
HYPERTENSION
THE SILENT KILLER

introduction:
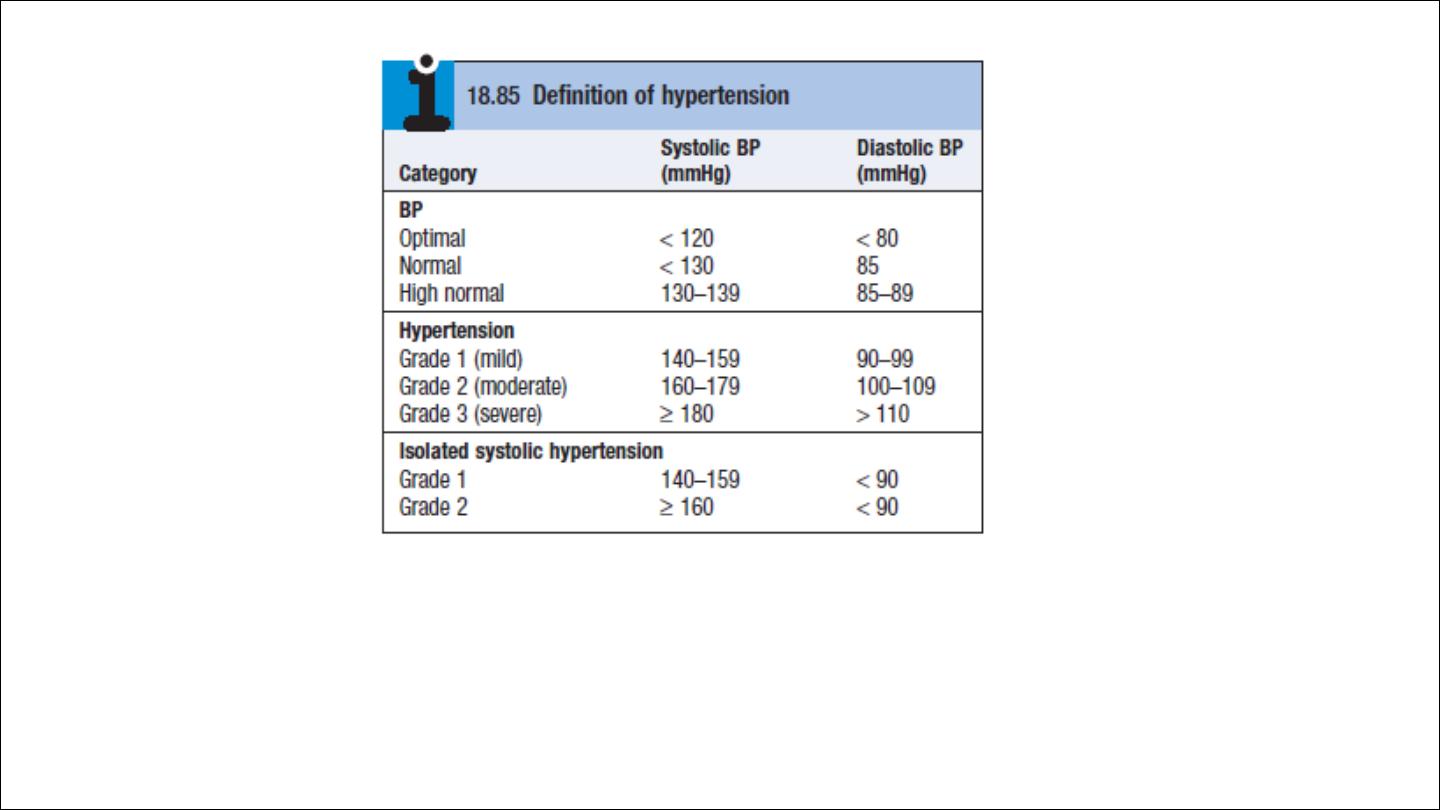
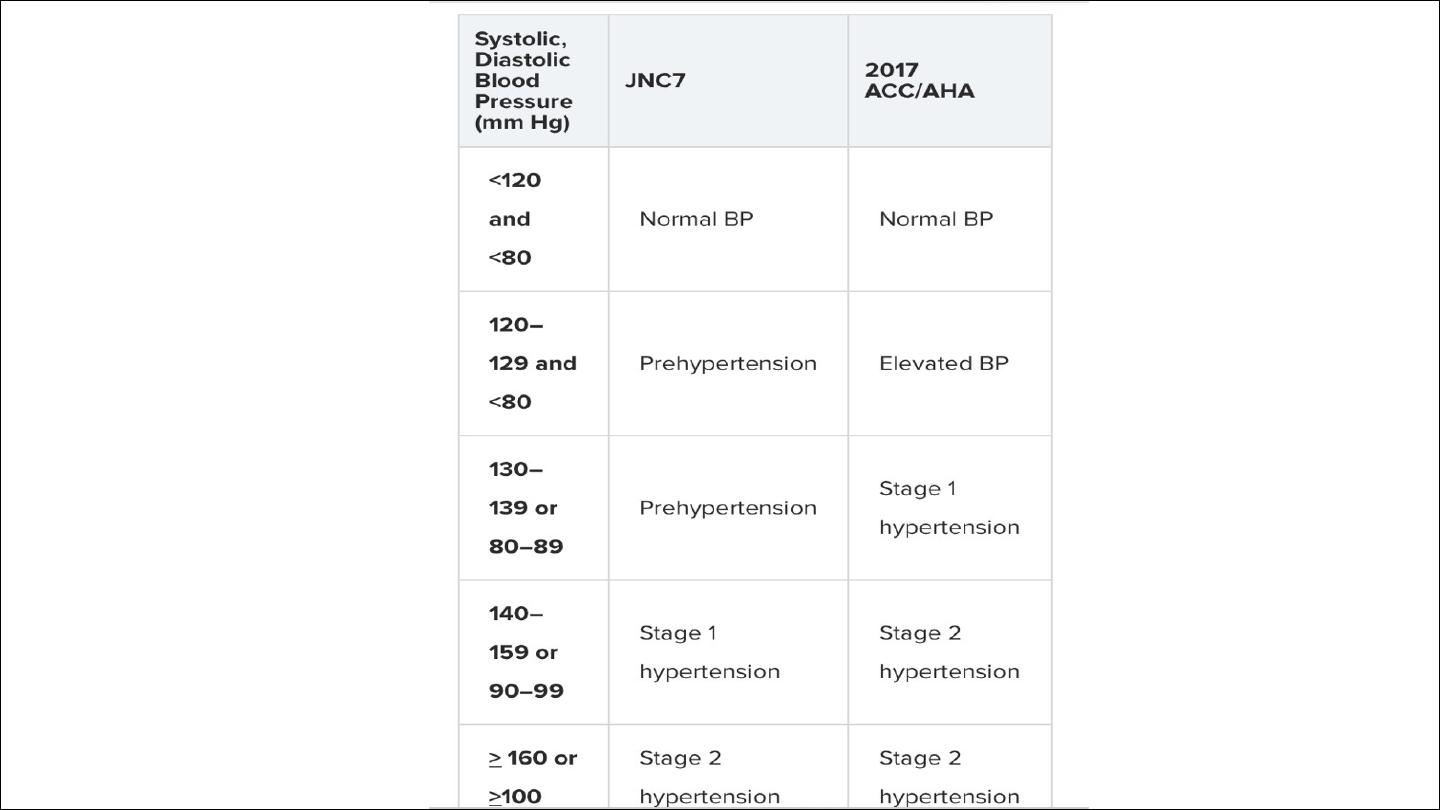
Blood pressure values are continuous variables, so the definition of
hypertension is arbitrary. Systemic BP rises with age.
incidence of cardiovascular disease (particularly stroke and coronary
artery disease) is closely related to average BP at all ages, even when
BP readings are within the so-called ‘normal range.
The cardiovascular risks associated with BP depend upon the
combination of risk factors in an individual, such as age, gender, weight,
physical activity, smoking, family history, serum cholesterol, diabetes
mellitus and pre-existing vascular disease
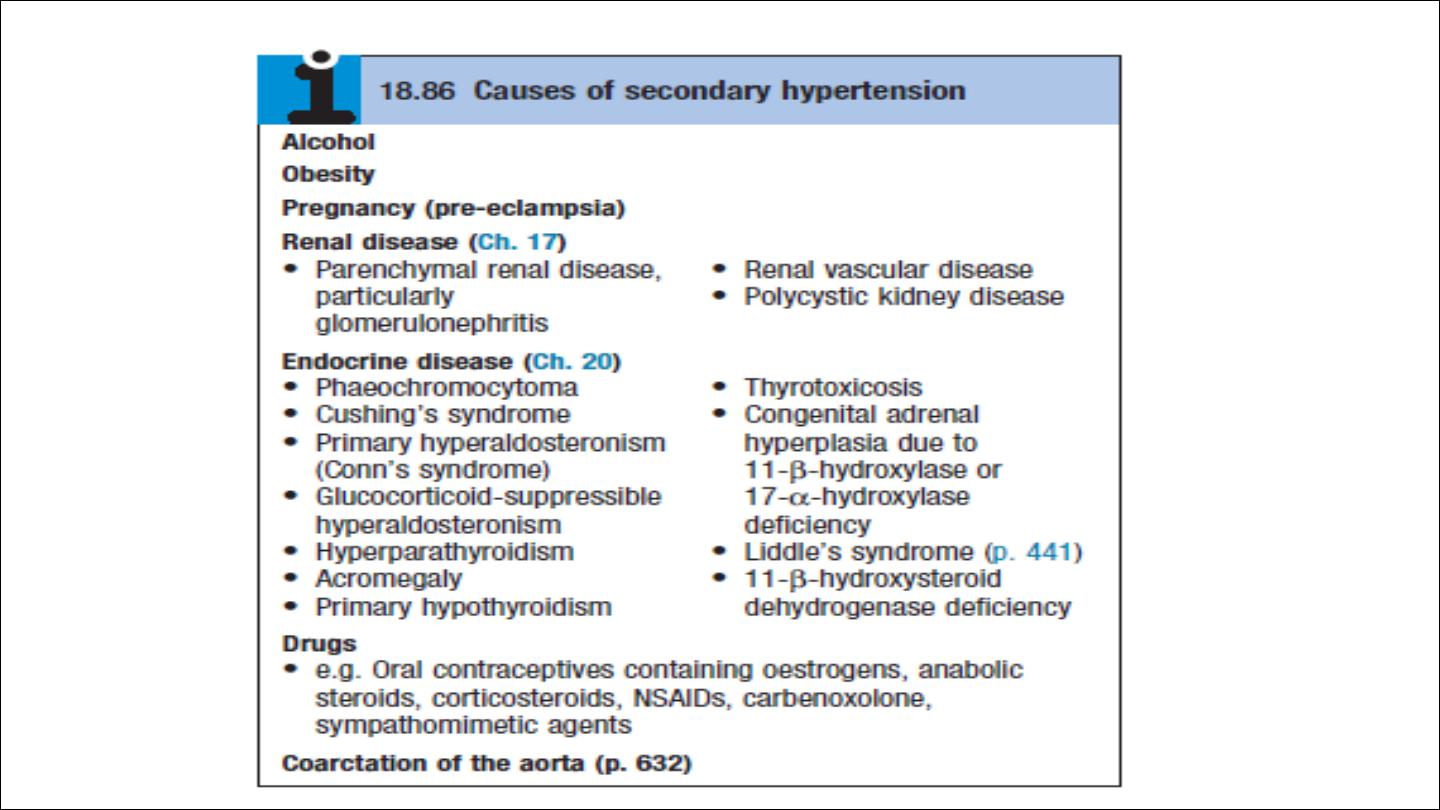
Etiology:
Primary , essential HPT account for 95%, no obvious cause can be
identified. The pathogenesis is not clearly understood. Many
factors may contribute to its development, including renal
dysfunction, peripheral resistance vessel tone, endothelial
dysfunction, autonomic tone, insulin resistance and neurohumoral
factors.
Hypertension is more common in some ethnic groups, particularly
African Americans and Japanese
, and approximately 40–60% is
explained by genetic factors. Age is a strong risk factor in all ethnic
groups.
Important environmental factors include a high salt intake, heavy
consumption of alcohol, obesity, lack of exercise and impaired
intrauterine growth. There is little evidence that ‘stress’ causes
hypertension.

Clinical features
Hypertension is usually asymptomatic until the diagnosis is made at a
routine physical examination or when a complication arises. Reflecting
this fact, a BP check is advisable every 5 years in adults over 40 years
of age to pick up occult hypertension.

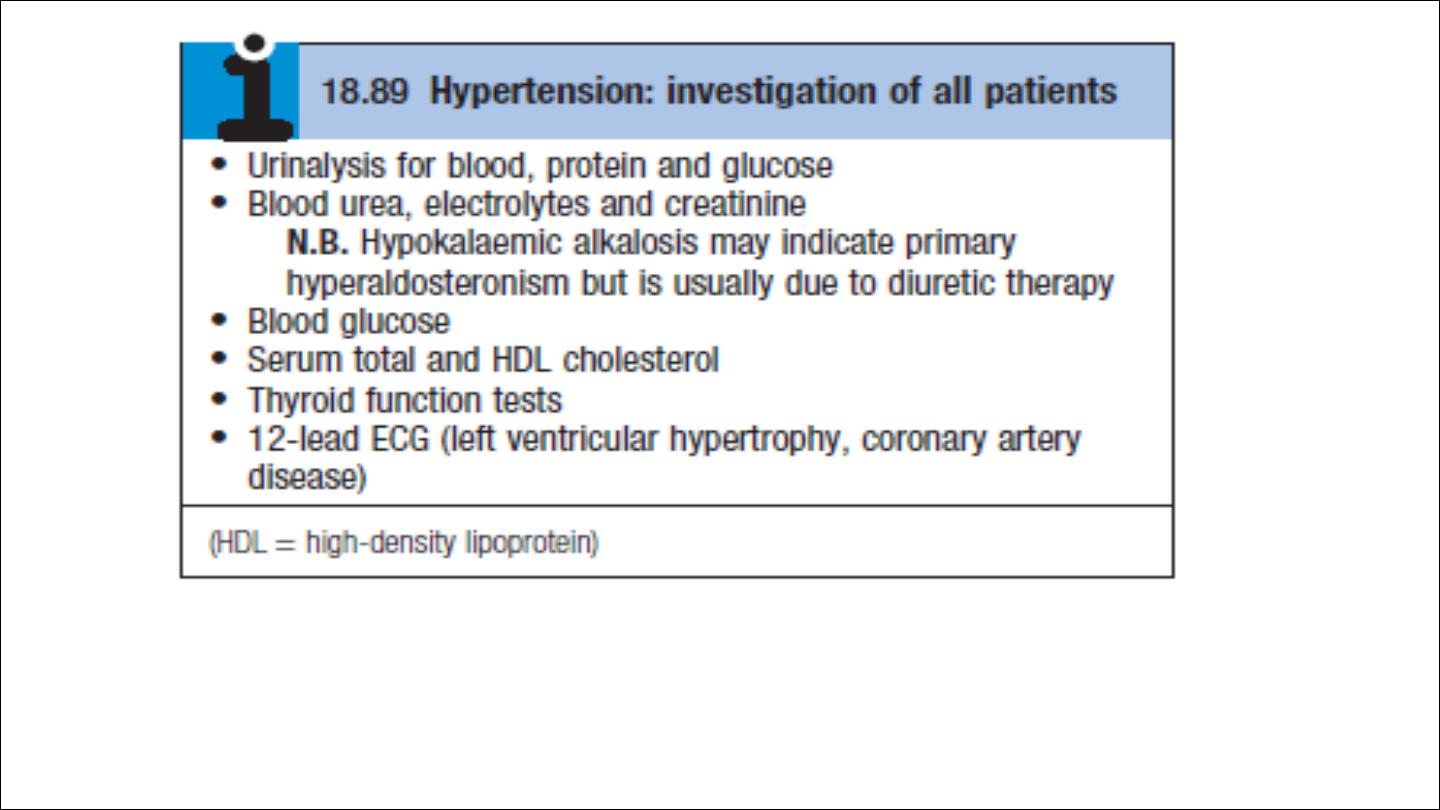
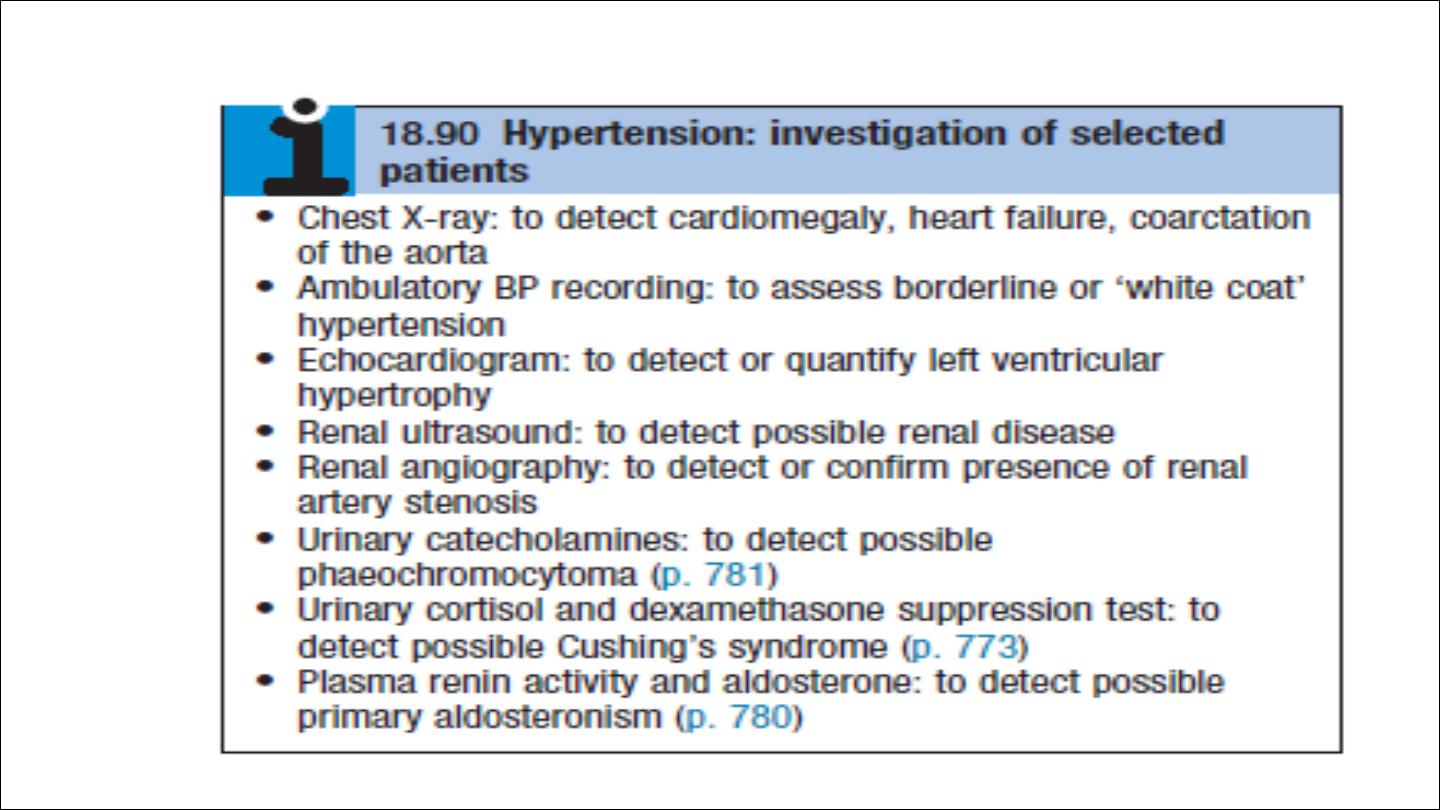
Investigations
A decision to embark on antihypertensive therapy effectively commits the
patient to life-long treatment, so readings must be as accurate as possible.
The objectives are to:
• confirm the diagnosis by obtaining accurate, representative BP
measurements
• identify contributory factors and any underlying causes
• assess other risk factors and quantify cardiovascular risk
• detect any complications that are already present
• identify comorbidity that may influence the choice of antihypertensive
therapy.
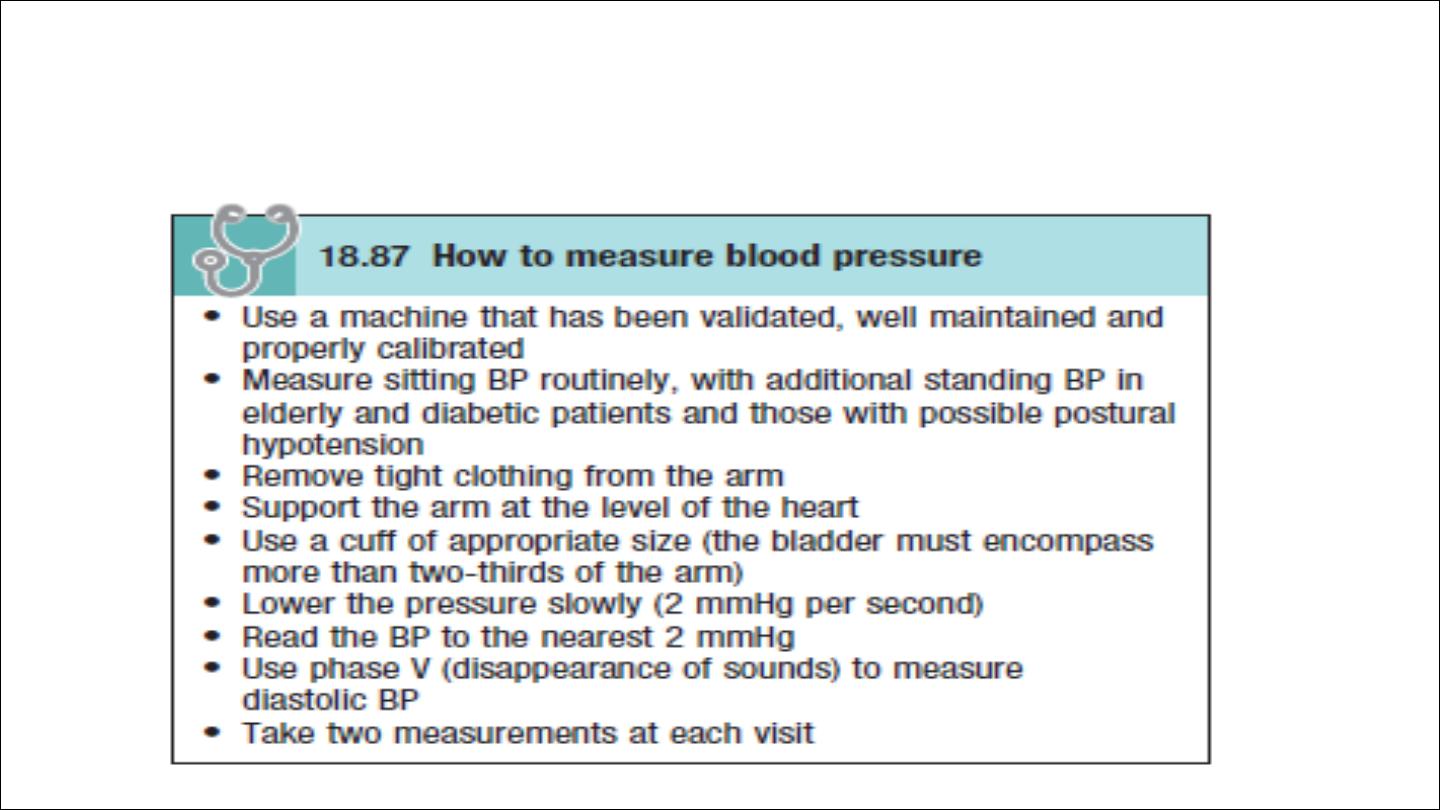
Measurement of blood pressure
Antihypertensive once started → life long treatment
Tight cuff → high pressure readings
Large cuff → low pressure readings
White coat hypertension:
Exercise, anxiety, discomfort and unfamiliar surroundings can all lead to
a transient rise in BP. as many as 20% of patients with apparent
hypertension in the clinic may have a normal BP when it is recorded by
automated devices used at home. The risk of cardiovascular disease in
these patients is less than that in patients with sustained hypertension
but greater than that in normotensive subjects.
ambulatory BP measurements obtained over 24 hours or longer
provides a better profile than a limited number of clinic readings and
correlates more closely with evidence of target organ damage than
casual BP measurements.
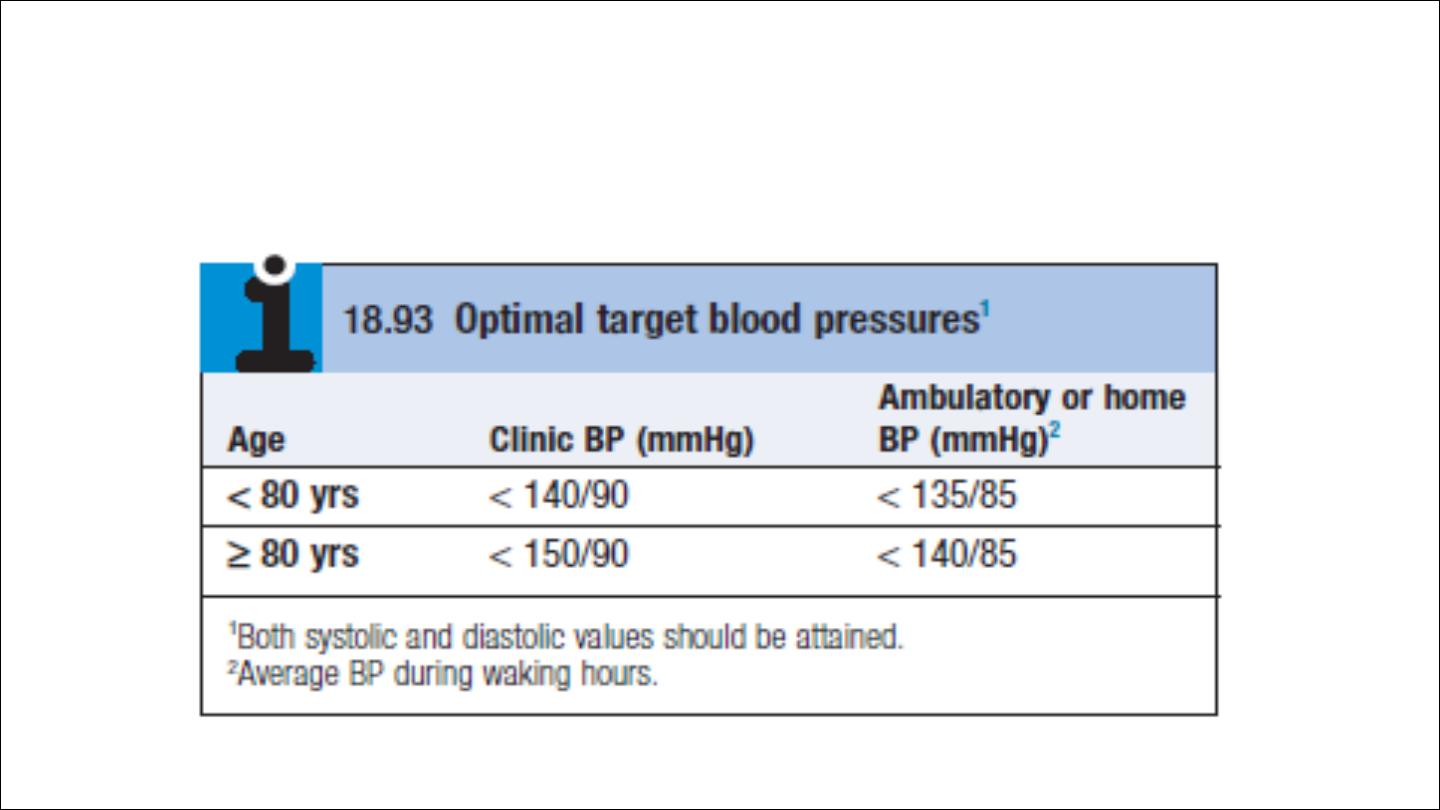
However, treatment thresholds and targets must be adjusted
downwards because ambulatory BP readings are systematically lower
(approximately 12/7mmHg) than clinic measurements.
The average ambulatory daytime (not 24-hour or night-time) BP should
be used to guide management decisions.

Home blood pressure measurements
Patients can measure their own BP at home using a range of
commercially available semi-automatic devices. The value of such
measurements is less well established and is dependent on the
environment and timing of the readings measured.
Home or ambulatory BP measurements are particularly helpful in
patients with unusually
labile BP
, those with
refractory hypertension
,
those who may have
symptomatic hypotension
, and those in whom
white
coat hypertension
is suspected.
History
Family history, lifestyle (exercise, salt intake, smoking habit) and other risk
factors should be recorded.
A careful history will identify those patients with drug- or alcohol-induced
hypertension and may elicit the symptoms of other causes of secondary
hypertension such as phaeochromocytoma (paroxysmal headache,
palpitation and sweating or complications such as coronary artery disease
(e.g. angina, breathlessness).

Examination may give clue to the underling cause of secondary HPT:
Radiofeomaral delay in coarctation
Renal bruit in RAS
Enlarged kidney in PCKD
Moon face in cushing syndrome
Examination may also reveal evidence of risk factors for hypertension, such
as central obesity and hyperlipidaemia.
Other signs may be observed that are due to the complications of
hypertension. These include signs of left ventricular hypertrophy,
accentuation of the aortic component of the second heart sound, and a
fourth heart sound. AF is common and may be due to diastolic dysfunction
caused by left ventricular hypertrophy or the effects of CAD.
Severe hypertension can cause left ventricular failure in the absence of CAD,
particularly when there is an impairment of renal function.

Target organ damage
1. Blood vessels
In larger arteries (> 1 mm in diameter), the internal elastic lamina is
thickened, smooth muscle is hypertrophied and fibrous tissue is deposited.
The vessels dilate and become tortuous, and their walls become less
compliant.
In smaller arteries (< 1 mm), hyaline arteriosclerosis occurs in the wall, the
lumen narrows and aneurysms may develop. These structural changes in the
vasculature often perpetuate and aggravate hypertension by increasing
peripheral vascular resistance and reducing renal blood flow, thereby
activating the renin–angiotensin–aldosterone axis.
Hypertension is a major risk factor in the pathogenesis of aortic aneurysm
and aortic dissection.
Wide spread atherosclerosis

2. CNS
Stroke:
Stroke is a common complication of hypertension and
may be due to cerebral haemorrhage or infarction. Carotid
atheroma and transient ischaemic attacks are more common
in hypertensive patients. Subarachnoid haemorrhage is also
associated with hypertension
Hypertensive encephalopathy
is a rare condition characterised by
high BP and neurological symptoms, including transient disturbances of
speech or vision, paraesthesiae, disorientation, fits and loss of
consciousness. Papilloedema is common. A CT scan of the brain often
shows haemorrhage in and around the basal ganglia; however, the
neurological deficit is usually reversible if the hypertension is properly
controlled.

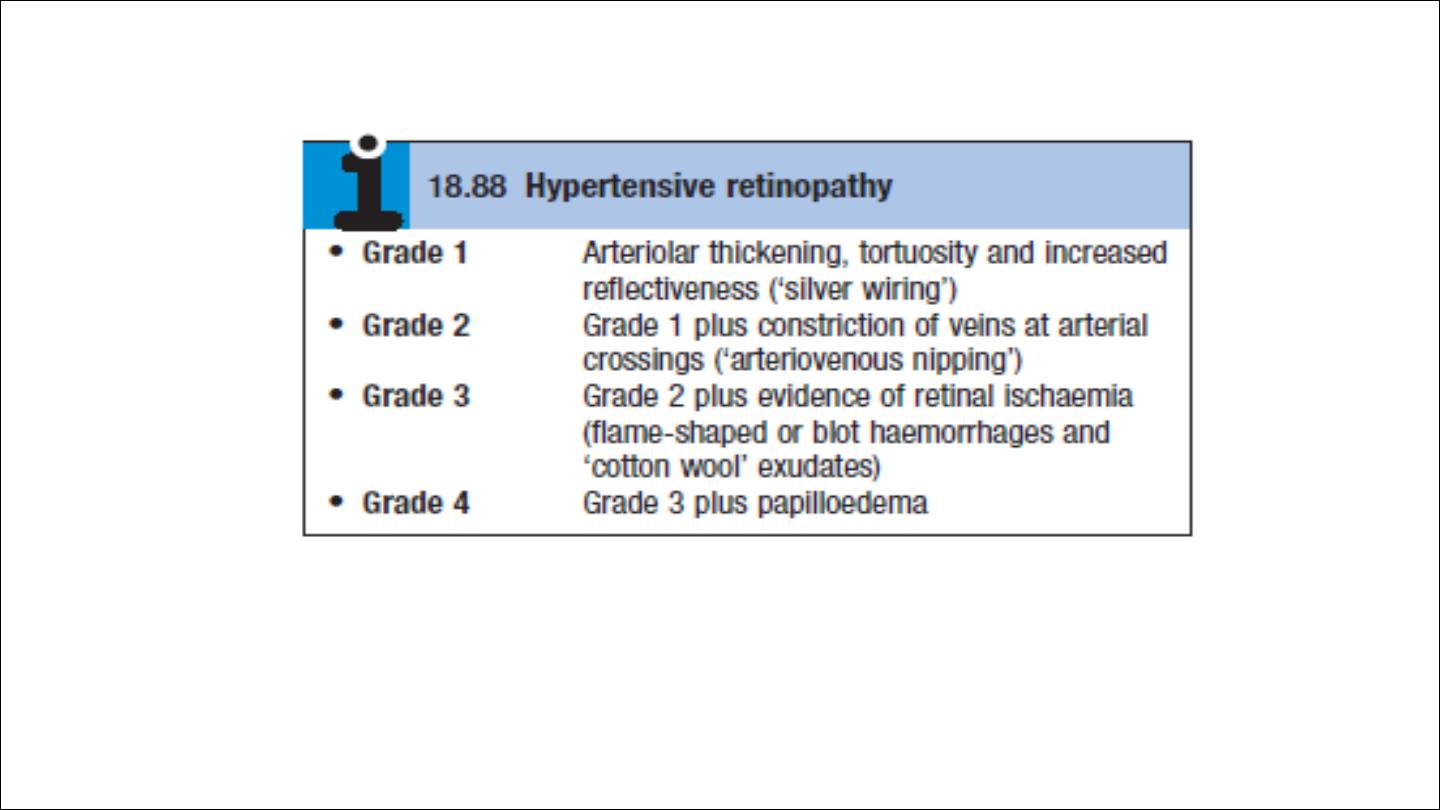
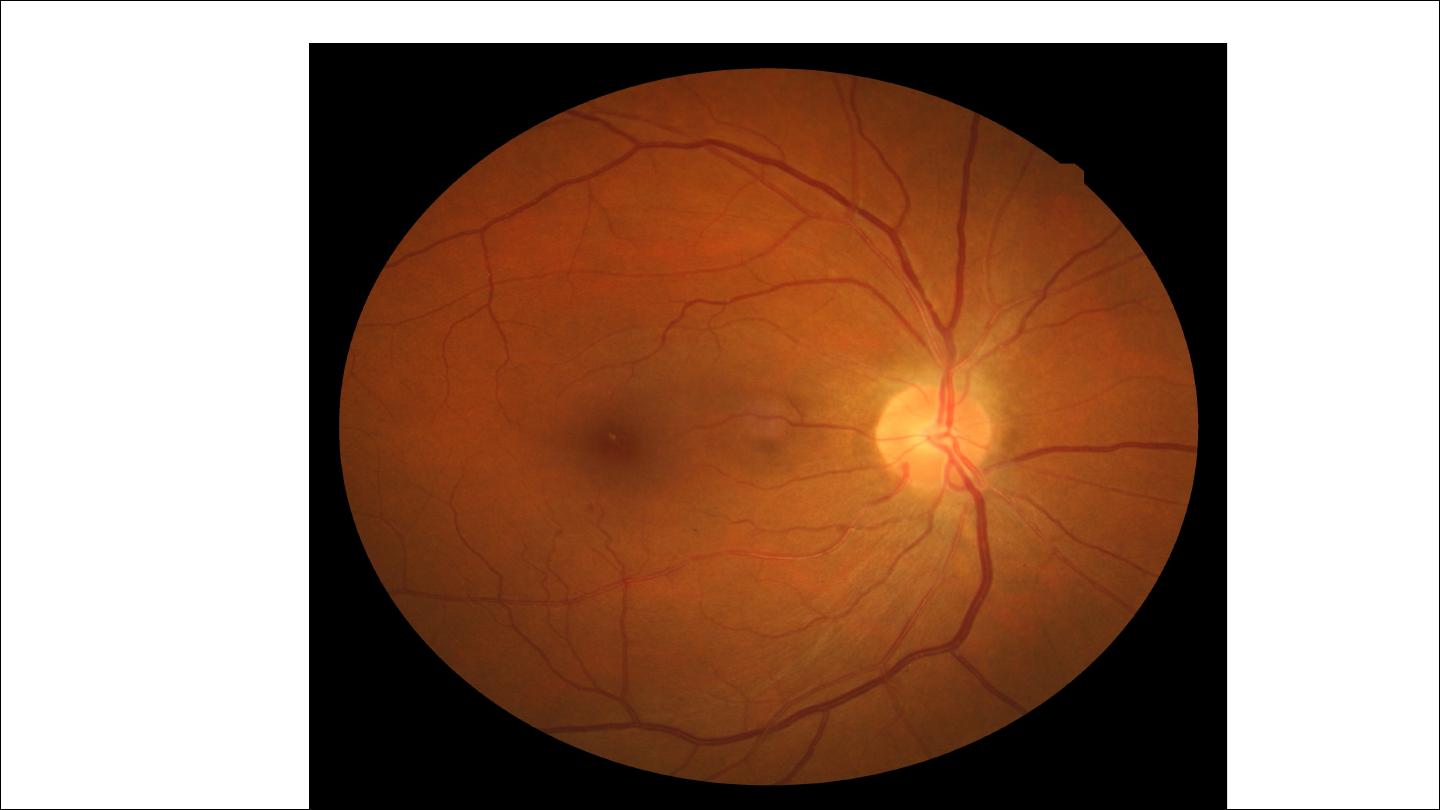
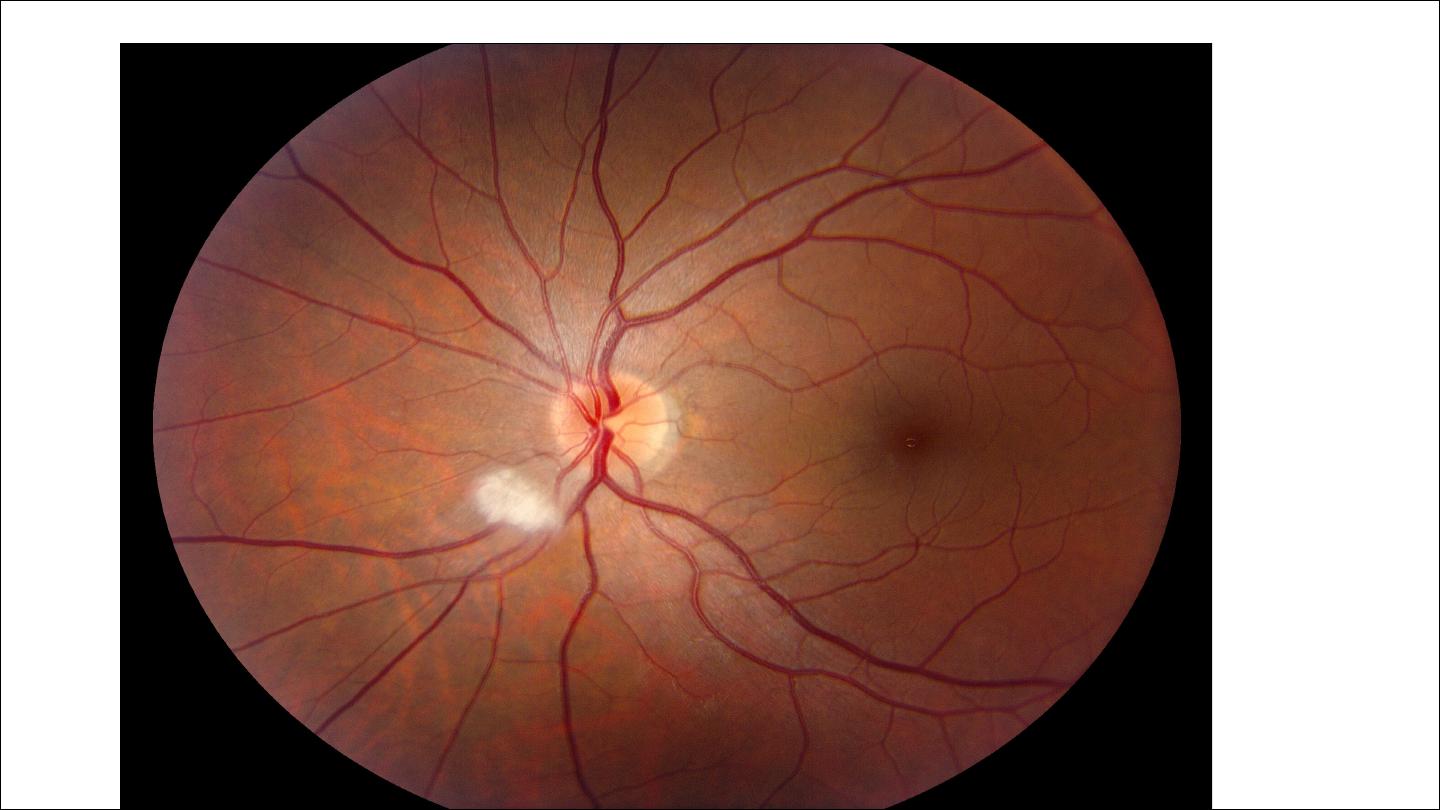
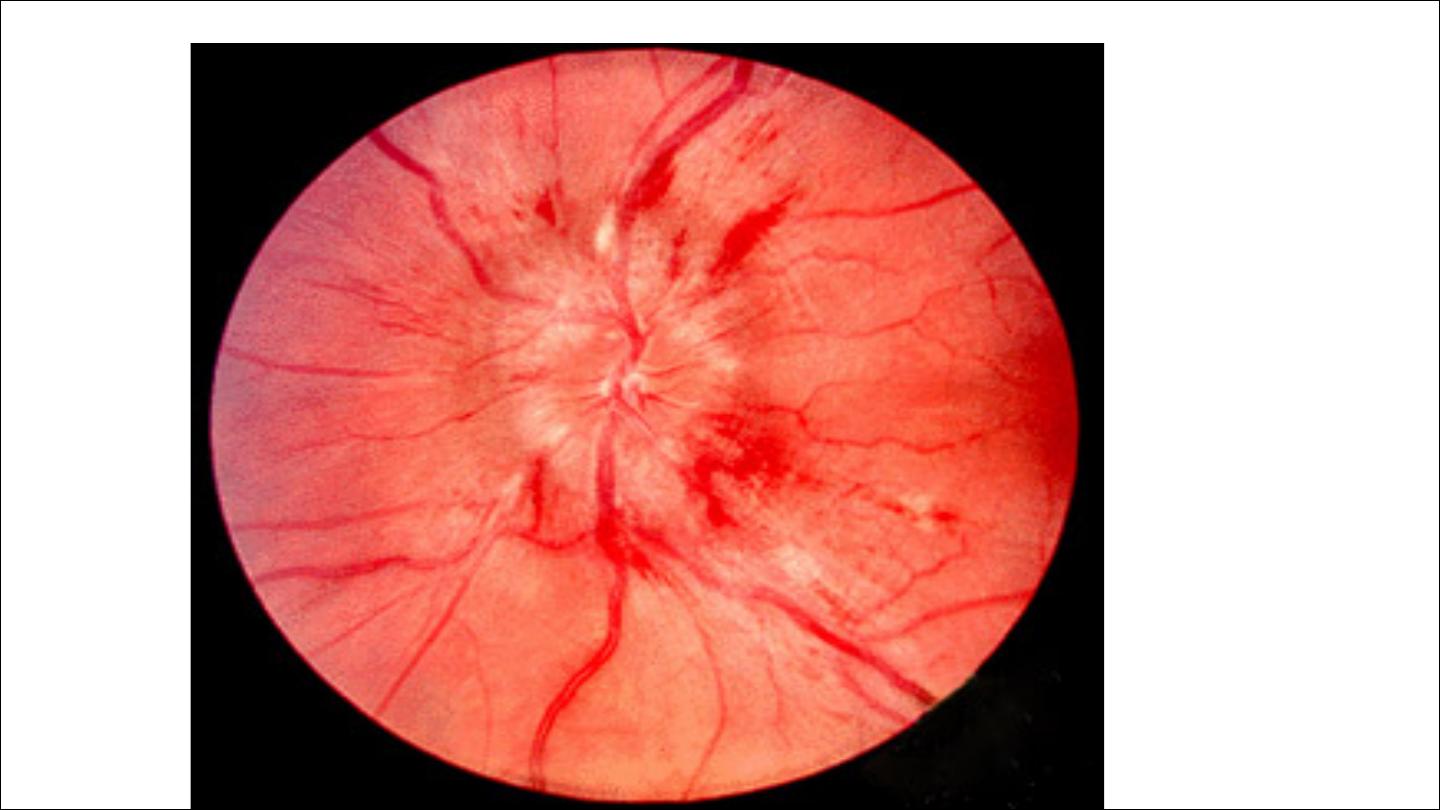
3. retina
Retina The optic fundi reveal a gradation of changes linked to the
severity of hypertension; fundoscopy can, therefore, provide an
indication of the arteriolar damage occurring elsewhere ‘Cotton wool’
exudates are associated with retinal ischaemia or infarction, and fade in
a few weeks . ‘Hard’ exudates (small, white, dense deposits of lipid)
and microaneurysms (‘dot’ haemorrhages) are more characteristic of
diabetic retinopathy . Hypertension is also associated with central
retinal vein thrombosis
4. Heart
The excess cardiac mortality and morbidity associated with hypertension are
largely due to a higher incidence of coronary artery disease. High BP places a
pressure load on the heart and may lead to left ventricular hypertrophy with
a forceful apex beat and fourth heart sound. ECG or echocardiographic
evidence of left ventricular hypertrophy is highly predictive of cardiovascular
complications and therefore particularly useful in risk assessment. Atrial
fibrillation is common and may be due to diastolic dysfunction caused by left
ventricular hypertrophy or the effects of coronary artery disease. Severe
hypertension can cause left ventricular failure in the absence of coronary
artery disease, particularly when renal function, and therefore sodium
excretion, is impaired.
5. Kidneys
Long-standing hypertension may cause proteinuria and progressive
renal failure by damaging the renal vasculature.
‘Malignant’ or ‘accelerated’ phase hypertension
characterised by accelerated microvascular damage with necrosis in the
walls of small arteries and arterioles (‘fibrinoid necrosis’) and by
intravascular thrombosis.
The diagnosis is based on evidence of high BP and rapidly progressive
end organ damage, such as retinopathy (grade 3 or 4), renal
dysfunction (especially proteinuria) and/or hypertensive
encephalopathy . Left ventricular failure may occur and, if this is
untreated, death occurs within months.

Threshold for intervention
Systolic BP and diastolic BP are both powerful predictors of
cardiovascular risk.

HPT IN ELDERLY
Prevalence: affects more than half of all people over the age of 60 yrs
(including isolated systolic hypertension).
Risks: hypertension is the most important risk factor for MI, heart failure
and stroke in older people.
Benefit of treatment: absolute benefit from therapy is greatest in older
people (at least up to age 80 yrs).
Target BP: similar to that for younger patients.
Tolerance of treatment: antihypertensives are tolerated as well as in
younger patients.
Drug of choice: low-dose thiazides but, in the presence of coexistent disease
(e.g. gout, diabetes), other agents may be more appropriate.
