
Part I: Endocrine Diseases in
Pregnancy
Part II: Neurological Diseases in
Pregnancy
Dr.Nadia Mudher Al-Hilli
FICOG
Department of Obs&Gyn
College of Medicine
University of babylon

Objectives
• To understand the pathophysiology &
management of thyroid disorders in pregnancy
• To know how to manage prolactinoma in
pregnant women
• To learn prepregancy, antenatal & intrapartum
care of epileptic women
• To know how to deal with migrain in pregnancy
• To learn management of Bell’s palsy in
pregnancy
Thyroid Disease in Pregnancy
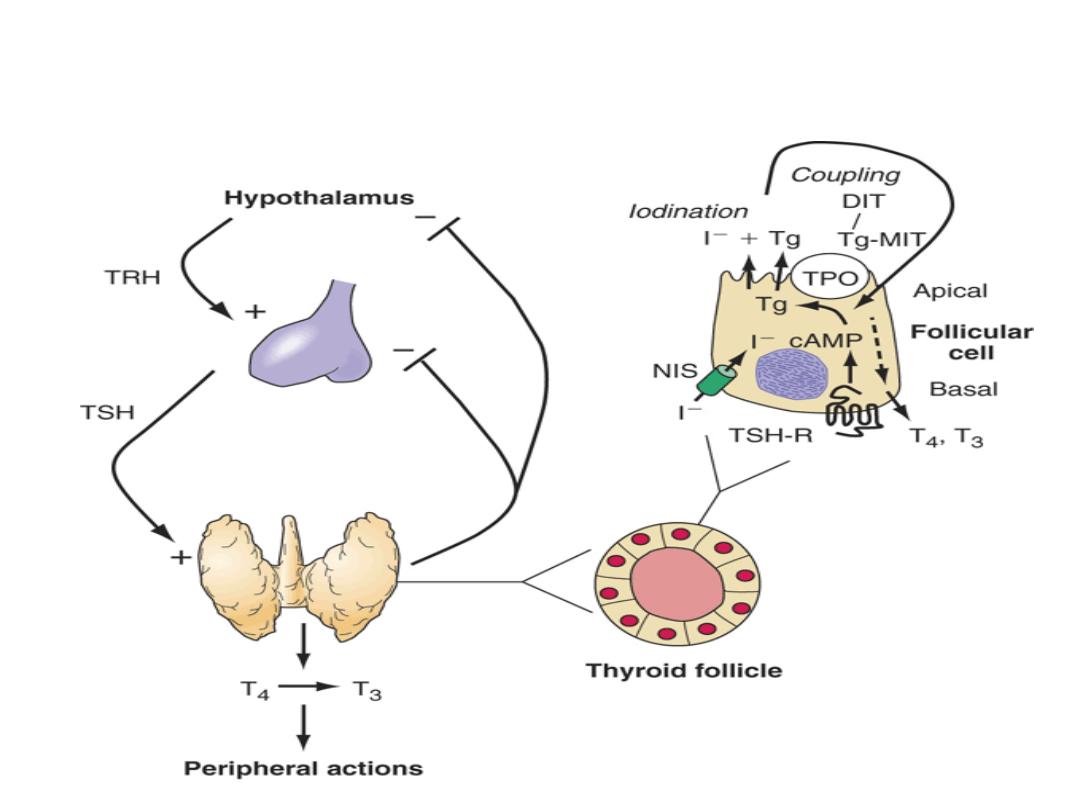
Thyroid Function in normal pregnancy:
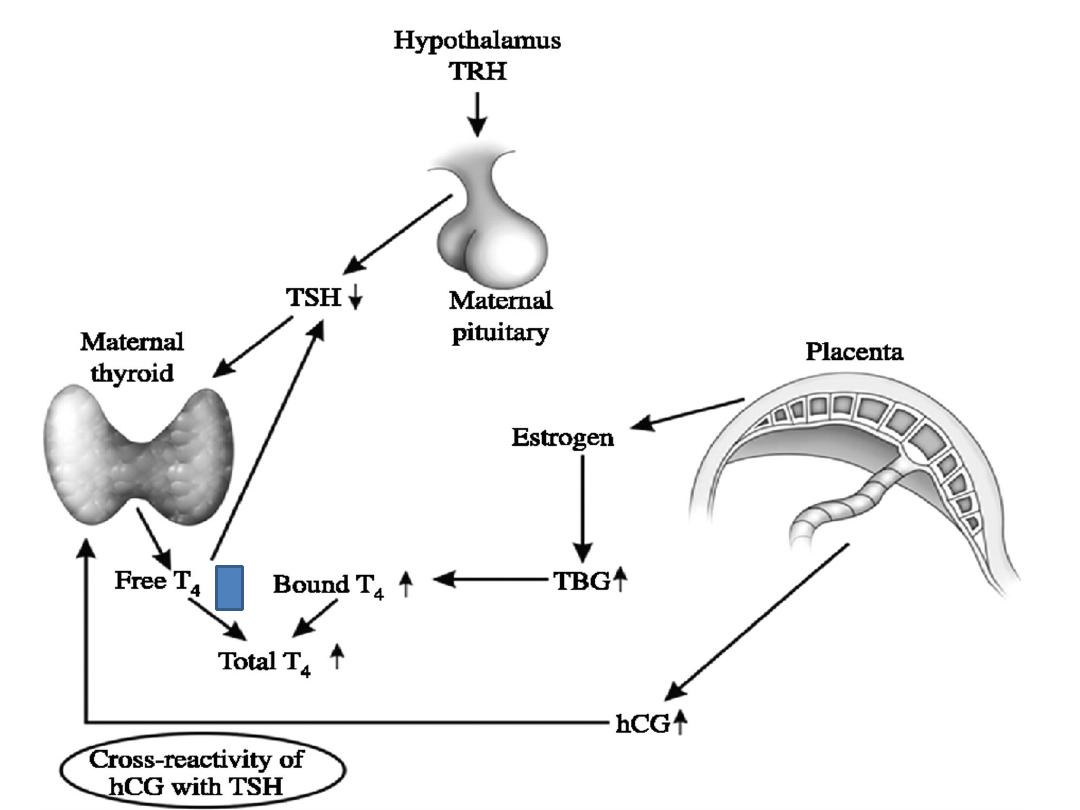
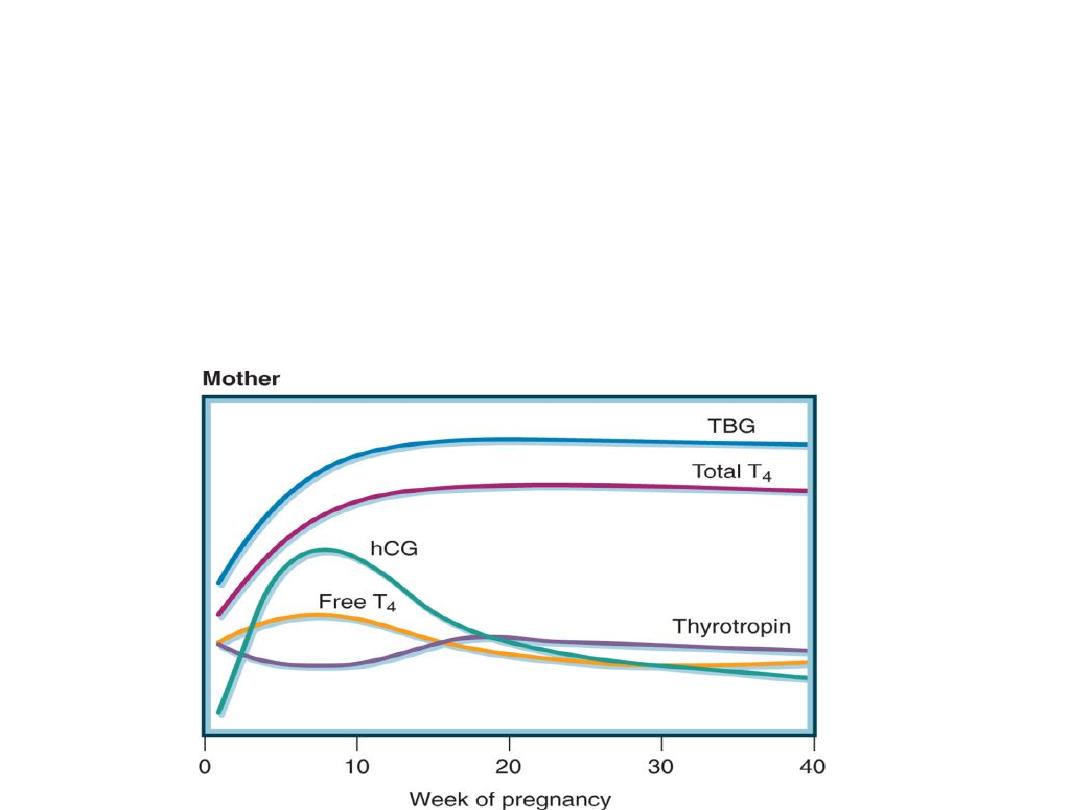
• increased Thyroid Binding Globulin
production. This leads to an increase in
total T4 and T3, but not the free
circulating thyroid hormones.

• iodine deficiency in pregnancy: due to
– increased glomerular filtration
–fetal thyroid activity.
This results in increased uptake by the
thyroid gland which enlarge and goitre
appears.

• As human chorionic gonadotrophin
(hCG) and TSH share a common alpha
subunit and have similar beta subunits,
TSH receptors are prone to stimulation by
hCG.

Fetal thyroid function:
• From 10 weeks' gestation, the fetal
thyroid gland produces both T4 and T3.
Fetal levels reach those of the adult at 16
weeks' gestation.
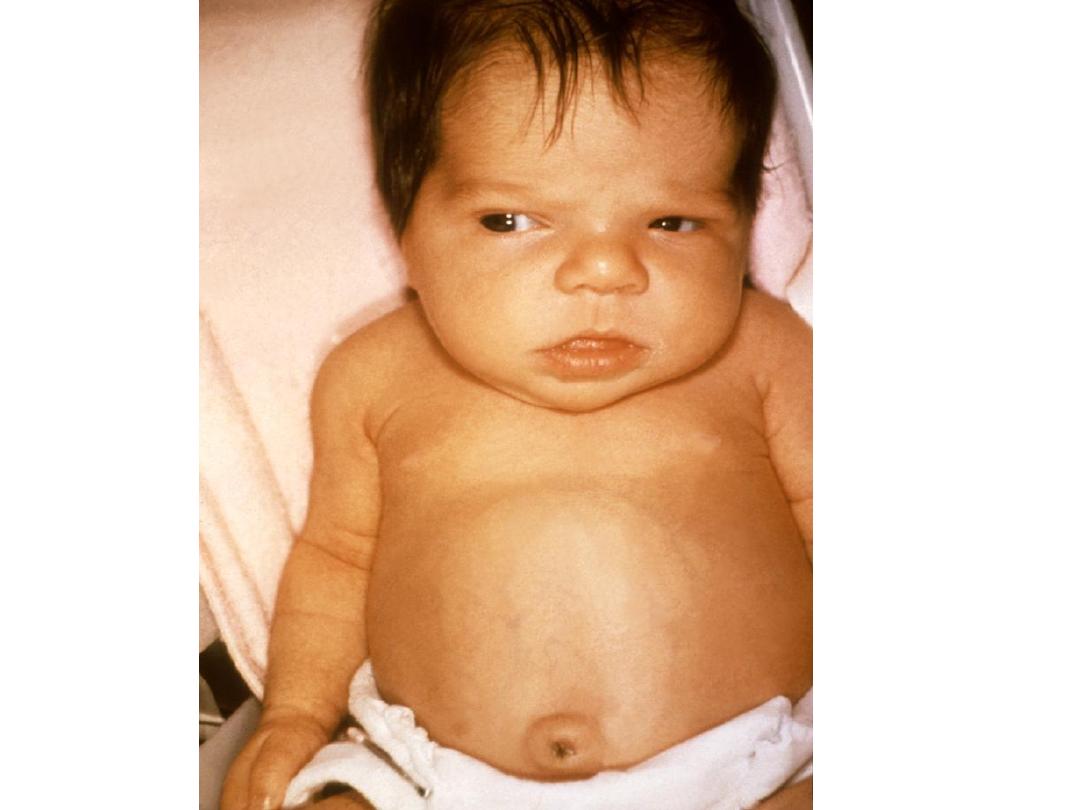
• Congenital hyperthyroidism can occur
through TSH receptor stimulating
antibodies which cross the placenta.
Iodine Deficiency:
• In iodine deficiency, the maternal thyroid
gland has a greater affinity for iodide than
the placenta and the fetuses are thus
prone to cretinism, the leading
preventable cause of mental retardation
worldwide.

• The fetal cochlea, cerebral neocortex and basal
ganglia are particularly sensitive to iodine
deficiency.
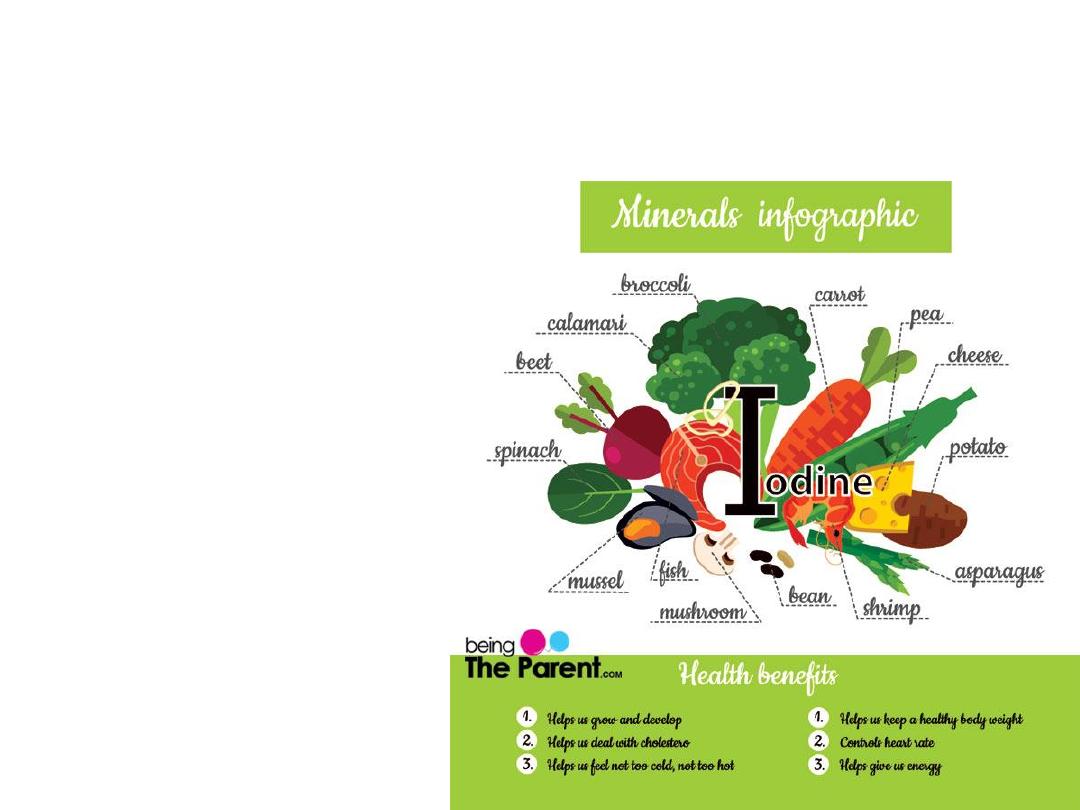
• Iodine administration
prior to conception
and up to the 2nd
trimester will improve
neurological outcome
by protecting the fetal
brain. Iodination of
water, salt or flour can
easily achieve this.
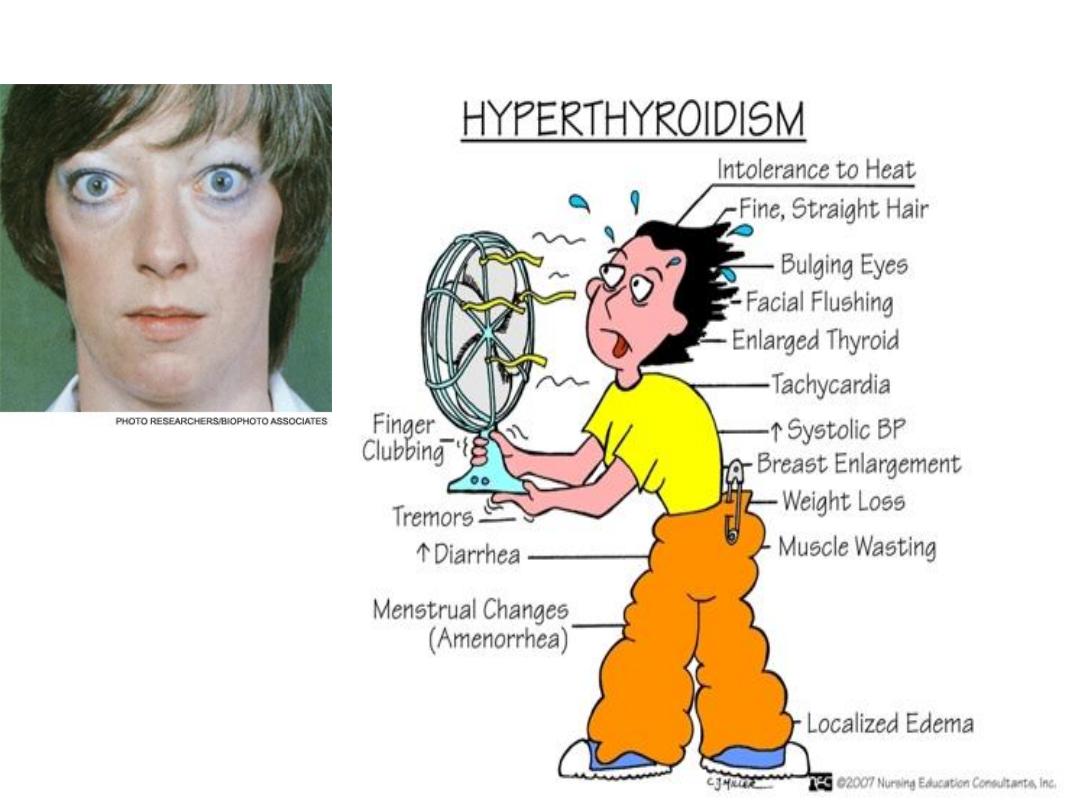
Hyperthyroidism

• occurs in approximately 1 in 500
pregnancies and is usually due to Graves'
disease
• Disease severity is correlated to IgG
thyrotropin receptor stimulating antibody
levels.
• Typical signs of hyperthyroidism are
difficult to elicit in pregnancy, but poor
weight gain in the presence of a good
appetite or a tachycardia can aid Dx.

• Maternal and fetal complications include
thyroid storm, heart failure and maternal
hypertension. Also increased rates of
premature labour, intrauterine growth
restriction and stillbirth.
Treatment:
• radioactive iodine must not be given.
• Surgery may be considered if medical
treatment fails or there is a clinical suspicion
of cancer or compressive symptoms due to a
goitre.

• Medical treatment involves
propylthiouracil PTU and carbimazole.
Both drugs cross the placenta in the same
proportion & are equally beneficial and
the dose of either can be titrated against
maternal well-being and biochemical
status.
• Neither PTU nor carbimazole is thought
to be teratogenic.
• It is recommended that thyroid function
tests be performed every 4-6 weeks.
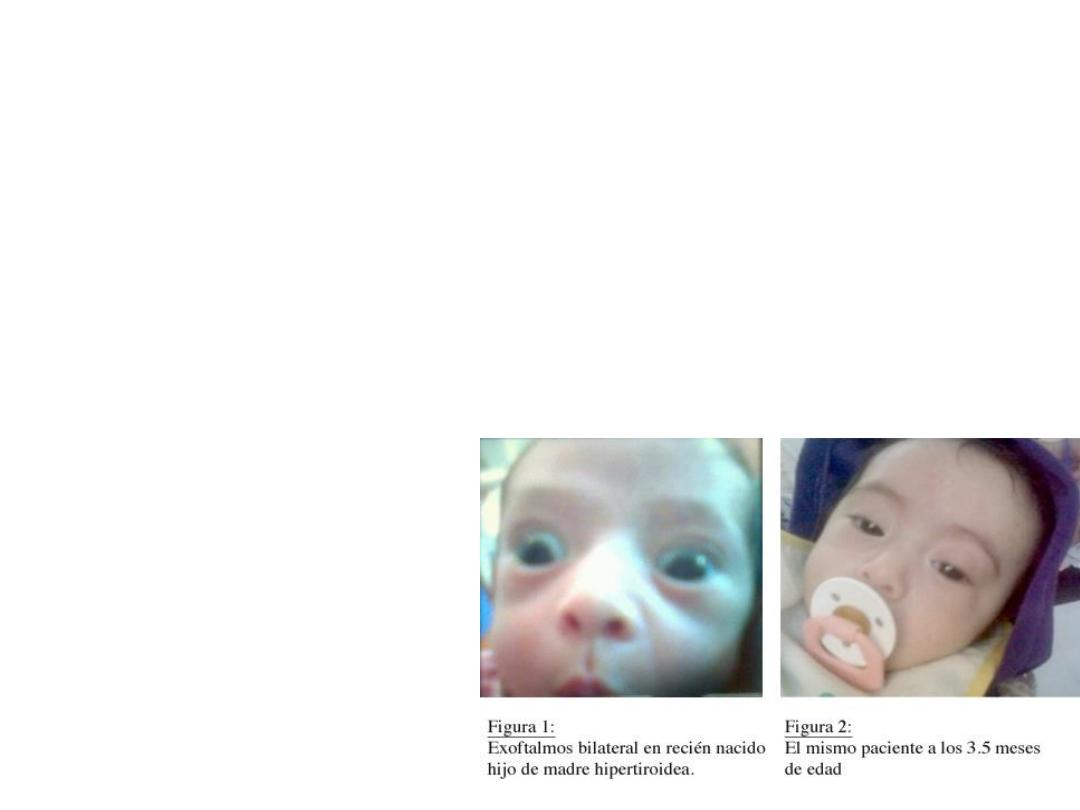
Fetal hyperthyroidism
• When maternal thyrotropin receptor
stimulating antibodies cross the placenta, they
can cause fetal or neonatal thyrotoxicosis. The
fetal thyroid is capable of responding to these
antibodies after 20 weeks' gestation.

• Assessment include maternal perception
of fetal movements and measurement of
the fetal heart rate, which is >160 bpm.
An ultrasound scan used to exclude a
fetal goitre or fetal growth restriction.
• In suspected cases cordocentesis for free
T4 & TSH estimation can be performed.
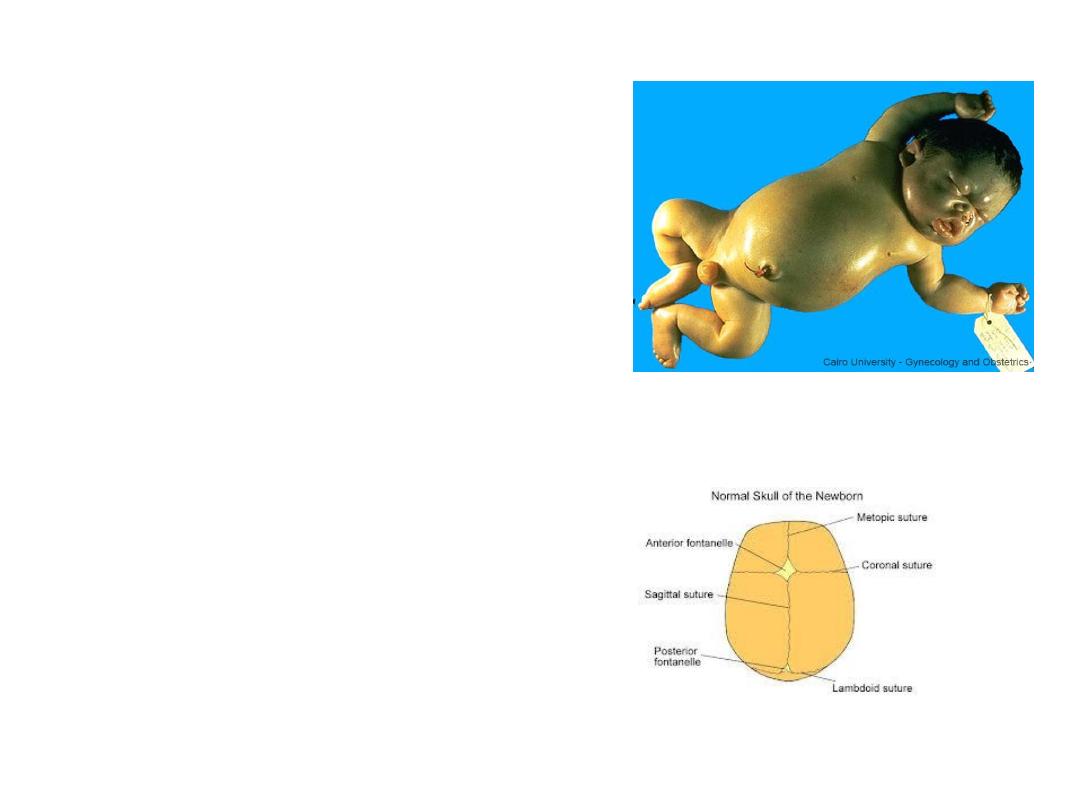
• Complications include
Premature delivery,
hydrops fetalis and
death.
• fetal goitre can cause
polyhydramnios and an
obstructed delivery.
• The condition is also
associated with
craniosynostosis and,
intellectual impairment.

• The fetus can be effectively treated by
maternal administration of antithyroid agents,
which cross the placenta. The fetal heart rate
can be used to titrate the dose of antithyroid
drugs

Hypothyroidism:
• Incidence: 1% of pregnant women and is
usually due to autoimmune Hashimoto's
thyroiditis or idiopathic myxoedema.
• There is a reduced IQ in babies of women with
hypothyroidism that are not adequately treated,
or that goes unrecognized. The insult is likely
to occur in the first trimester, and therefore
pre-conceptual optimization of T4 therapy is
important

• The classical symptoms of hypothyroidism are
common to pregnancy and cannot be relied
upon to discriminate onset or worsening of the
disease. The management is therefore based
principally on biochemical measures ( TFT).
• Thyroxine is titrated against biochemical
results and is safe in pregnancy and lactation.
As long as the patient is clinically euthyroid,
thyroid function test should be performed
every 2-3 months.

Postpartum thyroiditis:
• occur up to a year following delivery and
can manifest as high or low T4 levels.
• Associated with thyroid antiperoxidase
antibodies. Histology suggests a chronic
thyroiditis with lymphocytic infiltration.
• The disease may present initially between
1 and 3 months postpartum with
thyrotoxicosis and later with
hypothyroidism.
• Hyperthyroidism is due to destruction of
thyroid follicles & release of preformed
hormones. The destruction of thyroid
follicles ultimately leads to hypothyroid
phase. A course of T4 may be necessary.
• The period of hypothyroid state is variable,
and permanent hypothyroidism can result.
• The condition may recur in future
pregnancies and follow up is needed to
ensure that permanent hypothyroidism does
not occur.

Pituitary tumours in pregnancy
• Hyperprolactinaemia is an important cause of infertility and
amenorrhoea, and is most often due to a benign pituitary
microadenoma. Macroadenoma (>1 cm adenoma) can be found
• The diagnosis is confirmed with a combination of measurement of
the prolactin level and computed tomography (CT) or magnetic
resonance imaging (MRI) scanning of the pituitary fossa.
• In 80% of cases it is treated with a dopamine agonist
(bromocriptine or cabergoline), which causes the tumour to reduce
in size.
• Larger tumours may require surgery or radiotherapy, which is best
undertaken before pregnancy.

• The pituitary gland enlarges by 50% during pregnancy, but it is
rare for microadenomas to cause problems.
• Serial prolactin levels are unhelpful for monitoring tumour
growth in pregnancy.
• Bromocriptine and cabergoline stopped in pregnancy, and
visual fields and relevant symptoms such as frontal headache
are monitored.
• If there is evidence of tumour growth during pregnancy,
bromocriptine or cabergoline should be recommenced, and
appropriate neuroimaging arranged.
• In women with macroadenomas (>1 cm), it is advisable to
continue with dopamine agonists because of the risk of the
tumour enlarging under oestrogen stimulation.
Epilepsy in
pregnancy
• Incidence : 1 in 200 pregnancies
• Pre-pregnancy counselling
• Alter medication according to seizure frequency
• Reduce to monotherapy where possible & ensure
compliance
• Pre-conceptional folic acid 5 mg

• Explain risk of congenital malformation:
anticonvulsant medications are associated
with a two- to three-fold increased risk of fetal
abnormality
• Explain risk from recurrent seizures

• Many factors contribute to altered drug metabolism
in pregnancy and result in a fall in anticonvulsant
drug levels.
• The reasons for increased fit frequency in
pregnancy therefore include:
the effect of pregnancy on the metabolism of
anticonvulsant drugs
sleep deprivation or stress
poor compliance with medication.

• Polytherapy increases the risk of major congenital abnormality by
about 3% for each additional AED (antiEpileptic Drug).
• The major fetal abnormalities associated with anticonvulsant drugs
(including sodium valproate, carbamazepine, phenytoin,
phenobarbitone) are neural tube defects, facial clefts and cardiac
defects.
• detectable by ultrasound and therefore all women should be
offered detailed anomaly scanning.
• In the case of valproate, the likelihood of these effects is dose
dependent (>1,000 mg/day) and it should be avoided in pregnant
women, except when epilepsy cannot be controlled with other
AEDs.

• Delivery mode and timing is largely unaltered by
epilepsy
• Anticonvulsant medication should be continued
during labour.
• Breastfeeding can be encouraged, feeding is best
avoided for a few hours after taking medication.
• Information on safe handling of the neonate should
be given to all epileptic mothers.

Causes of seizures in pregnancy
• Epilepsy
• Eclampsia
• Encephalitis or meningitis
• Space-occupying lesions (e.g. tumour, tuberculoma)
• Cerebral vascular accident
• Cerebral malaria or toxoplasmosis
• Thrombotic thrombocytopenic purpura
• Drug and alcohol withdrawal
• Toxic overdose
• Metabolic abnormalities (e.g. hypoglycaemia)

Migraine
• Migraine is influenced by cyclical changes in the sex
hormones, and attacks often occur during the menstrual
period, attributed to a fall in oestrogen levels.
• Migraine often improves in pregnancy, worsening of
headaches occurring infrequently.
• Throughout pregnancy around 20% of pregnant women will
experience migraine-like headache.
• Obstetric complications are not increased in migraine
sufferers.
• Migraine during pregnancy should be treated with analgesics,
antiemetics and, avoidance of factors that trigger the attack.
• Low-dose aspirin or beta-blockers may be used to prevent
attacks.

Bell’s palsy
• The incidence of Bell’s palsy is increased 10-
fold during the third trimester of pregnancy.
• The outcome is generally good and complete
recovery is the norm if the time of onset is
within 2 weeks of delivery.
• The role of corticosteroids and antivirals is
controversial but both can be used in
pregnancy and they may hasten recovery if
given with 24 hours of the onset of symptoms.
Thank You
