
1
كلية الطب
⁄
جامعة بابل
المرحلة الرابعة
د
-
نسرين مالك
Obstetrics
The placenta, Membranes , And Umbilical cord
Placenta
:-The placenta is a usually regarded as a fetal organ , it is essential for normal
fetal growth , development, and for maintenance of a healthy pregnancy. The placenta fulfills
several critical roles like it preventing rejection of the fetal allograft; transporting and
metabolizing nutrients, and providing peptide and steroid hormones.
Developmental anatomy and structure:-
Development of the placenta and fetus is a continuous process that begins at the time of
fertilization.
The morula enter the uterine cavity 4 days after fertilization and fluid filled space (single
cavity) is formed, the embryo at this stage known as blastocyst.
The cells of the inner cell mass known as embryoblast are located at one pole, while of the
outer cell known as trophoblast, flattened to form the epithelial wall of blastocyst.
The blastocyst is bathed in uterine secretions that provide the embryo with oxygen and
metabolic substrates. However, this soon becomes inadequate for further development
therefore the embryo must implant in the uterine wall.
Implantation results from the action of trophoblast cells that develop over the surface of the
blastocyst. These cells secrete proteolytic enzymes that digest the adjacent cells of the uterine
endometrium. At the beginning of the 2nd week , the blastocyst is partially embedded in the
endometrial stroma .
The trophoblast, which form the epithelial wall of blastocyst
differentiates into 2 layers :
1- An inner ,actively proliferating layer(the cytotrophoblast).
2-An outer layer(the syncytiotrophoblast ).
The outer layer(the syncytiotrophoblast) is originated from the inner layer(the cytotrophoblast).
By day 9 lacuna develop in syncytiotrophoblast., subsequently, these syncytiotrophoblast
eroded maternal sinusoid, and this permit maternal blood to enter the lacunar network, so by
the end of the 2nd week, a primitive uteroplacental circulation begins.
2
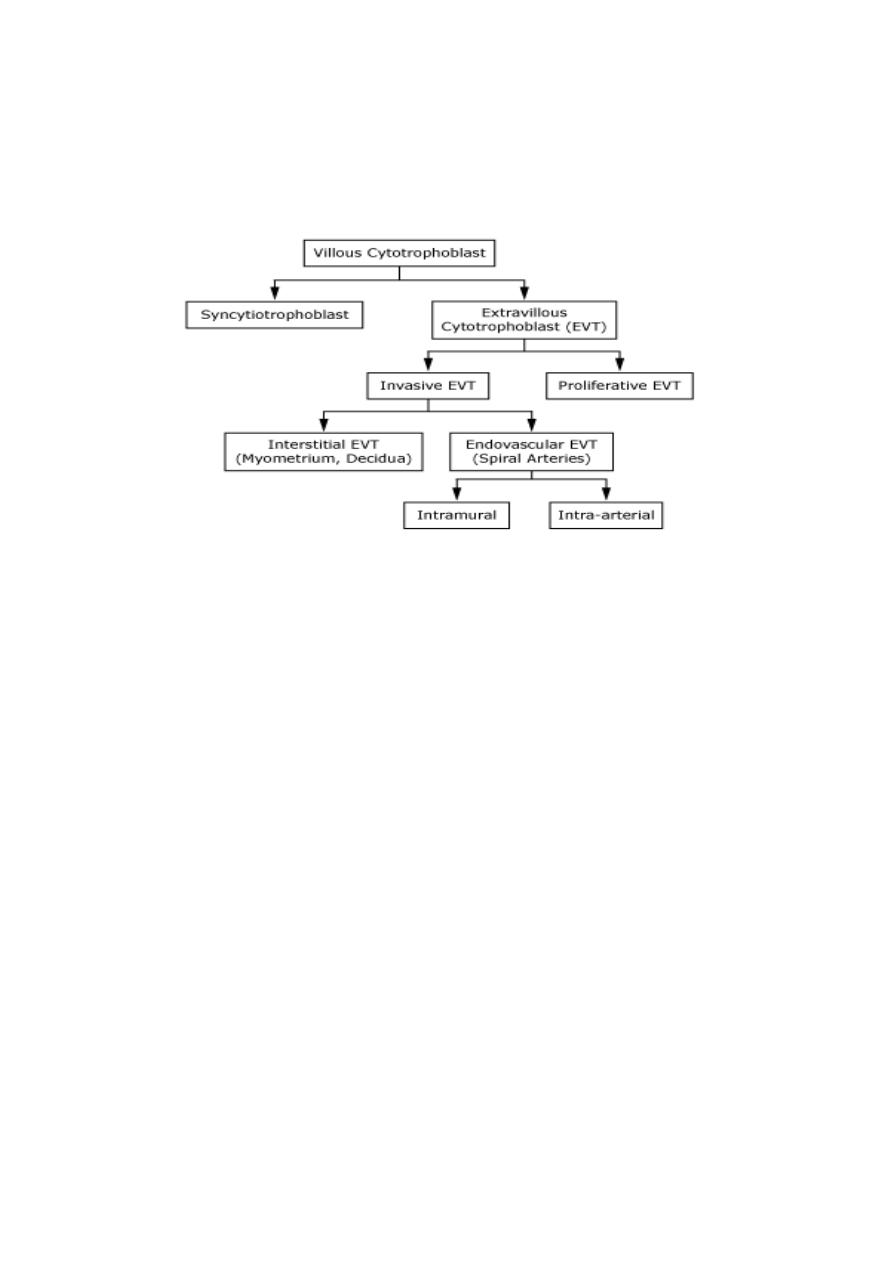
The progenitor villous cytotrophoblast cell is the stem cell of the placenta. It proliferates
throughout gestation, differentiating along two pathways to extravillous trophoblast (EVT) and
the syncytiotrophoblast ,as show in following figure.
The extra villous trophoblast ( EVT )is responsible for invasion, thereby anchoring the
placenta to the decidua and myometrium.
The syncytiotrophoblast is a specialized epithelium covering the villous tree and has several
functions, such as transport of gases, nutrients, waste products and synthesis of peptide and
steroid hormones that regulate placental, fetal, and maternal systems.
Alterations in villous trophoblast differentiation are seen in various pathophysiological
situations and may underlie several pregnancy disorders.
Endovascular EVTs are associated with spiral arteries, either within the vessel wall
(intramural) or replacing endothelium (intra-arterial). The endovascular EVTs transform the
narrow spiral arteries to wide uteroplacental arteries, which distribute blood into a low
resistance vascular network .
Defects in EVT invasion occur with preeclampsia and intrauterine growth restriction (IUGR),
where some spiral arteries are not invaded at all and some are superficially invaded, leading to
lack of the normal physiological adaptation of spiral arteries to pregnancy, reduced blood flow
into the intervillous space, and relative hypoxia/ischemia.
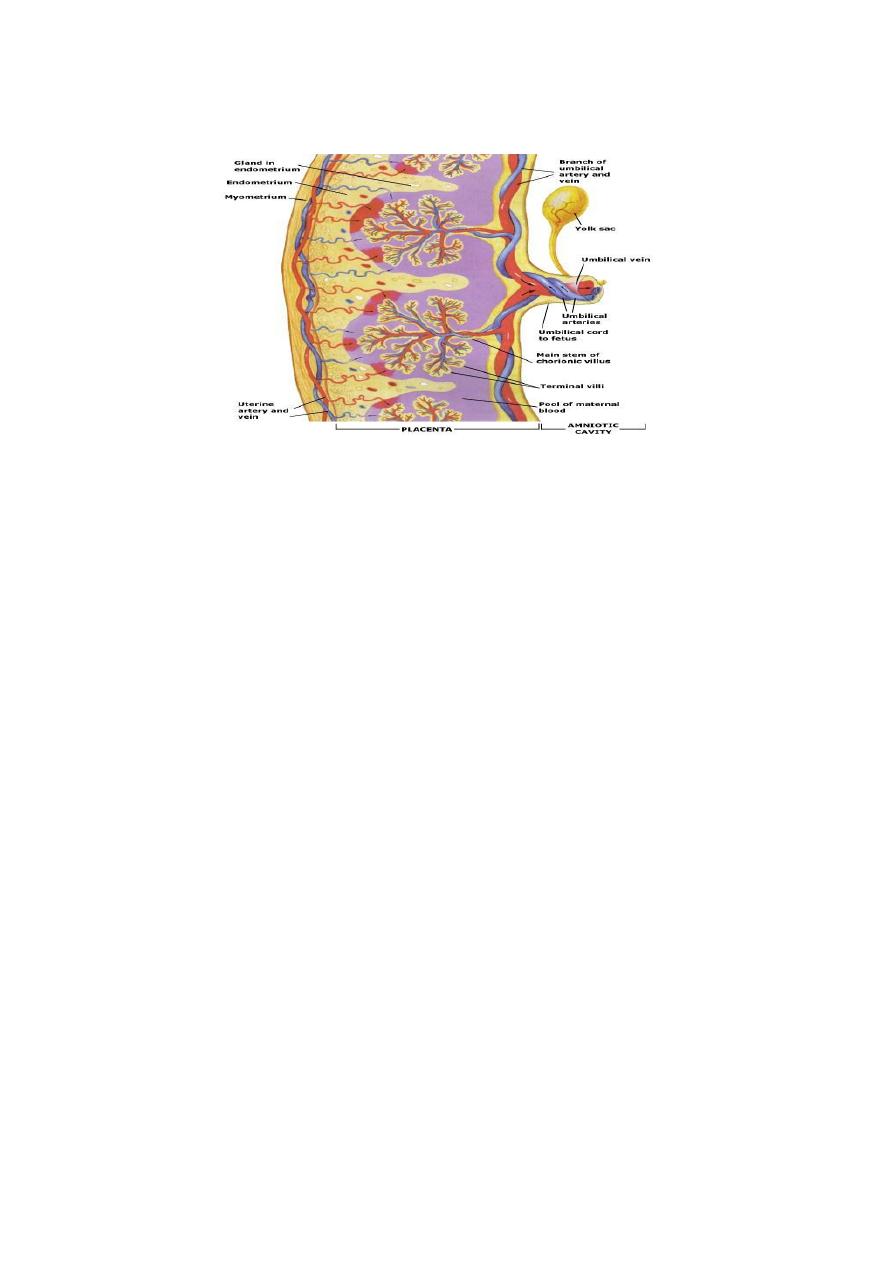
Vasculature of placenta:-
The proportion of the placenta occupied by blood vessels increases throughout gestation to
facilitate nutrient transport. The two umbilical arteries and one vein divide into networks of
secondary vessels, and then further divide into tertiary vessels before penetrating the chorionic
plate and entering the main stem villi. These then divide two to five times to form rami chorii
3
(intermediate villi) and further divide to form ramuli chorii, some of which terminate in the
terminal villi, which are the functional units of exchange as shown in following figure.
The terminal villi each contain up to 10 capillaries which form capillary loops and occasional
sinusoids, perhaps to reduce resistance and slow blood flow in order to maximize time for gas
and nutrient exchange.
The two umbilical arteries are carry deoxygenated blood from the fetal vessels to the placenta
then to the maternal veins in the decidua, while the one vein carries oxygenated blood from
maternal spiral arteries to the fetal circulation.
Gross structure of placenta:-
By the beginning of the 4th month , the placenta has 2 components:
1- A fetal portion:- formed by chorion frondosum ( the villli on embryonic pole , continue to
grow and expand ,thus giving rise to chorion frondosum).
2-A maternal portion:-formed by decidua basalis.
On the fetal side ,the placenta is bordered by the chorionic plate; on its maternal side, it is
bordered by the decidua basalis. Between the chorionic plate and decidual basalis there is a
space called the choriodecidual space (intervillous space) which contains maternal blood.
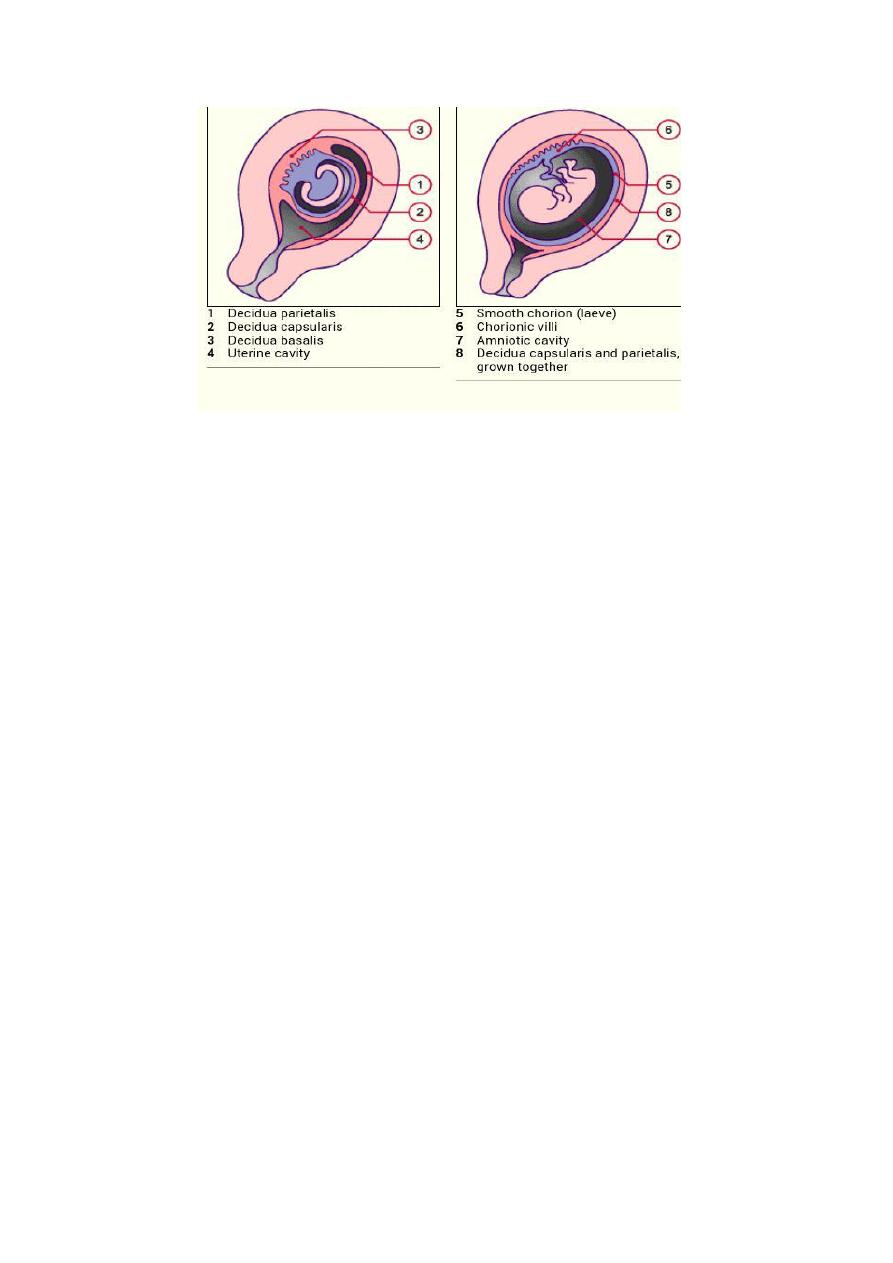
Decidua
: Is endometrium of the uterus after implantation, it consisting of 3 parts depending
on its relationship with the embryo;
1- Decidua basalis; where the implantation takes place and the basal plate is formed.This can
be subdivided into a zona compacta and zona spongiosa( where the detachment of the placenta
take placefollowing birth).
2- Decidua capsularis; lies like a capsule around thechorion.
3- Decidua parietalis; lining the opposite uterus wall.
After the 4 th month the growing fetus brings the deciduae capsularis into contact with the
deciduas parietalis .
The fusion of the two deciduas leads to the disappearance of the uterine cavity.
4
During the 4th and 5th months ,the decidua forms a number of septa, the decidual septa, which
project into the intervillous space but do not reach the chorionic plate, as result of this septum
formation, the placenta is divided into a number of compartments which are called cotyledons,
the mature human placenta has about 15-28 cotyledones, each consisting of fetal
vessels,chorionic villi, and intervillous space.
Since the decidual septa do not reach the chorionic plate ,contact between the intervillous
spaces in the various cotyledons is maintained.
As a result of fetus growth and uterus expansion ,the placenta also enlarged. The
enlargement of its surface area is roughly parallel to that of the expanding uterus, and through
out pregnancy it covers approximately 15-30 ٪of the internal surface of the uterus.
Circulation of placenta:-
Cotyledon receive their blood through 80-100 maternal spiral arteries that pierce the
decidual plate and enter the the choriodecidual space (intervillous space) .
The lumen of spiral artery is narrow ,resulting in an increased blood pressure when enter the
intervillous space, this pressure forces the blood deep into the intervillous spaces and bathes
numerous small villi ( of villous tree ) in oxygenated blood, then this blood carries to the fetus
through the single umbilical vein to the fetal circulation, while the deoxygenated blood that
coming from fetal body carries via the 2 umbilical arteries back to the placenta.
As the pressure decreases, blood flows back from chorionic plate toward the decidua, then to
maternal circulation through endometrial veins.
Since the maternal blood in the intervillous space is separated from fetal blood by a chorionic
derivative, the human placenta is consider to be of hemochorial type.
The maternal blood flow to the placenta increases throughout pregnancy from 50 ml\min in
the first trimester to 600 ml\min at term.

5
Full term placenta:-
At full term ,the placenta has a discoid shape , a diameter of 22-25
cm , central thickness 2.5-3 cm, and has a weight of about 450-500 gm.
After the birth of the child , the placenta is torn from the uterine wall at approximately 15- 30
minutes , and then expelled from the uterine cavity.
After birth , if the placenta is viewed from the maternal side , usually there are 15 -20
superficial cotyledons covered by a thin layer of decidua basalis are clearly recognizable.
The fetal surface of the placenta is covered entirely by the chorionic plate. A number of large
arteries and veins (the chorionic vessels) are converge toward the umbilical cord . The chorion
in turn covered by the amnion
.
Attachment of the umbilical cord is slightly eccentric .
Function of placenta:-
1-Gases and nutrient exchange( transporting and metabolizing nutrients).
2- Prevention of the fetal allograft rejection.
3-Metabolic functions:-In addition to gases and nutrient exchange, the placenta is capable of
synthesizing glycogen and cholesterol, which are energy sources to the developing fetus.
Additionally, cholesterol is an important precursor for hormone production by the feto-
placental
unit,
also
has
a
rule
in
protein
metabolism
and
lactate
removal.
4-Anticoagulant activity :-
Thrombosis in the placental vasculature can result in
pregnancy loss. To prevent stasis and coagulation of blood in the low velocity intervillous
space, the trophoblast actively secretes substances (nitric oxide and carbon monoxide) that
prevent platelet and leukocyte adhesion and aggregation to the trophoblast surface .
5 -Endocrine function:-The placenta also acts as an important endocrine organ and is
responsible for the release of hormones into both the fetal and maternal circulation. The
hormones produced by the placenta can be split into two categories:
A-
Peptide hormones :-
1-Human chorionic gonadotrophin (hCG). 2-Human placental lactogen(hPL).
3-Cytokines. 4-Growth hormone (GH).
5- Insulin-like growth factors (IGF's). 6-Corticotropin releasing hormone (CRH).
7-Placental growth factor (PIGF).
B-Steroid hormones :- estrogens, progesterone and glucocorticoids.
6-Immunoglobulin G(IgG) transfer :- Maternal antibodies are readily transported across the
placenta to confer immunity to the fetus. From early in the second trimester the concentration
of Immunoglobulin G (IgG) in fetal blood increases, with most antibodies being acquired in
the third trimester.
7-Imprenting genes:- Imprinting refers to the differential expression of genetic material
depending on whether it was inherited from the male or female parent.
6
Abnormal placentation:-
A-Abnormal trophoblast invasion:-
Pre-eclampsia,intrauterine growth retardation(IUGR) and abruption placenta are clinical
manifestations of total or patchy failure of trophoblast invasion of the myometrial segments of
the spiral arteries.
There are other general conditions associated with impaired perfusion of the placenta, such as
collagen vascular disease, antiphospholipid syndrome , sever diabetes mellitus and chronic
hypertension. All of these result in a small placenta with gross morphological changes. The
most serious of these changes are:-
1-Infarcts. 2-Basal haematomas.
An infarct represents an area of ischaemic necrosis of a cotyledon resulting from spiral artery
occlusion, usually by thrombosis, this usually seen in intrauterine growth retardation(IUGR).
Closely associated with infarcts are placental haematomas, which consist of a mass of blood in
the center of the fetal cotyledon due to rupture of a damaged spiral artery. This is also
associated with maternal hypertension. These pathological lesions should not be confused with
calcification or fibrin deposition in the placenta, which can often give it an unhealthy
appearance , but are benign.
B-Abnormal placental attachment:-
Normally the placenta attach to the deciduas and the superficial part of the myometrium .
Some times the placenta attaches itself into the wall of the uterus too deeply , this can cause
problems including:-
1- Placenta accrete:- the placenta attaches itself too deeply , and too firmly into the
uterus.
2- Placenta increta:- the placenta attaches itself even more deeply into the muscle wall
of the uterus.
3- Placenta percreta:- the placenta attaches itself and grows through the uterus ,
sometimes extended to nearby organs, such as bladder.

7
Membranes:-
The placental membranes are composed of two layers; the layer nearest
the fetus (facing the amniotic cavity) is the amnion, the layer immediately beyond it is the
chorion.
The amnion forms on day 8 in three phases as follow:
1-Blastocystic phase; whereas the amnion lies between the epiblast and trophoblast.
2-Chrionic vesicle stage; it is floored by the ectoderm and roofed by the primary mesoderm.
3-A clear, watery amniotic fluid stage (contained in the amniotic cavity) surrounding all the
embryonic aspects after folding.
The chorion is the outermost fetal membrane around the embryo. this membrane has an upper
layer of minimally cellular fibrous tissue and, more importantly, an epithelial cellular layer
composed of trophoblast cells adjacent to the decidua. The trophoblast cells of the chorion are
derived from the trophoblast cells which form the entire epithelial lining of the placenta.
Umbilical cord:-
The umbilical cord connects the body of the fetus with the placenta.
It is normally composed of two umbilical arteries and one umbilical vein supported by loose
gelatinous tissue called Wharton's Jelly. The cord increases in length as the fetus grows and it
has a characteristic twist or coil .
The average length is 55 cm, with a wide range typically considered normal (i.e. 35 to 80 cm).
