevent
or
treat
dehydration from diarrhea irrespective of the
cause or age group affected.
Contraindications
• Excessive vomiting
• Ileus
• Worsening of dehydration despite using ORS
• Patient with shock

Preparation and administration
• Dissolve one sachet of ORS in one liter of clean water. It should not be
used for >24 hr.
• Newborn may be given ORS with a dropper or a syringe. Infants under
two may be given a teaspoon of ORS fluid every one to two minutes.
Older children and adults should take frequent sips from a cup
.

Types of ORS
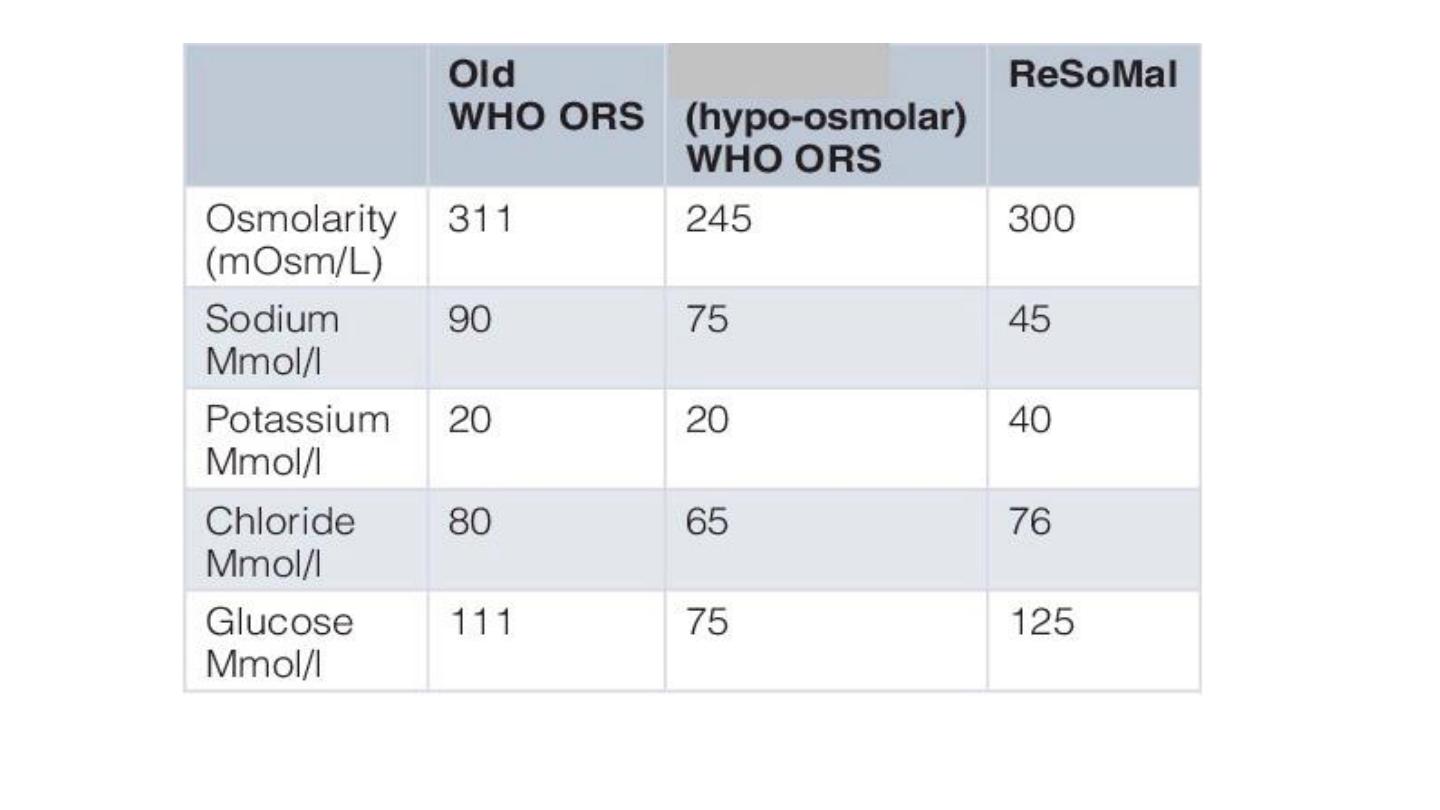
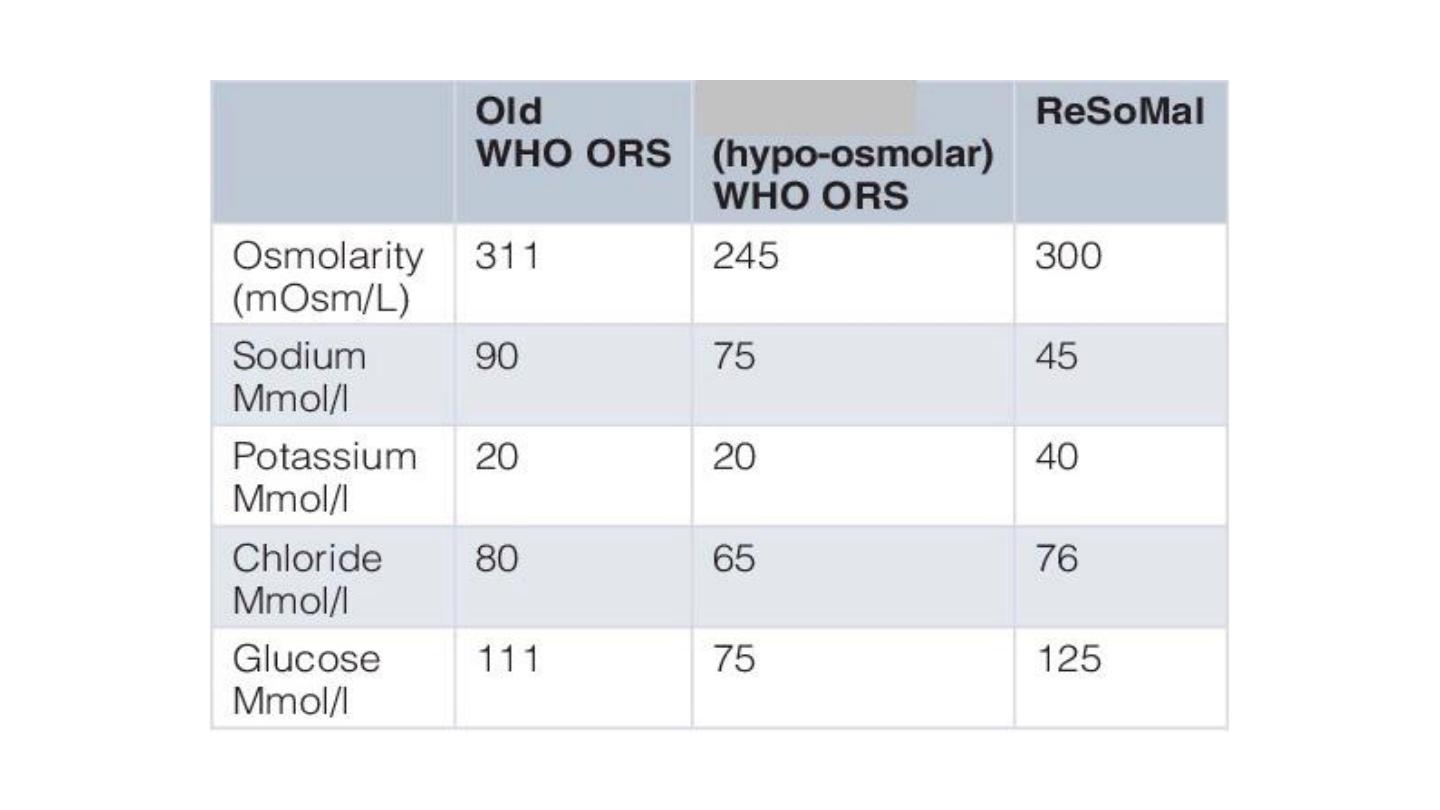
Reduced osmolarity ORS
• Recommended currently by WHO/UNICEF
Advantages or reduced osmolarity ORS
• As effective as standard ORS in rehydration
• 33%
reduced need for IV rehydration
• 25%
Reduce stool output
• Reduce vomiting
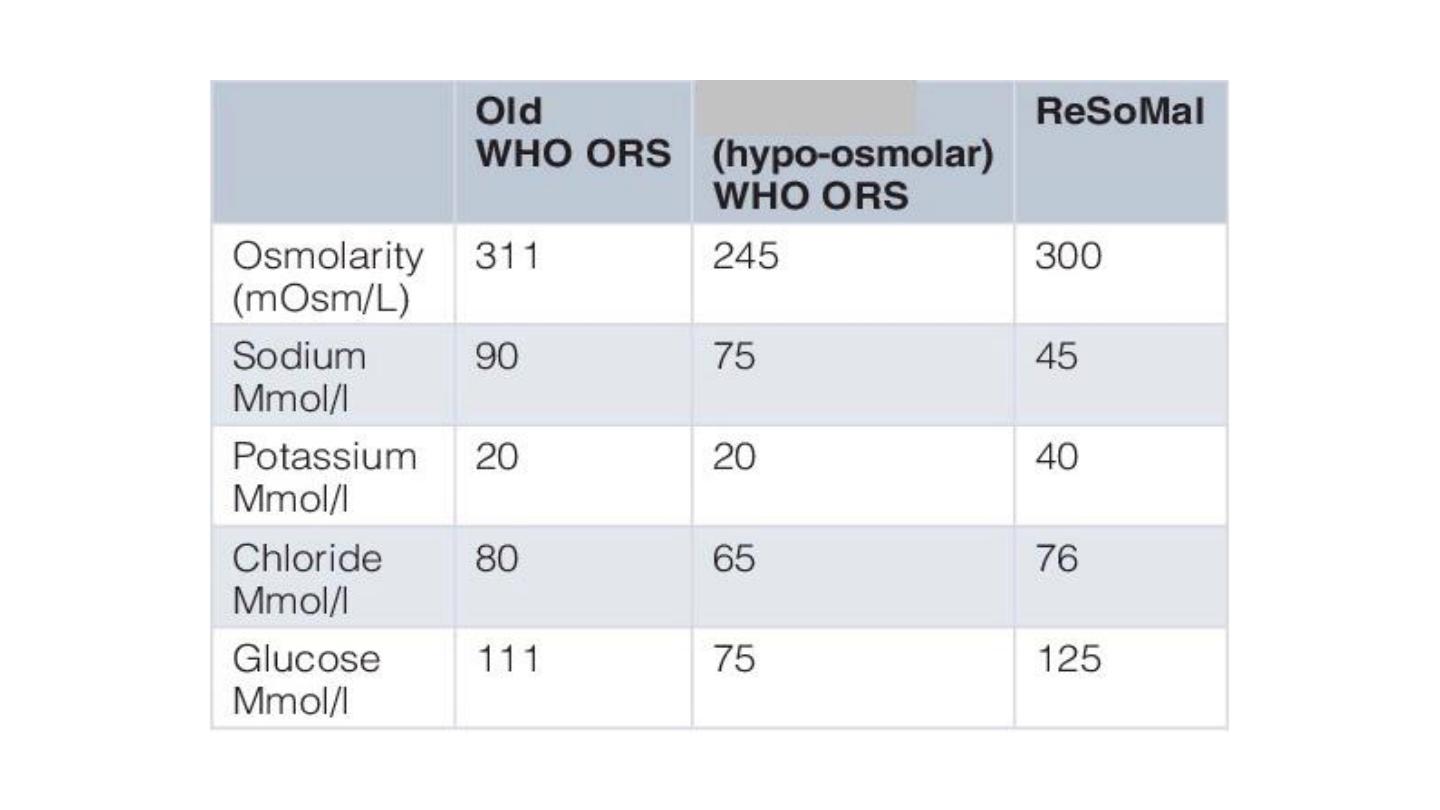
Types of ORS
Standard ORS
• 90 mmol/l sodium and 90 mmol/l glucose, total osmolarity 311 mmol/l).
• Previous version of ORS recommended by WHO before 2003.
Home prepared ORS
• A WHO publication for physicians recommends a homemade ORS consisting of
one liter water with
one teaspoon salt
(3 grams) and
two tablespoons sugar
(18
grams) added.

Types of ORS
ReSoMal (Rehydration Solution for Malnutrition)
• The original ORS (90 mmol sodium/L) and the current standard
reduced-osmolarity ORS (75 mmol sodium/L) both contain too much
sodium and too little potassium for severely malnourished children
with dehydration due to diarrhea.
• ReSoMal is recommended for such children. It contains
less sodium
(45 mmol/l) and
more potassium
(40 mmol/l) than reduced
osmolarity ORS.

Types of ORS
ReSoMal (Rehydration Solution for Malnutrition)
• Children with severe acute malnutrition and who have some or
severe dehydration but no shock should receive
5 mL/kg ReSoMal
every 30 min
for the first 2 h. Then, if the child is still dehydrated, 5–
10 mL/kg/h ReSoMal should be given in alternate hours, up to a
maximum of 10 h
• Children with severe acute malnutrition and signs of shock or severe
dehydration and who cannot be rehydrated orally or by nasogastric
tube should be treated with intravenous fluids.

Role of Zinc in treatment of diarrhea
Additive therapies
• As a part of oral rehydration therapy, the WHO recommends supplemental zinc
(10 to 20 mg daily) for ten to fourteen days, to reduce the
severity
and
duration
of the illness and make
recurrent
illness in the following two to three months less
likely.
• Preparations are available as a zinc sulfate solution for adults, a modified
solution for children and in tablet form.

Thank u
