Hepatic pathologyLecture 1Dr. Athraa Falah HasanPhD Pathology
ObjectivesAt the end of lecture the students will be know:
1-What the meaning of jaundice and cholestasis.
2-types of jaundice .
3-examples for Hyperbilirubinemia.
4-types of viral hepatitis infection
5-serological markers for hepatitis A infection and for hepatitis B infection
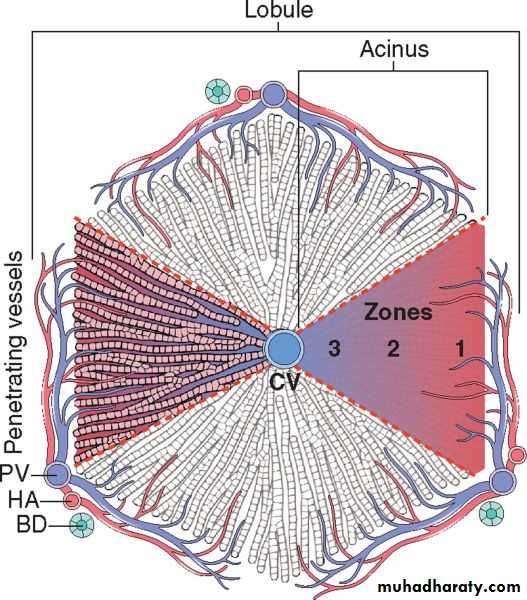
Microscopic anatomy of the liver; the two models, hepatic lobular model and acinar model, are illustrated. In the lobular model the terminal hepatic vein (CV) is at the center of a “lobule,” while the portal tracts (PV) are at the periphery. Pathologists refer to the regions of the parenchyma as “periportal and centrilobular.” In the acinar model, on the basis of blood flow, three zones can be defined, zone 1 being the closest to the blood supply and zone 3 being the farthest. BD, bile duct; HA, hepatic artery
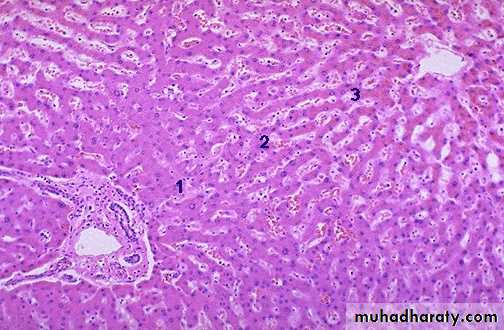
Liver is divided histologically into lobules. The center of the lobule is the central vein. At the periphery of the lobule are portal triads.
Portal triad
Central veinJaundice and Cholestasis
JAUNDICE AND CHOLESTASIS• Alterations of bile formation become clinically evident as yellow discoloration of the skin and sclera (jaundice and icterus, respectively) due to retention of bilirubin, and as cholestasis, characterized by systemic retention of not only bilirubin but also other solutes eliminated in bile.
Pathophysiology of Jaundice
There are two important pathophysiologic differences between the two forms of bilirubin.Unconjugated bilirubin is virtually insoluble in water at physiologic pH and exists in tight complexes with serum albumin.
This form cannot be excreted in the urine even when blood levels are high.
Normally, a very small amount of unconjugated bilirubin is present as an albumin-free anion in plasma.
This fraction of unbound bilirubin may diffuse into tissues, particularly the brain in infants, and produce toxic injury which may cause severe neurologic damage, referred to as kernicterus.
In contrast, conjugated bilirubin is water-soluble, nontoxic, and only loosely bound to albumin, and can be excreted in urine.
Serum bilirubin levels in the normal adult vary between 0.3 and 1.2 mg/dL,
• Jaundice occurs when retention of bilirubin leads to serum levels above 2.5 mg/dl.Jaundice occurs when the equilibrium between bilirubin production and clearance is disturbed by one or more of the following mechanisms :
((1) excessive extrahepatic production of bilirubin ex: Hemolytic anemias, thalassemia
(2) reduced hepatocyte uptake;ex: Some cases of Gilbert syndrome and some drugs
(3) impaired bilirubin conjugation; ex; Physiologic jaundice of the newborn, Breast milk jaundice , Gilbert syndrome, Diffuse hepatocellular disease (e.g., viral or drug-induced hepatitis, cirrhosis)
(4) decreased hepatocellular excretion; ex: Deficiency of canalicular membrane transporters (Dubin-Johnson syndrome, Rotor syndrome)
(5) impaired bile flow.
The first three mechanisms produce unconjugated hyperbilirubinemia, and the latter two produce predominantly conjugated hyperbilirubinemia.
• Neonatal Jaundice (Physiologic jaundice of the newborn)
Because the hepatic machinery for conjugating and excreting bilirubin does not fully mature until about 2 weeks of age, almost every newborn develops transient and mild unconjugated hyperbilirubinemia, termed neonatal jaundice or physiologic jaundice of the newborn.This may be exacerbated by breastfeeding, as a result of the presence of bilirubin-deconjugating enzymes in breast milk
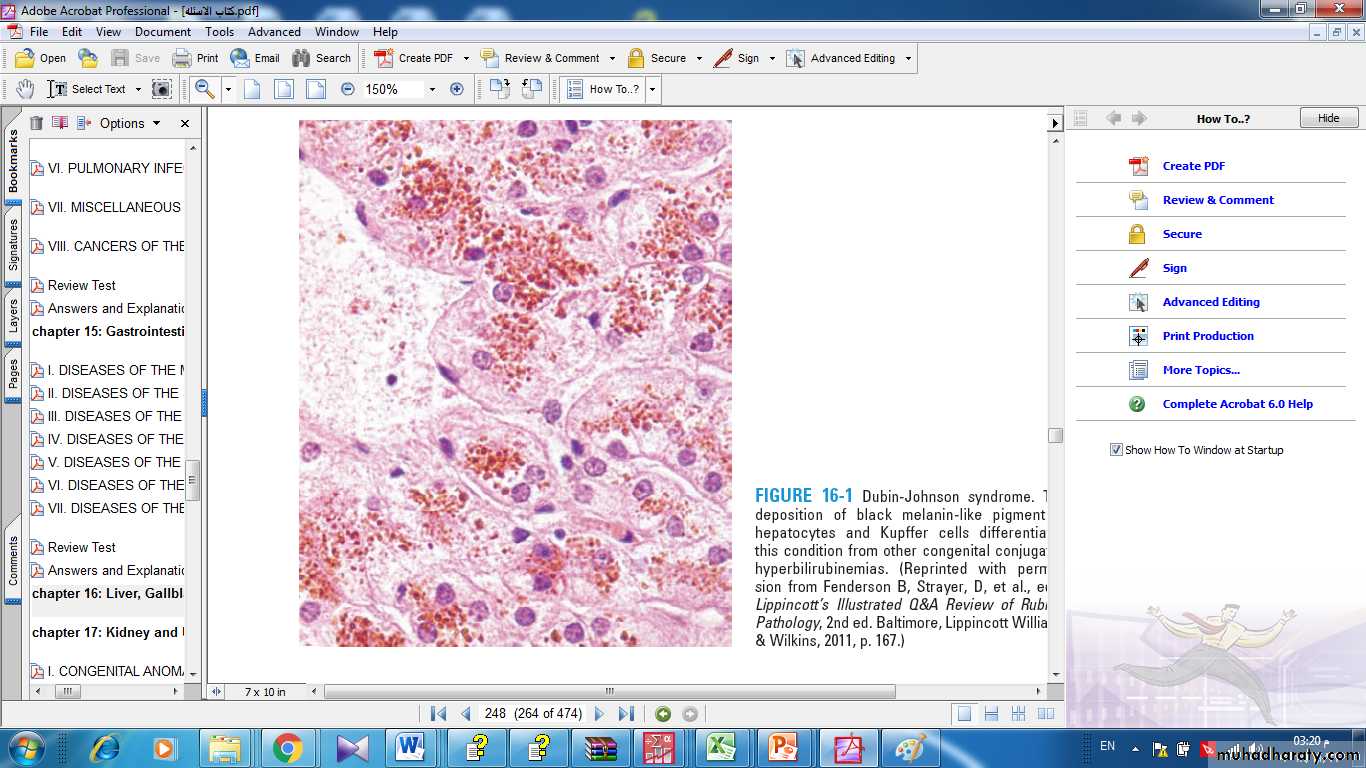
Hereditary Hyperbilirubinemias.
Multiple genetic mutations can cause hereditary hyperbilirubinemia.• Dubin-Johnson syndrome, showing abundant pigment inclusions in otherwise normal hepatocytes
Cholestasis
It is a pathologic condition of impaired bile formation and bile flow, leading to accumulation of bile pigment in the hepatic parenchyma. It can be caused by:-extrahepatic or intrahepatic obstruction of bile channels, or by
-defects in hepatocyte bile secretion.
Patients may have jaundice, pruritus, skin xanthomas (focal accumulation of cholesterol), or symptoms related to intestinal malabsorption, including nutritional deficiencies of the fat-soluble vitamins A, D, or K.
-A characteristic laboratory finding is elevated serum alkaline phosphatase and γ-glutamyl transpeptidase (GGT) enzymes.
Extrahepatic biliary obstruction is frequently amenable to surgical alleviation.
In contrast, intrahepatic cholestasis is not benefited by surgery (short of transplantation), and the patient's condition may be worsened by an operative procedure.
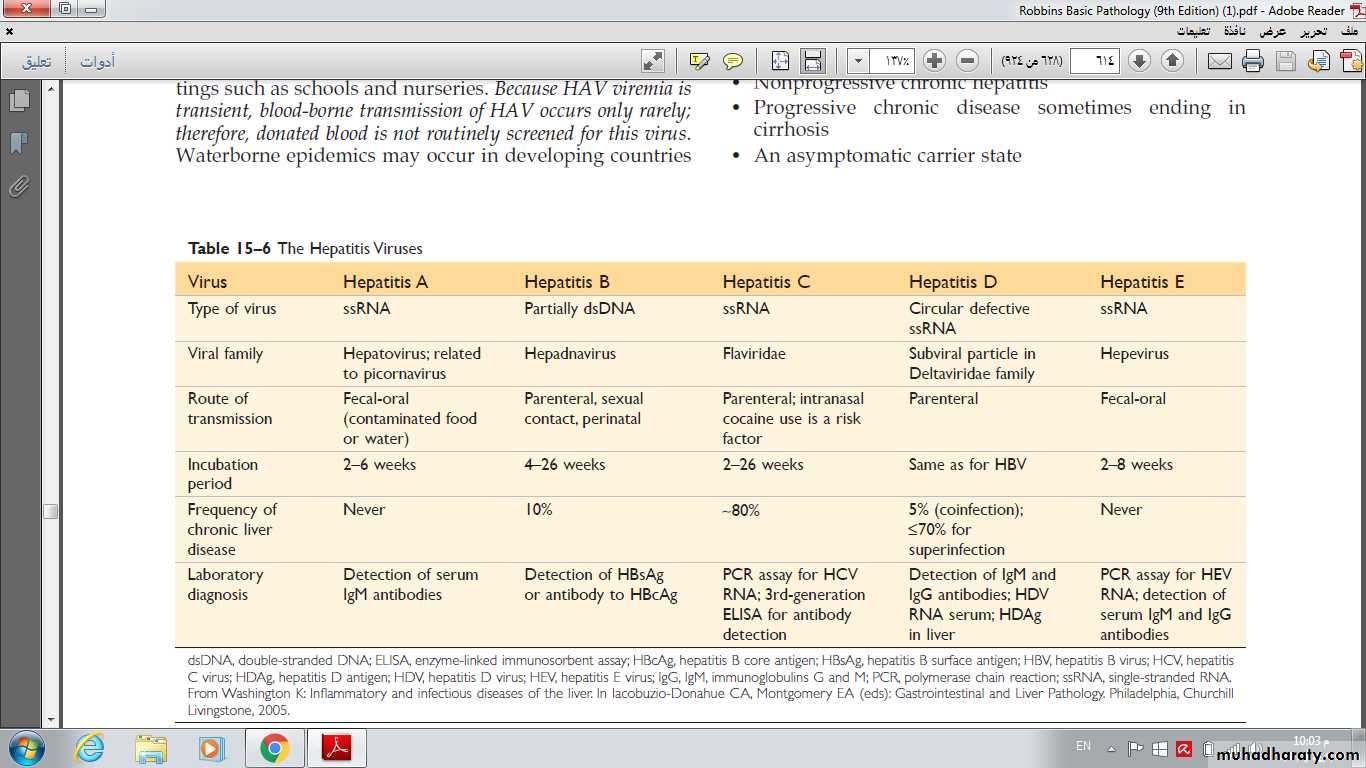
Infectious Disorders of liver VIRAL HEPATITIS Unless otherwise specified, the term viral hepatitis is applied for hepatic infections caused by a group of viruses known as hepatotropic virus (hepatitis viruses A, B, C, D, and E) that have a particular affinity for the liver.
Hepatitis A Virus
Hepatitis A virus (HAV) is a benign, self-limited disease with an incubation period of 2 to 4 weeks.HAV does not cause chronic hepatitis or a carrier state and only rarely causes fulminant hepatitis, so the fatality rate associated with HAV is about 0.1%.
HAV is endemic in countries with substandard hygiene and sanitation, where populations may have detectable antibodies to HAV by the age of 10 years.
Clinical disease tends to be mild or asymptomatic, and is rare after childhood.
Affected individuals have nonspecific symptoms such as fatigue and loss of appetite, and often develop jaundice.Laboratory findings
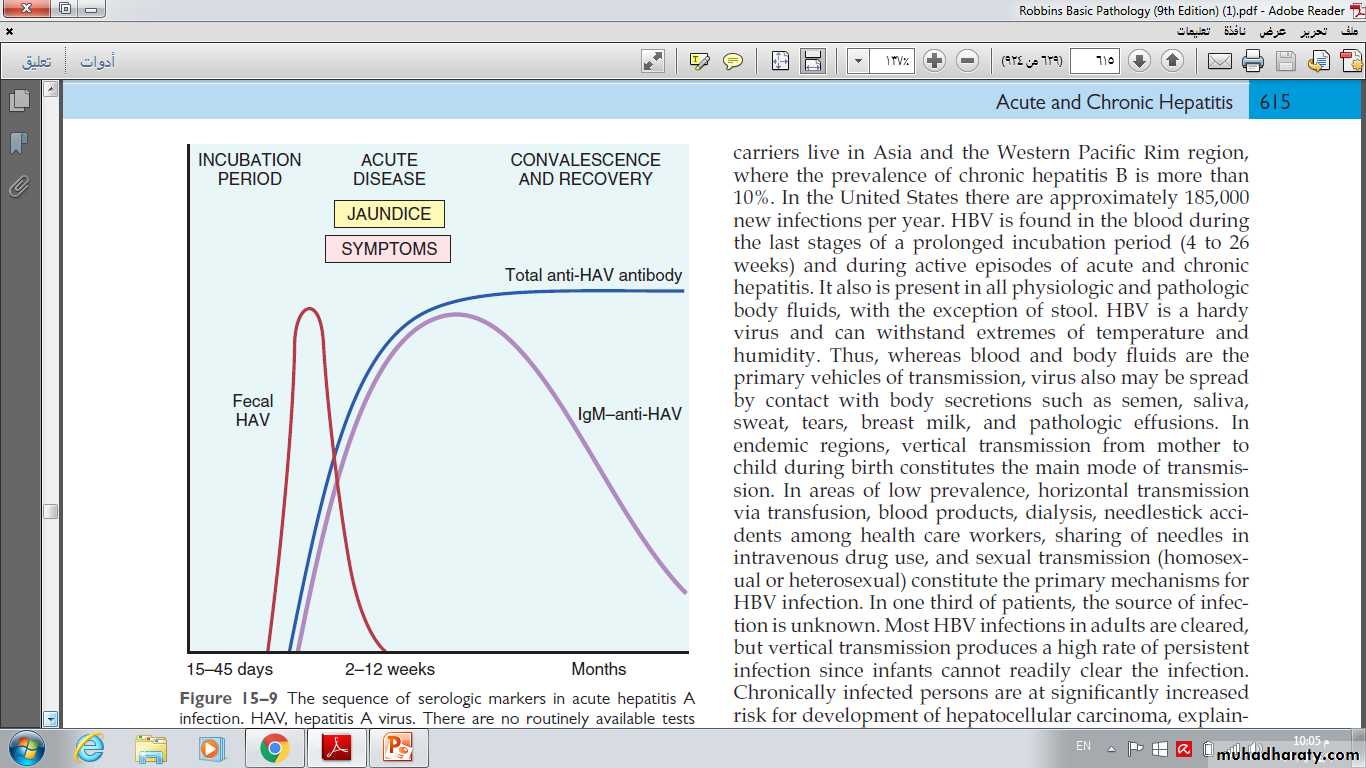
Specific IgM antibody against HAV appears in blood at the onset of symptoms, constituting a reliable marker of acute infection .Fecal shedding of the virus ends as the IgM titer rises.
The IgM response usually begins to decline in a few months and is followed by the appearance of IgG anti-HAV.
The latter persists for years, perhaps conferring lifelong immunity against reinfection by all strains of HAV. However, there are no routinely available tests for IgG anti-HAV.
The presence of this antibody is inferred from the difference between total and IgM anti-HAV.
The sequence of serologic markers in acute hepatitis A infection.
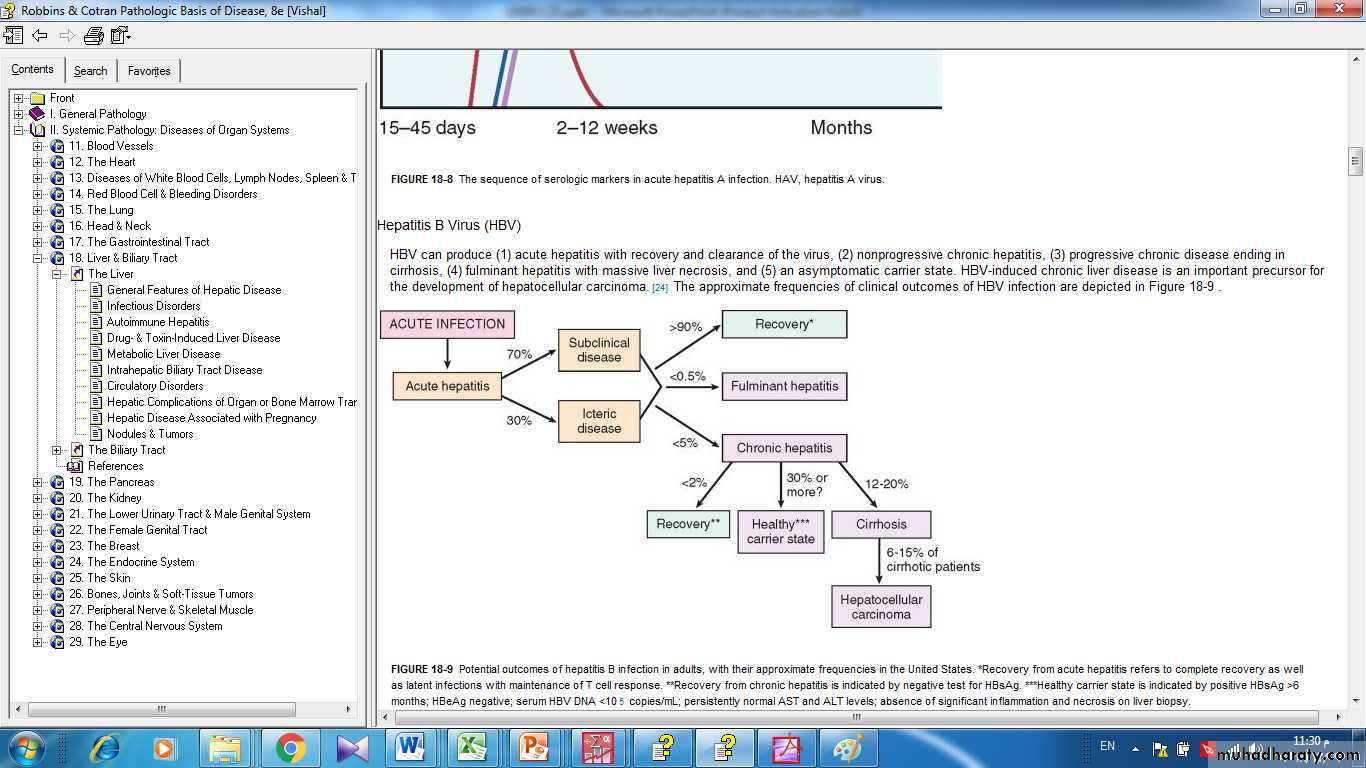
Hepatitis B Virus (HBV)The clinical outcomes of HBV infection are:
(1) acute hepatitis with recovery and clearance of the virus,
(2) nonprogressive chronic hepatitis,
(3) progressive chronic disease ending in cirrhosis,
(4) fulminant hepatitis with massive liver necrosis, and
(5) an asymptomatic carrier state.
HBV-induced chronic liver disease is an important precursor for the development of hepatocellular carcinoma .
The potential outcomes with hepatitis B infection in adults
One third of the world population (2 billion people) have been infected with HBV, and 400 million people have chronic infection.
The carrier rate is largely dictated by the age at infection, being the highest when infection occurs in children perinatally and the lowest when adults are infected.
The mode of transmission of HBV occurs in different ways:
-perinatal transmission during childbirth .-horizontal transmission (through minor cuts and breaks in the skin or mucous membranes among children with close bodily contact),
-unprotected heterosexual or homosexual intercourse and intravenous drug abuse (sharing of needles and syringes) .
The incidence of transfusion-related spread has decreased greatly in recent years due to screening of donated blood .
Approximately 70% have mild or no symptoms and do not develop jaundice. The remaining 30% have nonspecific constitutional symptoms such as anorexia, fever, jaundice, and upper right quadrant pain.
In almost all cases the infection is self-limited and resolves without treatment.
Chronic disease rarely occurs in adults in non-endemic areas.Fulminant hepatitis is also rare.
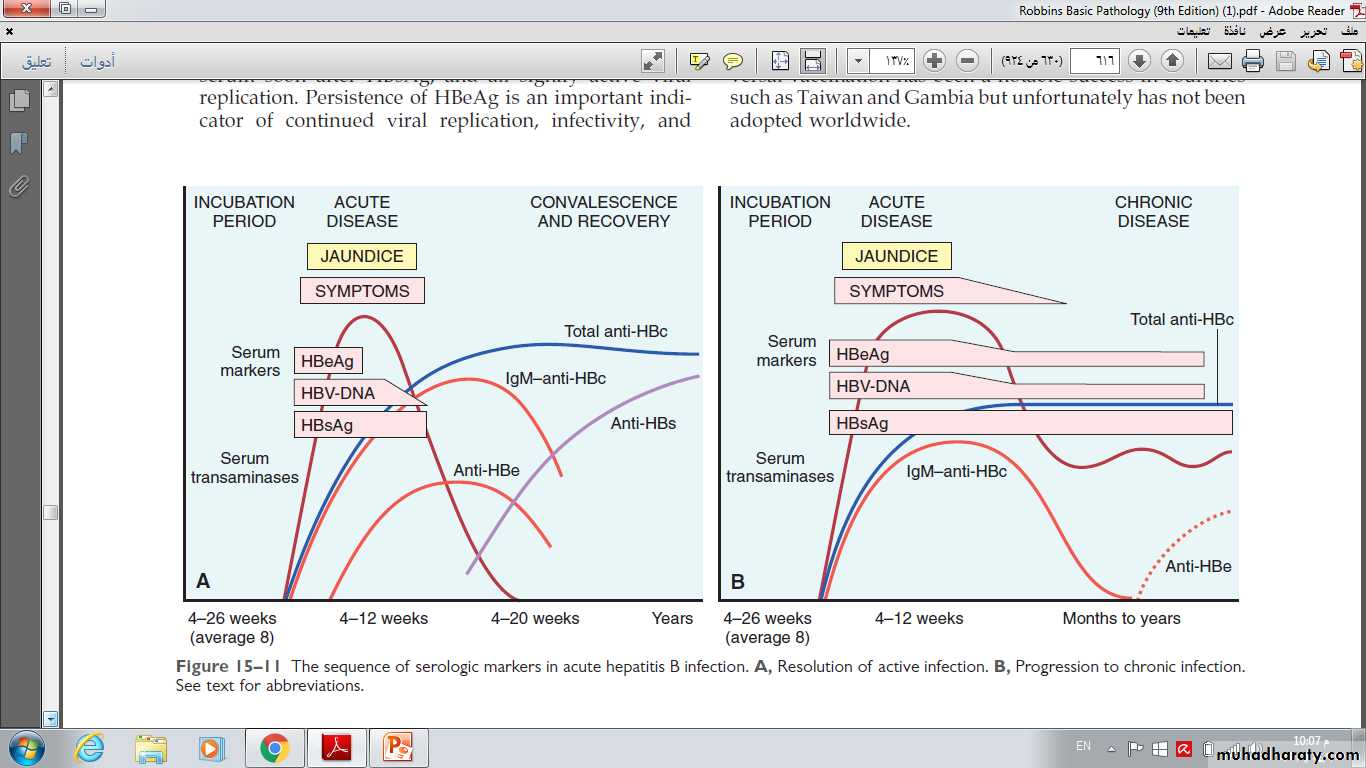
The sequence of serologic markers in acute hepatitis B infection.
A, Resolution of active infection.B, Progression to chronic infection.
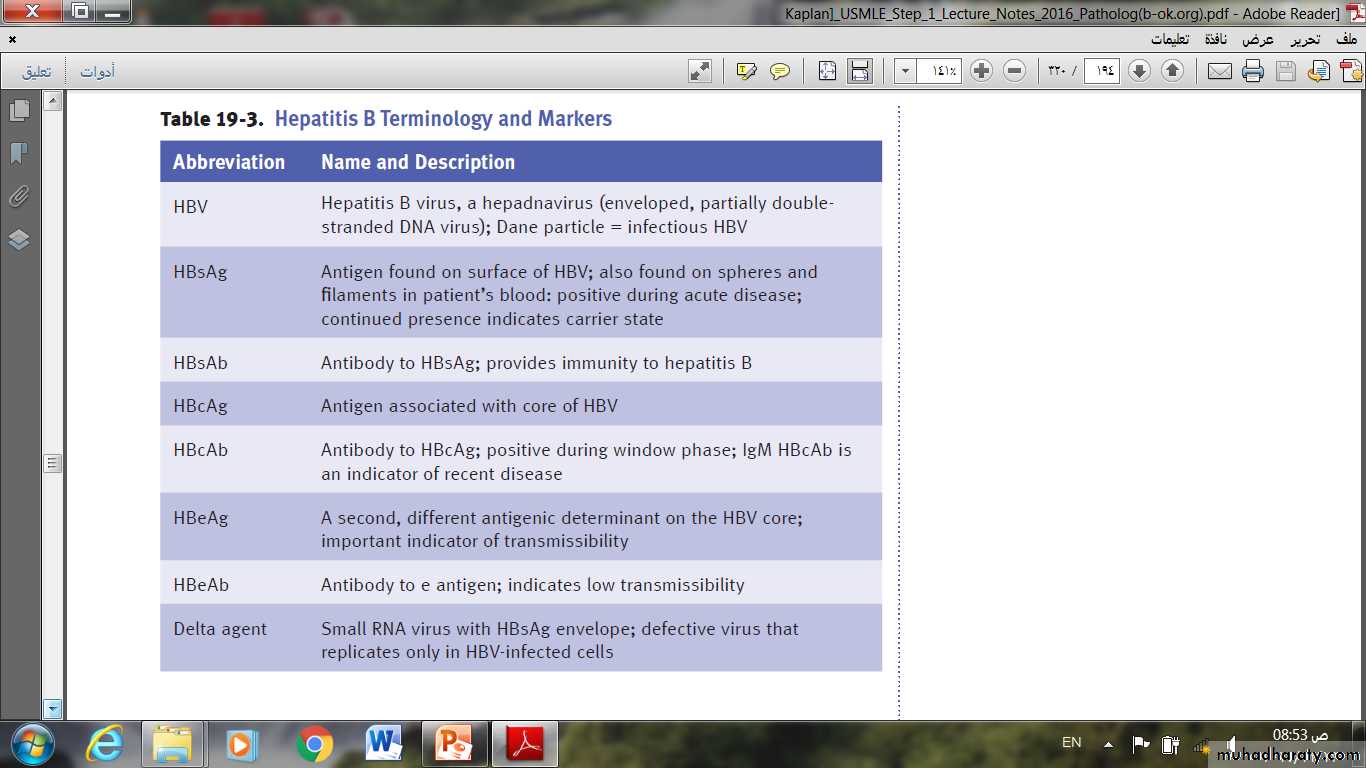
HBsAg appears before the onset of symptoms, peaks during overt disease, and then declines to undetectable levels in 3 to 6 months. (for diagnosis of acute infection)
•Anti-HBs antibody does not rise until the acute disease is over.
• HBeAg, HBV-DNA, and DNA polymerase appear in serum soon after HBsAg, and all signify active viral replication.Persistence of HBeAg is an important indicator of continued viral replication, infectivity, and probable progression to chronic hepatitis.
The appearance of anti-HBe antibodies implies that an acute infection has peaked and is on the wane.
• IgM anti-HBc becomes detectable in serum shortly before the onset of symptoms (for diagnosis of acute infection).Over a period of months the IgM anti-HBc antibody is replaced by IgG anti-HBc.