By
Dr.Salah Aljanaby
Ass. Prof
General and Laparoscopic Surgeon
Lecture 3
thyroid gland
NEOPLASMS OF THE THYROID
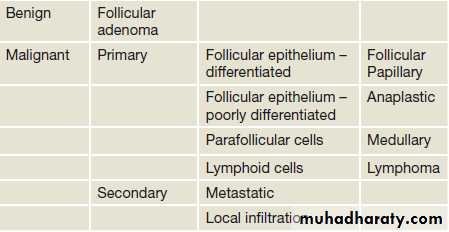
Classification of thyroid neoplasimsBenign tumours
Follicular adenomas present as clinically solitary nodulesdistinction between a follicular carcinoma and an adenoma can only be made by histological examination; in the adenoma there is no invasion of the capsule or of pericapsular blood vessels. For this reason, FNA, which provides cytologic detail but not tissue architecture, cannot differentiate between benign and malignant follicular lesions
. Diagnosis and treatment is therefore, by wide excision, i.e. total lobectomy.
The remaining thyroid tissue is normal so that prolonged follow-up is unnecessary.
Malignant tumours
The vast majority of primary malignancies are carcinomas derived from the follicular cellsSuch tumors were thought of as differentiated (papillary, follicular and Hürthle cell) and undifferentiated (anaplastic).
The parafollicular C cells can undergo malignant transformation into medullary carcinoma, and thyroid lymphoma is another primary thyroid malignancy.
the thyroid can be involved by direct spread from surrounding structures (larynx and oesophagus) or metastases (most commonly from renal cell carcinoma).
Lymph node and blood-borne metastases of thyroid cancer occur primarily to bone and lung and may be the mode of presentation
Aetiology of malignant thyroid tumours
The great majority of thyroid cancers have no known aetiological factor.The most important identifiable aetiological factor in differentiated thyroid carcinoma (particularly papillary) is irradiation of the thyroid under 5 years of age.
Short latency aggressive papillary cancer is associated with the ret/PTC3 oncogene and later developing, possibly less aggressive, cancers with ret/PTC1.
The incidence of follicular carcinoma is high in endemic goitrous areas, possibly due to TSH stimulation.
Malignant lymphomas sometimes develop in autoimmune thyroiditis
Clinical features of thyroid cancers
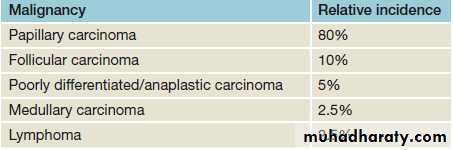
The annual incidence is about 0.6 per million of the population
The sex ratio is three females to one male.
The mortality rates remain static at over 80% 5-year survival for all groups.
anaplastic carcinoma predicts poor outcome
differentiated carcinomas generally having excellent outcomes.
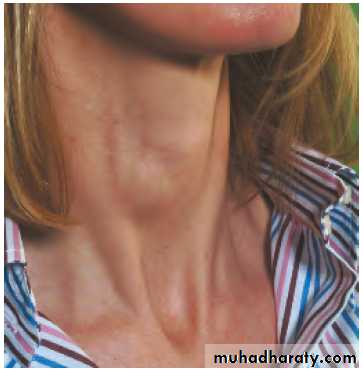
The most common presenting symptom is a thyroid swelling
Enlarged cervical lymph nodes may be the presentation of papillary carcinoma (PTC).
RLN paralysis is very suggestive of locally advanced disease.
Anaplastic growths are usually hard, irregular and infiltrating.
A differentiated carcinoma may be suspiciously firm and irregular, but is often indistinguishable from a benign swelling.
Small papillary tumours may be impalpable, even when lymphatic metastases are present.
Pain, often referred to the ear, is suggestive of nerve involvement from infiltrating
tumours.
Diagnosis of thyroid neoplasms
Clinical history and examination continue to be the cornerstone of diagnosis of thyroid neoplasms.radiation exposure and family history
Examination of the central neck and regional lymphatics should be combined with assessment of vocal cord function.
Biochemical assessment of thyroid function
Following initial assessment, the next step is ultrasound.
This non-invasive investigation is most accurate at assessing thyroid swellings. Not only can a judgement be made on the presence, size and number of thyroid nodules present, but an estimate of risk of malignancy can be made depending on these findings.
Following ultrasound, lesions can be categorised as benign, indeterminate or malignant. Benign lesions require no further assessment unless surgery is considered for compressive symptoms.
Indeterminate or malignant lesions should be investigated with FNAC.
Occasionally, the surgeon will encounter a thyrotoxic patient. Such cases are one of the few indications for a radioiodine uptake scan. This allows assessment of the function of a nodule. Hot nodules are very rarely malignant. Cold nodules will require assessment as for all other thyroid neoplasms.
Following clinical, ultrasound and cytological assessment, the vast majority of lesions will be characterised as benign, malignant or indeterminate. Further treatment will be planned accordingly.
Papillary carcinoma
is the most common thyroid malignancy.its propensity for lymph node metastases.
more common in younger patients
Distant metastases are uncommon in PTC.
‘papillary microcarcinoma’. This term is used to describe PTC that is <10 mm in size. These lesions are common (detected in about 10% of benign thyroid resections) and not associated with adverse outcomes, including recurrence or non-survival.
Follicular carcinoma
Follicular carcinoma can normally only be differentiated from follicular adenoma by the architecture on histology. For this reason, follicular lesions on FNA are unable to be diagnosed as malignant in the absence of clinical features such as metastasesMultiple foci of follicular carcinoma are seldom seen and lymph node involvement is much less common than in papillary carcinoma.
Blood-borne metastases are more common and the eventual mortality rate, although still low, is twice that of papillary cancer
Hürthle cell tumours are a rare variant of follicular neoplasm in which oxyphil (Hürthle, Askanazy) cells predominate histologically. Hürthle cell cancers are associated with a poorer prognosis.
Prognosis in differentiated thyroid carcinoma
The prognosis in differentiated thyroid carcinoma compared to most cancers is excellent.prognosis is much more dependent on age at diagnosis, size of the tumour, metastatic disease and the presence of either extrathyroidal spread (in papillary cancer) or major capsular transgression (in follicular carcinoma).
scoring systems all of which identify the group of patients at high (40 per cent at 20 years) or low (1 per cent at 20 years) risk of death
All patients should be TNM staged and this classification acknowledges the low risk of patients aged less than 45 years at presentation
Surgical treatment
Total thyroidectomy is recommended for tumours greater than 2 cm and those with nodal involvement or metastases and lobectomy for the remainder.
Additional measures
Thyroxinethyroxine in a dose of 0.1– 0.2 mg daily, to suppress endogenous TSH production, for all patients after operation for differentiated thyroid carcinoma on the basis that most tumours are TSH dependent.
Radioiodine
The indications for scanning after operations for differentiated carcinoma are also disputed, but radioiodine is indicated in patients with unresectable disease, local recurrence or metastatic disease, high-risk patients, and in those with a rising serum thyroglobulin level.
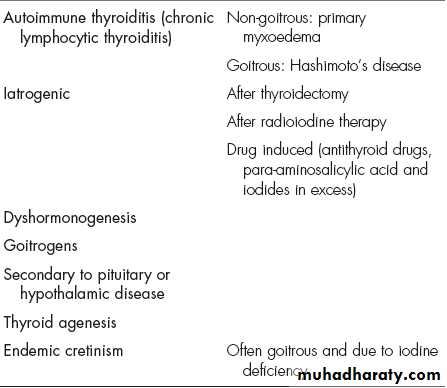
HYPOTHYROIDISM
Adult hypothyroidism
The term myxoedema should be reserved for severe thyroid failure and not applied to the much more ommon mild thyroid deficiency.The signs of thyroid deficiency are:
• bradycardia • cold extremities • dry skin and hair • periorbital puffiness • hoarse voice • bradykinesis, slow movements • delayed relaxation phase of ankle jerks.
The symptoms are:
• tiredness • mental lethargy • cold intolerance • weight gain • constipation • menstrual disturbance • carpal tunnel syndrome.
Thyroid function tests
These show low T4 and T3 levels with a high TSH (except in therare event of pituitary failure)
High serum levels of TPO antibodies are characteristic of autoimmune disease.
Treatment
Oral thyroxine (0.10–0.20 mg) as a single daily dose is curative.
Myxoedema
The signs and symptoms of hypothyroidism are accentuated. The facial appearance is typical, and there is often supraclavicular puffiness, a malar flush and a yellow tinge to the skin .Myxoedema coma, characterised by altered mental state, hypothermia and a precipitating medical condition, for example cardiac failure or infection, carries a high mortality.
Treatment
thyroid replacement, either a bolus of 0.50 mg of T4 or 10 μg of T3 either i.v. or orally every 4–6 hours. If the body temperature is less than 30°C, the patient must be warmed slowly.
Intravenous broad-spectrum antibiotics and hydrocortisone (in divided doses) are recommended.
Primary or atrophic myxoedema is considered to be an autoimmune disease similar to chronic lymphocytic (Hashimoto’s) thyroiditis but without goitre formation.
Delay in diagnosis is common and the degree of hypothyroidism is usually more severe than in goitrous autoimmune thyroiditis.