PARAPNEUMONIC EFFUSION AND
EMPYEMA
Dr.Ahmed Hussein Jasim (F.I.B.M.S)(resp)
Investigations
• Diagnostic pleural tap using US : is essential if pleural infection is
possible and fluid depth is >10mm (smaller effusions can usually be
monitored).
Frankly purulent or turbid/cloudy pleural fluid,
organisms on pleural fluid Gram stain or culture, or pleural fluid ph
<7.2 are all indications for chest tube drainage
. 40% of pleural
infections are culture-negative.
• Contrast-enhanced pleural-phase CT
may be useful both in
supporting the diagnosis and visualizing the distribution of fluid.
• Blood cultures positive in only 40% of cases.
• Bronchoscopy is only indicated if a bronchial obstructing lesion is
suspected.
Management
• Antibiotics all patients with pleural infection should be treated with
antibiotics; refer to local hospital prescribing guidelines.
• Community-acquired
empyema—β-lactam/β-lactamase inhibitor
(e.g. co-amoxiclav) or second-generation cephalosporin (e.g.
cefuroxime), combined with metronidazole for anaerobic cover.
Ciprofloxacin and clindamycin together may be appropriate.
• Hospital-acquired
empyema—cover Gram-positive and Gram-
negative organisms and anaerobes. MRSA infection is common.
Consult with microbiology team. One option is meropenem and
vancomycin.
• Chest tube drainage Indications for chest tube drainage • purulent
pleural fluid • Organisms on pleural fluid Gram stain or culture
•
pleural fluid ph <7.2.
• Intrapleural fibrinolytics
showed that the
combination of
intrapleural alteplase (tpa) and dornase alfa (DNase) significantly
improved CXr appearances for patients with pleural infection ( 1°
outcome) and reduced surgical referral and hospital stay with a
similar adverse event profile (2° outcomes).
• Nutritional support Dietician review; consider supplementary NG
feeding.
• Thromboprophylaxis
• Surgery
Consult with thoracic surgeon if there are ongoing features
of sepsis and residual pleural collection after 5–7 days despite tube
drainage and treatment with antibiotics.
Outcome about 5% of patients require surgery. Empyema 1y mortality is about
5%.
Increased age, renal impairment, low serum
albumin,
hypotension, and
hospital-acquired infection are associated with a poor outcome
. CXr may remain
abnormal despite successful treatment of empyema, with evidence of calcification
or pleural scarring or thickening.
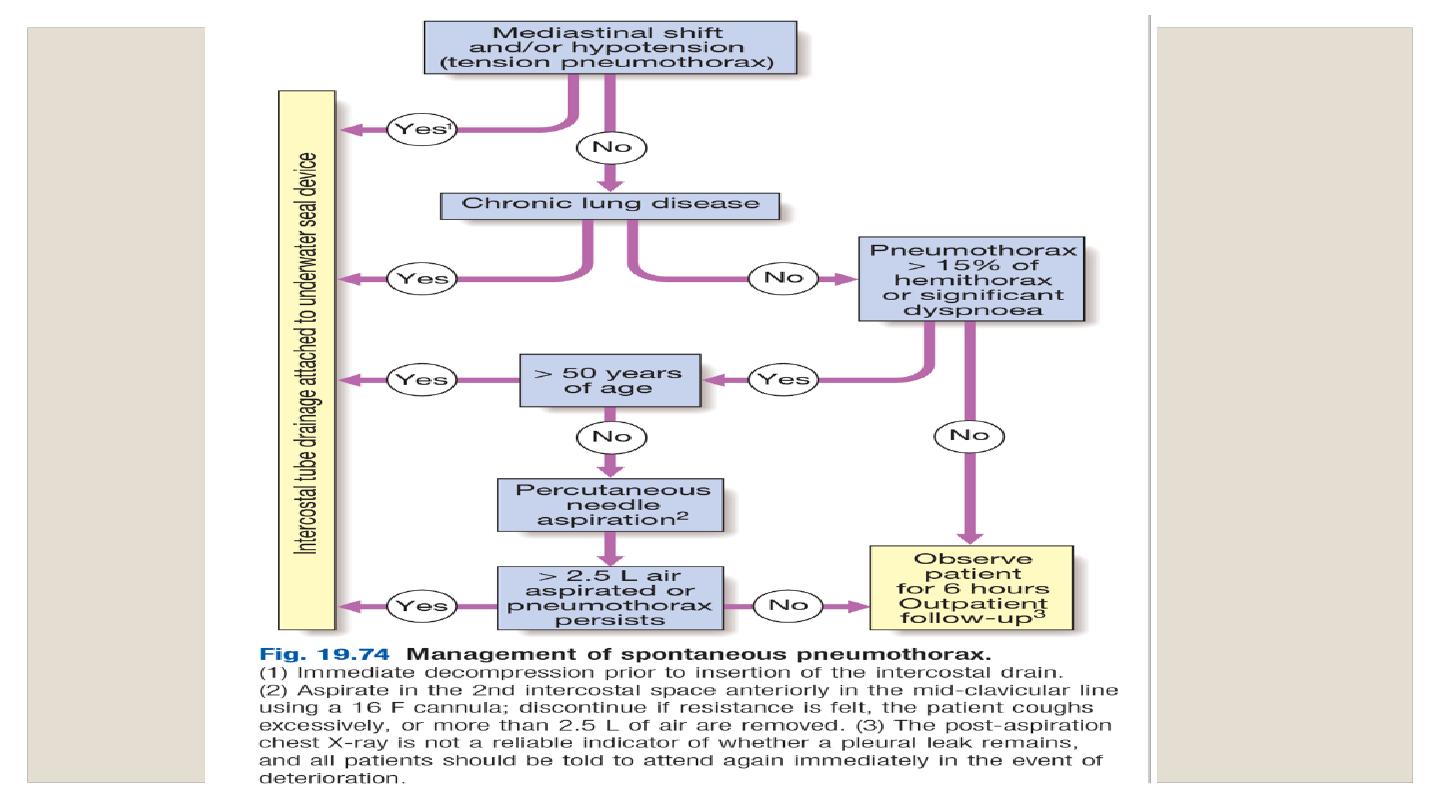
Pneumothorax
Definition a pneumothorax is air in the pleural space. May occur with
apparently normal lungs ( 1° pneumothorax) or in the presence of
underlying
lung disease
(2° pneumothorax).
May
occur
spontaneously or following trauma.
Causes and pathophysiology
1°
pathogenesis is poorly understood; pneumothoraces are presumed to
occur following an air leak from apical subpleural blebs and bullae.
2°
Underlying diseases include: COpD (60% of
cases), asthma, ILD,
necrotizing pneumonia, tB, PCP.
Clinical features
Classically presents with acute onset of pleuritic chest pain and/or
breathlessness.
signs of pneumothorax include tachycardia, hyperinflation, reduced
expansion, hyperresonant percussion note, and quiet breath sounds on
the pneumothorax side.
Investigations
o
CXR is the diagnostic test in most cases, revealing a visible lung edge
and absent lung markings peripherally. Width of the rim of air
surrounding the lung on CXr
may be used to classify
pneumothoraces into small (rim of air measured at level of hilum
≤2cm) and large (>2cm). a 2cm rim of air approximately equates
to a 50% pneumothorax in volume.
o
ABGs frequently show hypoxia and sometimes hypercapnia in 2°
pneumothorax.
o
CT chest
may be required to differentiate pneumothorax from
bullous
disease
and
is
useful
in
diagnosing
unsuspected
pneumothorax following trauma and in looking for evidence of
underlying lung disease.
Prognosis
Risk of recurrence increases with each subsequent pneumothorax; risk
of recurrence is around 30% after a first pneumothorax, about 40%
after a second, and >50% after a third
• Mortality of 2° pneumothorax is 10%