By
Dr.Salah Aljanaby
Ass. Prof
General and Laparoscopic Surgeon
Lecture 2
thyroid gland
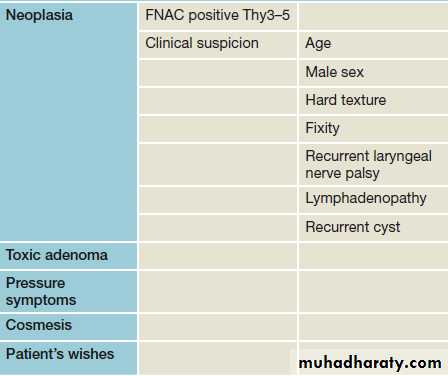
Indications for operation in thyroid swellings.
Colloid goitre
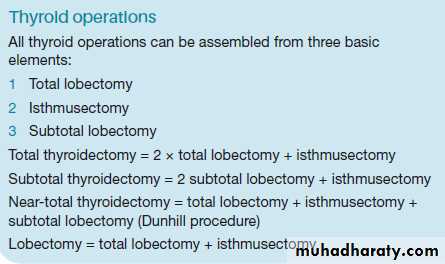
Selection of thyroid procedure
The choice of thyroid operation depends on:●● diagnosis (if known preoperatively);
●● risk of thyroid failure;
●● risk of RLN injury;
●● risk of recurrence;
●● Graves’ disease;
●● multinodular goitre;
●● differentiated thyroid cancer;
●● risk of hypoparathyroidism.
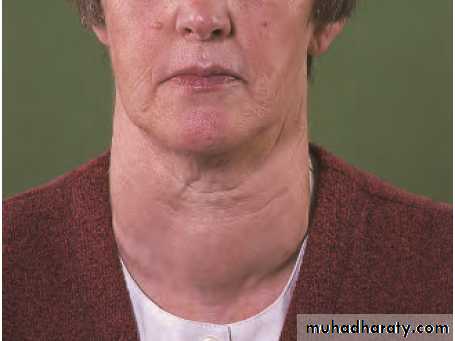
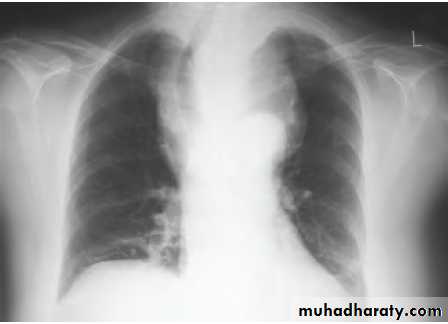
Retrosternal goitre
Arise from the slow growth of a multinodular gland down in to the mediastinum.As the gland enlarges within the thoracic inlet, pressure may lead to dysphagia, tracheal compression and eventually airway
symptoms.
Patient should be considered for surgery if there is significant airway compression
HYPERTHYROIDISM
Thyrotoxicosissymptoms due to a raised level of circulating thyroid hormones, is not responsible for all manifestations of the disease.
Clinical types are:
●● diffuse toxic goitre (Graves’ disease);
●● toxic nodular goitre;
●● toxic nodule;
●● hyperthyroidism due to rarer causes.
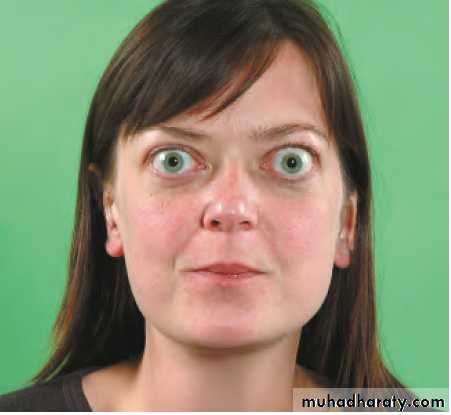
Clinical features
The symptoms are:• tiredness
• emotional lability
• heat intolerance
• weight loss
• excessive appetite
• palpitations.
The signs of thyrotoxicosis are:
• tachycardia
• hot, moist palms
• exophthalmos
• eyelid lag/retraction
• agitation
• thyroid goitre and bruit.
Diffuse toxic goitre
diffuse vascular goitre appearing at the same time as hyperthyroidism,
usually occurs in younger women
frequently associated with eye signs.
The syndrome is that of primary thyrotoxicosis
50% of patients have a family history of autoimmune endocrine diseases.
Toxic nodular goitre
A simple nodular goitre is present for a long time before the hyperthyroidismusually in the middle-aged or elderly
very infrequently is associated with eye signs.
The syndrome is that of secondary thyrotoxicosis.
Toxic nodule
solitary overactive nodule, which may be part of a generalised nodularity or a true toxic adenoma.It is autonomous and its hypertrophy and hyperplasia are not due to TSH-RAb.
TSH secretion is suppressed by the high level of circulating thyroid hormones and the normal thyroid tissue surrounding the nodule is itself suppressed and inactive.
Graves’ disease.
Principles of treatment of thyrotoxicosis
Non-specific measures are rest and sedationspecific measures, i.e. the use of antithyroid drugs, surgery and radioiodine.
ANTITHYROID DRUGS
Those in common use are carbimazole and propylthiouracil.used to restore the patient to a euthyroid state and to maintain this for a prolonged period in the hope that a permanent remission will occur, i.e. that production of thyroid-stimulating antibodies (TSH-RAb) will diminish or cease.
Antithyroid drugs cannot cure a toxic nodule.
●● Advantages.
No surgery
no use of radioactive materials.
●● Disadvantages.
Treatment is prolonged
failure rate is at least 50%.
The duration of treatment may be tailored to the severity of the toxicity, with milder cases
being treated for only 6 months and severe cases for 2 years before stopping therapy.
SURGERY
In diffuse toxic goitre and toxic nodular goitre with overactive internodular tissue, surgery cures by reducing the mass of overactive tissue by reducing the thyroid below a criticalmass.
Advantages.
The goitre is removed
the cure is rapid and the cure rate is high if surgery has been adequate.
Disadvantages.
Recurrence of thyrotoxicosis occurs in at least 5% of cases when subtotal thyroidectomy is carried out.
There is a risk of permanent hypoparathyroidism and nerve injury.
Young women tend to have a poorer cosmetic result from the scar.
Every operation carries a risk, but with suitable preparation and an experienced surgeon the mortality is negligible and the morbidity low.
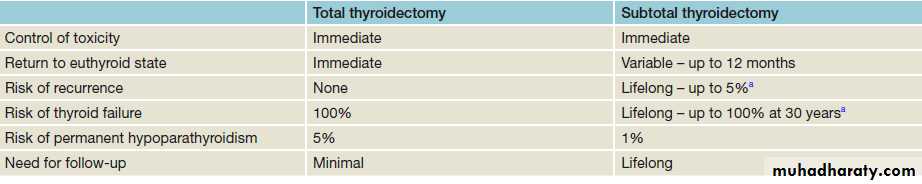
Comparison of surgical options for Graves’ disease.
RADIOIODINE
Radioiodine destroys thyroid cells and, as in thyroidectomy, reduces the mass of functioning thyroid tissue to below a critical level.●● Advantages.
No surgery
no prolonged drug therapy.
●● Disadvantages.
Isotope facilities must be available.
The patient must be quarantined while radiation levels are high and avoid pregnancy and close physical contact, particularly with children.
Eye signs may be aggravated.
Choice of therapy
Each case must be considered individually.guiding principles on the most satisfactory treatment for a particular toxic goitre at a particular age be modified according to the facilities available and the personality and wishes of the individual patient, business or family commitments and any other coexistent medical or surgical condition. Access to post-treatment care and availability of replacement thyroxine can be important considerations in resource-poor countries.
In advising treatment, compliance, influenced by social and intellectual factors, is important; many patients cannot be trusted to take drugs regularly if they feel well, and indefinite follow-up, which is essential after radioiodine or subtotal thyroidectomy is a burden for all.
DIFFUSE TOXIC GOITRE
Most patients have an initial course of antithyroid drugs with radioiodine for relapse. Exceptions are those who refuse radiation, have large goitres, progressive eye signs or are pregnant.
TOXIC NODULAR GOITRE
Toxic nodular goitre is often large and uncomfortable and enlarges still further with antithyroid drugs. A large goitre should be treated surgically because it does not respond as well or as rapidly to radioiodine or antithyroid drugs as does a diffuse toxic goitre.
TOXIC NODULE
Surgery or radioiodine treatment is appropriate.
Radioiodine is a good alternative for patients over the age of 45 years because the suppressed thyroid tissue does not take up iodine and thus there is minimal risk of delayed thyroid insufficiency.
FAILURE OF PREVIOUS TREATMENT WITH ANTITHYROID DRUGS OR RADIOIODINE
In this case, surgery or thyroid ablation with 123I is appropriate.
Surgery for thyrotoxicosis
Preoperative preparationaims to make the patient biochemically euthyroid at operation.
Preparation is as an out-patient and only rarely is admission to hospital necessary on account of severe symptoms at presentation, failure to control the hyperthyroidism or non-compliance with medication.
Carbimazole 30–40 mg per day is the drug of choice for
preparation.When euthyroid (after 8–12 weeks), the dose may be reduced to 5 mg 8-hourly or a ‘block and replace’ regime used. In this case, the high dose of carbimazole is continued to inhibit T3 and T4 production and a maintenance dose of 0.1–0.15 mg of thyroxine is given daily. The last dose of carbimazole may be given on the evening before surgery.
Iodides are not used alone because, if the patient needs preoperative treatment, a more effective drug should be given.
An alternative method of preparation is to abolish the clinical manifestations of the toxic state, using β-adrenergic blocking drugs.
These act on the target organs and not on the gland itself. Propranolol also inhibits the peripheral conversion of T4 to T3.
The appropriate dosages are propranolol 40 mg t.d.s. or the longer acting nadolol 160 mg once daily.
Clinical response to β-blockade is rapid and the patient may be rendered clinically euthyroid and operation arranged in a few days rather than weeks.
β-adrenergic blocking drugs do not interfere with synthesis of thyroid hormones, and hormone levels remain high during treatment and for some days after thyroidectomy. It is, therefore, important to continue treatment for 7 days postoperatively.
Iodine may be given with carbimazole or a β-adrenergic blocking drug for 10 days before operation.
Iodide alone produces a transient remission and may reduce vascularity.
POSTOPERATIVE COMPLICATIONS
Haemorrhageis the most frequent life-threatening complication of thyroidectomy
Around 1 in 50 patients will develop a haematoma, and in almost all cases this will develop in the first 24 hours. If an arterial bleed occurs, the tension in the central compartment pressure can rise until it exceeds venous pressure. Venous oedema of the larynx can then develop and cause airway obstruction leading to death.
If a haematoma develops, clinical staff should know to remove skin sutures in order to release some pressure and seek senior advice immediately.
Endotracheal intubation should be used to secure the airway while the haematoma is evacuated and the bleeding point controlled.
2. Recurrent laryngeal nerve paralysis and voice change
RLN injury may be unilateral or bilateral, transient or permanent.Injury to the external branch of the superior laryngeal nerve is more common because of its proximity to the superior thyroid artery. This leads to loss of tension in the vocal cord with diminished power and range in the voice. Patients, particularly those who use their voice professionally, must be advised that any thyroid operation will result in change to the voice even in the absence of nerve trauma.
3.Thyroid insufficiency
Following total thyroidectomy, clearly thyroxine replacement will be required.Around one in three patients who has a lobectomy will require supplementation; rates are higher in those with thyroid autoantibodies.
Subtotal thyroidectomy was at one time performed with the aim of leaving sufficient tissue to maintain thyroid function.
4.Parathyroid insufficiency
This is due to removal of the parathyroid glands or infarction through damage to the parathyroid end arteries; The incidence of permanent hypoparathyroidism should be less than 1% and most cases present dramatically
2–5 days after operation but, very rarely, the onset is delayed for 2–3 weeks or a patient with marked hypocalcaemia may be asymptomatic. The complication is limited to total thyroidectomy,
as when lobectomy is performed the contralateral parathyroid glands are sufficient to maintain calcium levels.
5,Thyrotoxic crisis (storm)
. acute exacerbation of hyperthyroidism.. occurs if a thyrotoxic patient has been inadequately prepared for thyroidectomy and is now extremely rare.
Very rarely, a thyrotoxic patient presents in a crisis and this may follow an unrelated operation.
Symptomatic and supportive treatment is for dehydration, hyperpyrexia and restlessness. This requires the administration of intravenous fluids, cooling the patient with ice packs, administration of oxygen, diuretics for cardiac failure, digoxin for uncontrolled atrial fibrillation, sedation and intravenous hydrocortisone.
Specific treatment is by carbimazole 10–20 mg 6-hourly, Lugol’s iodine 10 drops 8-hourly by mouth or sodium iodide 1g i.v. Propranolol intravenously (1–2 mg) or orally (40 mg 6-hourly) will block β-adrenergic effects.
6.Wound infection
Cellulitis requiring prescription of antibioticsA significant subcutaneous or deep cervical abscess is exceptionally rare and should be drained.
7.Hypertrophic or keloid scar
This is more likely to form if the incision overlies the sternum and in dark skinned individuals.
Intradermal injections of corticosteroid should be given at once and repeated monthly if necessary. Scar revision rarely results in significant long-term improvement.
8.Stitch granuloma
This may occur with or without sinus formation and is seen after the use of non-absorbable, particularly silk, suture material. Absorbable ligatures and sutures should be used throughout thyroid surgery. Some surgeons use a subcuticular absorbable skin suture rather than the traditional skin clips or staples.