
Infection in Bone and Joint

Infection in bone
Osteomyelitis
acute (subacute)
chronic
specific (eg TB)
non specific(most common)

Acute haematogenous OM
mostly children
boys> girls
history of trauma

Acute Osteomyelitis
Source Of Infection
infected umbilical cord in infants
boils, tonsillitis, skin abrasions
in adults UTI, arterial lines

Acute Osteomyelitis
Organism
Gram +ve
staphylococus aureus
strep pyogen
strep pneumonie
Gram -ve
haemophilus influnzae (50% < 4 y)
e .coli
pseudomonas auroginosa,
proteus mirabilis

Acute Osteomyelitis
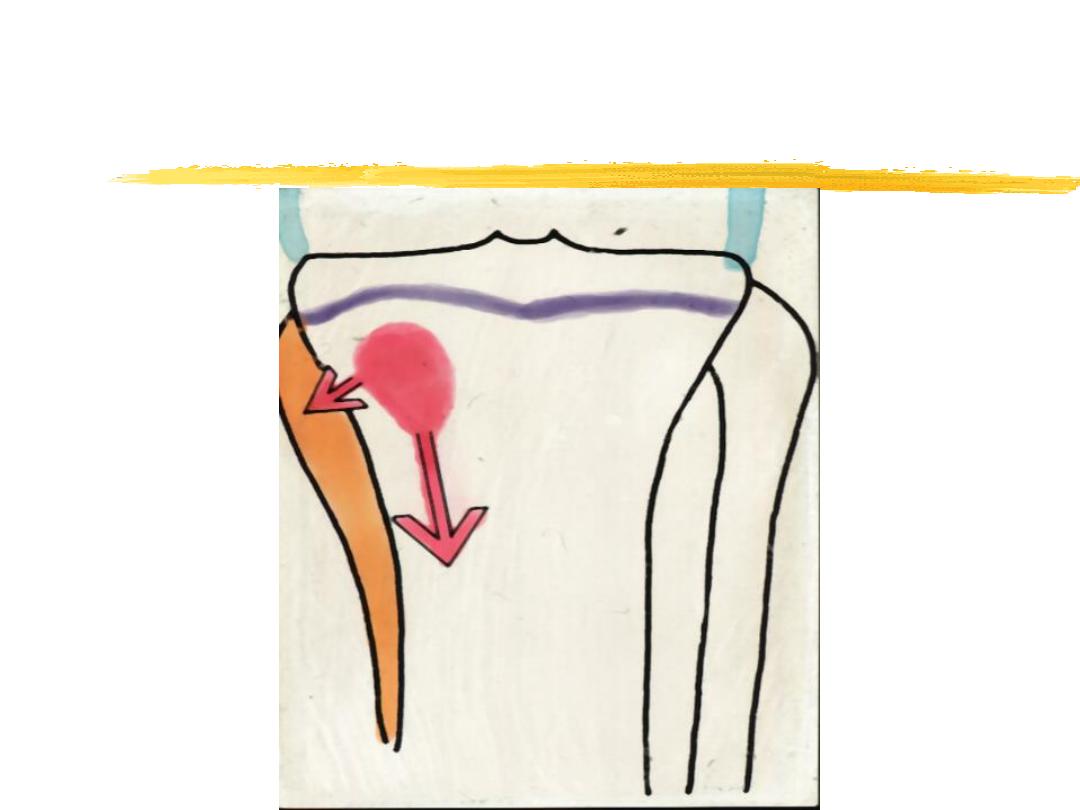
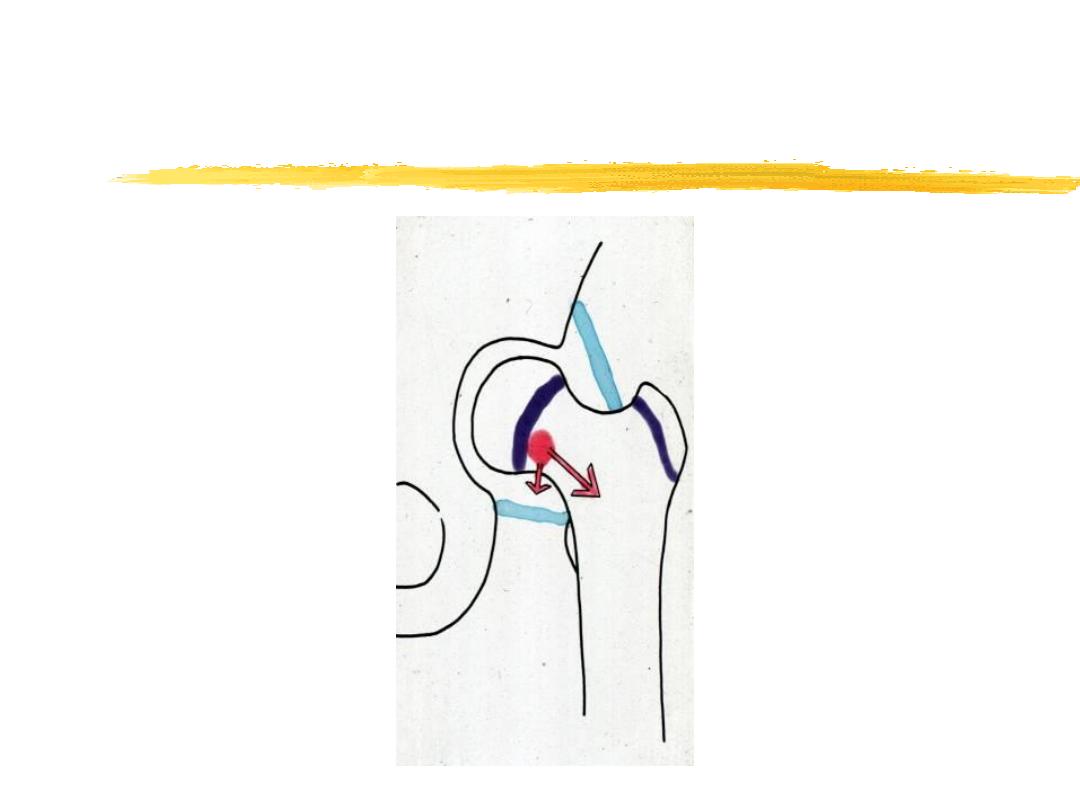
Pathology
starts at metaphysis
?trauma
vascular stasis
acute inflammation
suppuration
necrosis
new bone formation
resolution
Acute Osteomyelitis
Acute Osteomyelitis

Acute Osteomyelitis
Clinical Features
severe pain
reluctant to move
fever
malaise
toxemia

Acute Osteomyelitis
Infant
failure to thrive
drowsy
irritable
metaphyseal tenderness
decrease ROM
commonest around the knee

Acute Osteomyelitis
Adult
commonly thoracolumbar spine
fever
backache
history of UTI or urological procedure
old ,diabetic ,immunocompromised

Acute Osteomyelitis
Diagnosis
History and clinical examination
CRP, ESR, B.C.
X-ray (normal in the first (10-14) days
Ultrasound
Bone Scan Tc 99, Gallium 67
MRI
Aspiration

Acute Osteomyelitis

Acute Osteomyelitis
Differential Diagnosis
cellulitis
acute septic arthritis
acute rheumatism
sickle cell crisis
Gaucher’s disease

Acute Osteomyelitis
Treatment
supportive treatment for pain and
dehydration
splintage
antibiotics
surgery

Acute Osteomyelitis
Complications
septicemia
metastatic infection
septic arthritis
altered bone growth
chronic osteomyelitis

Subacute Osteomyelitis
Clinical features
long history (weeks, months)
pain, limp
swelling occasionally
local tenderness

Subacute Osteomyelitis
Pathology
Brodies abscess
a well defined cavity
in cancellous bone

Subacute Osteomyelitis
Investigation
X ray
Bone scan
Biopsy(50%) grow organism


Subacute Osteomyelitis
Treatment
antibiotics for 6 months
surgery

Other types of OM
Sclerosing OM (non suppurative OM)
Post-operative
early (within 3 months)
late

Chronic Osteomyelitis
May follow acute OM
May start De Novo
following operation
following open #

Chronic Osteomyelitis
Organism
usually mixed infection
mostly staph. Aureus E. Coli . Strep
Pyogen, Proteus

Chronic Osteomyelitis
Pathology
cavities
dead bone
cloacae
involucrum
histological picture is one of chronic
inflammation
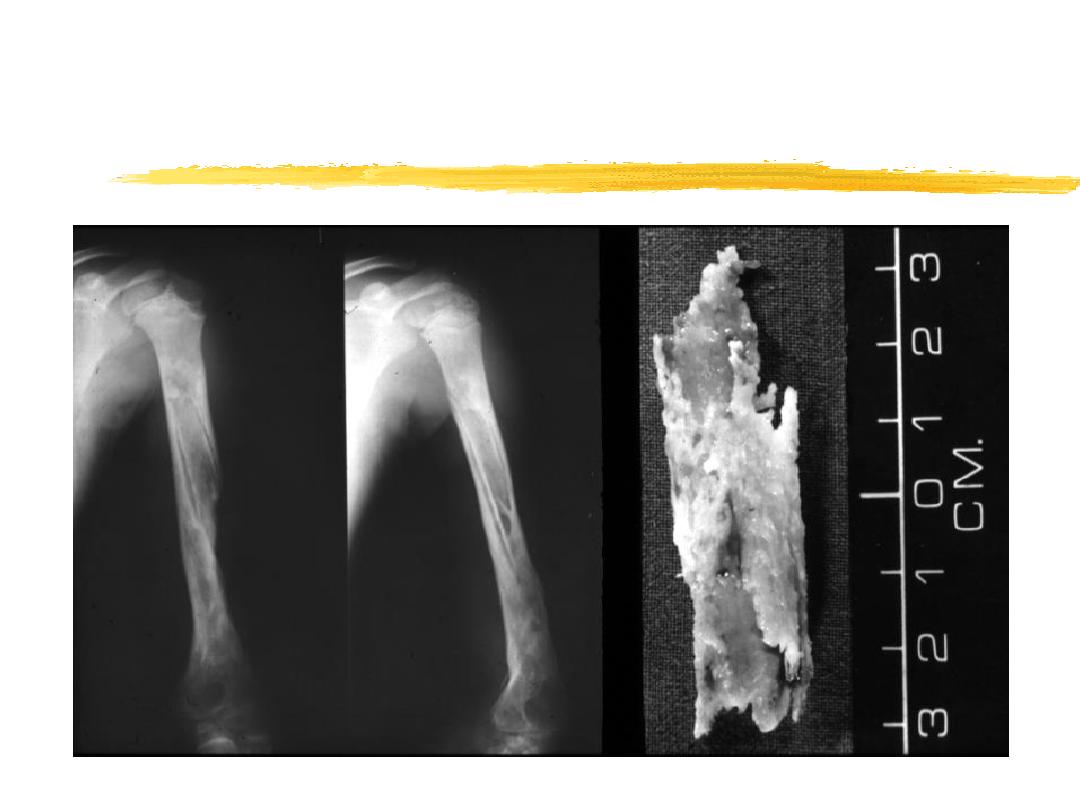
Chronic Osteomyelitis
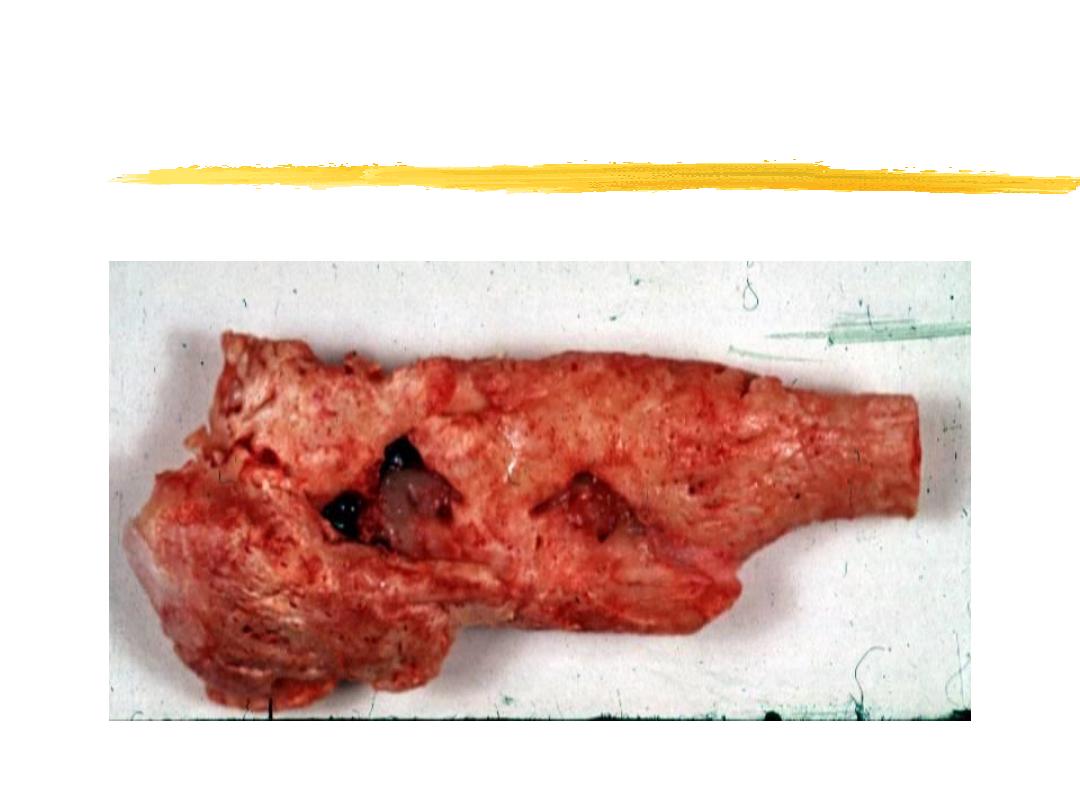
Chronic Osteomyelitis
Sequestrum
Treatment
1-antibiotics
2-surgery; sequestrectomy, muscle flap,
double lumen tube,ilazrov.

Acute Septic Arthritis
Route of Infection
direct invasion penetrating wound
intra articular inj
arthroscopy
eruption of bone abscess
haematogenous

Acute Septic Arthritis
Organism
staphylococus aureus
haemophilus influenzae
streptococcus pyogenes
escherishae coli

Acute Septic Arthritis
Pathology
acute synovitis with purulent joint effusion
articular cartilage attacked by bacterial
toxin and cellular enzyme
complete destruction of the articular
cartilage.

Acute Septic Arthritis
Sequelae
complete recovery
partial loss of the articular cartilage
fibrous or bony ankylosis

Acute Septic Arthritis
Neonate
Picture of Septicemia
irritability
resistant to movement

Acute Septic Arthritis
Child
Acute pain in single large joint
reluctant to move the joint
increase temp. and pulse
increase tenderness

Acute Septic Arthritis
Adult
often involve superficial joint (knee, ankle,
wrist)
investigation
BC, WBC, ESR, CRP ,blood culture
x ray
ultrasound
aspiration

Acute Septic Arthritis
Differential Diagnosis
acute osteomyelitis
trauma
irritable joint
hemophilia
rheumatic fever
gout
Gaucher disease

Acute Septic Arthritis
Treatment
general supportive measures
antibiotics
surgical drainage

Tuberculosis
Bone And Joint
vertebral body
large joints
multiple lesions in 1/3 of patient

Tuberculosis
Clinical Features
contact with TB
pain, swelling, loss of weight
joint swelling
decrease ROM
ankylosis
deformity

Tuberculosis
Pathology
primary complex ( in the lung or the gut)
secondary spread
tuberculous granuloma

Tuberculosis
Spinal
little pain
present with abscess or kyphosis

Tuberculosis
Diagnosis
long history
involvement of single joint
marked thickening of the synovium
marked muscle wasting
periarticular osteoporosis
+ve Mantoux test

Tuberculosis
Investigation
ESR,
Mantoux skin test.
Xray
soft tissue swelling
periarticular osteoporosi
articular space narrowing
Joint aspiration
AAFB identified in 10-20%
culture +ve in 50% of cases

Tuberculosis
differential diagnosis
transient synovitis
monoarticular ra
haemorhagic arthritis
pyogenic arthritis

Tuberculosis
Treatment
chemotherapy
rifampicin
isoniazid 8 weeks
ethambutol
rifampicin and isoniazid 6-12 month
rest and splintage
operative drainage rarely necessary
