Hernia
Lecture 3د مهند الشلاه
LEARNING OBJECTIVES
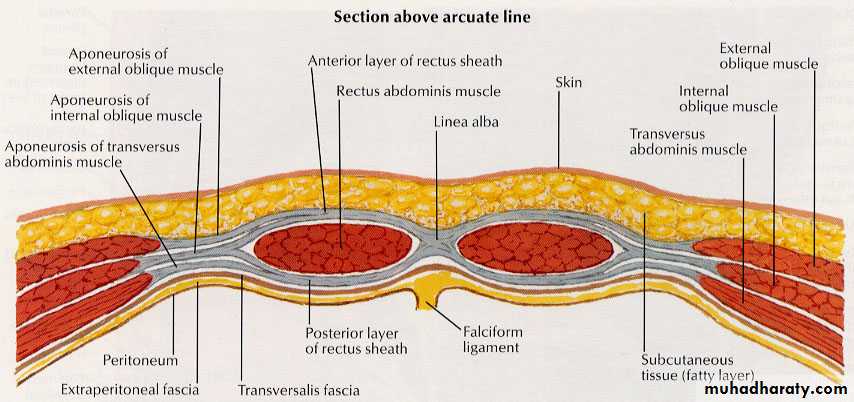
To know and understand:• Applied anatomy of the anterior abdominal wall
• Pathophysiology, clinical features, Investigations and principles of management of ventral herniaUmbilical hernias are congenital defects that may enlarge over time and become protuberant and symptomatic.
Most newborn umbilical hernias close spontaneously by the second year of life.
However, umbilical hernias are also common in adults.Patients with ascites have a high incidence of umbilical hernias.
Umbilical hernias greater than 3 cm should be repaired with a prosthetic mesh.Umbilical hernia in adults
Conditions which cause stretching and thinning of the midline raphe (linea alba), such as pregnancy, obesity and liver disease with cirrhosis, predispose to reopening of the umbilical defect.
In adults, the defect in the median raphe is immediately adjacent to (most often above) the true umbilicus, although at operation this is indistinguishable.
The term paraumbilical hernia is commonly used.
The defect is rounded with a well-defined fibrous margin. Small umbilical hernias often contain extraperitoneal fat or omentum.
Larger hernias can contain small or large bowel but, even when very large, the neck of the sac is narrow compared with the volume of its contents.
As a result, in adults, umbilical hernias which include bowel are prone to become irreducible, obstructed and strangu- lated.
Umbilical hernia in adults
■ Common in overweight men or multiparous women■ Progressively increase in size and may get very large indeed
■ Round defect with rigid fibrous margins
■ Surgery advised because of risk of obstruction and strangulation
Epigastric hernias are hernias of the linea alba above the umbilicus.
They occur more frequently in athletically active young men or women.Usually, they produce epigastric pain that may be falsely attributed to other abdominal diagnoses. The diagnosis is made by palpation of a subcutaneous epigastric mass; most such hernias occur within a few centimeters of the umbilicus and are associated with a small (1 to 2 cm) fascial defect.
Very small epigastric hernias have been known to disappear spontaneously, probably due to infarction of the fat.
Small to moderate-sized hernias without a peritoneal sac are not inherently dangerous and surgery should only be offered if the hernia is sufficiently symptomatic.
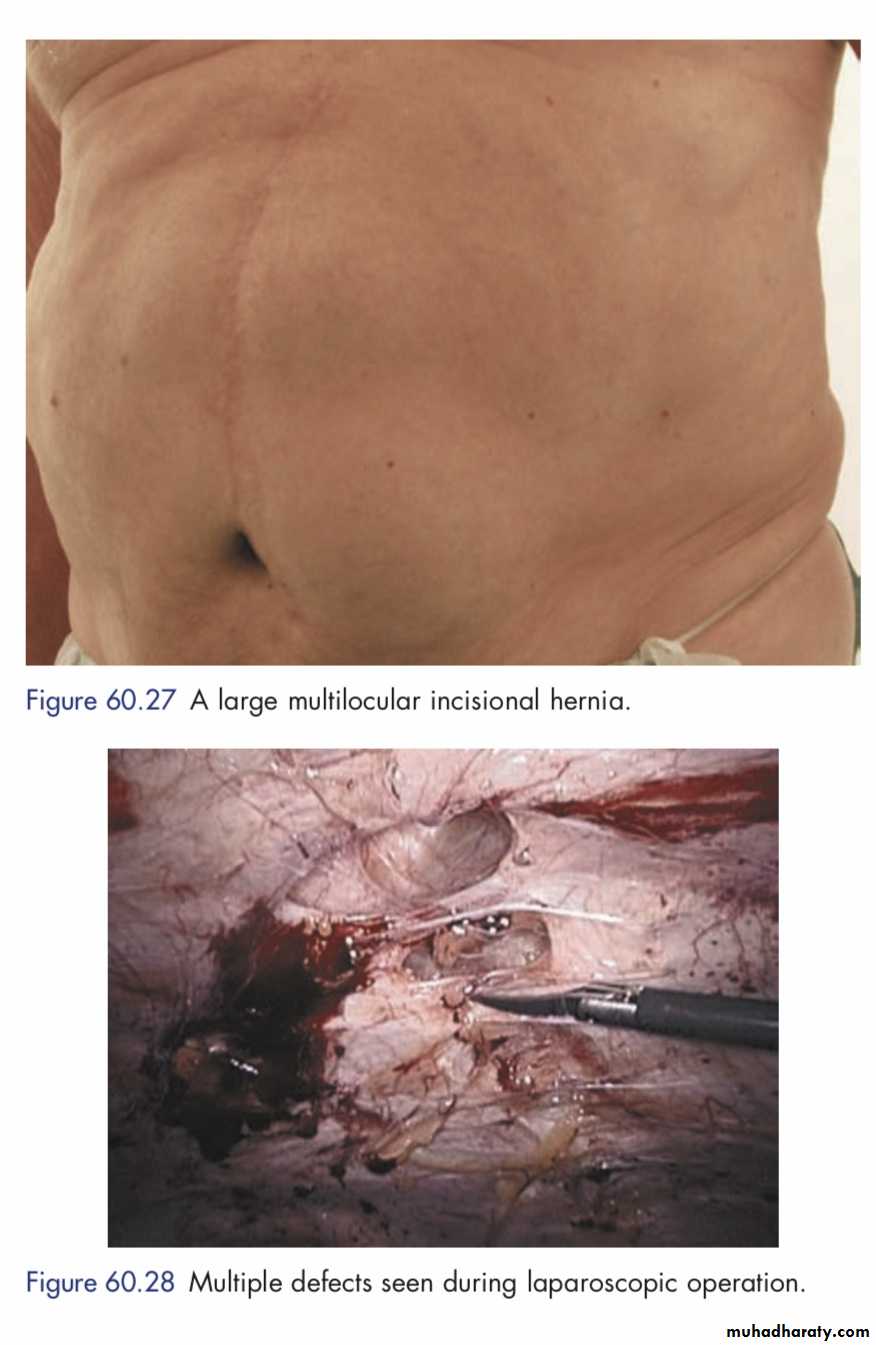
Ventral incisional hernia
Ventral Hernia: AnatomyVentral Incisional Hernia
4-5 million laparotomies/year1,2400-500,000 incisional hernias develop3
200,000 incisional hernia repairs/yr1-3
Common occurrence after abdominal surgery (up to 13% of laparotomy incisions)4,5
• National Centre for Health Statistics. Combined surgery data (NHDSand NSAS) data highlights. Available at: http://www.cdc.gov/nchs/about/major/hdasd. 1996. Accessed September 14,2007.
• Lomanto, S. Surg Endosc 2006;20:1030 –5.
• Burger J. Ann Surg. 2004;240:578-585.
• Mudge, M. Br J Surg 1985;72:70 –1.
• Lewis, RT. Can J Surg 1989;32:196 –200.
• Hoer, J. Chrirug 2002;73:474–480.
Why fix them?
• Increase in size over time• Can lead to: - obstruction- incarceration- strangulation- enterocutaneous fistula- chronic back/abd pain- loss of abdominal domain- poor pulmonary function
Predictors of VIH
• Obesity• Pulmonary disease
• Wound infection
• Intra-abdominal sepsis
• Malnutrition
• Anaemia
• Corticosteroid dependency
• Prior VIH repair
• Collagen vascular diseases
• AAA
• Low CI:CIII ratios and elevated MMPs
Effect of Stitch Length on Wound Complications After Closure of Midline Incisions; A Randomized Controlled Study
Issues with repair
• No universal technique for repair• Functional repair versus prosthetic covering
• High recurrence rate (RR) for repairs- Primary suture repair near ~50% RR 1-3- Mesh repair 2-36% RR
• Mannien MJ. Eur J Surg 1991;157:29 –31
• Anthony T. World J Surg 2000;24:95–1000
• Luijendijk RW. N Engl J Med 000;343:392–8.
Guidelines for Laparoscopic Ventral Hernia Repair
Earle D, Roth S, Saber A, Haggerty S, Bradley III JF, Fanelli R, Price R, Richardson W, Stefanidis D.SAGES Guidelines Committee 2014
(Society of American Gastrointestinal and Endoscopic Surgeons)
PARASTOMAL HERNIA
Occurs through defects adjacent to stoma siteIncidence: 12-32% paracolostomy
< 10% paraileostomy
Prevention: Small fascial incision
Complications:
1. Obstruction;
2. Incarceration
3. Poor Appliance fit
4. Local pain
Parastomal Hernia
An Incisional Hernia related to an abdominal wall stoma.
Particularly noticeable on tensing the abdominal wall muscles- coughing, sneezing, straining or standing.
Para Stomal Hernia
Management of a parastomal hernia is a common clinical dilemma.Once such a hernia is established, it is difficult to treat, and many operative factors have been claimed to influence its occurrence and many techniques of repair have been described.
[Carne, Robertson and Frizelle]
Diagnosis
• History• Examination - Standing - Lying
• Valsalva manoeuvre
• Digital examination of stoma
• CT Scan
Risk Factors
• Intrinsic
• Age
• Obesity
• Wound Infection
• Smoking
Extrinsic
• Emergency Surgery
• Location of Stoma
• Previous repair
Indications for Surgical Repair
• Strangulation• Obstruction
• Fistula formation
• Ischaemia
• Pain
• Body Image - patient expectation
Choice of Surgical Procedures
• 1. Stoma Relocation• 2. Local Tissue Repair
• 3. Prosthetic Repair - intraperitoneal
• - extraperitoneal
• - fascial onlay
Surgical Repair
Increased infection rates
Recurrence 39% [Reiger, 2004]
Complications 57% [Hughes, 1999]
Laparoscopic repair with mesh 10% recurrence [Le Blanc, 2004]