TWINS AND HIGHER
MULTIPLE GESTATIONS
Multiple pregnancies consist of two or more fetuses.
There are rare exceptions to this, such as twin gestations
made up of a singleton viable fetus and a complete mole.
Pregnancies with three or more fetuses are referred to as
‘higher multiples.
Risk factors
for multiple gestations include assisted
reproductive techniques (both ovulation induction and in
vitro fertilization (IVF)), increasing maternal age, high
parity, black race and maternal family history.
Traditionally, the expected incidence was calculated
using Hellin
’s rule. Using this rule, twins were expected in
1 in 80 pregnancies, triplets in 1 in 80
2
and so on. The
incidence of monozygotic or identical twins is generally
accepted to be constant at 1 in 250, It is not influenced by
race, family history or parity.
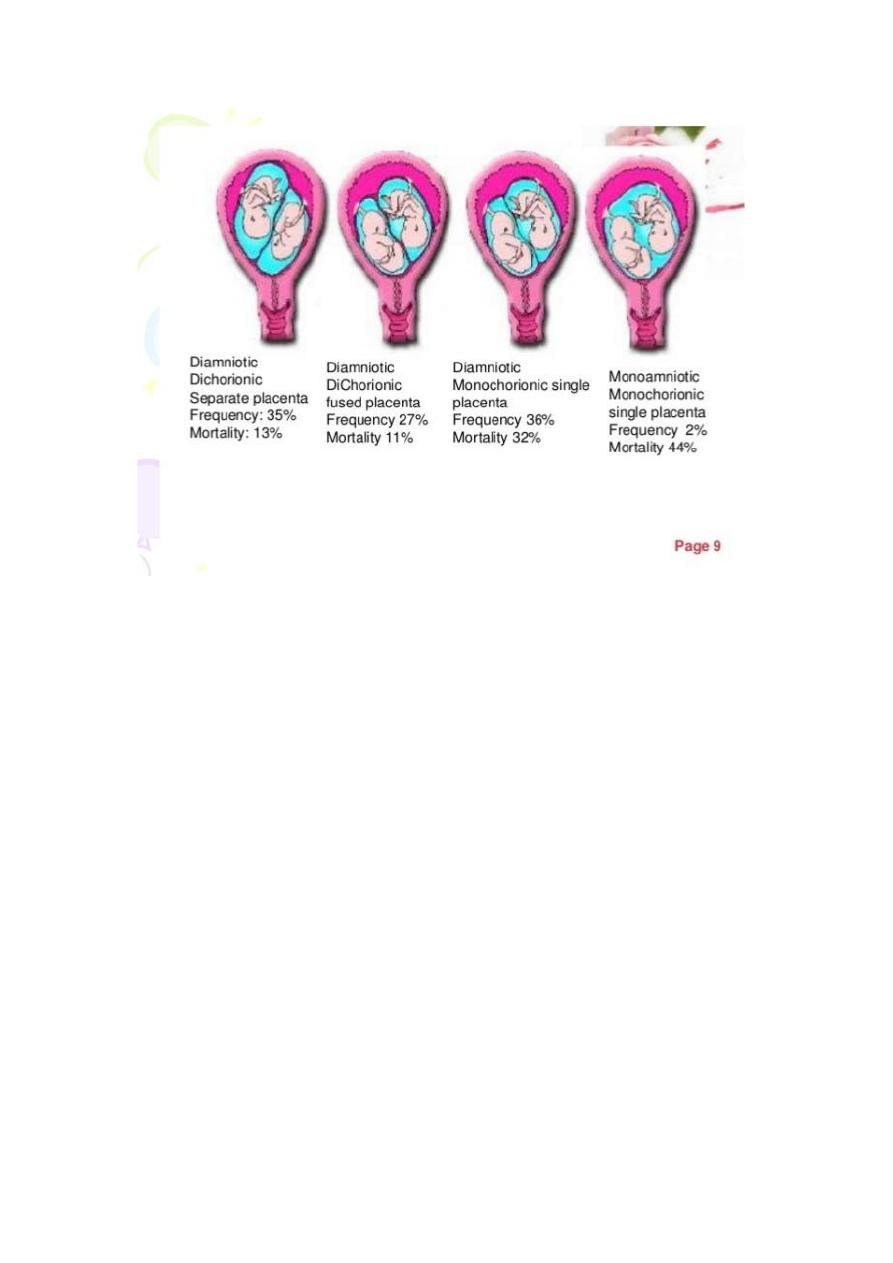
Non-identical or fraternal twins are dizygotic, having
resulted from the fertilization of two separate eggs.
Although they always have two functionally separate
placentae (dichorionic), the placentae can become
anatomically fused together and appear to the naked eye
as a single placental mass. They always have separate
amniotic cavities (diamniotic) and the two cavities are
separated by a thick three-layer membrane (fused amnion
in the middle with chorion on either side). The fetuses can
be either same-sex or different sex pairings.
Identical twins are monozygotic
– they arise from
fertilization of a single egg and are always same-sex
pairings.
They
may
share
a
single
placenta
(monochorionic)
or
have
one
each
(dichorionic)(DCDA). If dichorionic, the placentae can
become anatomically fused together and appear to the
naked eye as a single placental mass, as mentioned
above. The vast majority of monochorionic twins have two
amniotic cavities (diamniotic) but the dividing membrane
is thin, as it consists of a single layer of amnion
alone(MCDA). Monochorionic twins may occasionally
share a single sac (monoamniotic).(MCMA).
Dizygotic twins may arise spontaneously from the
release of two eggs at ovulation.
Monozygotic twins arise from a single fertilized
ovum that splits into two identical structures. The type of
monozygotic twin depends on how long after conception
the split occurs. When the split occurs within 3 days of
conception, two placentae and two amniotic cavities
result, giving rise to a dichorionic diamniotic (DCDA)
pregnancy. When splitting occurs between days 4 and 8,
only the chorion has differentiated and a monochorionic
diamniotic (MCDA) pregnancy results. Later splitting after
the amnion has differentiated leads to both twins
developing in a single amniotic cavity, a monochorionic
monoamniotic (MCMA) pregnancy. If splitting is delayed
beyond day 12, the embryonic disc has also formed, and
conjoined, or
‘Siamese’ twins will result.
All the physiological changes of pregnancy (increased
cardiac output, volume expansion, relative haemodilution,
diaphragmatic splinting, weight gain, lordosis, etc.) are
exaggerated in multiple gestations. This results in much
greater stresses being placed on maternal reserves. The
‘minor’ symptoms of pregnancy also may be exaggerated.
Complications relavent to twin pregnancy:
• Miscarriage and severe preterm delivery.
• increase in perinatal mortality will be due to the
excess of preterm delivery in monochorionic twins.
• Death of one fetus in a twin pregnancy.
With the more liberal use of early pregnancy scanning, it
has been recognized that up to 25 per cent of twins may
suffer an early demise and subsequently
‘vanish’ well
before they would have previously been detected. After
the first trimester, the intrauterine death of one fetus in a
twin pregnancy may be associated with a poor outcome
for the remaining co-twin. Maternal complications such as
disseminated
intravascular
coagulation
have
been
reported, but the incidence of this appears to be very low.
In dichorionic twins, the second or third trimester
intrauterine death of one fetus may be associated with the

onset of labour, although in some cases the pregnancy
may continue uneventfully and even result in delivery at
term. Careful fetal and maternal monitoring is required. By
contrast, fetal death of one twin in monochorionic twins
may result in immediate complications in the survivor.
These include death or brain damage with subsequent
neurodevelopmental
handicap.
Acute
hypotensive
episodes, secondary to placental vascular anastomoses
between the two fetuses, result in haemodynamic volume
shifts from the live to the dead fetus. The acute release of
vasoactive substances into the survivor
’s circulation
may also play a role. Death or handicap of the co-twin
occurs in up to 30 per cent of cases.
• Fetal growth restriction.
• Compared
to
singletons,
(dichorionic)
twin
pregnancies Fetal abnormalities.
carry at least twice the risk of the birth of a baby with an
anomaly. In contrast, each fetus in a monochorionic twin
pregnancy carries a risk for abnormalities that is four times
that of a singleton.
• Chromosomal defects and twinning.
In twins, as in singletons, the risk for chromosomal
abnormalities increases with maternal age.
Monozygotic twins arise from a single fertilized egg
and therefore have the same genetic make up. It is clear
that in monozygotic twin pregnancies, chromosomal
abnormalities such as Down
’s syndrome affect neither
fetus or both. The risk is based upon maternal age. In
dizygotic twins, the maternal age-related risk for
chromosomal abnormalities for each individual twin
remains the same as for a singleton pregnancy.
Therefore, at a given maternal age, the chance that at

least one of the twin pair is affected by a chromosomal
defect is twice as high as for a singleton pregnancy. For
example, a 40-year-old woman with a singleton pregnancy
has a fetal risk of trisomy 21 of 1 in 100.
If she has a dizygotic twin pregnancy, the risk that
one fetus would be affected is 1 in 50 (1 in 100 plus
1 in 100).
• Complications unique to monochorionic twinning:
In all monochorionic twin pregnancies there are placental
vascular
anastomoses
present,
which
allow
communication
between
the
two
fetoplacental
circulations.In approximately 15 per cent of monochorionic
twin pregnancies, imbalance in the flow of blood across
these arteriovenous communications results in twin-to-twin
transfusion syndrome (TTTS). One fetus becomes
overperfused
and
the
other
underperfused.
The
development of mild, moderate or severe TTTS depends
on the degree of imbalance. The growth-restricted donor
fetus suffers from hypovolaemia and becomes oliguric. As
fetal urine is the major component of amniotic fluid, this
fetus develops oligohydramnios. The recipient fetus
becomes hypervolaemic, leading to polyuria and
polyhydramnios. There is also a risk of myocardial
damage and high output cardiac failure.
The long-standing method of treatment has been
amniocentesis every 1
–2 weeks with the drainage of
large volumes of amniotic fluid. More recently, a small
number of centres have used fetoscopically guided laser
coagulation to disrupt the placental blood vessels that
connect the circulations of the two fetuses.
• Complications unique to monoamniotic twinning.
Monoamniotic twins share a single amniotic cavity,

with no dividing membrane between the two fetuses. They
are at increased risk of cord accidents, predominantly
through their almost universal cord entanglement.
• Complications in labour are more common with twin
gestations. These include premature birth, abnormal
presentations, prolapsed cord, premature separation
of the placenta and postpartum haemorrhage.
Antenatal management
• Routine antenatal care for all women involves
screening for hypertension and gestational diabetes.
These conditions occur more frequently in twin
pregnancies and there is also a higher risk of other
problems (such as antepartum haemorrhage and
thromboembolic
disease);
however,
the
management is the same as for a singleton.
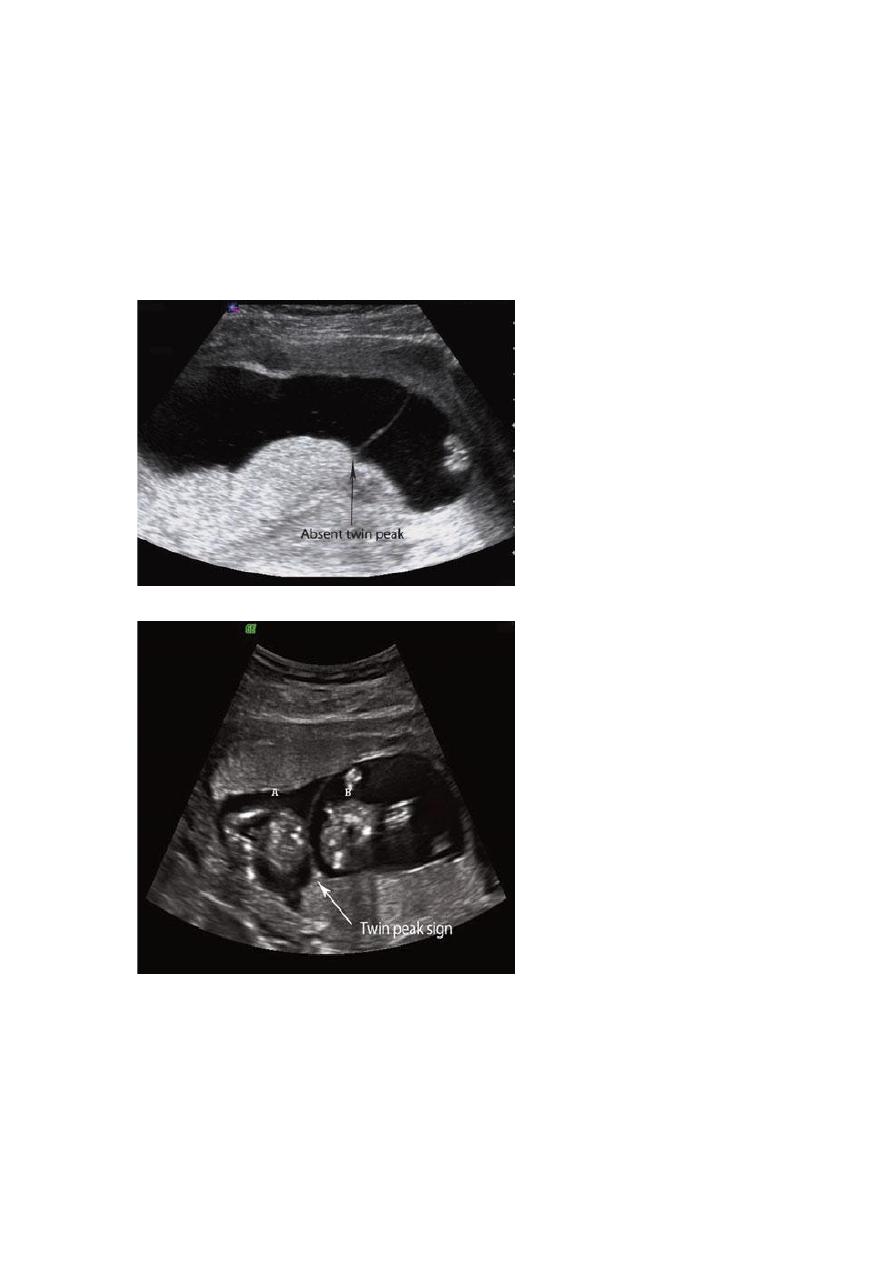
• Determination of chorionicity ,this is done
most reliably by ultrasound in the late first trimester.
In dichorionic twins, there is a V-shaped extension
of placental tissue into the base of the inter-twin
membrane, referred to as the
‘lambda’ or ‘twin-peak’
sign. In monochorionic twins, this sign is absent and
the inter-twin membrane joins the uterine wall in a
T shape .Different-sex twins must be dizygotic and
therefore dichorionic. In same-sex twins, two separate
placentae mean dichorionic, although the babies may still
be monozygotic.
• Screening for fetal abnormalities
The measurement of nuchal translucency at 12 weeks
gestation allows each fetus to have an individualized

assessment of risk.Monochorionic twins are monozygotic
and therefore only one sample is needed for karyotyping.
Both amniocentesis and chorion villus sampling
(CVS) can be performed in twin pregnancies, but in
dichorionic pregnancies, it is essential that both fetuses
are sampled.
• Monitoring fetal growth and well-being
Measurement of symphysis
–fundal height and maternal
reporting of fetal movements are unreliable, as the
individual contribution of each twin cannot be assessed.
Monitoring for fetal growth and well-being in twins is
principally by ultrasound.
In monochorionic twins, features of TTTS should be
sought, including discordances between fetal size, fetal
activity, bladder volumes, amniotic fluid volumes and
cardiac size. It is reasonable to plan 4- to 6-weekly
ultrasound scans in uncomplicated dichorionic twins.
However, due to their higher background risk, fortnightly
ultrasound is appropriate in monochorionic pregnancies
Intrapartum management
• A twin CTG machine should be used for fetal
monitoring and a portable ultrasound machine
should be available during the delivery.
• It is essential that two neonatal resuscitation trolleys,
two obstetricians and two pediatricians are available
and that the special care baby unit and anaesthetist are
informed well in advance of the delivery.
• Epidural analgesia is recommended
• An abnormal fetal heart rate pattern in the
f rst twin may be assessed using fetal scalp sampling, as

for a singleton pregnancy. However, a non-reassuring
pattern in the second twin will usually necessitate
delivery by Caesarean section. The condition of the
second twin must be carefully monitored after the
delivery of the first twin, as acute complications such
as cord prolapse and placental separation are well
recognized.
• Vaginal delivery of vertex–vertex, After the delivery
of the first twin, abdominal palpation should be
performed to assess the lie of the second twin. If the
lie is longitudinal with a cephalic presentation, one
should wait until the head is descending and then
perform amniotomy with a contraction. If contractions
do not ensue within 5
–10 minutes after delivery of the
first twin, an oxytocin infusion should be started.
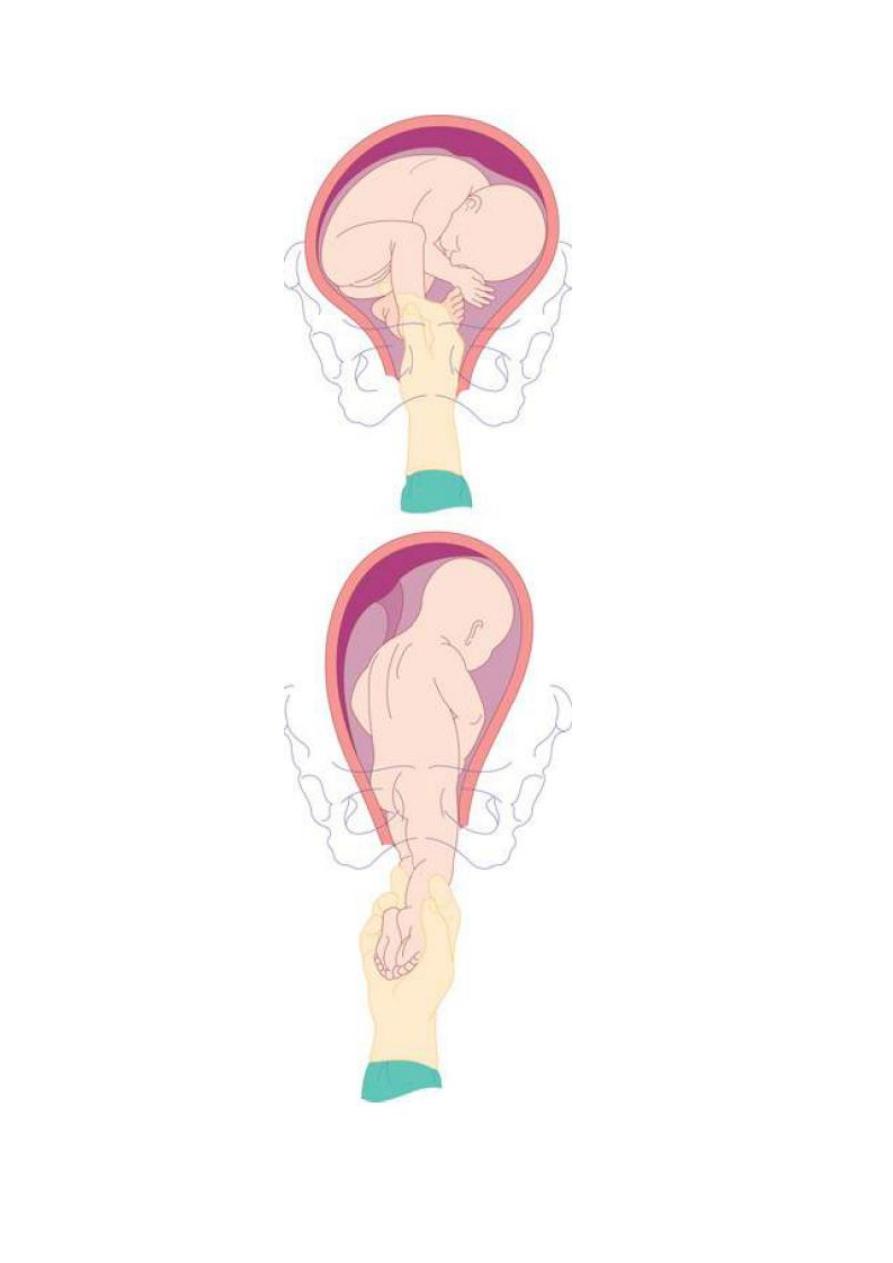
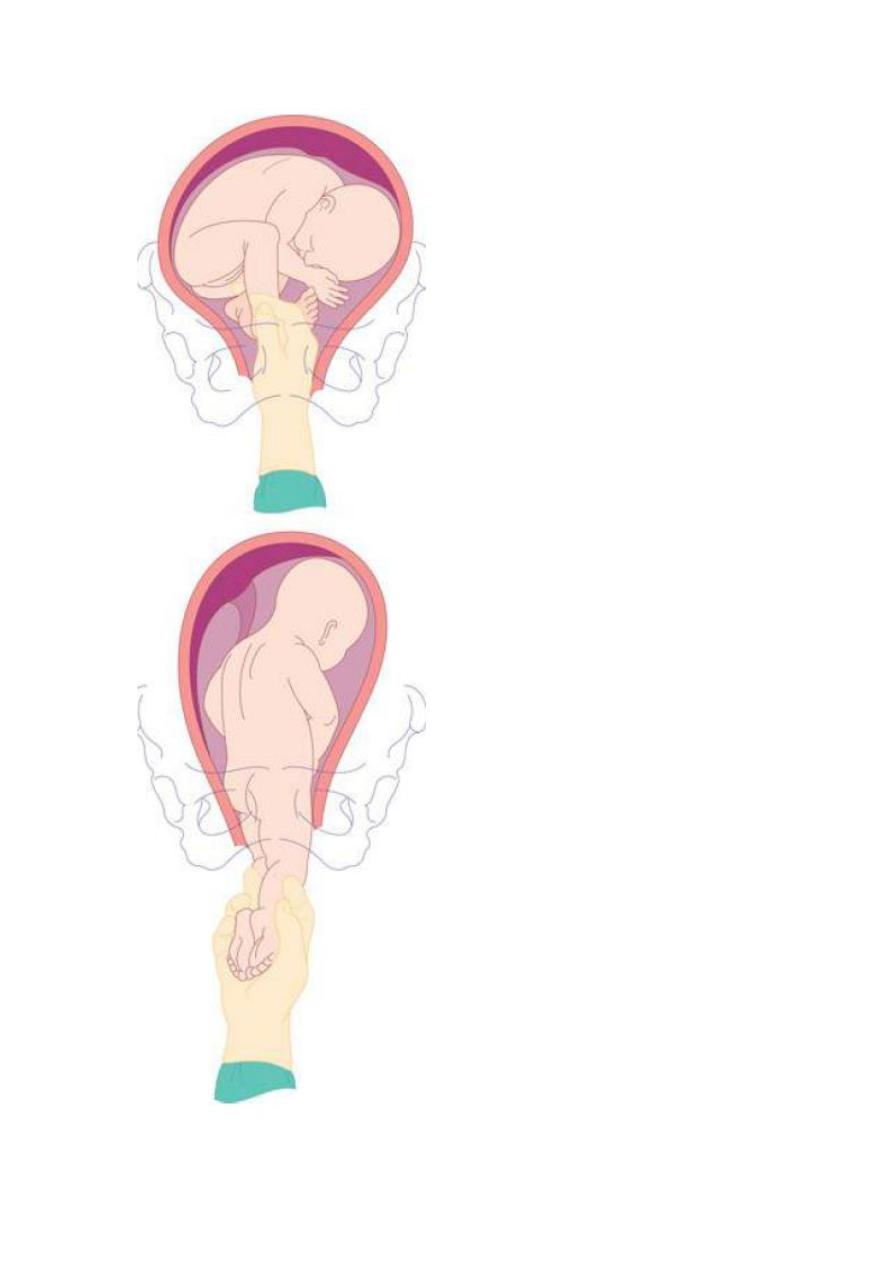
• Delivery of vertex–non-vertex,
If the second twin is a breech, the membranes can
be ruptured once the breech is fi xed in the birth canal.
A total breech extraction may be performed if fetal
distress occurs or if a footling breech is encountered,
• Where the second fetus is transverse, external
cephalic version can be successful,if not an internal
podalic version can be undertaken
• Non-vertex first twin
When the first twin presents as a breech, clinicians
usually recommend delivery by elective Caesarean
section.
• The risk of postpartum haemorrhage is increased in
twin pregnancies due to the larger placental site and
uterine over-distension. For that reason, all multiple
gestations should have an intravenous line and blood
grouped and saved during labour. Management is
generally
no
different
from
that
of
postpartum
haemorrhage complicating singleton delivery
• Higher multiples, Caesarean section is usually
advocated for delivery due to the difficulties of
intrapartum fetal monitoring.