• Urethra and Penispart IIDr. Wadhah A. Marzooqassisst prof. (URO)dr_wadhah_uro@yahoo.com4th stage student2020
Inflammation of urethra
Gonorrheal urethritis• Gonorrhea is a sexually transmitted disease caused by Neisseria gonorrhea (gonococcus), a Gram-negative kidney-shaped diplococcus that infects the anterior urethra in men, the urethra and cervix in women
• discharge up to 10 days after exposure.
• There is often scalding dysuria. In some there may be no symptoms other than slight discharge.
• Investigation. Urinalysis…….pus cell, gram stained urethral swab…….intracellular diplococci, culture of urethral discharge
• Treatment………cephalosporine (ceftriaxone 250 mg single dose) if mixed infection add azthromycine 1 gm single dose orally)
• Complications.. posterior urethritis, prostatitis (acute or chronic), acute epididymoorchitis, periurethral abscess and urethral stricture. Gonococcal arthritis, iridocyclitis
Non-specific urethritis (non-gonococcal urethritis)
• Diagnosed by exclusion of gonorrhoea and other known infections. 40% …Chlamydia trachomatis and some …..Ureaplasma urealytica. causative agent in up to 50% of cases is unknown.• Dysuria and a mucopurulent urethral discharge appear up to 6 weeks after sexual intercourse. Epididymitis is not uncommon and urethral stricture rarely results.
• Tetracycline, doxycycline or azithromycine
Urethral stricture
Causes of urethral stricture• inflammatory:
– post-gonorrhoea, Chlamydia.
• Congenital;
• traumatic;
• instrumental:
– indwelling catheter;
– urethral endoscopy;
• postoperative:
– open prostatectomy;
– amputation of penis.
Clinical feature of urethral stricture are those of bladder outlet obstruction however its severity depends on the degree of stricture.
Diagnosis is done by retrograde urethrocystogram.
Treatment of urethral stricture:
Treatment of urethral stricture is by:• dilatation:
– gum-elastic bougie;
– filiform and follower;
– metal sounds;
– self-dilatation with Nélaton catheter;
• urethrotomy:
– internal visual urethrotomy;
• urethroplasty:
– excision and end-to-end anastomosis;
– patch urethroplasty.
Periurethral abscess
Penile periurethral abscess
A penile periurethral abscess arises as an acute gonococcal infection of one of the glands of Littre. The tender induration felt on the underside of the penis points and discharges externally, often leaving a fistula.
Treatment
An anterior urethrotomy will encourage the abscess to burst into the urethra.
Bulbar periurethral abscess
A bulbar periurethral abscess is a spreading cellulitis caused by infection with streptococci and anaerobic organisms, possibly associated with a stricture. Extravasation of urine is not unusual.Clinical features
There is perineal pain with pyrexia, rigors and tachycardia. Tenderness and swelling rapidly spread from the perineum to the penis and the anterior abdominal wall.
Treatment
Antibiotics are essential. Collections of pus should be drained and the urethra should be defunctioned by a suprapubic urinary catheter.
Urethral calculi
Urethral calculi can arise primarily behind a stricture or in an infected urethral diverticulum. More commonly, the stone is a renal calculus that has migrated to the urethra via the bladder.Clinical features
Migratory calculi cause sudden pain in the urethra soon after an attack of ureteric colic. There is blockage to the flow of urine and, if the stone is small, the force of the jet will expel it from the external urethral meatus. Larger stones get stuck and must be removed endoscopically. It is sometimes possible to feel the calculus as a hard lump in the urethra, but if there is doubt the diagnosis is confirmed by urethroscopy.
A stone formed within the urethra is less likely to cause recognizable symptoms and is usually detected during urethroscopy or bouginage.
Treatment
A stone in the prostatic urethra is displaced back into the bladder and treated by lithopaxy or suprapubic cystotomy as if it were a bladder stone. Calculi in more distal parts of the urethra are removed by basketing under vision or fragmented in situ using the electrohydraulic or ultrasonic lithotripter. It may be necessary to perform a meatotomy to deliver the stone. Open removal by external urethrotomy is rarely necessary.Neoplasms of the urethra.
Benign
Polyp
Genital warts
Angioma
Malignant primary …..SSC not common, metaplasia, urethral stricture, poor prognosis, bloody urethral discharge. Treatment by surgery.
TCC extend from the bladder.
THE FEMALE URETHRA
ProlapseProlapse occurs in later life and is usually symptomless. Prolapse of the urethral lining also occurs as a congenital abnormality, when it causes discomfort proportional to the degree of prolapse.
Stricture
This is uncommon in women but follows urethritis or, more commonly, the trauma of a difficult labour
Diverticulum (urethrocele)
Diverticulum is more common in women than men. Some seem to be congenital. Others are acquired by rupture of a distended urethral gland or injury of the urethra during childbirth
Caruncle
This is common in elderly women. It presents as a soft, raspberry like, pedunculated granulomatous mass about the size of a pea, attached to the posterior urethral wall near the external meatus. It is composed of highly vascular connective tissue stroma infiltrated with pus cells.There may be frequency of micturition and pain afterwards
Treatment is by excision and diathermy coagulation of the base of the stalk
Papillomata acuminata
Papillomata acuminata are the same as the sexually transmitted warts that occur on the penis. They are treated in the same way. In African women, papillomata acuminata are common and may grow to such a large size during pregnancy that they obstruct labour and necessitate a Caesarean section.Carcinoma of the urethra
This occurs twice as often in women as in men. Whether a caruncle can become malignant is disputed, but caruncles and tumours often occur close together. Malignant swellings of the urethra feel harder than benign ones.Treatment by radiotherapy or radical surgery is often ineffective.
The overall prognosis is poor.
THE PENIS
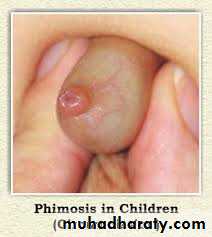
Phimosis.Failure of retraction of the prepuce over the glans penis
The physiological adhesions between the foreskin and the glans penis may persist until 6 years of age or more.
Presentation difficult urination.
Treatment is by circumcision.
Paraphimosis
A tight foreskin once retracted may be difficult to return and a paraphimosis results.In this condition, the venous and lymphatic return from the glans and distal foreskin is obstructed and these structures swell, causing even more pressure within the obstructing ring of prepuce.
Treatment
Icebags, gentle manual compression and injection of a solution of hyaluronidase in normal saline may help to reduce the swelling. Such patients can be treated by circumcision if careful manipulation fails. A dorsal slit of the prepuce under local anaesthetic may be enough in an emergency.
Circumcision
Indications1- Social or religious reasons.
2- True phimosis caused by BXO (rare under the age of 5 years);
3-Recurrent attacks of balanoposthitis; and recurrent urinary tract infections .
4- Inability to retract for intercourse.
5- splitting of an abnormally tight frenulum.
6-before radiotherapy for carcinoma of the penis.
Penile Injuries
Avulsion of the skin of the penis
. Repair is effected by burying the shaft of the penis in the scrotum with subsequent release at the time of a definitive plastic surgical repair.
Fracture of the penis
• Usually occurring when the erect penis is bent violently downwards during intercourse.• The extravasation of blood causes great pain and swelling with sudden detumesence.
• In early cases, incision and drainage of the clot with suture of the defect in the tunica of the ruptured corpus cavernosum gives acceptable results.
Strangulation of the penis.
Strangulation of the penis by rings placed on the penis, usually for sexual reasons, can cause venous engorgement which prevents their removal. It may help to aspirate the corpora cavernosa but often the ring must be cut off with a ring cutter or hacksaw.Inflammations
Balanitis. inflammation of the glansPosthitis Inflammation of the prepuce
Balanoposthitis
• Skin conditions such as lichen planus and psoriasis affect the penis
• Drug hypersensitivity reactions can affect the skin of the penis
• Balanoposthitis is associated with penile cancer, diabetes and phimosis
• Monilial infections are quite common
Peyronie’s disease
Peyronie’s disease is a relatively common cause of deformity of the erect penis.
On examination, hard plaques of fibrosis can usually be palpated in the tunica of one or both corpora cavernosa. The plaques may be calcified.
The presence of the unyielding plaque tissue within the normally elastic wall of the corpus cavernosum causes the erect penis to bend, often dramatically, towards the side of the plaque.
The aetiology is uncertain but it may be a result of past trauma – there is an association with Dupuytren’s contracture.
Treatment
is difficult. Some cases continue to progress. Others seem to remit after 3–5 years.Various drug treatments have been suggested but their beneficial effect is hard to prove in such a chronic condition.
When the deformity of the penis is causing distress, it may be possible to straighten it by placing nonabsorbable sutures in the corpus cavernosum opposite the plaque.
Priapism.
Prolong erection and usually painful1-Low flow ( ischemic).
The condition is usually seen as a complication of a blood disorder such as
• Sickle cell disease or leukaemia.
• Therapeutic injection of papaverine .
• Abnormally prolonged bout of otherwise normal sexual activity.
• A tiny proportion is caused by malignant disease in the corpora cavernosa or the pelvis.
• Priapism is rarely seen as a consequence of spinal cord disease.
Treatment
An underlying cause should be excluded.
The patient should be referred for specialist urological care.
If aspiration of the sludged blood in the corpora cavernosa fails to cause detumescence,
repeated injection 1:100 000 adrenaline (epinephrine) solution .
It may be necessary to decompress the penis by an anastomosis between the corpus spongiosum and one of the corpora cavernosa.
The outlook for normal erectile function is poor.
High flow (non ischemic).
This type is not painful and is usually result from an arteriovenous fistula caused by previous trauma. It is less risky than the low flow type and not need an urgent treatment.The treatment is by surgical closure of the fistula.
Carcinoma of the penis
Most commonly SCCCircumcision soon after birth confers immunity against carcinoma of the penis. Later circumcision does not seem to have the same effect
Chronic balanoposthitis is known to be a contributory factor.
Precarcinomatous lesions.
Leukoplakia
long standing genital warts
Paget’s disease of the penis. (synonym:erythroplasia of Queyrat)
Pathology SCC
Clinical features
About 40% of patients are under 40 years of age
Mild discomfort and light discharge
large and secondary infection causes a foul bloody discharge
In total, 60% present with inguinal lymph node enlargement but in half of these this is caused by sepsis
Untreated, the whole glans may be replaced by a fungating offensive mass
Treatment
Circumcision precedes treatmentRadiotherapy is effective (60–70% survival rate at 5 years)
Surgery is for large anaplastic growths
SEXUALLY TRANSMITTED GENITALINFECTIONS
Genital herpesis caused by sexual transmission of the herpes virus
hominis (type 2, occasionally type 1)…. Genitofemoral ….. Acyclovir.
Lymphogranuloma venereum
Lymphogranuloma venereum is a sexually transmitted tropical disease caused by Chlamydia trachomatis (Chlamydia A). … painless, genital papule or ulcer often unnoticed by the patient…. The inguinal glands become enlarged and painful in both sexes between 2 weeks and 4 months after infection. The masses of nodes mat together .
Treatment is by a combination of antibiotics, which may include sulphonamide, oxytetracycline and erythromycin. The multilocular bubo should not be incised; aspiration is permissible to reduce discomfort.
Condylomata acuminata (synonym: genital warts)
Genital warts are caused by infection with human papillomavirus and are sexually transmitted.
Condyloma acuminata, are due to low-risk human papilloma virus types (usually 6 and 11).
Certain “highrisk” genital human papilloma virus types, usually 16 and 18, cause bowenoid papulosis
Patient-applied treatment is either podophyllotoxin or imiquimod.
Physician-applied treatments include liquid
nitrogen cryotherapy , and electrocautery. Laser therapy and intralesional or systemic immunotherapies