Hepatic pathologyLecture 2Dr. Athraa Falah HasanPhD Pathology
ObjectivesAt the end of lecture the students will be know:
1-serological markers for hepatitis C, D and E viral infection
2-What the meaning of chronic hepatitis and a carrier state.
3-Morphology of viral hepatitis .
4-Forms of alcoholic liver disease.
5-Pathogenesis and morphology of alcoholic liver disease
Hepatitis C Virus
Hepatitis C virus (HCV) is a major cause of liver disease and it is the most common chronic blood-borne infection.In contrast to HBV, progression to chronic disease occurs in the majority of HCV-infected individuals, and cirrhosis may develop over 5 to 20 years after acute infection in 20% to 30% of patients with persistent infection.
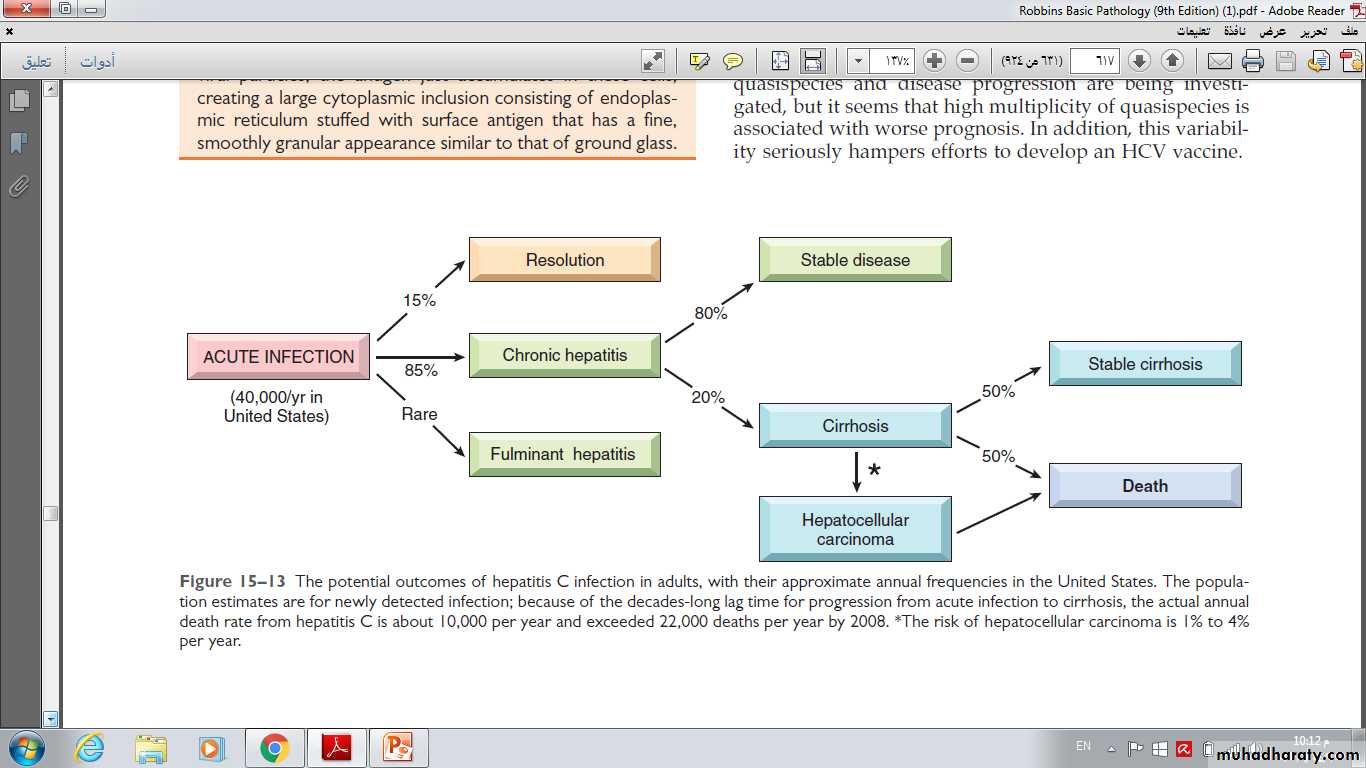
The potential outcomes of hepatitis C infection in adults, with their approximate annual frequencies in the United States.
*The risk of hepatocellular carcinoma is 1% to 4% per year.
The most common risk factors for HCV infection are:
Intravenous drug abuse (common one)
Multiple sex partners
Having had surgery within the last 6 month
Needle stick injury
Multiple contacts with an HCV-infected person
Employment in medical or dental fields (least one)
Unknown (32%)
For children, the major route of infection is perinatal, but is much lower than for HBV (6% vs. 20%).
In about 85% of individuals, the clinical course of the acute infection is asymptomatic and easily missed.
The clinical course of acute HCV hepatitis is milder than that of HBV.
Serologic markers for HCV hepatitis
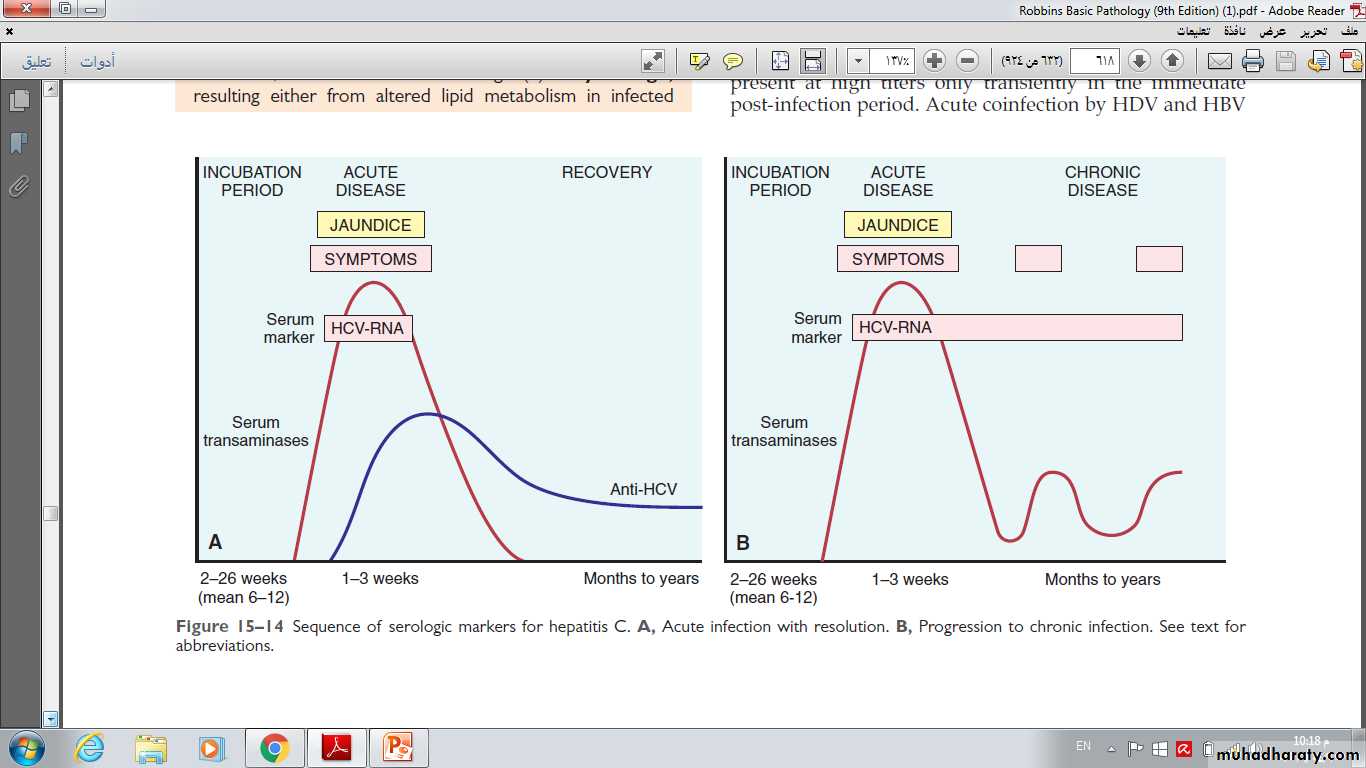
HCV RNA is detectable in blood for 1 to 3 weeks, coincident with elevations in serum transaminases.In symptomatic acute HCV infection, anti-HCV antibodies are detected in only 50% to 70% of patients; in the remaining patients, the anti-HCV antibodies emerge after 3 to 6 weeks.
In chronic HCV infection, circulating HCV RNA persists in many patients despite the presence of neutralizing antibodies, including more than 90% of patients with chronic disease.
A clinical feature that is quite characteristic of chronic HCV infection is episodic elevations in serum aminotransferases, with intervening normal or near-normal periods.
Sequence of serologic markers for hepatitis C.
A, Acute infection with resolution.B, Progression to chronic infection.
Hepatitis D Virus (H Delta virus)
HDV is a unique RNA virus that is dependent for its life cycle on HBV. Infection with HDV arises in the following settings.1- Acute coinfection occurs following exposure to serum containing both HDV and HBV.
2- Superinfection occurs when a chronic carrier of HBV is exposed to a new inoculum of HDV.
Diagnosis.
HDV RNA is detectable in the blood and liver just before and in the early days of acute symptomatic disease.IgM anti-HDV is the most reliable indicator of recent HDV exposure.
Acute co-infection by HDV and HBV is best indicated by detection of both IgM anti HDV and IgM anti HBc (denoting new infection with hepatitis B).
Treatment of HDV infection is limited to IFN-α. Other antiviral agents for HBV have not shown effectiveness. Vaccination for HBV can also prevent HDV infection.
Hepatitis E Virus
Hepatitis E virus (HEV) hepatitis is an enterically trans-mitted, water-borne infection that occurs primarily in young to middle-aged adults; sporadic infection and overt illness in children are rare.HEV is a zoonotic disease with animal reservoirs, such as monkeys, cats, pigs, and dogs.
A characteristic feature of HEV infection is the high mortality rate among pregnant women, approaching 20%.
In most cases the disease is self-limiting; HEV is not associated with chronic liver disease or persistent viremia.
Diagnosis.
Before the onset of clinical illness, HEV RNA and HEV virions can be detected by PCR in stool and serum.
The onset of rising serum aminotransferases, clinical illness, and elevated IgM anti-HEV titers are virtually simultaneous.
Symptoms resolve in 2 to 4 weeks, during which time the IgM is replaced with a persistent IgG anti-HEV titer.
Chronic Hepatitis.
Chronic hepatitis is defined as symptomatic, biochemical, or serologic evidence of continuing or relapsing hepatic disease for more than 6 months.The clinical features of chronic hepatitis are extremely variable.
In some patients the only signs of chronic disease are persistent elevations of serum transaminases.
The most common symptom is fatigue; less common symptoms are malaise, loss of appetite, and occasional bouts of mild jaundice.
Physical findings are few, the most common being spider angiomas, palmar erythema, mild hepatomegaly, hepatic tenderness, and mild splenomegaly, occasionaly vasculitis (subcutaneous or visceral,) and glomerulonephritis.
Laboratory studies may reveal prolongation of the prothrombin time and, in some instances, hyperglobulinemia, hyperbilirubinemia, and mild elevations in alkaline phosphatase levels.
The development of chronic infection after exposure to HBV is an important clinical problem.
Age at the time of infection is the best determinant of chronicity. The younger the age at the time of infection, the higher the probability of chronicity.
Despite progress in the treatment of chronic HBV infection, complete cure is extremely difficult to achieve.
HCV is by far the most common cause of chronic viral hepatitis.
The clinical diagnosis may not be apparent because patients with chronic HCV infection often have mild or no symptoms.However, even patients with normal transaminases are at high risk of developing permanent liver damage.
Therefore, any individual with detectable HCV RNA in the serum needs medical attention.
The Carrier State.
A “carrier” in the case of hepatotropic virus can be interpreted to mean:
(1) individuals who carry one of the viruses but have no liver disease;
(2) those who harbor one of the viruses and have non-progressive liver damage, but are essentially free of symptoms or disability.
In both cases, particularly the latter, these individuals constitute reservoirs for infection.
In the case of HBV infection a “healthy carrier” is often defined as an individual with continuous presence of Hbs Ag ,without HBeAg, but with presence of anti-HBe, normal aminotransferases, low or undetectable serum HBV DNA, and a liver biopsy showing a lack of significant inflammation and necrosis.
In non-endemic areas such as the United States, less than 1% of HBV infections acquired by adults produces a carrier state.
In contrast, HBV infection acquired early in life in endemic areas gives rise to a carrier state in more than 90% of cases.
Morphology of Acute and Chronic Hepatitis.
The morphologic changes in acute and chronic viral hepatitis are shared among the hepatotropic viruses from A to E.A few histologic changes may be indicative of a particular type of virus.
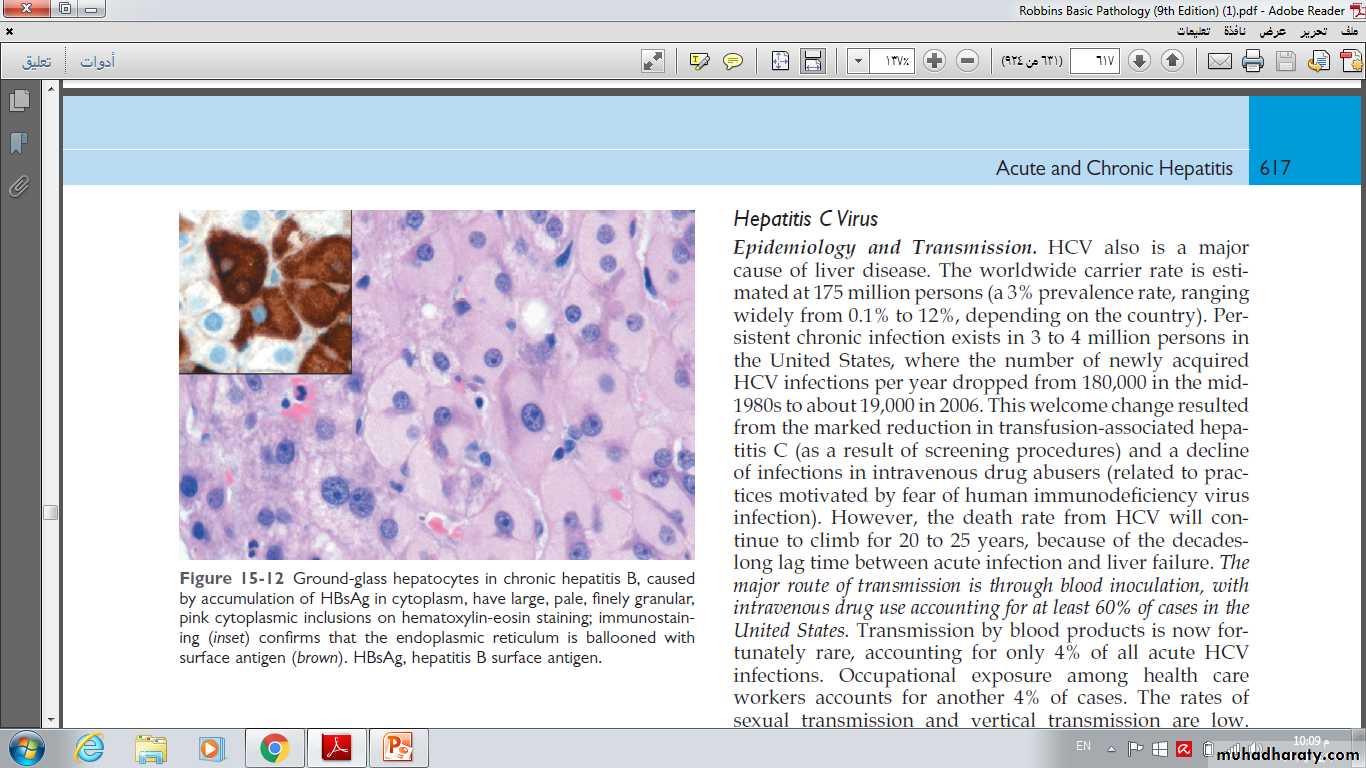
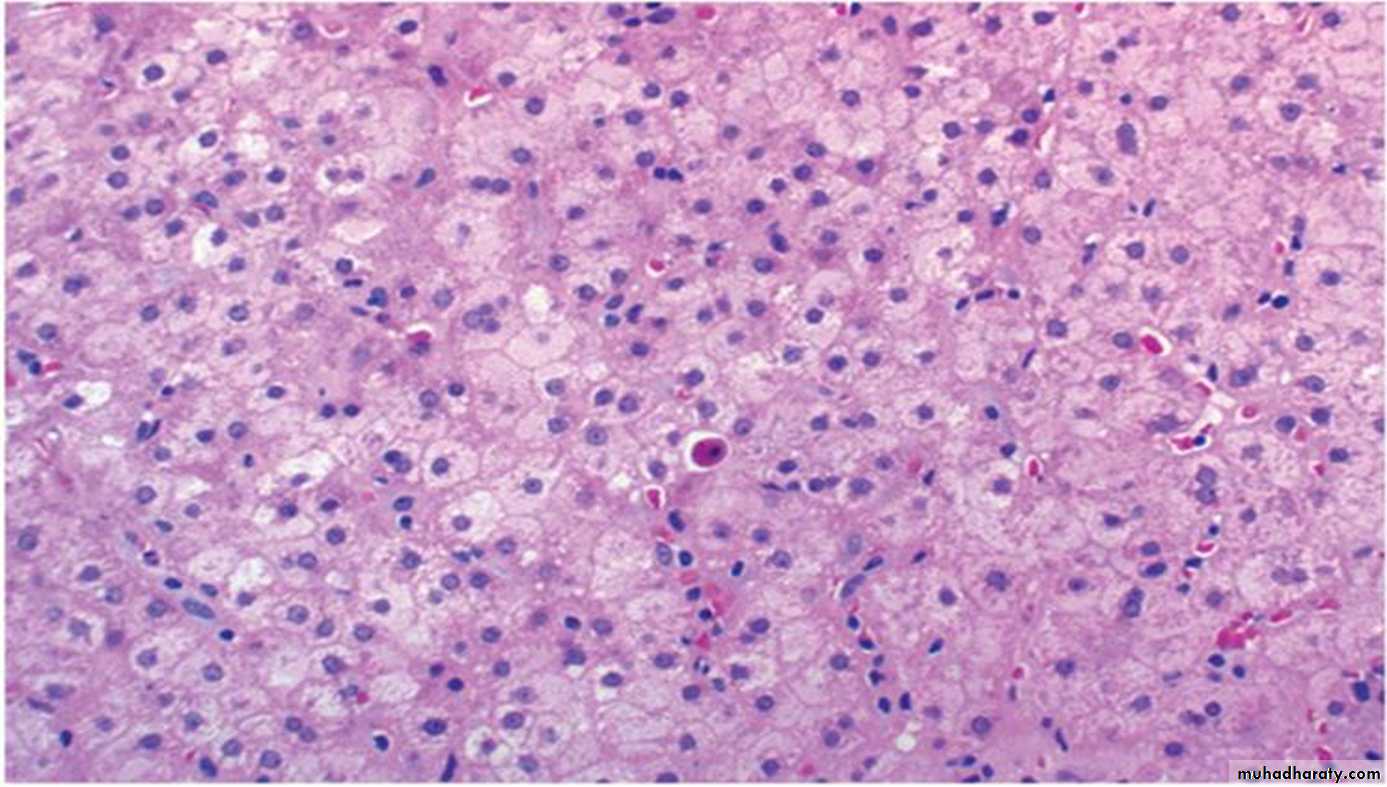
HBV-infected hepatocytes may show a cytoplasm packed with spheres and tubules of HBsAg, producing cell with large, pale, finely granular, pink cytoplasmic inclusions on hematoxylin-eosin staining (“ground-glass hepatocytes”).
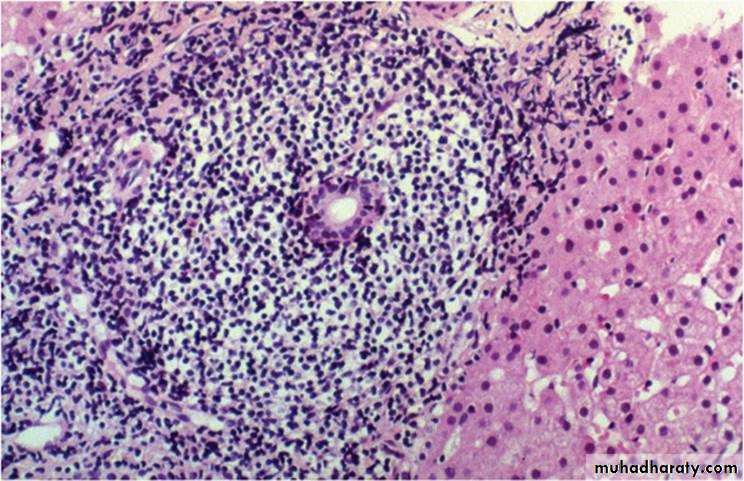
HCV-infected livers frequently show lymphoid aggregates within portal tracts and focal lobular regions of hepatocyte macrovesicular steatosis(fatty change).
Ground-glass hepatocytes in chronic hepatitis B, caused by accumulation of HBsAg in cytoplasm, have large, pale, finely granular, pink cytoplasmic inclusions on hematoxylin-eosin staining; immunostaining (inset) confirms that the endoplasmic reticulum is ballooned with surface antigen (brown).
Ground glass hepatocytes, characterized by more pale, eosinophilic, and homogeneous cytoplasm than surrounding normal (more granular) hepatocytes.
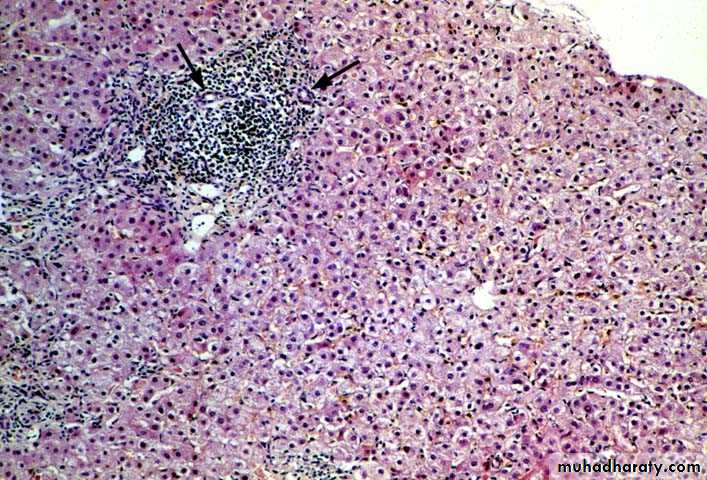
Hepatitis C virus infection with typical lymphoid aggregate formation in portal tracts
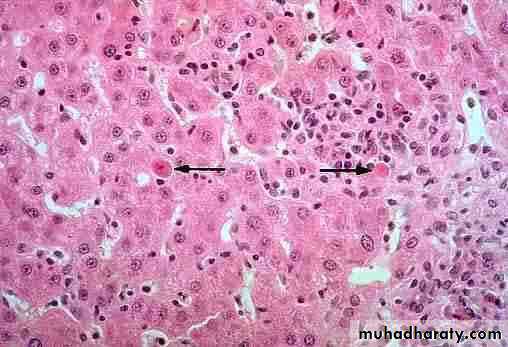
Acute Hepatitis. Hepatocyte injury takes the form of diffuse swelling(ballooning degeneration), so the cytoplasm looks empty and contains only scattered eosinophilic remnants of cytoplasmic organelles.• ballooning of hepatocytes (arrowhead) councilman bodies(arrow)
Several patterns of hepatocyte cell death are seen.-Rupture of the cell membrane leads to cell death and focal loss of hepatocytes, and scavenger macrophage aggregates mark sites of hepatocyte loss.
-Apoptosis, Apoptotic hepatocytes shrink, become intensely eosinophilic, and have fragmented nuclei(councilman bodies)
Councilman” Bodies
-In severe cases of acute hepatitis, confluent necrosis of hepatocytes may lead to bridging necrosis connecting portal-to-portal, central-to-central, or portal-to-central regions of adjacent lobules.Inflammation is a characteristic and usually prominent feature of acute hepatitis.
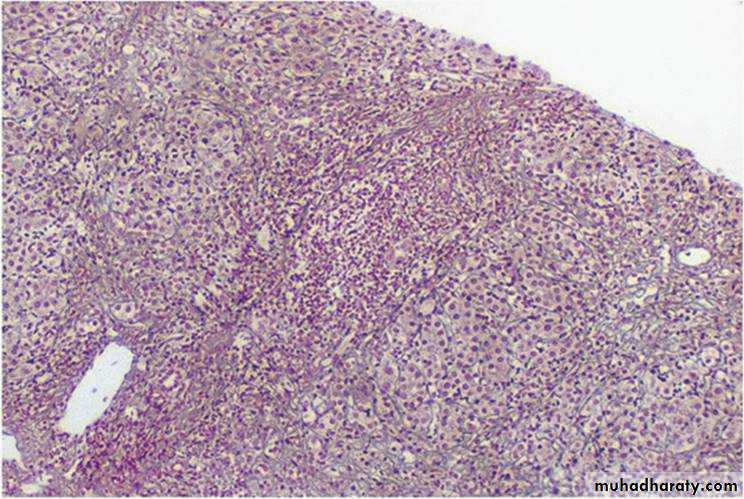
The portal tracts are usually infiltrated with a mixture of inflammatory cells specially mononuclear cells.The inflammatory infiltrate may spill over into the adjacent parenchyma, causing apoptosis of periportal hepatocytes. This is known as interface hepatitis (piecemeal necrosis), which can occur in acute and chronic hepatitis.
This image shows an expanded portal tract (arrowhead) with moderate to marked inflammation and interface hepatitis (piecemeal necrosis)(arrows)
At high power ,mononuclear inflammatory cell infiltrate extends from portal areas and disrupts the limiting plate of hepatocytes which are undergoing necrosis, the so-called "piecemeal" necrosis(interface hepatitis)
Chronic Hepatitis. The histologic features of chronic hepatitis range from exceedingly mild to severe.
In the mildest forms, inflammation is limited to portal tracts and consists of lymphocytes, macrophages, occasional plasma cells, and rare neutrophils or eosinophils.
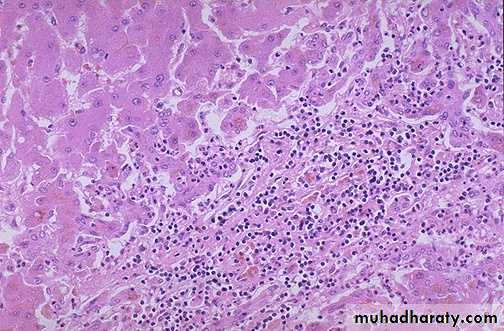
In chronic HCV infection, common findings are lymphoid aggregates and focal mild to moderate fatty change of liver.
In all forms of chronic hepatitis, continued interface hepatitis and bridging necrosis between portal tracts and portal tracts-to-terminal hepatic veins, are harbingers of progressive liver damage.
The hallmark of chronic liver damage is the deposition of fibrous tissue.
At first, only portal tracts show increased fibrosis, but with time periportal septal fibrosis occurs, followed by linking of fibrous septa (bridging fibrosis), especially between portal tracts.Continued loss of hepatocytes and fibrosis results in cirrhosis.
chronic hepatitis, portal tract inflammation appears, but the lobular changes persist. There continues to be lobular disarray, However, despite the presence of portal inflammation, there is no significant bile duct infiltration or damage(arrow).
Alcoholic liver disease
- Alcohol is a direct hepatotoxic agent.-15% of alcoholics can be expected to develop cirrhosis.
-The amount of alcohol necessary to produce chronic liver disease is about 80g/day.
-Women are more susceptible to alcoholic liver damage than men.
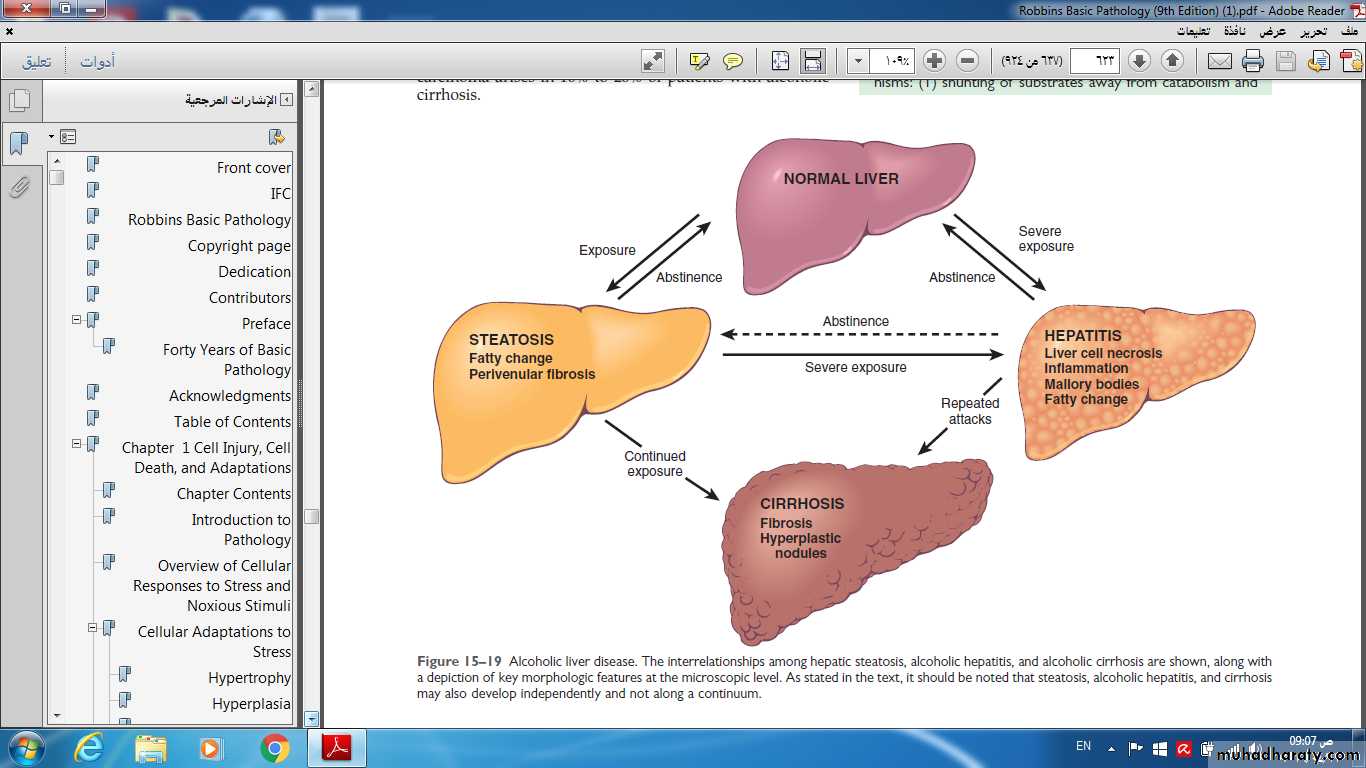
Alcoholic liver disease:
There are three distinctive, overlapping, forms of alcoholic liver disease:A) Fatty liver.
B) Alcoholic hepatitis.
C) Cirrhosis.
Alcoholic liver disease. The interrelationships among hepatic steatosis, alcoholic hepatitis, and alcoholic cirrhosis are shown, along with a depiction of key morphologic features at the microscopic level. As stated in the text, it should be noted that steatosis, alcoholic hepatitis, and cirrhosis may also develop independently and not along a continuum.
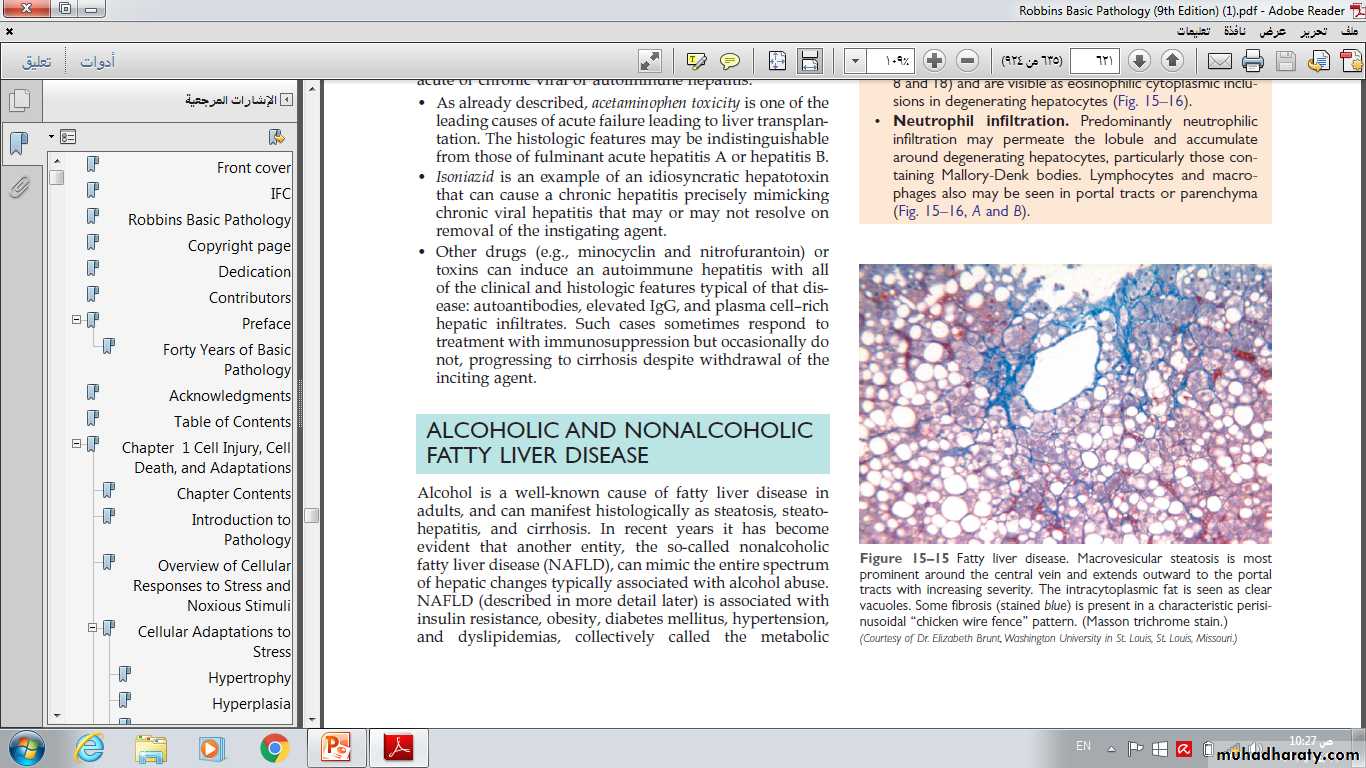
• Fatty Liver:
Morphology.Hepatic Steatosis (Fatty Liver). After even moderate intake of alcohol, microvesicular lipid droplets accumulate in hepatocytes. With chronic intake of alcohol, lipid accumulates creating large, clear macrovesicular globules that compress and displace the hepatocyte nucleus to the periphery of the cell.
Macroscopically, the fatty liver of chronic alcoholism is a large (as heavy as 4 to 6 kg), soft organ that is yellow and greasy. The fatty change is completely reversible if the person will stop alcohol intake.
Fatty liver disease. Macrovesicular steatosis is most Prominent around the central vein and extends outward to the portal tracts with increasing severity. The intracytoplasmic fat is seen as clear vacuoles. Some fibrosis (stained blue) is present in a characteristic perisinusoidal “chicken wire fence” pattern. (Masson trichrome stain.)
Pathgenesis
(1) Alcohol increases fatty synthesis as a result of generation of excess reduced nicotinamide adenine dinucleotide (NADH + H+) by the two major enzymes , alcohol dehydrogenase and acetaldehyde dehydrogenase.(2) impaired assembly and secretion of lipoproteins.
(3) increased peripheral catabolism of fat.
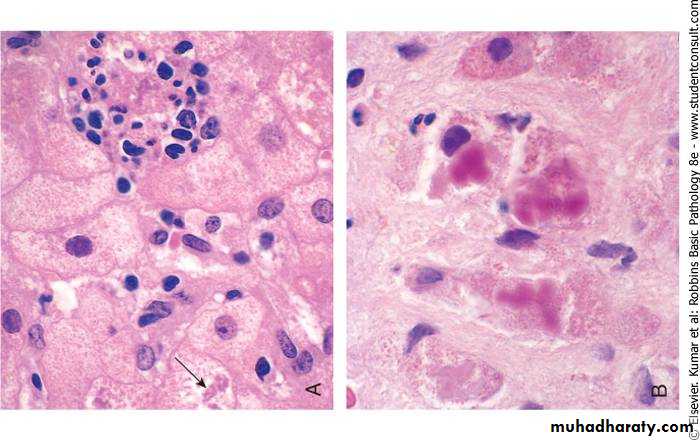
B) Alcoholic hepatitis:
It is an acute inflammation, characterized by
1-Hepatocyte swelling and necrosis: Single or scattered foci of cells undergo swelling (ballooning) and necrosis. The swelling results from the accumulation of fat ,water and proteins that normally are exported.
2-Mallory bodies: which are visible as eosinophilic cytoplasmic clumps in hepatocytes.
This bodies result from accumulation of cytokeratin in complex with other proteins inside scattered hepatocytes.
These inclusions are a characteristic but not specific feature of alcoholic liver disease.
3-Neutrophilic reaction: Neutrophils accumulate around degenerating hepatocytes, particularly those having Mallory bodies.
4-Fibrosis: Alcoholic hepatitis is almost always accompanied by prominent activation of sinusoidal stellate cells and portal tract fibroblasts, giving rise to fibrosis.
Alcoholic hepatitis: inflammation and Mallory bodies
Pathogenesis:
The causes of alcoholic hepatitis are uncertain, but some of the factors in its pathogenesis are:- Acetaldehyde induces lipid peroxidation and acetaldehyde-protein adduct formation, which may disrupt cytoskeleton and membrane function.
-Cytochrome P-450 metabolism produces reactive oxygen species (ROS) that react with cellular proteins, damage membranes, and alter hepatocellular function.
• -TNF is considered to be the main effector of injury; IL-1, IL-6, and IL 8 may also contribute.
Clinical features:
Patients present with acute symptoms: right upper quadrant pain, anorexia, fever and jaundice.
Serum enzymes are abnormal and the white count may reach 25000. Mortality rate can reach up to 20%.
C) Alcoholic cirrhosis:
Fatty liver and alcoholic hepatitis may lead to cirrhosis in about 15% of alcoholics.The term denotes the formation of fibrous septa surrounding hepatocellular nodules.
Alcoholic cirrhosis is one of the most common causes for liver transplantation, since it is usually considered as end stage liver disease.
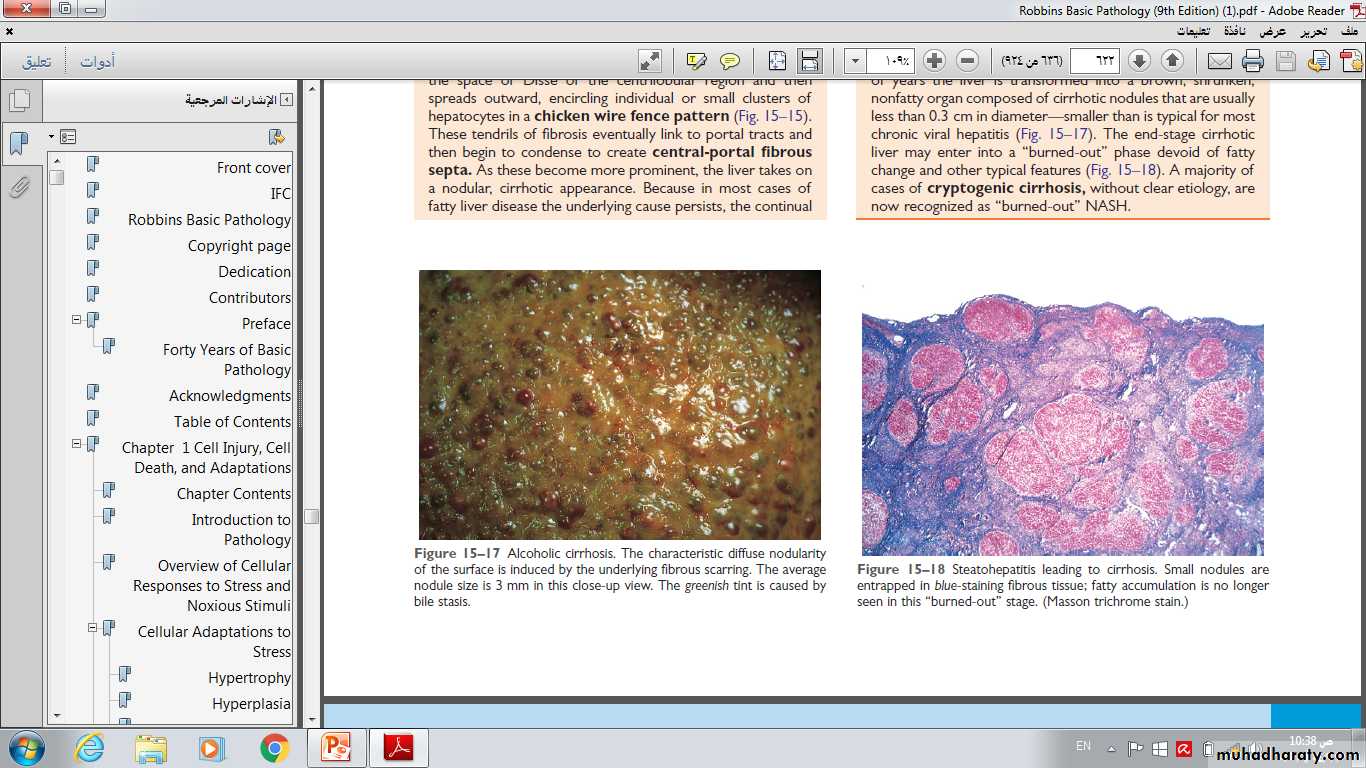
Alcoholic cirrhosis. The characteristic diffuse nodularity of the surface is induced by the underlying fibrous scarring. The average nodule size is 3 mm in this close-up view. The greenish tint is caused by
bile stasis.