Breast
Lecture 3د مهند الشلاه
Learning objectivesBreast reconstructive surgery
Breast cancer prognosis
Breast Surveillance
• Familial breast cancer
• Communication skills in breast cancer
• Gynecomastia
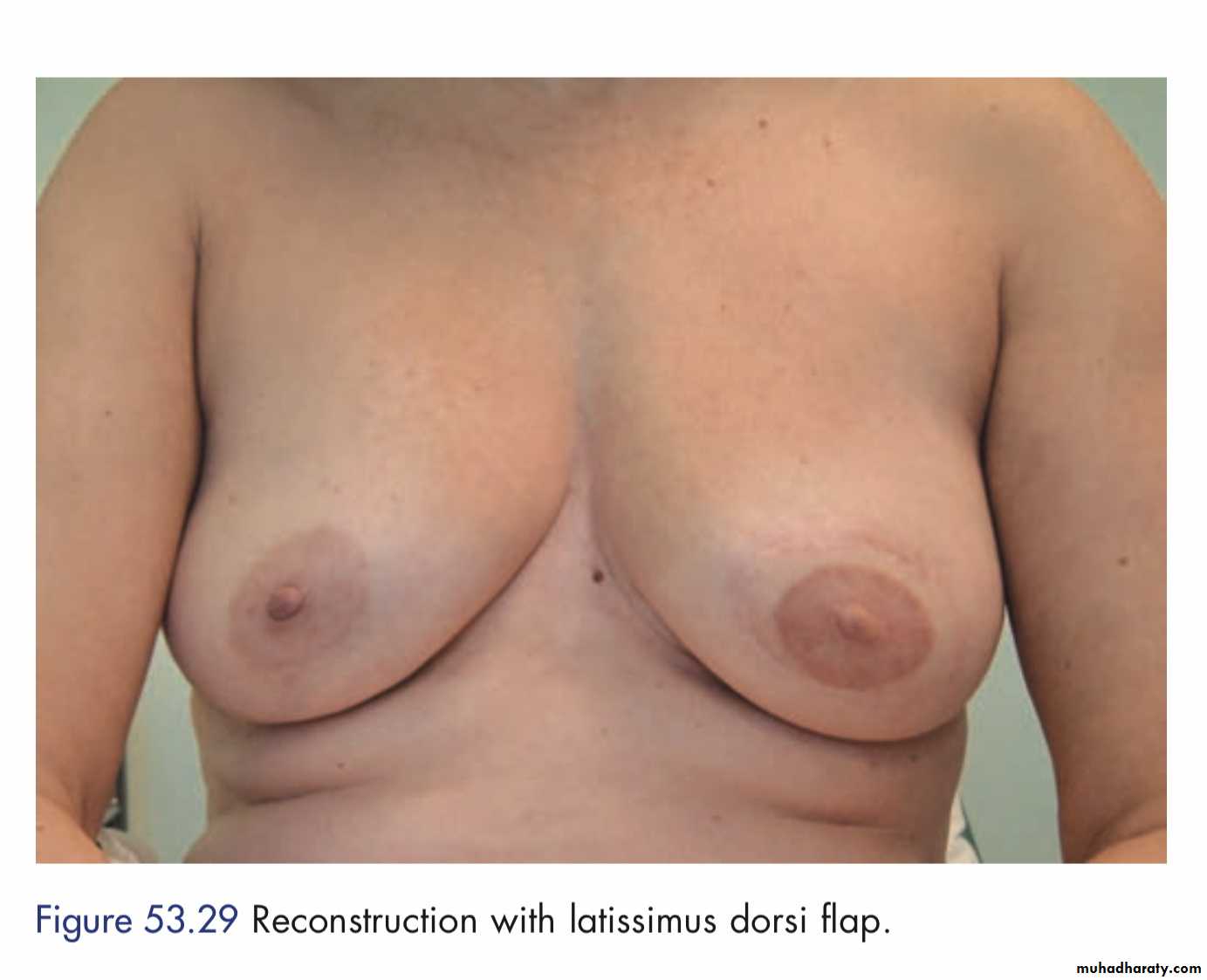
Breast reconstruction
Women can now be offered immediate or delayed reconstruction of the breast.The easiest type of reconstruction is using a silicone gel implant under the pectoralis major muscle.
This may be combined with prior tissue expansion using an expandable saline prosthesis first which creates some ptosis of the new breast.
If the skin at the mastectomy site is poor (e.g. following radiotherapy) or if a larger volume of tissue is required, a musculocutaneous flap can be constructed either from
• Latissimus dorsi muscle (an LD flap) or
• Transversus abdominis muscle TRAM flap
Nottingham prognostic index = (0.2* tumor size in cm) + tumor grade (1–3) + lymph node stage (1–3)
– Value < or = 2.4 – excellent prognosis
– Value < or = 3.4 – good prognosis– Value < or = 5.4 – moderate prognosis
– Value > 5.4 – poor prognosis.
Prognosis
• Monthy self examination
• 6 monthly clinical examination and systemic examination for 1st 2 years and yearly thereafter.• Yearly mammogram.
• Metastatic follow-up as per the symptoms.
Follow-up
Screening for breast cancer
• Because the prognosis of breast cancer is closely related to stage at diagnosis so breast screening by mammography in women over the age of 50 years will reduce cause-specific mortality by up to 30 per cent.• Three-yearly mammographic screening for women between the ages of 50 and 64 years (now increased to 70 years).
Breast Surveillance
Early detection of breast cancer by surveillanceFamilial breast cancer
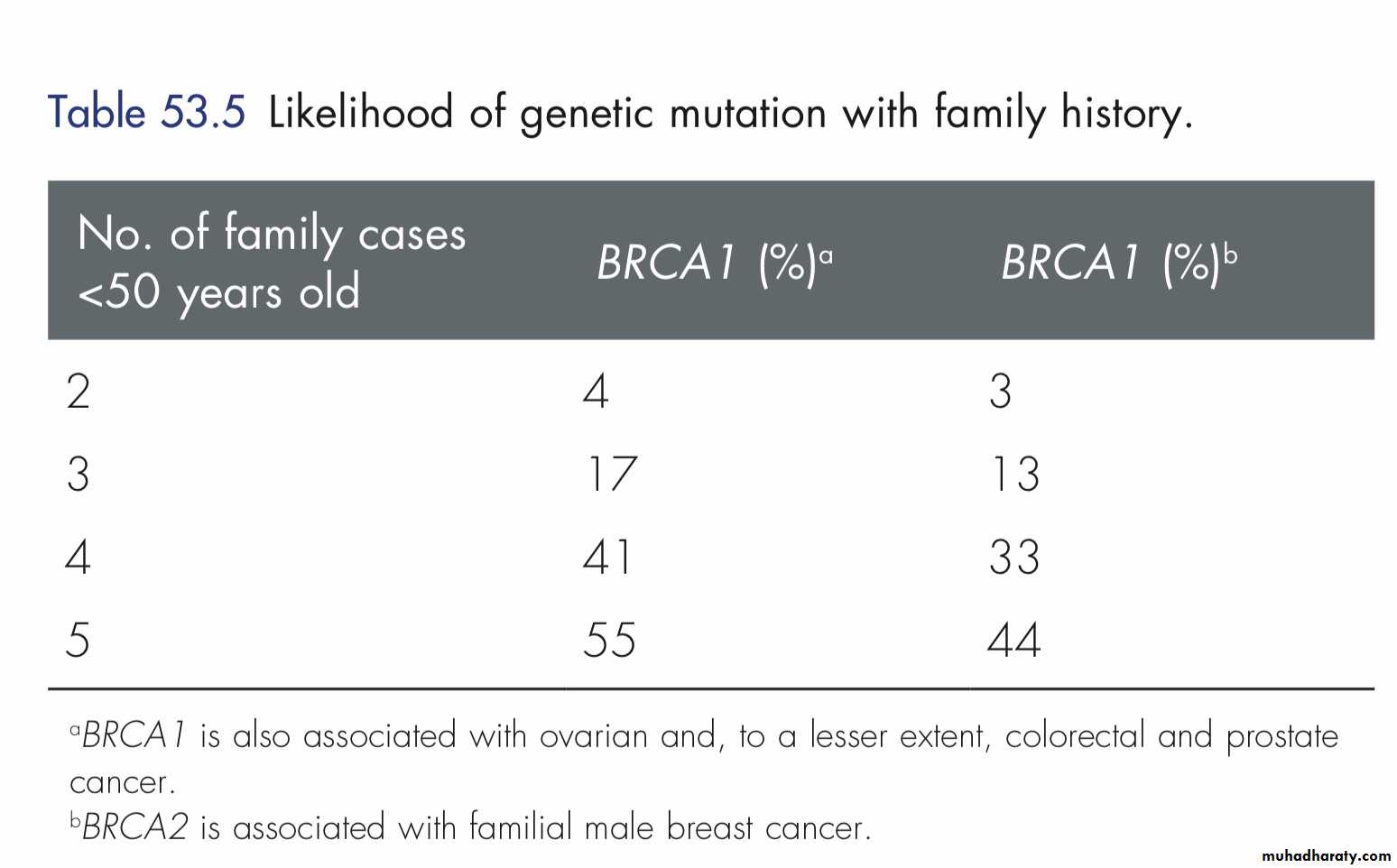
• Breast cancer is due to an inherited genetic change actually account for less than 5 per cent of all cases of breast cancer.
• Those who prove to be ‘gene positive’ have a 50–80 per cent risk of developing breast cancer, predominantly while premenopausal.
• Many will opt for prophylactic mastectomy.
For the great majority of women with a positive family history, who are unlikely to be carriers of a breast cancer gene should be assessed and followed-up.
Tamoxifen given for five years appears to reduce the risk of breast cancer by 30–50 per cent.
Familial breast cancer
It’s noncancerous increase in the size of male breast tissue.Gynecomastia
Causes of gynecomastia are as follows:
Physiological• Neonatal gynecomastia due to placental estrogens.
• Adolescent gynecomastia due to relative estrogen excess.
• Senescent gynecomastia due to relative testosterone deficiency.
Pathological
• Idiopathic—mc
• Estrogen excess
Gynecomastia
Primary testicular failure
−Klinefelter syndrome,
testicular feminization syndrome
Secondary testicular failure
− Orchitis, trauma, castration, leprosy, − Renal failure− Myotonic dystrophy or spinal cord injury
Increased testicular production
− Testicular tumors (Leydig cell, sertolicell, granulose/ theca cell tumor)− Bronchogenic carcinoma and
transitional cell tumor of urinary tract
Increased aromatization
− Adrenal hyperplasia or carcinoma− Cirrhoses, thyrotoxicoses, exogenous androgen administration
Common Drugs (DOC4KS ) Digitalis, oral contraceptive pills, cimetidine, clomiphene, captopril, calcium channel blockers, ketoconazole, spironolactone.
Other drugs: Isoniazid, tricyclic antidepressants, methyldopa, flutamide.
Grade 1
Mild enlargement, no skin redundancyGrade 2A
Moderate enlargement, no skin redundancy
Grade 2B
Moderate enlargement, skin redundancy
Grade 3
Marked enlargement with skin redundancy and ptosis
Simon grading
Investigations
History and physical examination.
Evaluate testis: Testicular ultrasound, serum testosterone, LH, DHEAS, endocrine profile—estrogen, prolactin, adrenal CT.
Thyroid function tests.
Breast mammogram, ultrasound, biopsy.
Liver function test, abdominal CT.
Treatment
• Stop offending drug.• Treat the systemic disease, if present.
• Karyotyping for klinfelter if positive, consider bilateral mastectomy.
• Most cases resolve spontaneously and 1 year observation period is suggested.
• Pharmacology during observation: Tamoxifen, danazol, aromatase inhibitors all have been used in the treatment of gynecomastia.
• Surgery is done for gynecomastia of long duration, cosmetic or psychological reason, symptomatic or suspected malignancy.
• Simple mastectomy, subcutaneous mastectomy, liposuction, reduction mammoplasty are all suggested procedures.
How do you tell a patient she is at increased risk for breast cancer?
What do you tell them?A young woman who has a family history associated with an increased risk for the BRCA1 or BRCA2 or other gene mutations
How do you tell a patient she has breast cancer?
SIGN 84 Management of breast cancer in women. A national clinical guideline. Available online at: www.sign.ac.uk
A 32-year-old woman presents for evaluation of a lump that she noticed in her right breast on self-examination. She says that while she does not perform breast self-examination often, she thinks that this lump is new. She denies nipple dis charge or breast pain, although the lump is mildly tender on palpation. She has never noticed any breast masses previously and has never had a mammogram. She has no personal or family history of breast disease. She takes oral contraceptive pills (OCPs) regularly, but no other medications. She does not smoke cigarettes or drink alcohol. She has never been pregnant. On examination, she is a well-appearing, somewhat anxious, and thin woman. Her vital signs are within normal limits. On breast examination, in the lower outer quadrant of the right breast, there is a 2-cm, firm, well-circumscribed, freely mobile mass without over lying erythema that is mildly tender to palpation. There is no skin dimpling, retraction, or nipple discharge. While no other discrete breast masses are palpable, the bilateral breast tissue is noted to be firm and glandular throughout. There is no evidence of axillary, supraclavicular, or cervical lymphadenopathy. The remainder of her physical examination is unremarkable.
What is the most likely diagnosis of this breast lesion?
What is the first step in evaluation?What is the recommended follow-up for this patient?
Routine use of screening mammography in women ≥50 years of age reduces mortality from breast cancer by 25%. MRI screening is recommended in women with BRCA mutations and may be considered in women with a greater than 20% to 25% lifetime risk of developing breast cancer.
Core-needle biopsy is the preferred method for diagnosis of palpable or nonpalpable breast abnormalities.
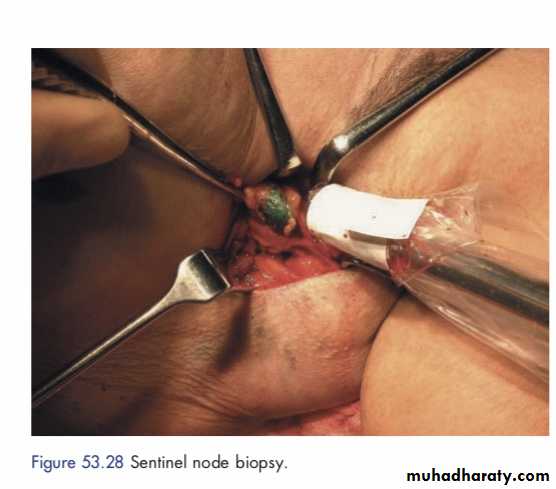
Sentinel node dissection is the preferred method for staging of the regional lymph nodes in women with clinically node-negative invasive breast cancer. Axillary dissection may be avoided in women with 1 to 2 positive sentinel nodes who are treated with breast conserving surgery, whole breast radiation and systemic therapy.
Local-regional and systemic therapy decisions for an individual patient with breast cancer are best made using a multidisciplinary treatment approach. The sequencing of therapies is dependent on patient and tumor related factors including breast cancer subtype.