
Injuries of the knee and leg
Acute knee ligaments injuries
The bony structure of the knee joint is inherently unstable , but the the strong capsule,
intra and extra-articular ligaments and controlling muscles provide stability.
Valgus stresses are resisted by fascia lata , pes anserinus, superfacial and deep layers
of the medial collateral ligament and posteromedial part of the capsule .In full
extension all these structures , as well as anterior cruciate ligament (ACL) , act
together to prevent both valgus and rotation.At 30 of flexion , the medial collateral
ligament is the main stabilizer.
The main checks to varus angulation are the illiotibial tract and the lateral collateral
ligament(LCL).
The cruciate ligaments provide both anteriopsterior and rotary stability.
Injuries of the knee ligaments are common ,particularly in sport and RTA, where
they may be associated with fractures and dislocation. They vary in severity from
simple strain to complete rupture.
Most ligaments injuries occur while the knee is bent, when the capsule and ligaments
are relaxed and the femur is allowed to rotate on the tibia.
Clinical presentation-
The patient gives a history of twisting injury and may even claim to have heard a
pop as the tissue snapped, the knee is swollen which appear immdiatley.there is pain
and tenderness is most acute over the torn ligament, and stressing one or other side of
the joint may produce severe pain . With complete tear the patient may have little or
no pain , whereas with partial tear the knee is painful , swelling also is worse with
partial tear, because the haemorhage remains confined the knee joint , with complete
tear the ruptured capsule permits leakage and diffusion. With partial tear attempted
movements is always painful, the abnormal movements of complete tear is often
painless or prevented by spasm. Abrasion suggest the site3 of impact , but bruising is
more important and indicates he site of damage . The doughy feel of haemarthrosis
distinguishes ligament injuries from meniscus injury with fluctuant feel. Tenderness
localizes the lesion , but the sharply defined tender spot of partial tear contrast with
the diffuse tenderness of complete one. The entire limb should be examined for other
injuries and for vascular and nerve damage.
The most important aspect of examinations is to test for stability , partial tear
permit no abnormal movements but causes pain. Complete tears permits abnormal
movements which sometimes is painless. To distinguish between the two is important
because their treatment is different , so if there is doubt , examination under
anesthesia is mandatory.
Imaging –plain x- ray may show that ligament has avulsed a small piece of bone –
the medial ligament usually from the femur , the lateral ligament from the the fibula ,
the anterior cruciate ligament from the tibial spine and the posterior cruciate ligament
from the back of upper tibia.
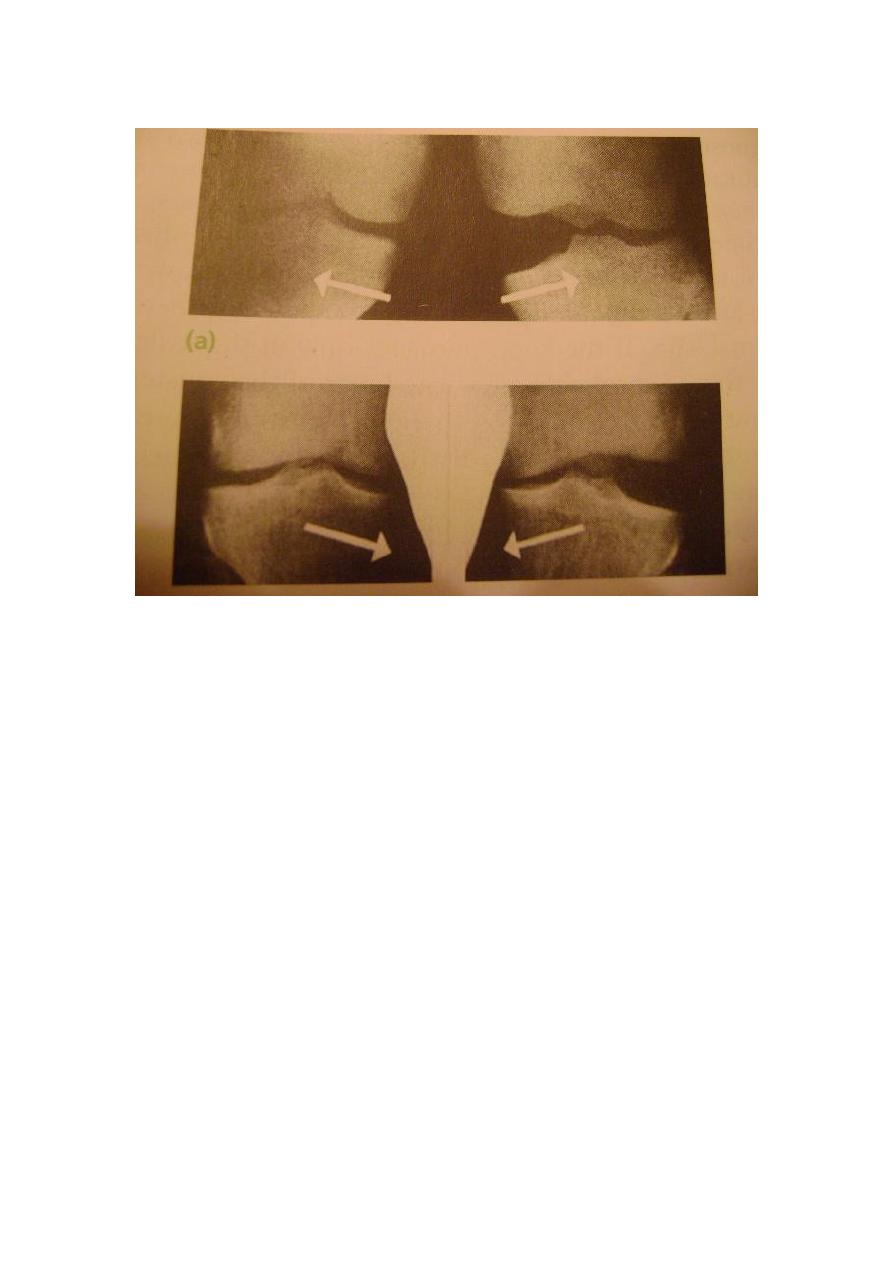
Stress film demonstrates if the joint hinge open on one side .
MRI is sometimes needed to distinguishes partial tear from complete tears.CT scan
may help to define osteo-articular fractures prior to internal fixation.
Arthroscopy is needed if there suspicions of isolated tear anterior cruciate ligament
tear and to exclude other internal injuries such as mensical tears.
Treatment
A-sprains and partial tear – the intact fibers splint the torn ones and spontaneous
healing will occur. The hazard is the adhesions , so active exercises is prescribed from
the start and facilitated by aspiration of tense effusion , applying of ice packs to the
knee and , sometimes by injecting local anesthesia into the tender area. Weight –
bearing is permitted but the knee is protecte4d from rotation or angulation strains by
heavy padded bandage or functional brace.
B-complete tears
1-isolated tear of medial collateral ligament: long cast brace is applied for 6 weeks
and thereafter graded exercise are encouraged.
2-isolated tear of lateral ligament : treated as for medial ligament(MCL).
3-isolated tear of ACL: operative reconstruction is indicated in a-professional
sportsmen b- if there is avulsion of tibial spine . in others , the treatment is
conservative , the cast brace is worn only until symptoms subsides and thereafter
movement and muscle strengthing exercise are encouraged.
4-isolated tear of posterior cruciate ligament treated conservatively.
5- combined injuries: a) combined ACL and collateral ligament injury –
reconstruction of the ACL often obviates the need for collateral ligament treatment .
b) combined posterior cruciate ligament and collateral ligament injuries – similar is
used but , here all the damaged structures to be repaired.
Dislocation of the knee
The knee can be dislocated by considerable violence , as in RTA . The cruciate
ligaments and one or both lateral ligaments are torn.
Clinical features: a-severe bruising b- swelling c- gross deformity d- the distal
pulsation must be examined to exclude damage of the popliteal artery also sensation
of the limb must be checked.
x-ray – in addition to the dislocation , the film occasionally reveal a fracture of the
tibial spine . if there is any doubt about the circulation ., an arteriogram should be
done.
Treatment
a) closed reduction under anesthesia must be done urgently , this achieved by pulling
directly in the line of the leg , but hyperextension must be avoided because of the
danger to the popliteal vessels , after that the limb is rested on a back splint with the
knee in 15 degree of flexion , the circulation is checked during the next week. If the
joint is unstable , an anterior external fixation can be applied. B) open reduction is
indicated in 1-failure of closed reduction 2-open wound 3-vascular damage. When
swelling ha subsided , a cast is applied and worn for 12 weeks , weight bearing in the
plaster is permitted as soon as the patient can left the leg.
Complication
a) early 1- arterial damage – popliteal artery damage is common and need immediate
repair 2- nerve injury – the common peroneal nerve may be injured , but fortunately it
recover by itself

b) late 1- joint instability 2- stiffness may occur due to prolonged immobilization.
Acute injuries of the extensor apparatus
Disruption of the extensor apparatus may occur in the quadriceps tendon , at the
attachment of quadriceps tendon to the proximal surface of the patella , through the
patella and retinacular expansion , the patellar ligament or at the insertion of the
patellar ligament to the tibial tubercle.
In all but direct fractures of the patella , the mechanism of the injury is the same ,
sudden resisted extension of the knee or sudden passive flexion of the knee while the
quadriceps is contracting.
The lesion tends to occur at progressively higher level with increasing age :
adolescent suffer avulsion fracture of the tibial tubercle , young adult sport men tear
the patellar ligament , middle aged adult fracture their patella , and older people suffer
acute tear of the quadriceps.
Rupture of the quadriceps tendon
The patient is usually elderly , may have a history of diabetes or rheumatoid
disease, or may have been treated with corticosteroid .occasionally acute rupture is
seen in young athlete. the typical injury is followed by tearing pain and giving away
of the knee .There is bruising and local tenderness, sometimes a gap can be felt
proximal to the patella . Active knee extension either impossible (complete tear) or
weak(partial tear) . The diagnosis can be confirmed by MRI.
Treatment
a)partial tear :plaster cylinder is applied for 6 weeks followed by physiotherapy.
b)complete tear :need operative treatment.
Rupture of the patellar ligament
This is uncommon injury , it is usually seen in young athletes and the tear is almost
always at the proximal or distal attachment of the ligament. There may be previous
history of tendonitis and local injection of corticosteroid.
The patient gives a history of sudden pain on forced extension of the knee , followed
by bruising , swelling and tenderness at the lower edge of the patella or more distally.
X- ray may show a high riding patella and a tell-tale flake of bone torn from the
proximal or distal attachment of the ligament. MRI will help to differentiate a partial
from a complete tear.
Treatment
Partial tear can be treated by applying plaster cylinder .complete tear need operative
repair or reattachment to the bone.
Fracture patella
The patella is a sesamoid bone in continuity with quadriceps tendon and the patellar
ligament . there are additional insertion from the vastus medialis and lateralis into the
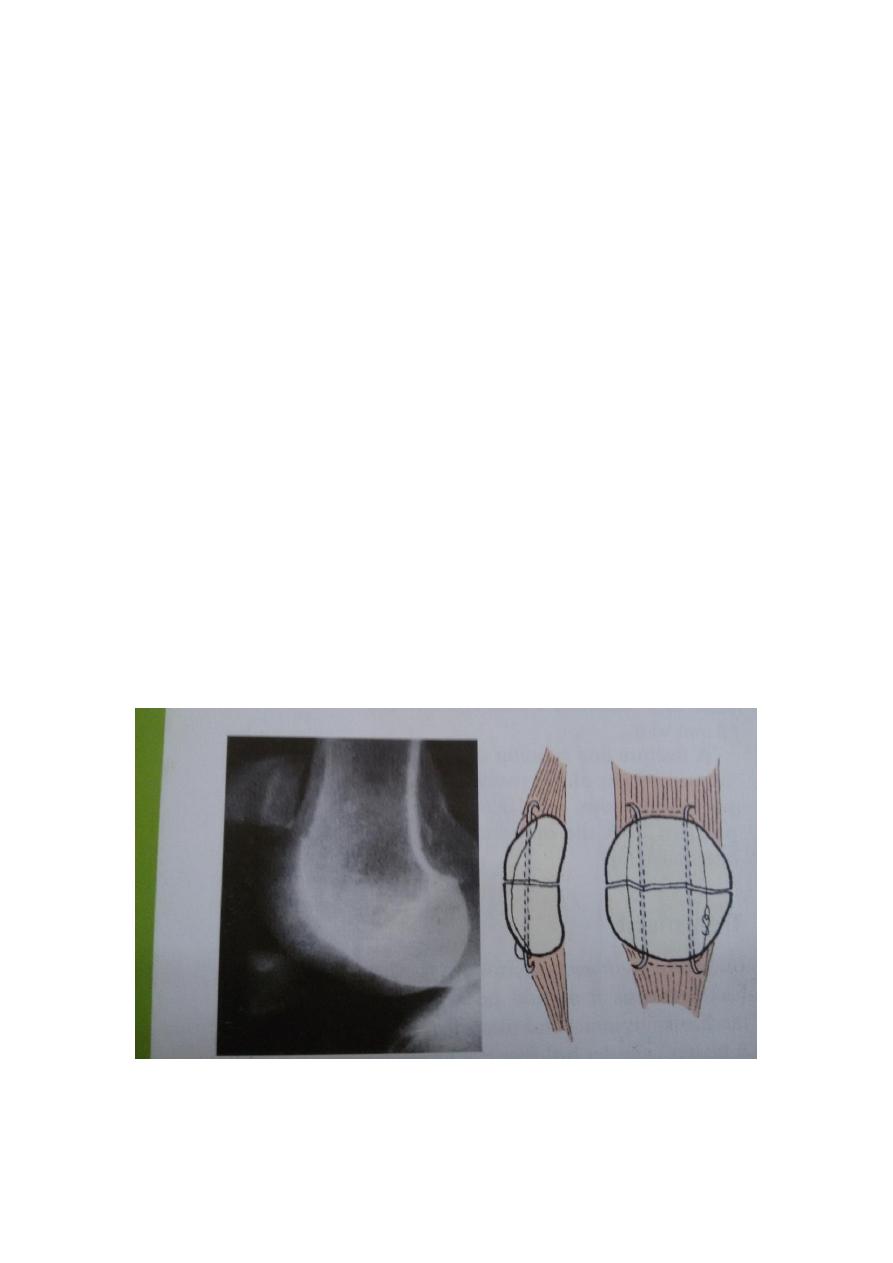
medial and lateral edges of the patella. The extensor strap is completed by the medial
and lateral extensor retinacula which bypass the patella and insert into the proximal
tibia.
The key to the management of patellar fractures is the state of the entire extensor
mechanism.if the extensor retinacula are intact , active knee extension is still possible
even if the patella itself is fractured..
Mechanism of injury
The patella may be fractured by direct force or by indirect traction force that pulls
the bone apart.
Direct injury usually a fall into the knee or a blow against the dashboard of a car
causes either undisplaced c rack or a comminuted fracture, without severe damage to
the extensor expansion.
Indirect injury occurs typically when someone c atches the foot against a solid
obstacle and to avoid falling , contracts the quadriceps muscle forcefully . this is a
transverse fracture with a gap between the fragments.
Clinical features
The knee is painful , swollen. there may be abrasion or bruising over the front the
joint . the patella is tender and sometimes a gap can be felt.
Active knee extension should be tested , if the patient an left the leg, quadriceps
mechanism is still intact. If there is an effusion , aspiration may reveal the presence of
blood and fat droplets.
X-ray may show one or more fine fracture lines without displacement , multiple
fracture lines with irregular displacement or transverse fracture with gap between the
fragments.
Patellar fractures are classify as transverse ,polar ,longitudinal or comminuted.
Displacement is significant if the the gap between the fragment is more than 3mm or
if the displacementc reate astep on the articular surface of the
patella.
Treatment

a)undisplaced or minimal displaced fractures : a cylinder cast holding the knee
strieght is worn for 3-4 weeks with quadriceps exercises, if there is a haemoarthrosis
it is aspirated.
b)comminuted fracture can be treated by cylinder cast .
c)displaced transverse fracture
the lateral expansions are and the entire extensor mechanism is disrupted, operation is
essential.
Dislocation of the patella
Because the knee is normally angled in slight valgus , there is natural tendency for the
patella to pull towards the lateral side when the quadriceps muscle contract. Lateral
deviation of the patella during extension is prevented by number of factors 1-
intercondlyler groove2-medial patellofemoral ligament3-medial patellomensical and
patellotibial ligaments 4-medial retinacular fibers.
Mechanism of injury
1-while the knee is flexed and quadriceps muscle relaxed , the patella may be forced
laterally by direct violence which is rare. 2- indirect force due to sudden severe
contraction of quadriceps muscle while the knee is steched in valgus and external
rotation, this is more common.
Predisposing factors
1-genu valgum 2- tibial torsion 3- high riding patella 4-shallow intercondylar groove
5- patellar hyper mobility.
Clinical features
The patient may feel a tearing pain sensation and feeling that the knee has gone out
of the joint , when running , the patient may collapse and fall into the ground . often
the patella spring back into position spontaneously , however if it remains unreduced ,
there is obvious deformity, the displaced patella seated on the lateral side of the knee ,
neither active or passive movement is possible.
If dislocation has reduced spontaneously , the knee may be swollen and there may
be bruising and tenderness on the medial side.
Imaging
Ap ,lateral and tangential x-ray views are needed . in an unreduced dislocation , the
patella is seen to be laterally displaced and tilted or rotated.
MRI may reveal soft tissue lesion, torn ligaments and articular cartilage and bone
damage.
Treatment
In mostc ases the patella can be pushed back into place without much difficulty and
anesthesia not needed , the exception is intra articular dislocation which may need
open reduction, the knee is aspirated and then immobilized in full extension in cast for
2-3 weeks .

Tibial plateau fractures
Fractures of the tibial plateau are caused by avarus or valgus force combined with
axial loading. This sometime the result of car striking a pedestrian , more often it is
due to a fall from height in which the knee is forced into valgus or varus.the tibial
ondyle is crushed or split by the opposing femoral condyle which remain intact.
Classification
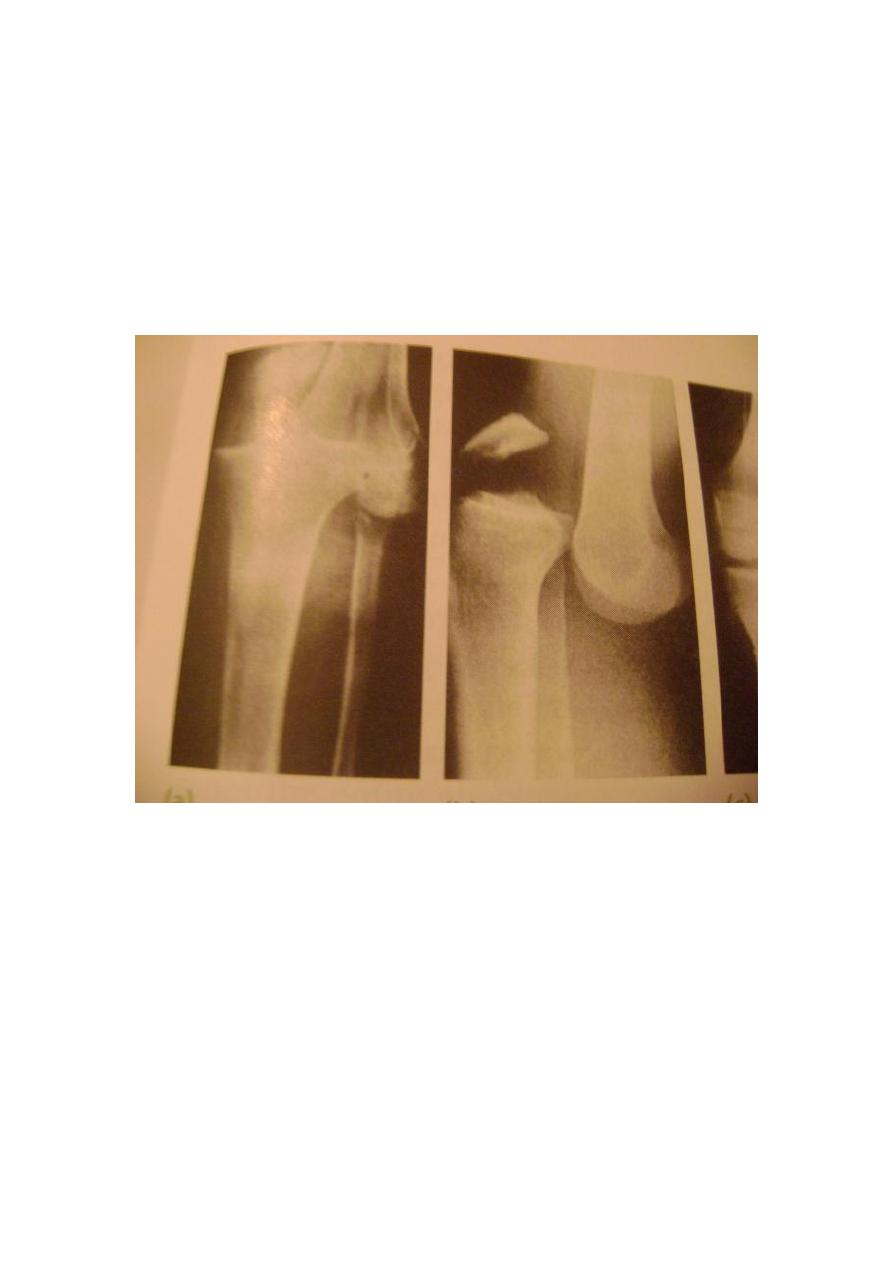
The most useful classification is that of Schatizker
Type 1- vertical split fracture of the lateral condyle . this is a fracture through
dense bone , usually in young people .
Type 2- vertical split of the lateral condyle combined with depression of adjacent
load bearing part of the condyle .
Type 3- depression of the artciular surface with intact condyler rim , this injury is
the commonest one , typically occurs in older people who are osteoporotic.
Type 4- fracture of the medial tibial condyle .
Type 5- fracture of bothc ondyles, and tibial shaft is wedged between them.
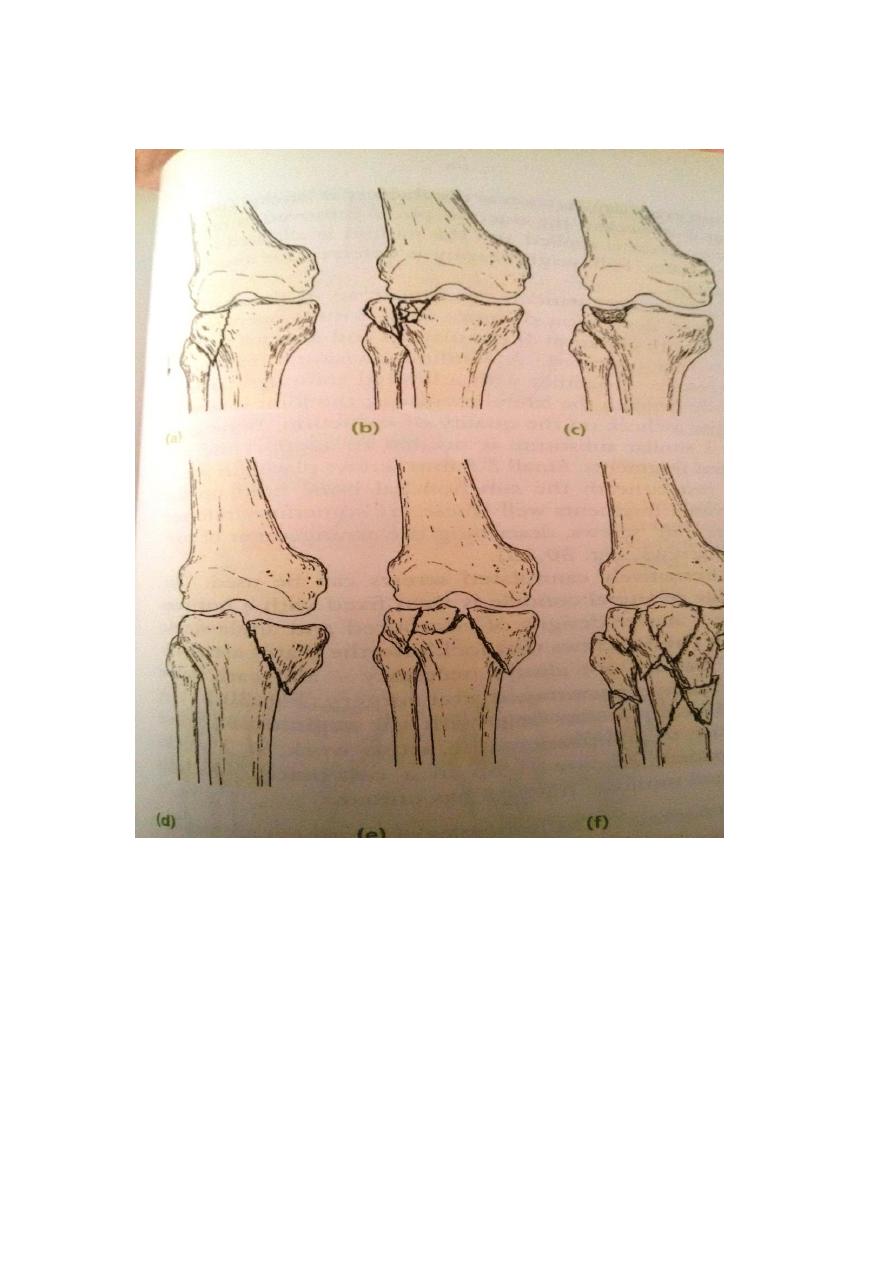
Type 6- combined condyler and subcondyler fractures, this is a high energy injury
which may result in severec omminution.
Clinical features
The knee is swollen and may deformed. Bruising is usually extensive and the tissue
feel doughy because of haemoarthrosis. Gentle examination may suggest medial or
lateral instability. The leg and foot should be examined for signs of vascular or
neurological injury.
X-ray
Ap,lateral and oblique views will usually show the fracture, but the amount of
Comminution may not appreciated without tomograghy.
Stress views are sometimes helpful in assessing the degree of joint instability.
Treatment

Type 1- fractures if undisplaced can be treated conservatively . the haemarthrosis is
aspirated and a compression bandage is applied, as soon as the acute pain subside and
selling subsided , a hinge cast brace is fitted and the patient is allowed up . after 4
weeks , partial weight bearing is permitted but full weight bearing is delayed until the
fracture has healed.
Displaced fractures should be treated by open reduction and internal fixation.
Type 2- if depression is slight (less than 5 mm), the knee is stable and the patient is
old and frail, the fracture is treated closed with the aim of regaining mobility and
function. After aspiration and compression bandaging, skeletal traction is applied via
a threaded pin passed through the tibia 7 cm below the fracture. An attempt is made to
squeeze the condyle into place , the knee is then flexed and extended several times to
mould the upper tibia on the opposing femoralc ondyle, as soon as the fracture is
sticky , the traction pin is removed , a hinged cast brace is applied and the patient is
allowed up on crutches, but full weight bearing is deferred for 10 weeks .
In young patients , and more so in those with central depression of wore than 5mm
.open reduction and internal fixation is preferred.
Type 3- the principles of treatment are similar to type 2 fractures.
Type 4- a) osteoporotic crush fracture of medial plateau are difficult to reduce , in
long term the patient is likely to be left with some degree of varus deformity . the
principles of treatment are the same as for rush fracture of the lateral plateau.
b) for medial condyler split fracture , if undisplaced can be treated closed as for an
undisplaced type 1 fracture . displaced fracture will need open reduction and internal
fixation.
Type 5&6 fractures , a simple bicondyler fracture in an elderly patient can often be
reduced by traction and the patient is then treated as for type 2 injury , more complex
fractures with Comminution especially in younger adult are better managed
operatively.
Complications
Early
1- compartment syndrome , with closed type 5&6 fractures , there is considerable
bleeding and swelling of the leg.
Late
1-joint stiffness 2- deformity 3- osteoarthritis
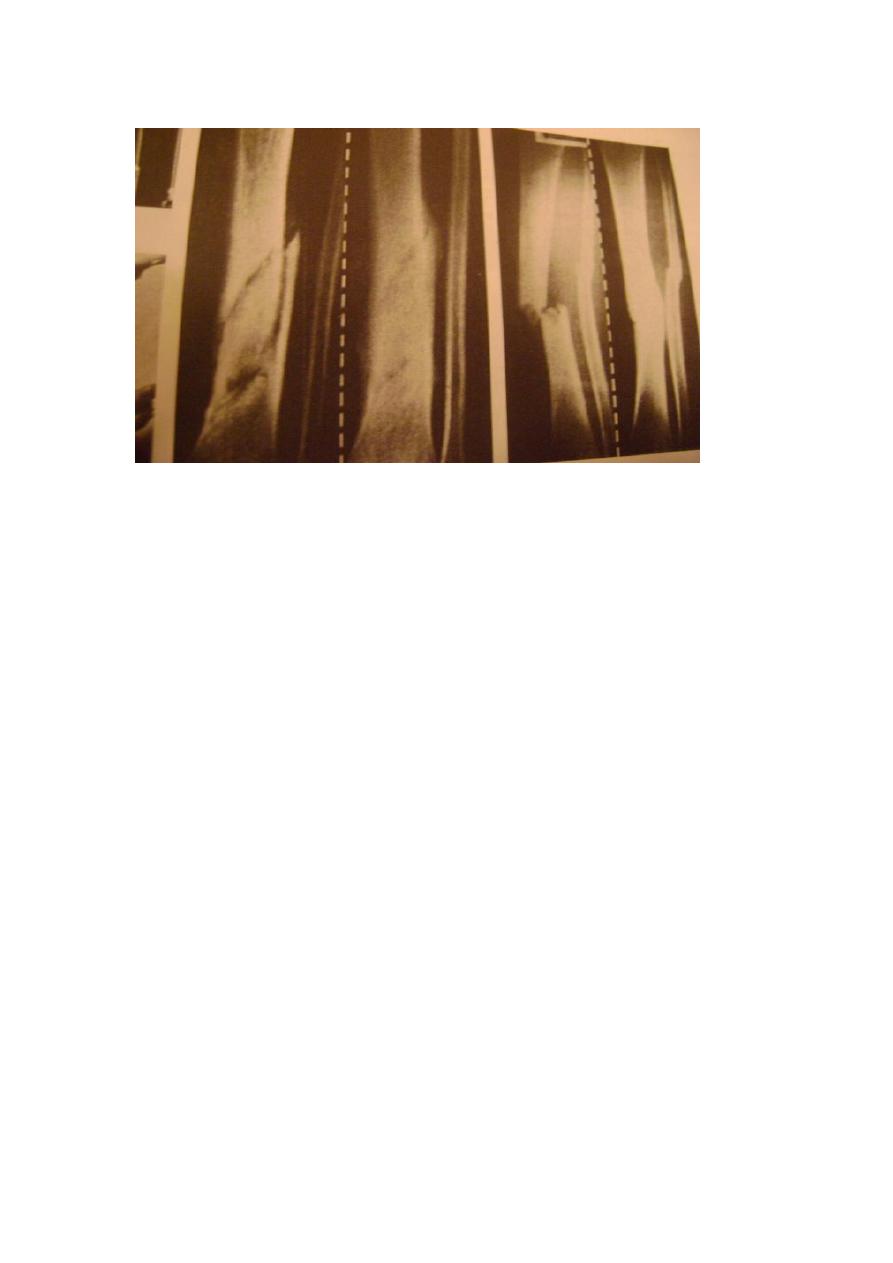
Fractures of the tibia and fibula
The tibia is more commonly fractured , and more commonly sustain an open fracture
than any other long bone because of its subcutaneous position.
Mechanism of injury
A twisting force causes a spiral fracture of both leg bones at different levels ,
angulatory force produces transverse or short oblique fractures at the same level.
Direct injury rushes or split the skin over the fracture, this is usually a high energy
lesion.
The risk of complication and progress to fracture healing are directly related to the
amount and type of soft tissue damage.
The following table show Gustilos classification of open fractures
Bone injury
Soft tissue injury
Wound
Grade
Simple low energy fracture , spiral or
long oblique
minimal
Less than 1
cm long
1
Moderate comminution
Moderate , some muscle damage
More than
1cm long
2
High fracture pattern , comminuted
but soft tissue cover possible
Severe deep contusion plus –
minus compartment syndrome
More than
1cm long
3a
Requires soft tissue reconstruction
for cover
Severe loss of soft tissue cover
More than 10
cm long
3b
Requires soft tissue reconstruction
for cover
As 3b , with vascular injury that
need repair
More than
10cm long
3c
Clinical features
The limb should be carefully examined for signs of soft tissue damage :bruising ,
severe swelling , crushing or tenting of the skin , an open wound , circulatory changes
, diminution or loss of sensation and inability to move the toes . always be on the alert
for signs of an impending compartment syndrome.
X-ray
The entire length of both tibia and fibula , as well as the knee and the ankle joint must
be seen. Spiral fractures without Comminution are low energy injuries .transverse ,
short oblique and comminuted fractures especially if displaced are usually high
energy
injuries.
Management
The main objectives are 1-tolimit soft tissue damage and preserve cover2- to prevent
or at least recognize compartment swelling 3- to obtain and hold fracture alignment 4-
b to start early weight bearing 5- to start joint movement as soon as possible.
Low energy fractures
Most low energy fractures including Gustilo 1&2 injuries after attention to the wound
can be treated non operative methods.
If the fracture is undisplaced or minimally displaced a full length cast from upper
thigh to metatarsal neck is applied with the knee slightly flexed and the ankle at right
angle , displacement of the fibular fracture is ignored.
If the fracture is displaced , it is reduced under general anesthesia with x-ray control
. apposition need not to be complete but alignment must be near perfect (no more 7
degree of angulation) and rotation absolutely perfect. A full length cast is applied as
for undisplaced fractures. The position is checked by x-ray , minor degrees of
angulations can still bec orreted by making transverse cut in the plaster and wedging it
into a better position.
The limb is elevated and the patient is kept under observation for 48-72 hours to
avoid compartment syndrome. After 2 weeks , the position is checked by x – ray . the
cast is retained until the fracture unites , which is 8 weeks in children but seldom
under 16 weeks in adults.
Indication for fixation in low energy fractures
1-failure of closed reduction 2- non union 3- unstable fractures.
High energy fractures
Initially the most important consideration is the viability of the damaged soft tissue
and underlying bone.
Tissues around the fracture should be disturbed as little as possible and open
operation should be avoided unless there is already an open wound, transverse
fractures are usually stable after reduction, they can be treated closed , provided a
careful watch is kept for symptoms and signs of compartment syndrome.
Comminuted and segmental fractures , those associated with bone loss and any
high energy fracture which is inherently unstable requires early surgical stabilization.
Open fractures
A suitable treatment for open fractures include : 1- antibiotics 2- debridement 3- soft
tissue cover 4- rehabilitation
Antibiotics are started immediately , a second generation cephalosporin is suitable
for Gustilo type 1-3a wounds , but more severe grades benefit from gram –negative
cover as well. If the wound result from agricultural accident, anaerobic cover with
metronidazole should be added.
Adequate debridement is possible only if the original wound is extended , however
excise as little skin as possible .
Gustilo grade 1 injury an be closed primarily and then treated as for closed injuries
, more severe wounds are left open and reexamined within 48 hours , if necessary a
further debridement is carried out.
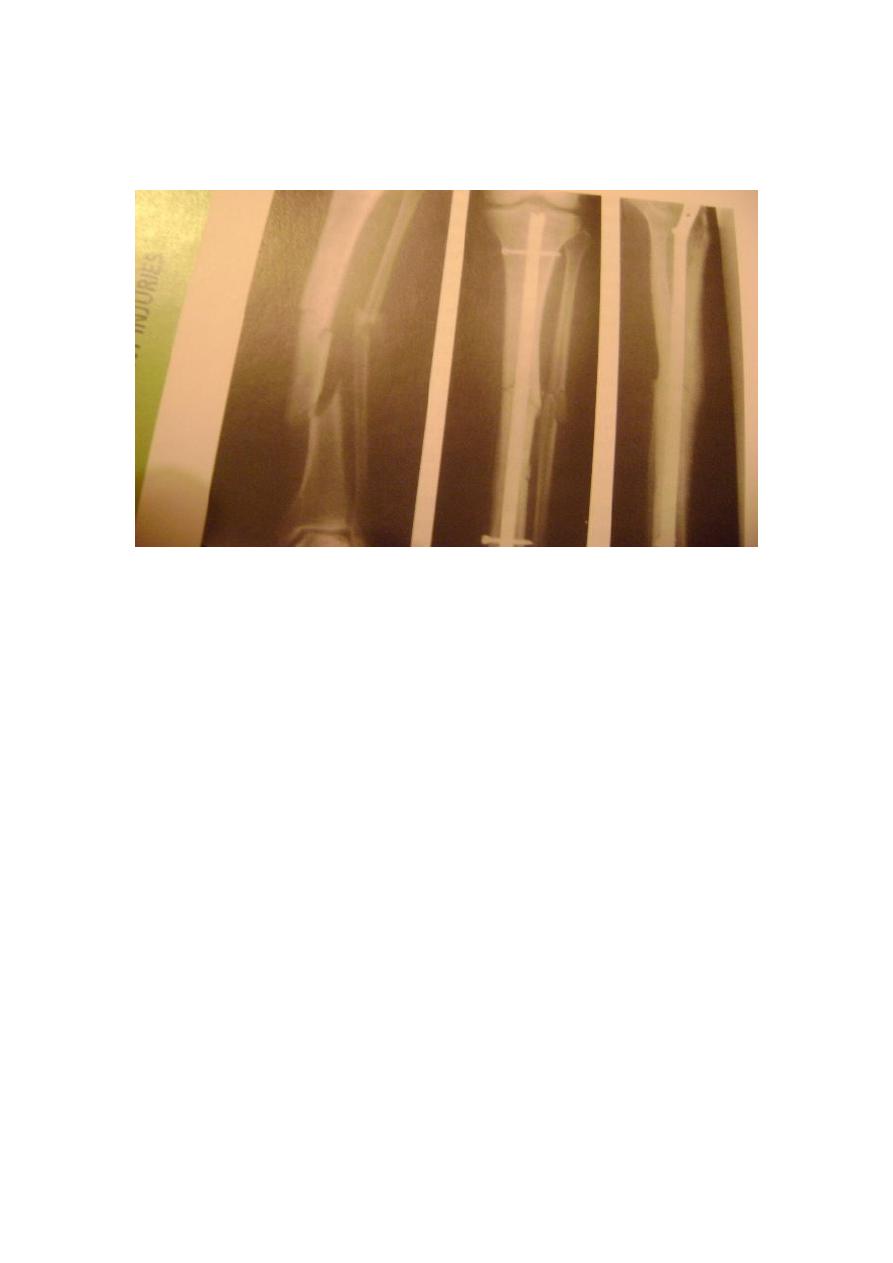
It is important to stabilize the fracture , for Gustilo 1,2,3a injures locked
intramedullary nailing is permissible. For Gustilo 3 b&c , it is wiser to apply an
external fixators , leaving the wound free to be inspected and treated as
necessary.
Early complications
1-vascular injury , due to fractures of proximal half of the tibia may damage popliteal
artery , this require urgent repair.
2- compartment syndrome . tibial fractures, both open and closed and intramedullary
nailing are the commonest causes of compartment syndrome of the leg.
3- infection ,open fractures are always at risk .

Late complications
1-malunion 2- delayed union 3- non union 4- joint stiffness 5-osteoporosis 6-
algodystrophy.
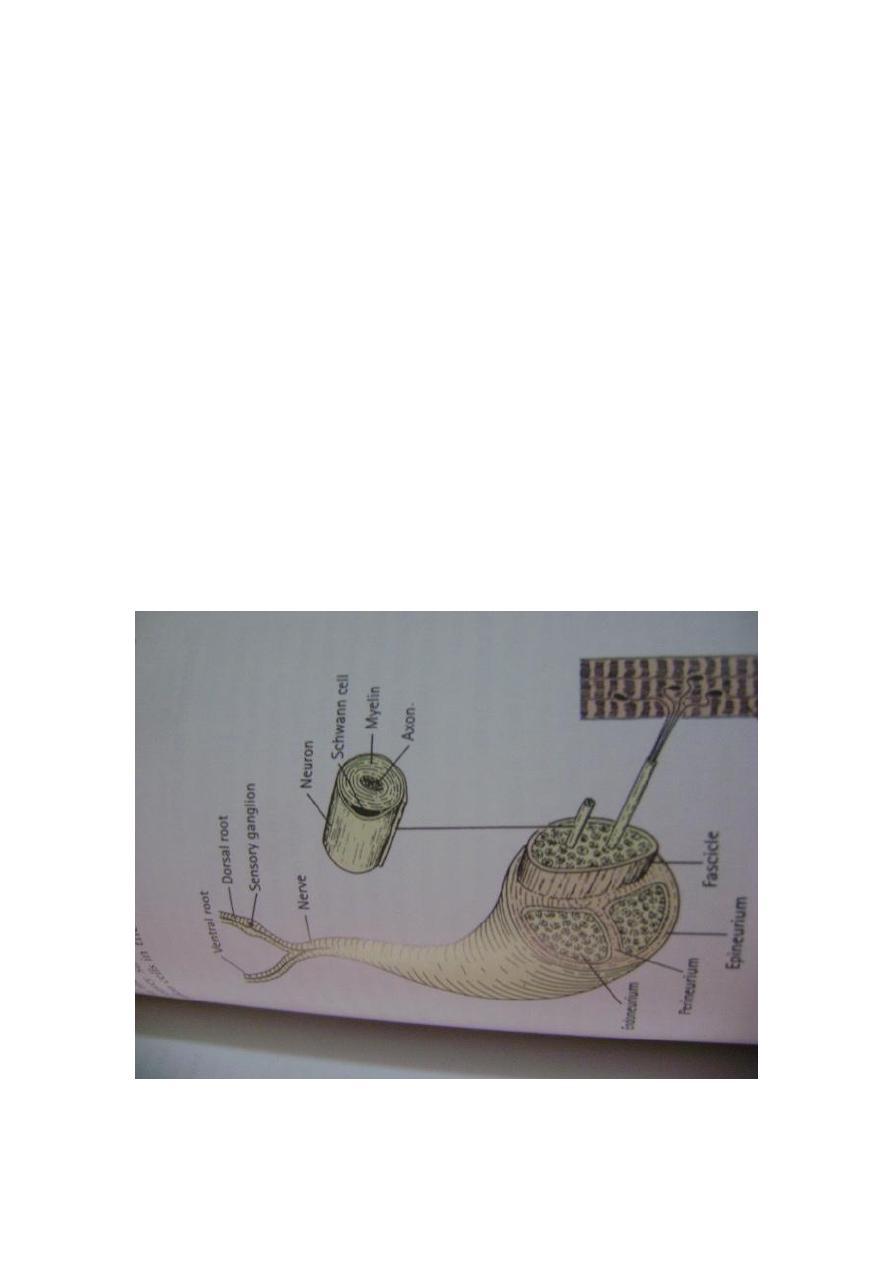
Peripheral nerve injuries
Seddon description of three different types of nerve injury (neuropraxia,
axonotmmesis, and neurotemesis) served as useful classification for many years .
Increasingly ,however, it has been recognized that manyc ases falls into an area
some where between axonotemesis and neurotemesis. Therefore , following
Sunderland, amore useful practical classification is offered here .
1-first degree injury , this embraces transient ischemia and neuropraxia , the effect is
reversible.
2-secnd degree injury , this correspond to axontemesis , the endoneurium is
preserved, regeneration can lead to complete or near complete recovery without the
need for intervention.
3- third degree injury , this is worse than axonotemesis , the endoneurium is disrupted
but the perineurial sheaths are intact and the internal damage is limited . fibrosis and
cross connection will limit recovery.
4-fourth degree injury ,here only the epineurium is intact. The nerve trunk is still in
continuity but the internal damage is severe , recovery is unlikely , the injured
segment should be excised and the nerve repaired or grafted.
5- fifth degree injury, the nerve is divided and will have to be
repaired.
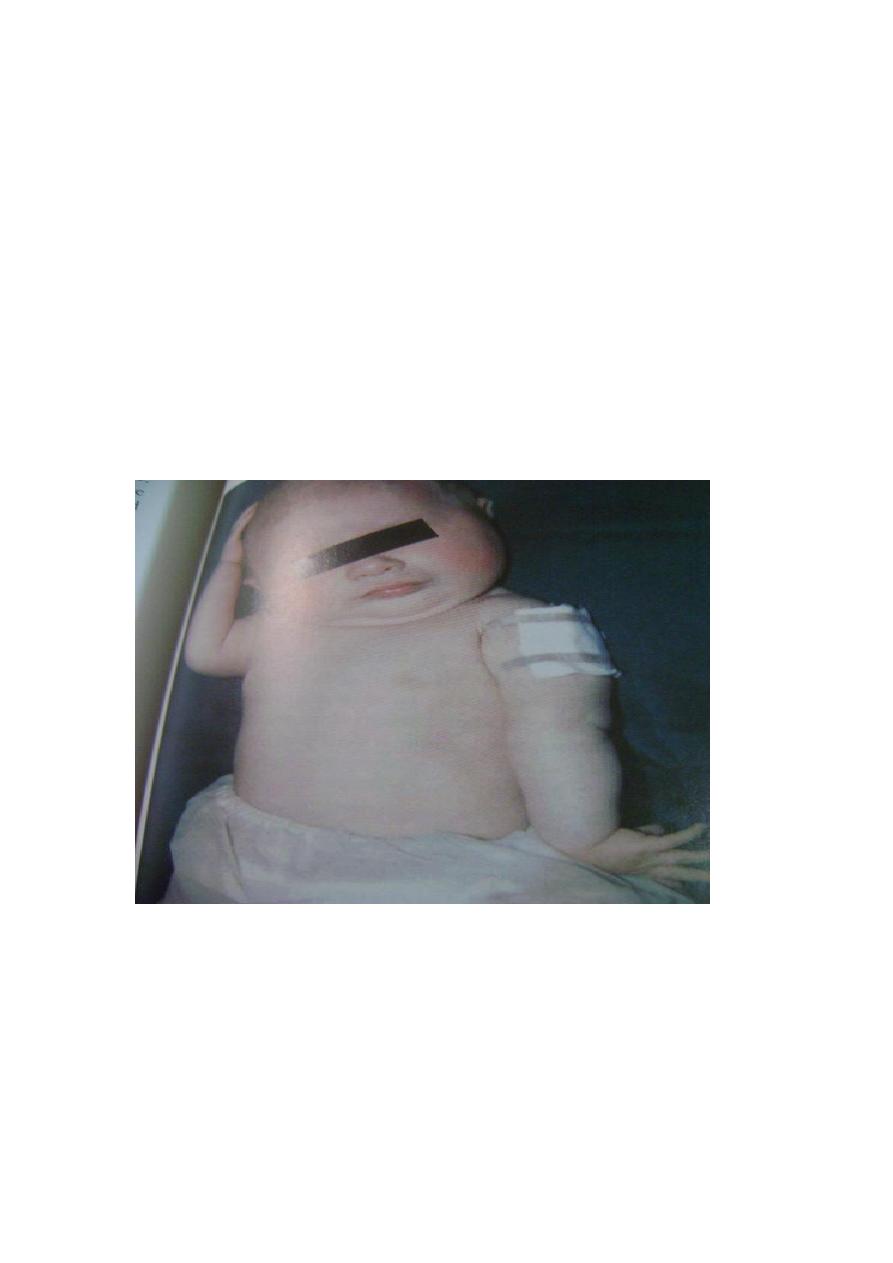
Obstetrical brachial plexus palsy
Obstetrical palsy is caused by excessive traction on the brachial plexus during the
childbirth . two pattern are seen 1- upper root injury (Erb palsy), typically in
overweight baby with shoulder dystocia delivery or 2- complete plexus
injury(Klumpkes palsy) , usually after breech delivery of smaller babies.
Clinical features
The diagnosis is usually obvious at birth , after a difficult delivery the baby has a
floppy or flail arm. Further examination a day or two later will define the type of
brachial plexus injury .
Erb palsy is caused by injury of c5& c6 and s.t c7 , the abductors and external
rotators of the shoulder and the supinator are paralyzed. The arm is held to the side ,
internally rotated and pronated . there may also be loss of finger extension. Sensation
can not be tested reliably in baby.
Klumpk is much less common , but more worse. This is complete plexus lesion , the
arm is flail and pale , all finger muscles are paralyzed and there may be also be
vasomotor impairment and unilateral Horner syndrome.
x-ray should be taken to exclude shoulder or clavicular
fracture.
Management
Over the next few weeks one of several things may happen
1-paralysis may recover completely , many of the upper root lesions recovers spont. A
fairly reliable indicator is return of biceps activity after 3 month.
2- paralysis may improve . atotal lesion may partially resolve , leaving the infant with
either an upper root or c omplete root syndrome which is unlikely to change.
3- paralysis may remain unaltered, this is more likely with complete lesion.
While waiting for recovery , physiotherapy is applied to keep the joint mobile.
Operative treatment

If there is no biceps recovery by 3 months , operative intervene., should be considered
. unless the roots are avulsed , it may be possible to excise the scar and bridge it with
nerve graft. If the root are avulsed , nerve transfer may give good results.
Axillary nerve
The axillary nerve (c5&c6) arises from the posterior cord of the brachial plexus. The
nerve is sometimes ruptured in brachial plexus injury. More often it is injured during
shoulder dislocation or fractures of the humeral neck. Iatrogenic injuries occur in
transaxillay operation and with lateral deltoid splitting incisions.
Clinical features
The patient complains of shoulder weakness , and the deltoid is wasted . although
abduction can be initiated, it can not maintained . retropulsion is impossible , careful
testing will reveal a small area of numbness over the deltoid.
Treatment
Nerve injury associated with fractures or dislocation recovers spontaneously in about
80% of cases . if the deltoid shows no signs of recovery by 6-8 weeks , EMG should
be done , if tests suggest denervation then the nerve is explored. If operation of repair
failed , provided that trapezius and serratus anterior are functioning , shoulder
arthrodesis can provide both stability and some degree of abduction.
Radial nerve
The radial nerve may be injured at the elbow , in the upper arm or in the axilla.
Clinical features
Low lesion are usually due to fractures or dislocation at the elbow , or to local wound
. iatrogenic lesion of posterior interosseous nerve where it winds through the
supinator muscle are sometimes seen after operation on the proximal end of the
radius. The patient complains of clumsiness and on testing , can not extend the
metacarpophalingeal joints of the hand. In the thumb , there is also weakness of
abdution and interghalangeal extension. Wrist extension is preserved because the
branch to the extensor carpi radialis longs arises proximal to the elbow.
High lesion occur with fractures of the humerus or after prolonged tourniquet
pressure . there is an obvious wrist drop , due to weakness of the radial extensor of
the wrist , as well as an ability to extend their metacarpoghalangeal joints . sensory
loss is limited to a small patch on the dorsum around the anatomical snuffbox.
Very high lesions may be caused by trauma or operation around the shoulder. More
often , they are due to chronic compression in the axilla , this is seen in drinker and
drug addicts (Saturday night palsy) or in thin elderly patients using crutches. In
addition to weakness of the wrist and hand , the triceps is paralyzed and triceps reflex
is
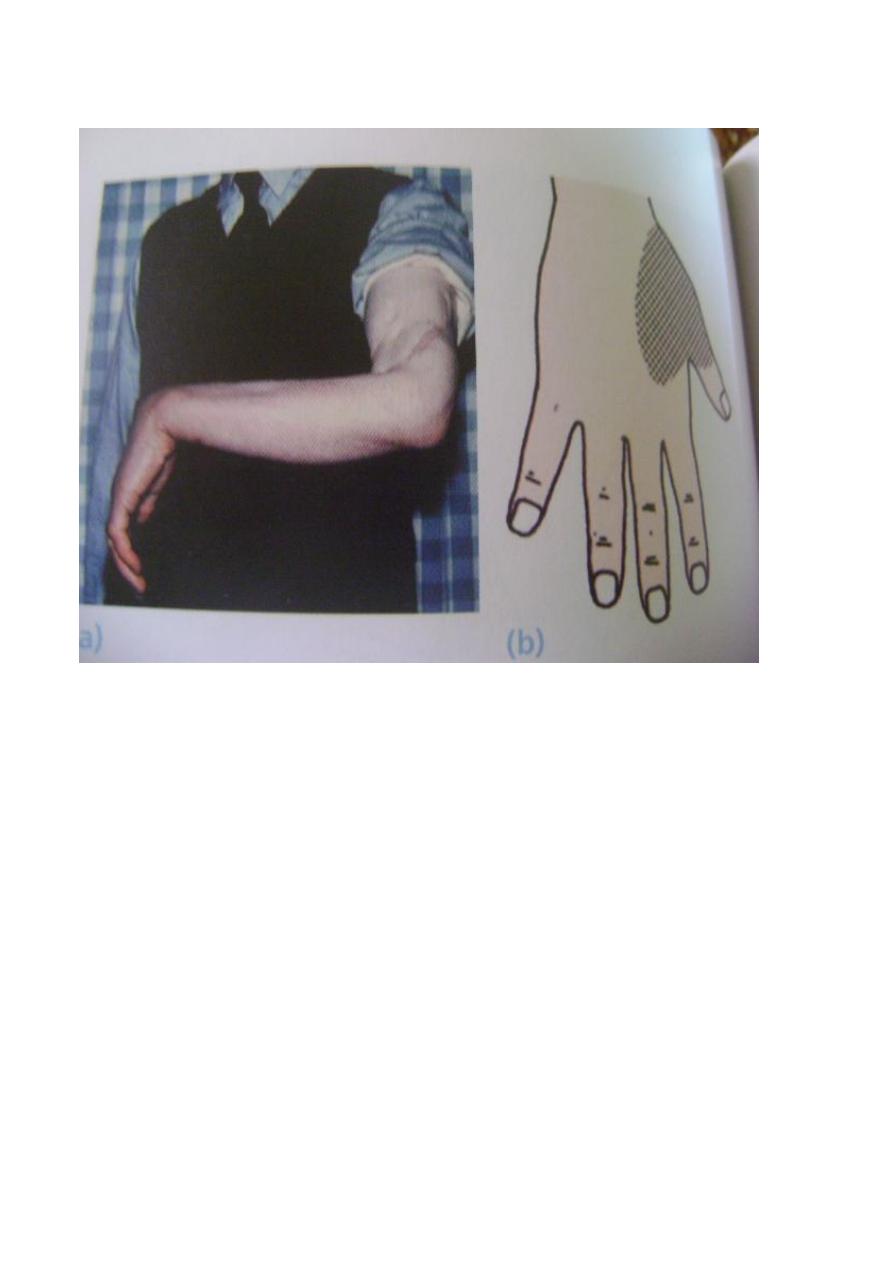
absent.
Treatment
Open injuries should be explored and the nerve is repaired or grafted. Closed injuries
are usually first or second degree lesions , and function eventually returns .
If the palsy is present on admission , one can afford to wait for 6 weeks to see if it
starts to recovers. If it does not , then EMG should be performed , if this show
denervation potentials , then the nerve should explored.
While recovery is awaited , the small joints of the hand must be put through a full
range of passive movements. If recovery does not occur , the disability can be largely
overcome by tendon transverse.
Ulnar nerve
Injuries of the ulnar are usually either near the wrist or near the elbow , although
open wounds may damage it at any level.
Clinical features
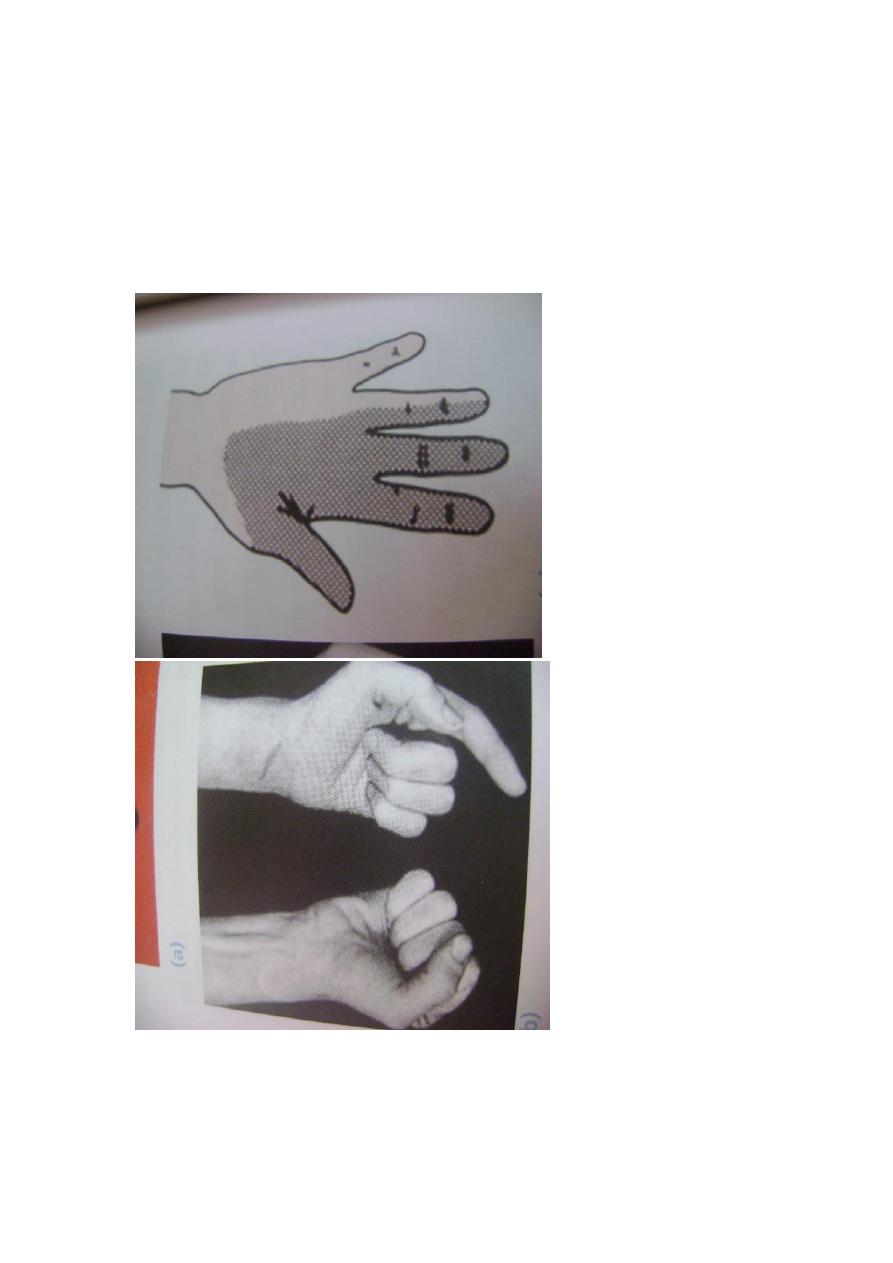
Low lesions are often caused by cuts on shattered glass. There is numbness of the
ulnar one and a half fingers. The hand assumes a typical posture – the claw hand
deformity , with hyperextension of the metacrpophalangeal joinof the ring and little
fingers , due to weakness of the internsic muscles. Hypothenar and interosseous
wasting may be obvious by comparison with normal hand. Fingers abduction is weak
and this , together with loss of thumb addiction , makes pinch difficult. The patient is
asked to grip a sheet of paper forcefully between thumb and index fingers while the
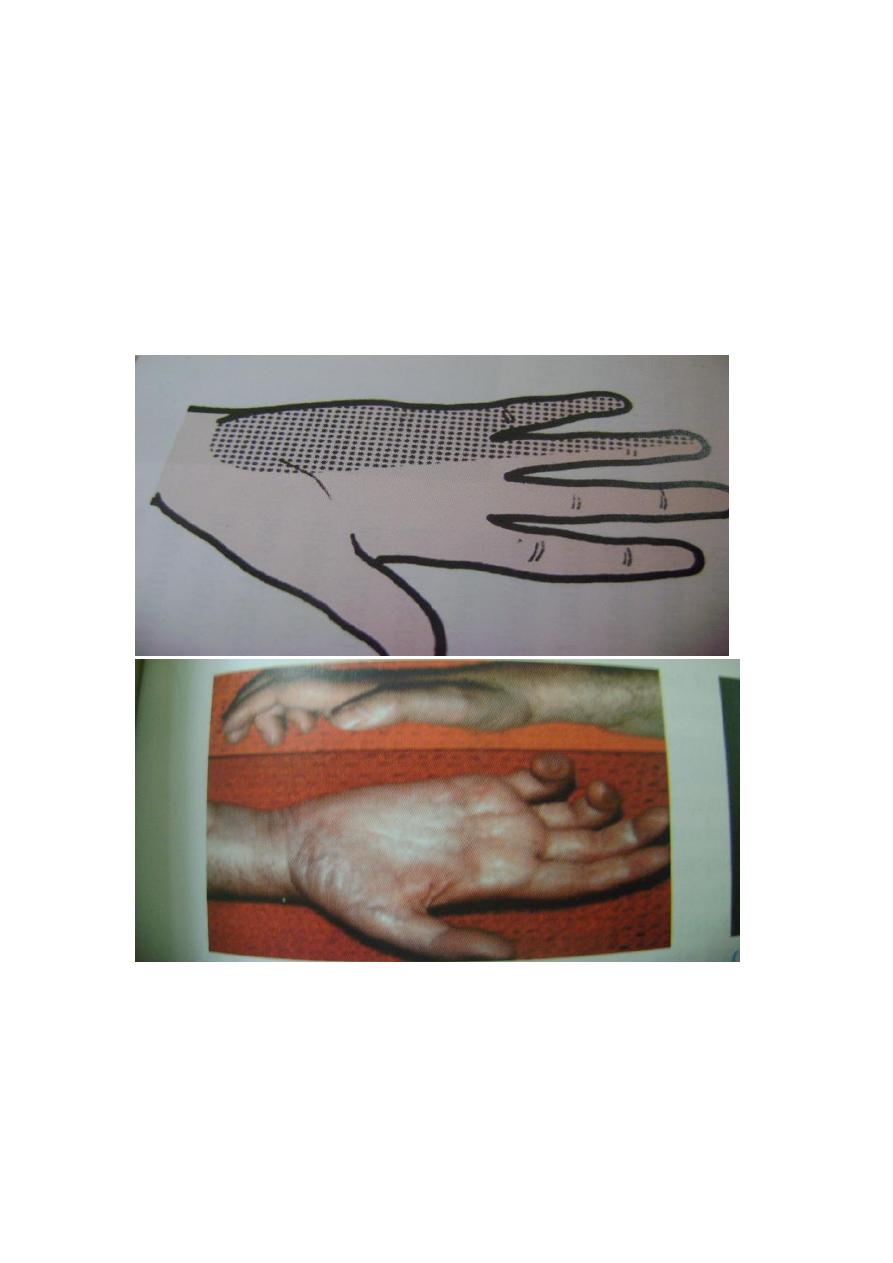
examiner tries to pull it away, there will be powerful flexion of thumb
interphalangeal joint (Forments sign).
High lesions occur with elbow fractures or dislocation . the hand is not markedly
deformed because the ulnar half of flexor digitorum profundus is paralyzed and the
fingers are therefore less clawed , otherwise motor and sensory loss are the same as in
low lesions.
Treatment
Exploration and suturing of a divided nerve , anterior transposition at the elbow
permits closure of gap up to 5cm. while recovery is awaited , the skin should be
protected from burn, passive physiotherapy keeps the hands supple and useful.
If there is no recovery after nerve repair , tendon transfer can be
done
e.
Median nerve
The median nerve is most commonly injured near the wrist or high up in the forearm.
Clinical features
Low lesion may be caused by cuts in front of the wrist or by carpal dislocation .
the patient is unable to abduct the thumb and sensation is lost over the radial three and
a half digit. In long standing cases the thenar eminence is wasted and trophic changes
may be seen.
High lesions are generally due to forearm fractures or elbow dislocation, but stabs
and gunshot wounds may damage the nerve at any level. The signs are the same as
those of low lesions but , in addition the long flexor of the thumb, indexand middle
fingers, the radial wrist flexor and the forearm pronaters muscles are all paralyzed.
Typically , the hand is held with the ulnar fingers flexed and the index straight ( the
pointing sign) . also because the thumb and index flexor are deficient , there is
characteristic pinch defect.
Isolated anterior interosseous nerve lesions are extremely rare . the signs are
similar to those of a high median nerve injury , but without any sensory loss.
.
Treatment
If the nerve is divided , suturing or nerve grafting should always be attempted.
Postoperatively the wrist is splinted in flexion to avoid tension.
Late lesions are sometimes seen, if there has been no recovery , tendon transfer can
be done .

Femoral nerve
The femoral nerve may be injured by gunshot wound , by pressure or traction
during operation or bleeding into the thigh.
Clinical features
Quadriceps action is lacking and the patient is unable to extend the knee actively.
There is numbness of the anterior thigh and medial aspect of the leg. The knee reflex
is depressed.
Treatment
This is a fairly disabling lesion and if possible counter measures should be
undertaken . a thigh hematoma may need to be evacuated . a clean cut of the nerve
may treated successfully by suturing or grafting. The alternative would be a caliper to
stabilize the knee , or tendon transfers of hamstring to quadriceps.
Sciatic nerve
Division of the main sciatic nerve is rare except in gunshot wounds. Traction
lesions may occur with traumatic hip dislocation and with pelvic fractures.
Clinical features
In a complete lesion the hamstrings and all muscles below the knee are paralyzed ,
the ankle jerk is absent. Sensation is lost below the knee , except on the medial side of
the leg which is supplied by saphanous branch of the femoral nerve . the patient walks
with a drop foot and a high stepping gait to avoid dragging the insensate foot on the
ground .
Sometimes only the deep part of the nerve is affected , producing what essentially a
common peroneal palsy. If sensory loss extend into the thigh and the gluteal muscles
are weak , suspect an associated lumbosacral plexus injury.
In late cases the limb is wasted , with trophic ulcers of the foot and fixed deformity
of the foot.
Treatment
If the nerve is known to be divided , suturing or nerve grafting should be attempted
even though it may take more than a year for leg muscles to be reinnervated. While
recovery is awaited , a below – knee drop foot splint is fitted.
The chances of recovery are generally poor at best , will be long delay and
incomplete , partial lesion , in which there is protective sensation of the sole can s.t be
managed by transferring tibialis posterior to the front in order to counteract the drop
foot . the deformities should be corrected if they threaten to cause pressure sores. If
there is no recovery whatever , amputation may be preferable to flail , deformed and
insensitive limb.
Peroneal nerves
Injuries may affect either the common peroneal nerve or one of its branches the deep
or superficial nerves.

Clinical features
The common peroneal nerve is often damaged at the level of the fibular neck by
severe traction when the knee is forced into varus or by pressure from a splint or a
plaster cast , from lying with the leg externally rotated , by skin traction , by
intraneural ganglion or by wounds. The patient has a drop foot and can neither
dorsiflex nor evert the foot . the patient walks with a high stepping gait to avoid
catching the toes. Sensation is lost over the front and outer half of the leg and the
dorsum of the foot . in late c ases pain may be a major feature.
The deep peroneal nerve runs between the muscles of the anterior compartment of
the leg and emerge at the lower border of the extensor retinaculum of the ankle . it
may be threatened in an anterior compartment syndrome. This lead to pain and
weakness of dorsiflexion and sensory loss in a small area of skin between the first and
second toes.
The superfacial peroneal nerve descend along the fibula , innervating the peroneal
muscles and emerging through the deep fascia 5-10 cm above the ankle to supply the
skin over the dorsum of the foot and the medial four toes. The muscular portion may
be involved in lateral compartment syndrome. The patient complains of pain in the
lateral part of the leg and numbness of the foot , there may be weakness of evertion
and sensory loss on the dorsum of the foot
.
Treatment
Direct injuries of the common peroneal nerve and its branches should be explored
and repaired or grafted . while recovery is awaited a splint may be worn to control
ankle weakness . if there is no recovery , the disability can be minimized by tibialis
posterior transfer or by foot stabilization , the alternative is a permanent splint.

Tibial nerves
The tibial nerve is rarely injured except in open wounds. The distal part is
sometimes involved in injuries around the ankle.
Clinical features
The patient is unable to planter-flex the ankle or flex the toes , sensation is abscent
over the sole and part of the calf. Because both the long the long flexor and the
intrinsic muscles are involved, there is no much clawing , with time the calf and foot
become atrophic and pressure ulcers may appear on the sole . fractures and
dislocation around the ankle may injure any of the branches and result picture depend
on the level of the lesion , thus posterior tibial nerve causes wide sensory loss and
clawing of the toes due to paralysis of the intrinsic with active long flexor , but injury
to one of the smaller branches causes only limited sensory loss and less motor
weakness.
Treatment
A complete nerve division should be sutured as soon as possible. While recovery
is awaited, a suitable orthosis is worn to prevent excessive dorsiflexion and the sole is
protected from pressure ulceration. In suitable cases , weakness of planter flexion can
be treated by hindfoot fusion or transfer of the tibialis anterior to the back of the foot .

