Respiratory Diseases in
Pregnancy
Dr.Nadia Mudher Al-Hilli
FICOG
Assistant Prof at
Department of Obs&Gyn
College of Medicine
University of babylon
Objectives
Learn how to deal with common respiratory
problems during pregnancy including:
Pneumonia
Asthma
the new world wide infection with Corona Virus
( COVID-19 )
Physiological changes in pregnancy
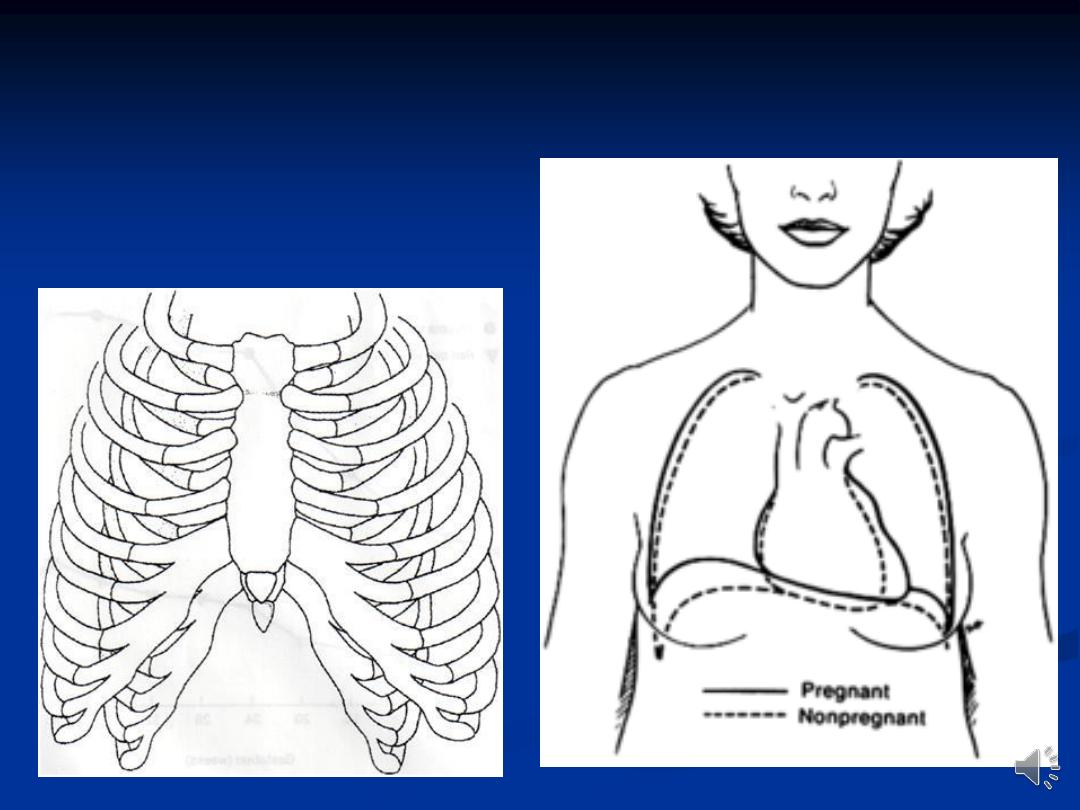
Dyspnea is experienced by approximately half of all
pregnant women by 20 weeks gestation because of
high progesterone levels which acts via the
Hypothalamus to increase respiratory drive.
Anatomically, the lower chest wall circumference
increases by 5-7 cm, the diaphragm is elevated 4-5
cm by term & the costal angle widens. These
changes occur due to the pressure from the expanding
uterus & the relaxation of thoracic ligaments.
Respiratory infection
pregnancy is a significant risk factor for the development of
severe respiratory disease attributable to viral infection.
a seasonal flu vaccine is recommended in pregnancy.
Viral pneumonia follows a more complicated course in
pregnancy and women often decompensate more quickly.
Prompt treatment and early involvement of respiratory and
infectious disease specialists in addition to the intensive care
is essential.
Bacterial pneumonia should be treated with penicillin or
cephalosporins usually the first choice, and erythromycin
used if atypical organisms are suspected.
Pneumonia: warning signs
Respiratory rate >30/minute.
Hypoxaemia; pO2 <7.9 kPa on room air.(
normal >10.5 kpa
Acidosis; pH <7.3. (normal 7.35-7.45)
Hypotension.
Disseminated intravascular coagulation.
Elevated blood urea.
Evidence of multiple organ failure.
Coronavirus (COVID-19) Infection in
Pregnancy
Novel coronavirus (SARS-COV-2) is a new strain of
coronavirus causing COVID-19
Pregnant women do not appear to be more likely to
contract the infection than the general population.
Vertical Transmission: antepartum or
intrapartum is probable.
Effect on the mother: majority mild or
moderate cold/flu like symptoms. changes to
their immune system in pregnancy can be
associated with more severe symptoms.
Effect on the fetus: no increased risk of
miscarriage or early pregnancy loss in relation to
COVID-19. no teratogenic effects.
Attendance for routine antenatal care in women with
suspected or confirmed COVID-19: should be
delayed until after the recommended period of
isolation
Women attending for intrapartum care with
suspected/confirmed COVID-19 and no/mild
symptoms: encouraged to remain at home (self-
isolating) in early (latent phase) labour.
When attend the maternity unit, settled in an isolation
room, a full maternal and fetal assessment should be
conducted to include:
• Assessment of the severity of COVID-19 symptoms
should follow a multi-disciplinary team approach
• Maternal observations including temperature,
respiratory rate and oxygen saturations
• Confirmation of the onset of labour
• Electronic fetal monitoring using cardiotocograph
(CTG)
If the woman has signs of sepsis, investigate & treat but
also consider active COVID-19 as a cause of sepsis.
Mode of birth should not be influenced by the presence
of COVID-19, unless the woman’s respiratory condition
demands urgent delivery.
epidural or spinal analgesia or anaesthesia are not
contraindicated in the presence of coronaviruses.
They minimise the need for general anaesthesia if urgent
delivery is needed, and better than Entonox which may
increase aerosolisation and spread of the virus.
If Entonox is used then the breathing system must
contain a filter to prevent contamination with the virus.
In case of deterioration in the woman’s
symptoms, decision of proceeding to emergency
caesarean birth if this is likely to assist efforts to
resuscitate the mother
steroids for fetal lung maturation cause no harm
in the context of COVID-19.
Asthma in Pregnancy
The prevalence of asthma in pregnancy is about
3 –12 per
cent.
Effect of pregnancy on asthma severity:
stable in one-third of women, worsens in another third and
improves in the remaining third.
most episodes occur between 24 and 36 weeks of pregnancy
The potential benefit of pregnancy-induced immune system
modulation & progesterone-mediated bronchodilatation
may be opposed by the reluctance of patient & physician to
treat asthma for the fear of harming the fetus through drug
exposure.
The effect of asthma on pregnancy:
Severe & poorly controlled asthma have a
detrimental effect on pregnancy including:
intrauterine growth restriction
hypertensive disorders
preterm labour
intrauterine fetal death.
Labour and delivery : are not usually affected by
asthma and attacks are uncommon in labour.
Postpartum, there is no increased risk of
exacerbations and those whose asthma deteriorated
during pregnancy have usually returned to pre-
pregnancy levels by three months after birth.
Management of asthma in pregnancy:
Same as in non-pregnant patient. Prevention is the
key & known triggers of exacerbations should be
avoided .
Short-acting & long-acting beta2-agonists, inhaled
steroids & theophylline can be used in pregnancy.
These drugs will suffice for mild to moderate
asthmatics
Epinephrine should be avoided in the pregnant
patient. it can lead to possible congenital
malformations, fetal tachycardia, and
vasoconstriction of the uteroplacental circulation

Women with more severe asthma who have
stabilized on leukotriene receptor antagonist
(montelukast) may continue them through out
pregnancy.
Prednisolone is the oral steroid of choice in
pregnancy, as 88 % of it is metabolized by the
placenta, limiting fetal exposure.
The teratogenic risk & possible harmful fetal
effects of maternal steroid treatment remain an
area of controversy.

Managing pregnancy in asthmatic patients:
For those with poorly controlled or severe
asthma , care should be multidisciplinary.
Baseline investigations, such as peak flow
measurements should be obtained at booking.
Medical treatment should be optimized, with
repeated reassurance about the use of
necessary drugs in pregnancy.
Women taking Prednisolone should be
screened for glucose intolerance

Labour & delivery:
Parenteral steroid cover may be needed for those who are on
regular steroids
regular medications should be continued throughout labour .
bronchoconstrictors, such as ergometrine or prostaglandin
F2α, should be avoided.
Adequate hydration is important.
regional anaesthesia favoured over general, to decrease the
risk of bronchospasm, provide adequate pain relief and to
reduce oxygen consumption and minute ventilation.
Breast feeding
is not contraindicated with any
of the medications used although high-dose oral
steroid use ( ≥ 40 mg per day )carries a risk of
neonatal adrenal suppression

