
VALVULAR HEART DISEASE
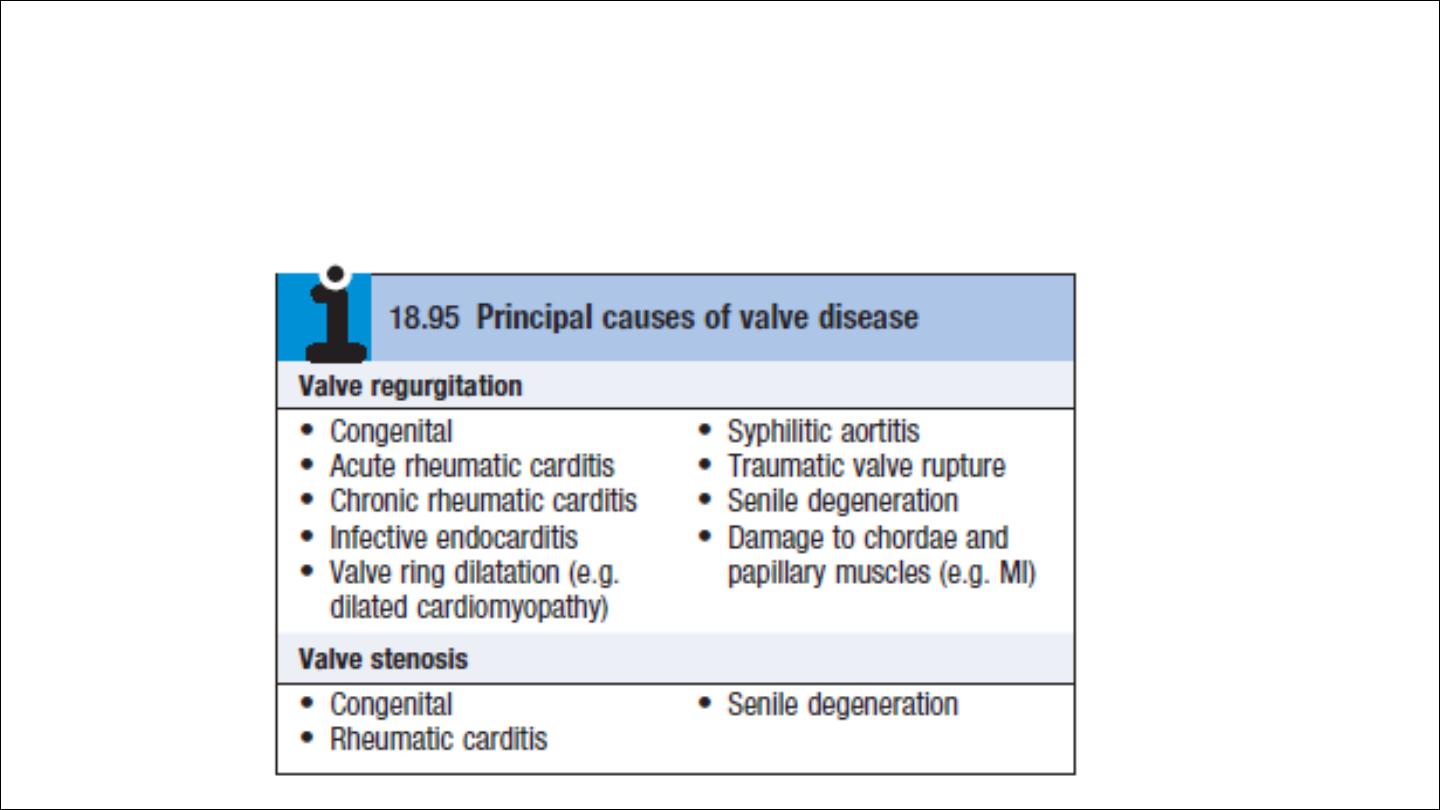
1. Stenosis : the valve orifice narrowed
2. Regurgitation or reflux: the valve fail to close adequately
3.Combination of stenosis and regurgitation
Mitral valve disease
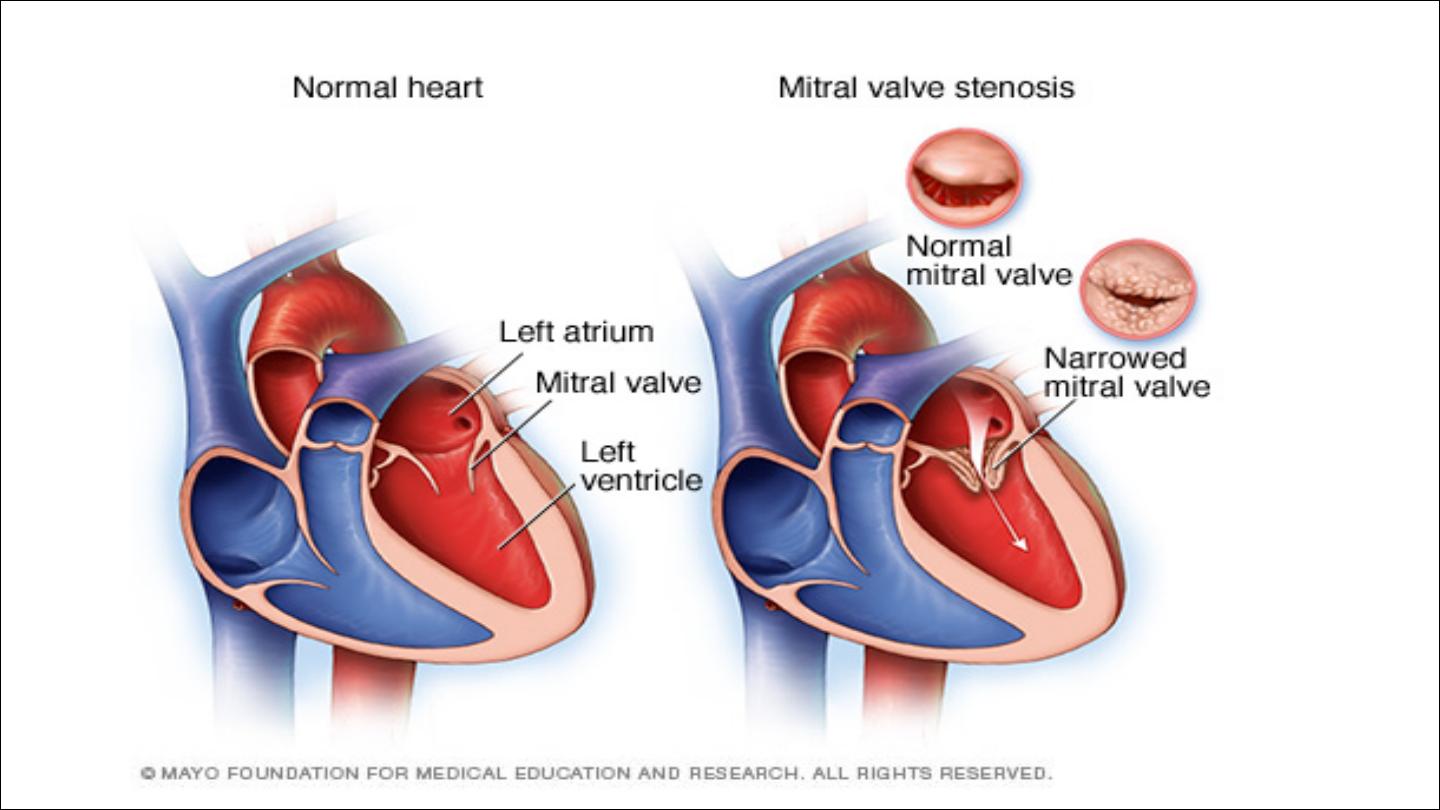
Mitral stenosis
Aetiology and pathophysiology:
•
Mitral stenosis is almost always
rheumatic
in origin
•
Senile
degenerative changes heavy calcification of the mitral valve
apparatus
•
Rarely
congenital
In rheumatic mitral stenosis, the mitral valve orifice is slowly diminished
by progressive fibrosis, thickening, calcification of the valve leaflets, and
fusion of the cusps and subvalvular apparatus.
LA → LV flow reduced, so LA pressure increase leading to pulmonary
venous congestion and breathlessness
q
Any increase in heart rate shortens diastole when the mitral valve is
open and produces a further rise in left atrial pressure. Situations that
demand an increase in cardiac output also increase left atrial
pressure, so exercise and pregnancy are poorly tolerated.
q
Normal MV orifice 5 cm 2, Symptom occur when the orifice less than
2 cm 2, Severe MS less than 1 cm 2
q
Dyspnea due to reduced lung compliance due to chronic pulmonary
venous congestion. Fatigue due to reduced CO

q
AF is common. Fewer than 20% of patients remain in sinus rhythm; many
of these have a small fibrotic LA and severe pulmonary hypertension.
Sudden rise in LA pressure → pulmonary odema.
In contrast, a more gradual rise in left atrial pressure tends to cause an
increase in pulmonary vascular resistance, which leads to pulmonary
hypertension that may protect the patient from pulmonary oedema.
Pulmonary hypertension leads to right ventricular hypertrophy and
dilatation, tricuspid regurgitation and right heart failure.
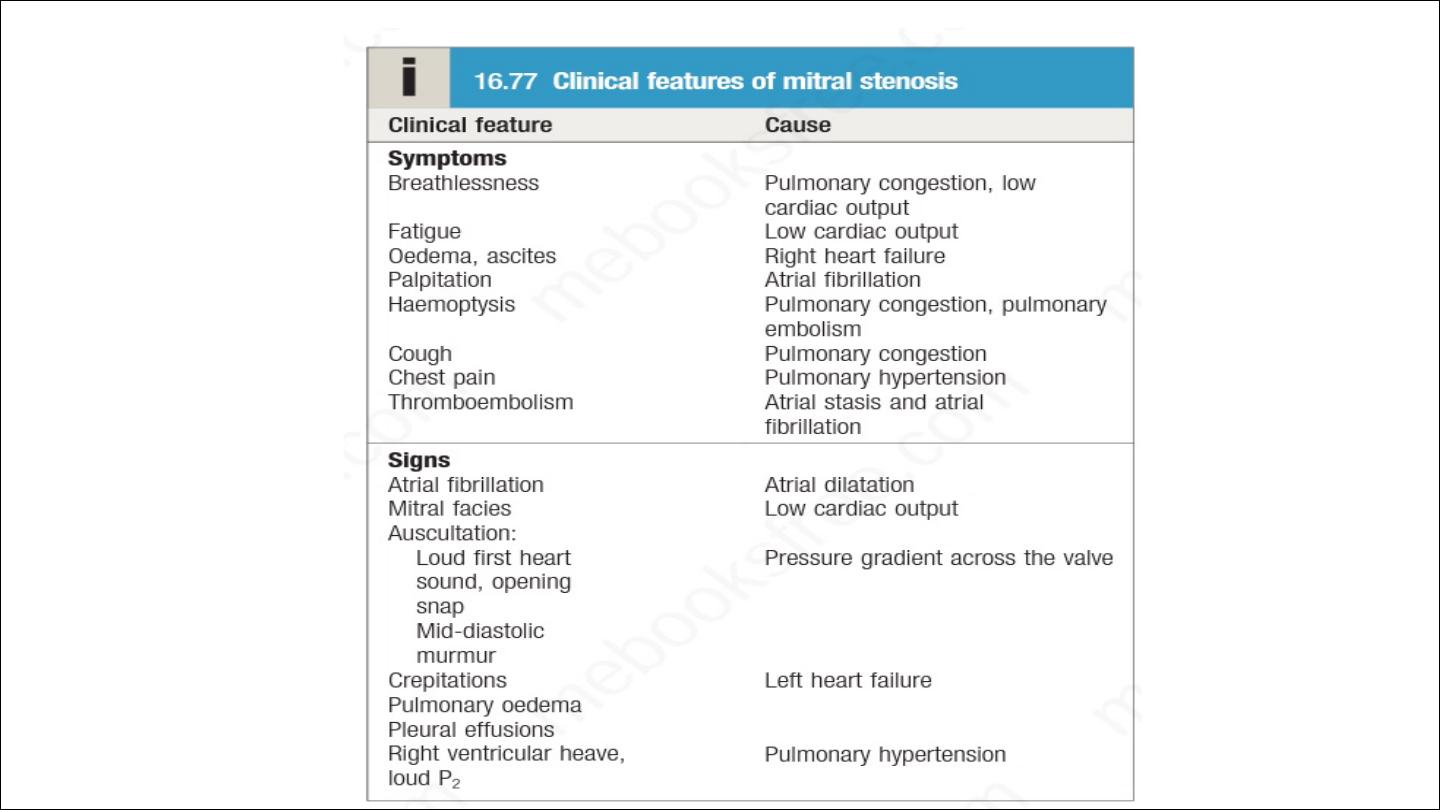
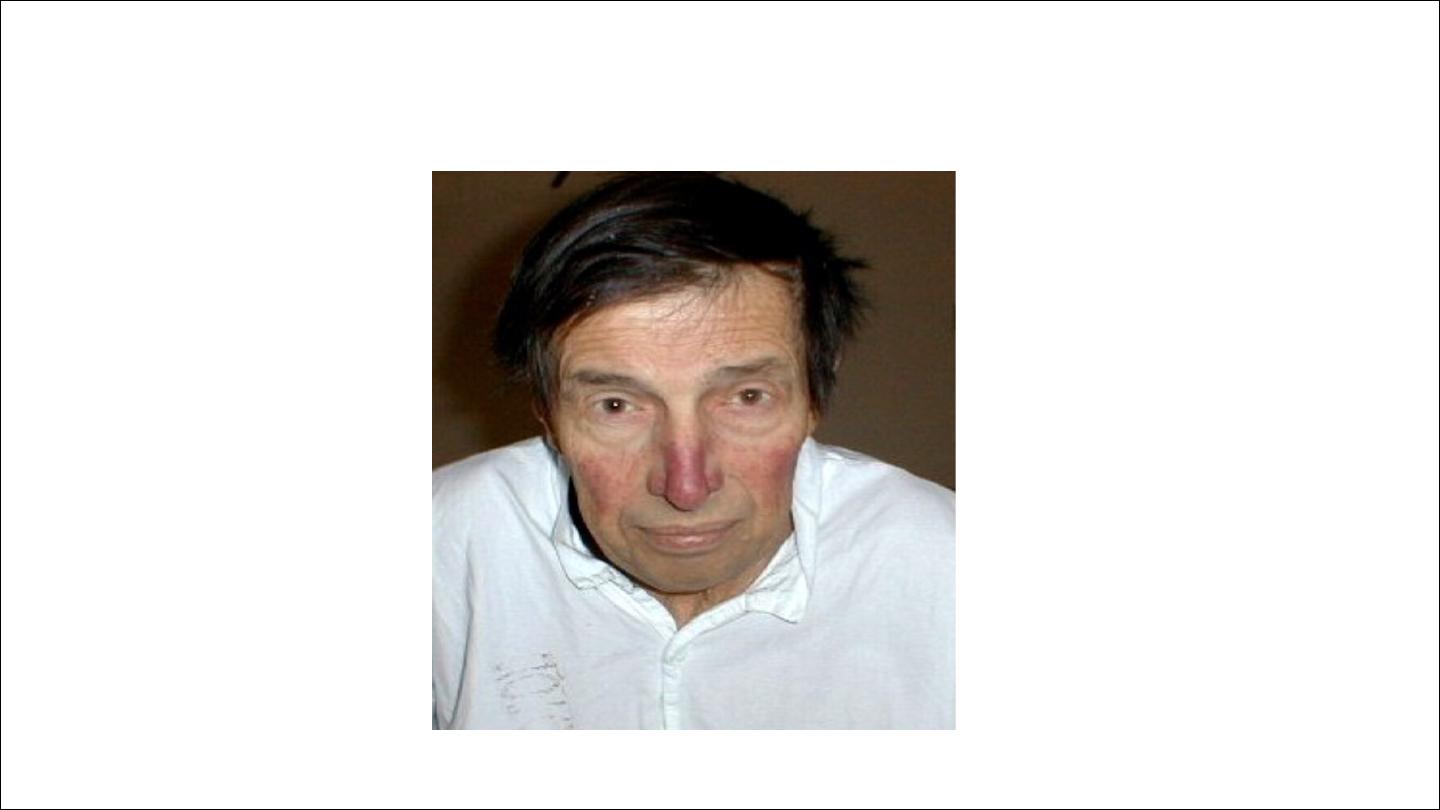
Mitral facies

Effort-related dyspnea is usually the dominant symptom . Exercise
tolerance typically diminishes very slowly over many years and patients
often do not appreciate the extent of their disability. Eventually,
symptoms occur at rest.
All patients with mitral stenosis, and particularly those with atrial
fibrillation, are at risk from left atrial thrombosis and systemic
thromboembolism.
Auscultatory finding in mitral stenosis
S 1 may be soft in heavily calcified valve
Opening snap indicate pliable leaflet, become closer to S1 as the
severity of the valve increase, absent in heavily calcified valve.
The duration of murmur increase with the severity of mitral stenosi

Clinical signs of sever MS
1. LONG RUMBLING DIASTOLIC MURMUR
2. OPENING SNAP CLOSE TO S2 OR ABSCENT
3. SIGN OF PHT, LOUD P2, RV HEAVE
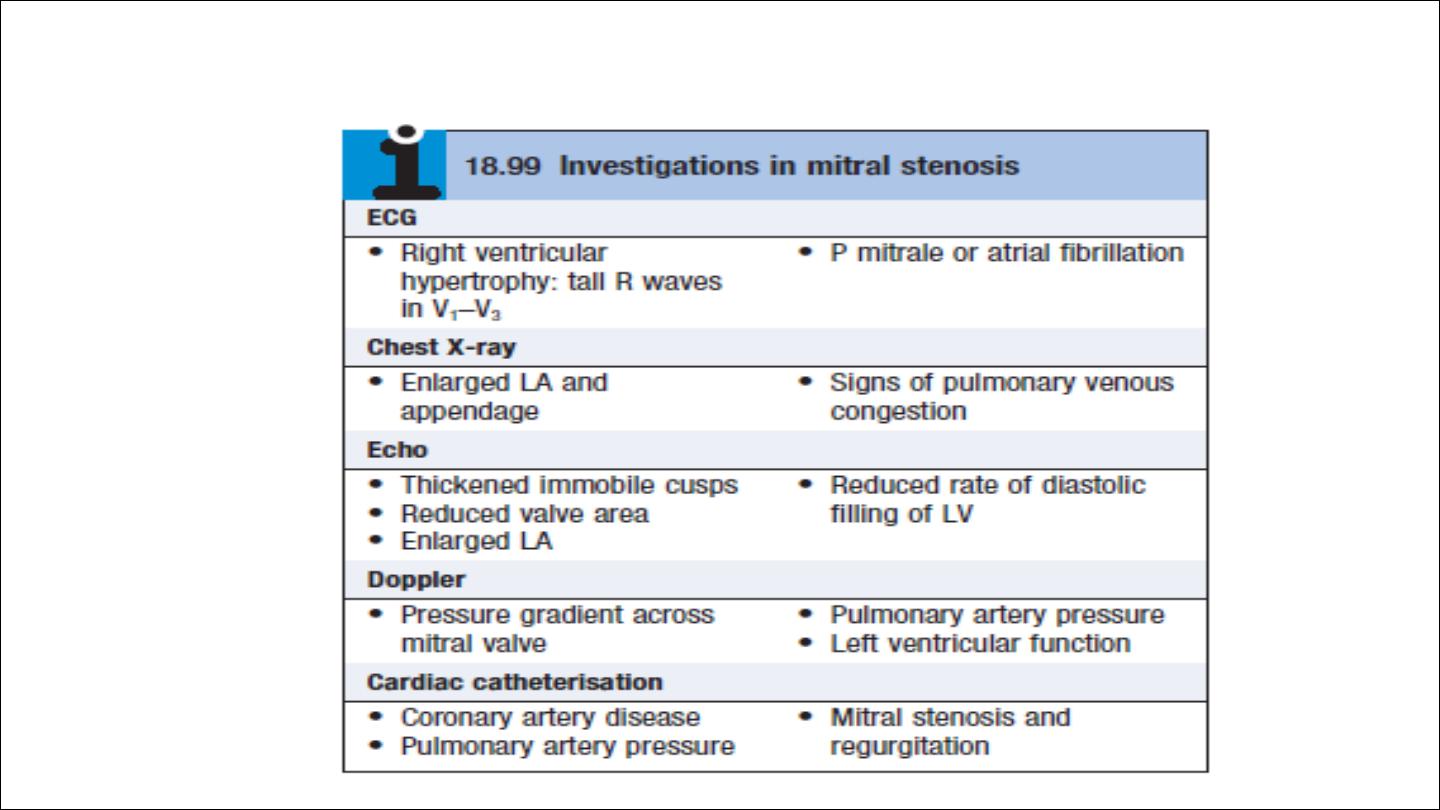
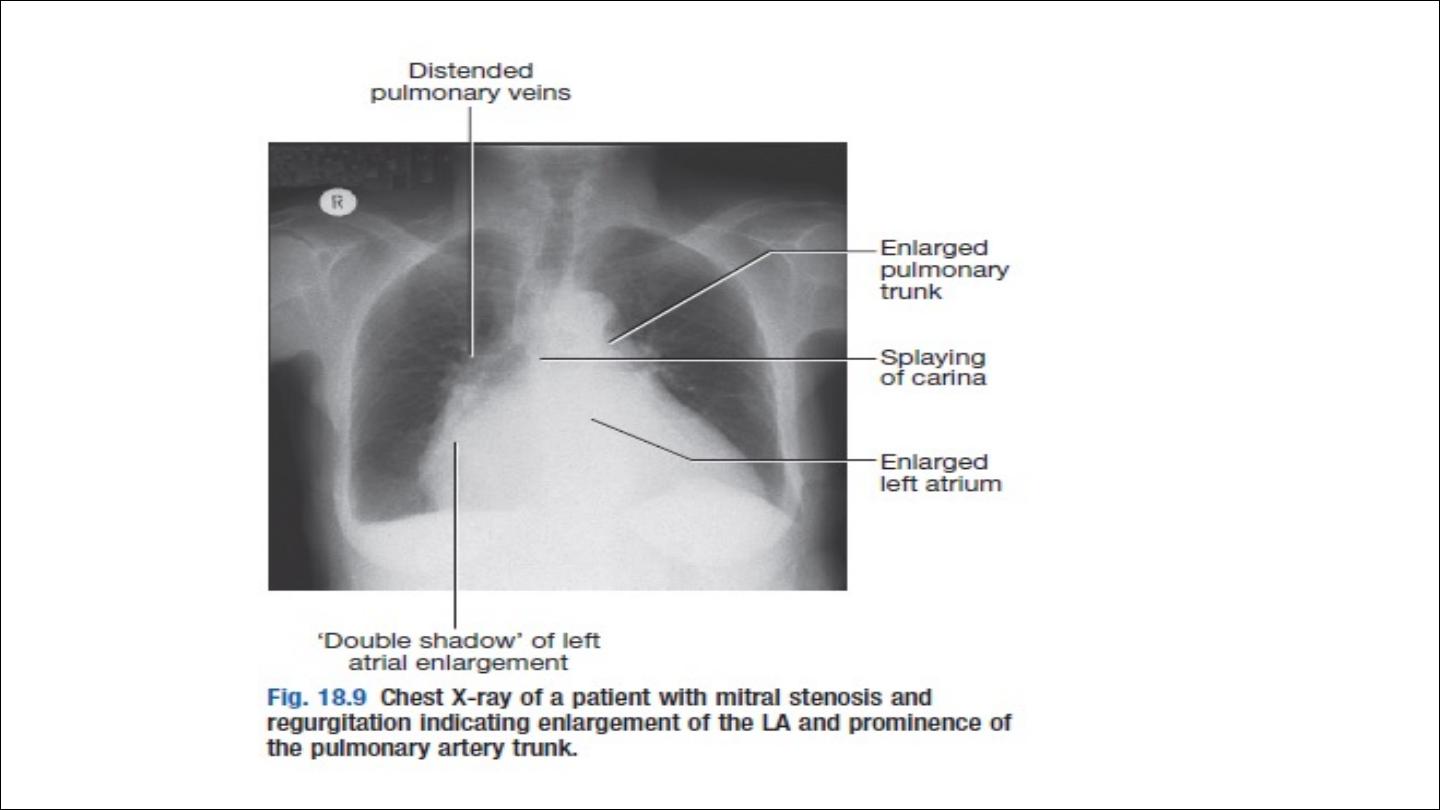
Investigation
Management
Medical treatment
1. Rate control for AF and rapid ventricular rate
2. anticoagulation; AF, thromboembolism, spontaneous echo contrast
3. Diuretics to relieve pulmonary congestion
4. Antibiotic prophylaxis against infective endocarditis is no longer
routinely recommended

•
If patients remain symptomatic despite medical treatment, intervention
include balloon valvuloplasty, mitral valvotomy or mitral valve replacement
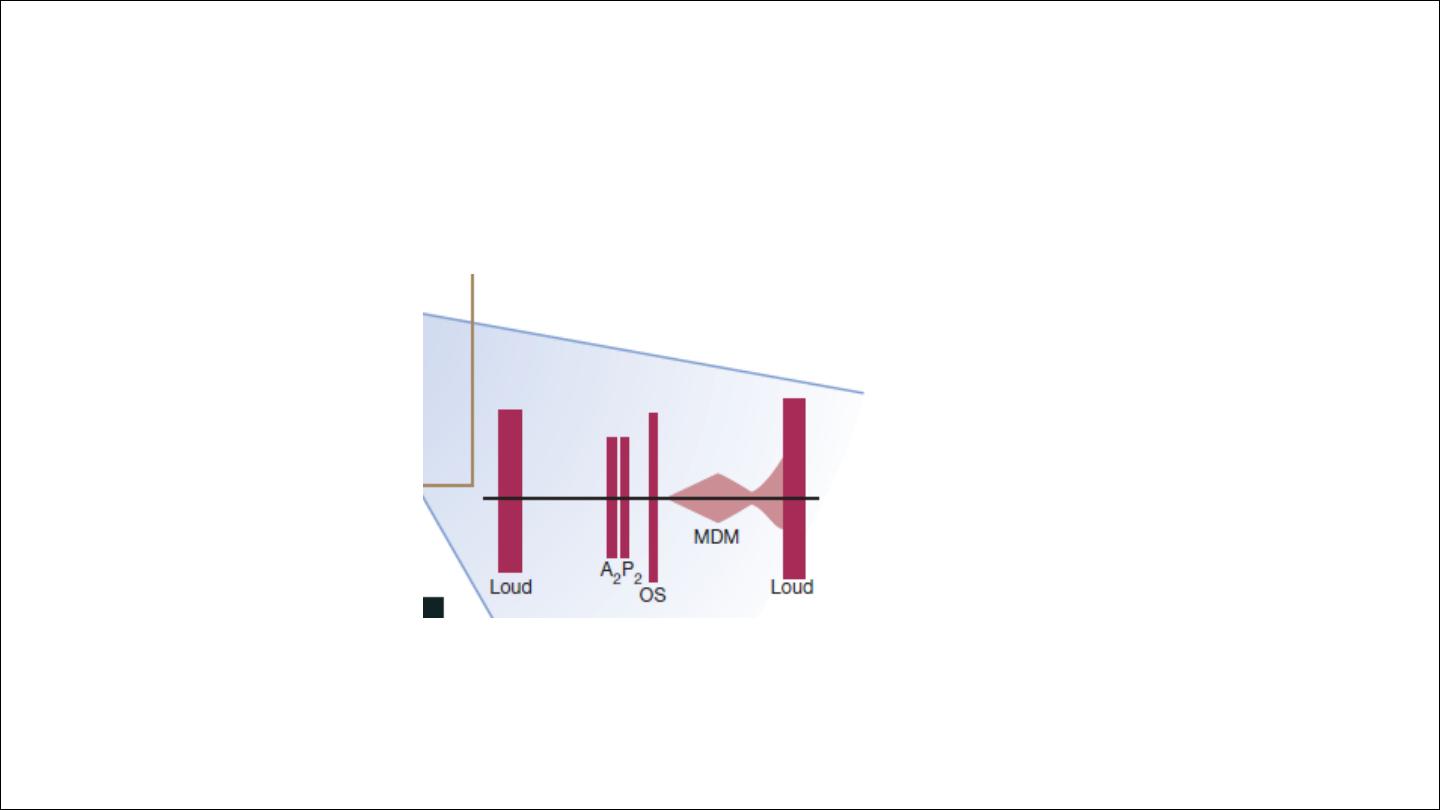
Criteria for mitral valvuloplasty
•
Significant symptoms
•
Isolated mitral stenosis
•
No (or trivial) mitral regurgitation
•
Mobile, non-calcified valve/subvalve apparatus on echo
•
LA free of thrombus
•
Follow up after balloon valvoplasty at 1 to 2 years interval as restenosis can
occur
Surgival Open or closed mitral valvotomy is acceptable alternative
Valve replacement is indicated if there is substantial mitral reflux or if the
valve is rigid and calcified
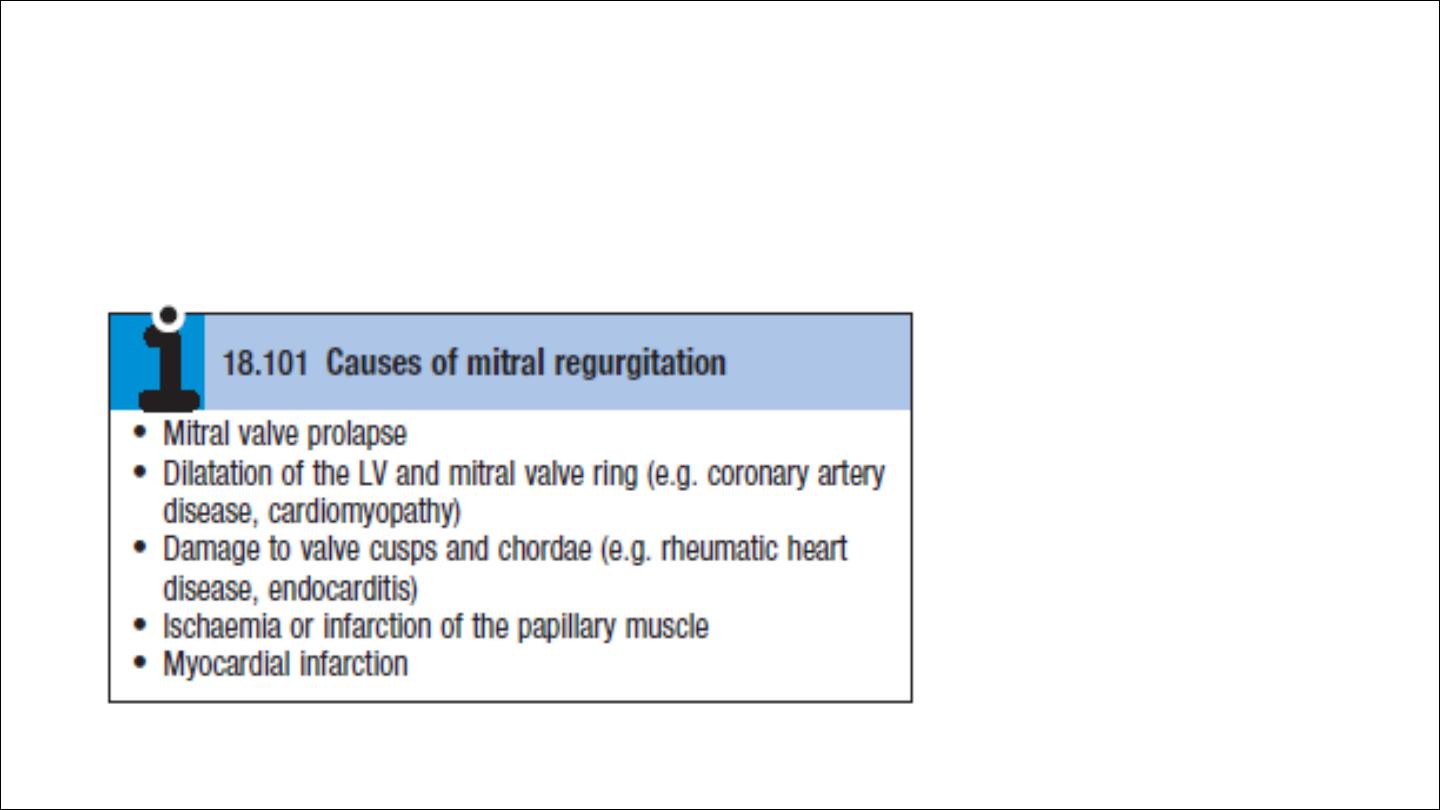
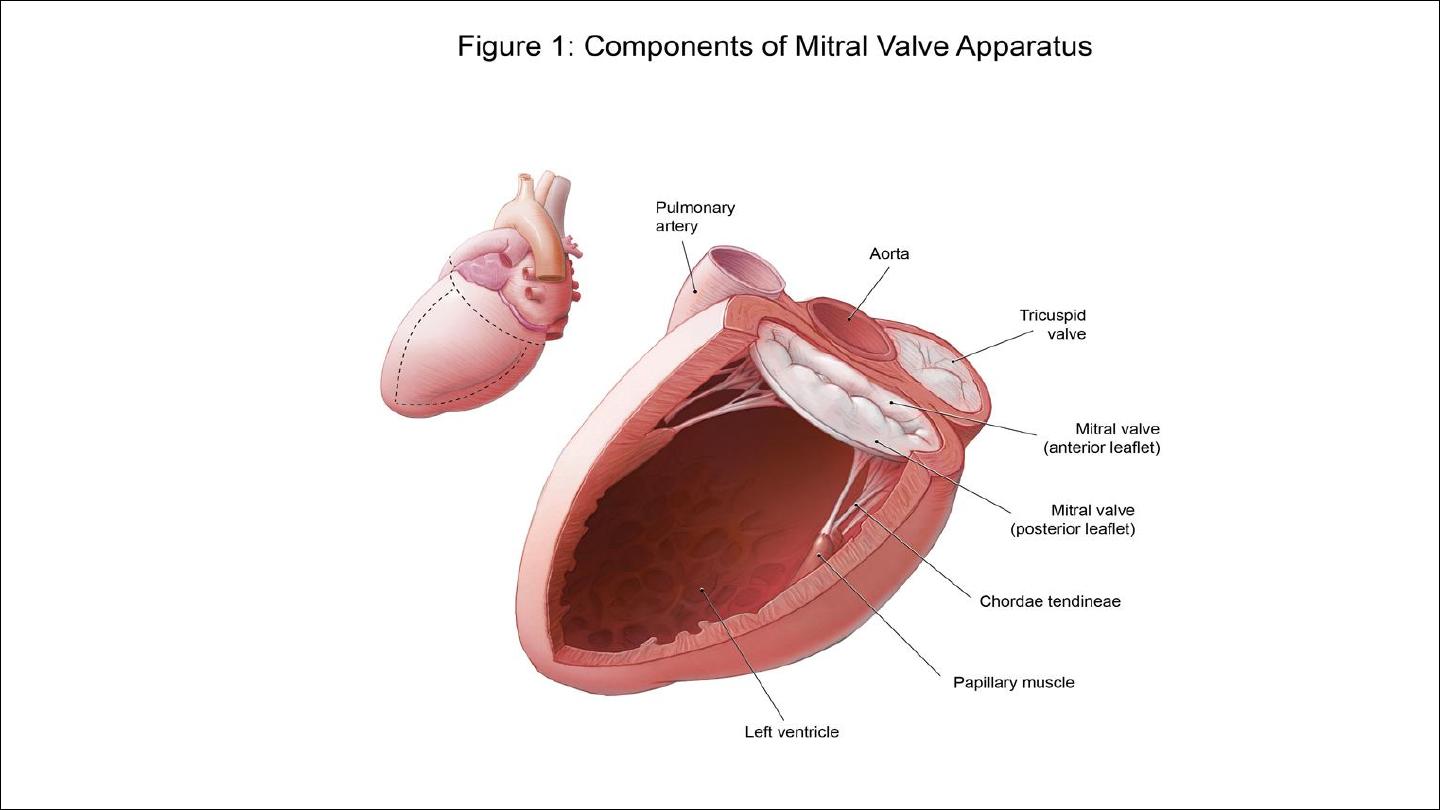
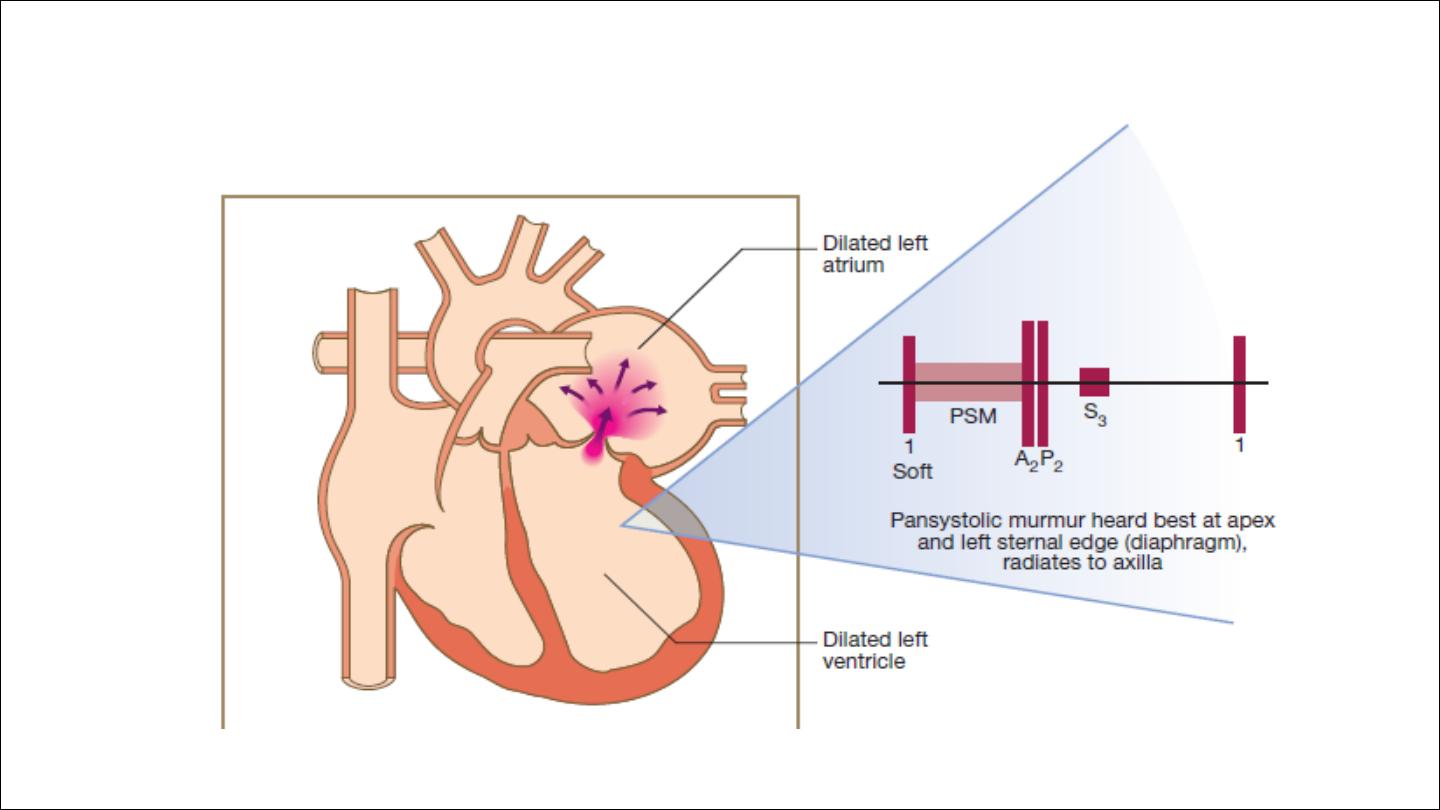
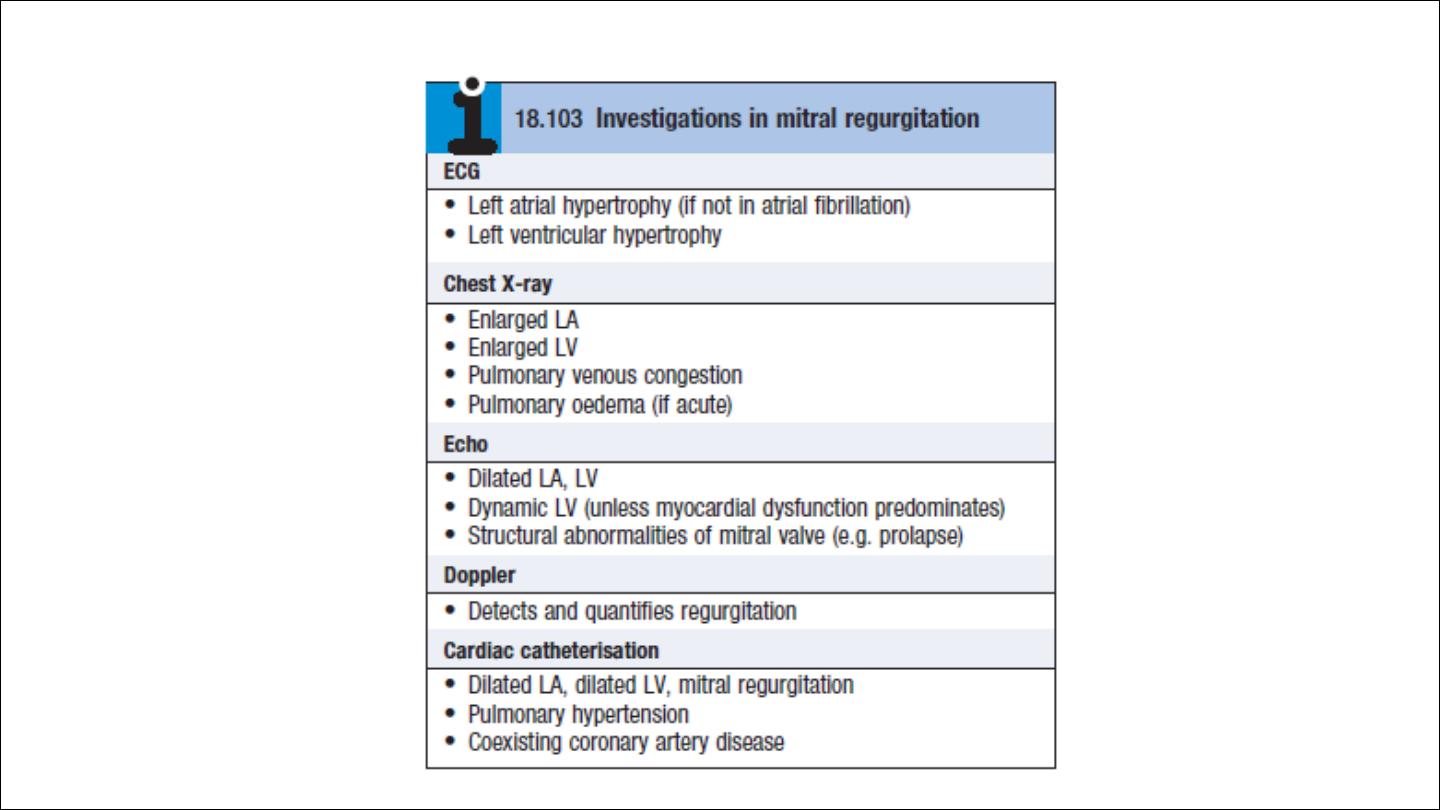
Mitral regurgitation
Aetiology and pathophysiology:
Rheumatic disease is the principal cause in countries where rheumatic
fever is common
Mitral regurgitation may also follow mitral valvotomy or valvuloplasty
.
ACUTE MR
1. RUPTURE PAPILLARY MUSCLE COMPLICATING ACUTE MI
2. RUPTURE CHORDAE TENDONAE DUE TO IE OR MVP
3. IE CAUSING VALVE PERFORATION

Chronic mitral regurgitation causes gradual dilatation of the LA with
little increase in pressure and therefore relatively few symptoms.
Nevertheless, the LV dilates slowly and the left ventricular diastolic and
left atrial pressures gradually increase as a result of chronic volume
overload of the LV
In acute mitral regurgitation causes a rapid rise in left atrial pressure
(because left atrial compliance is normal) and marked symptomatic
deterioration.

•
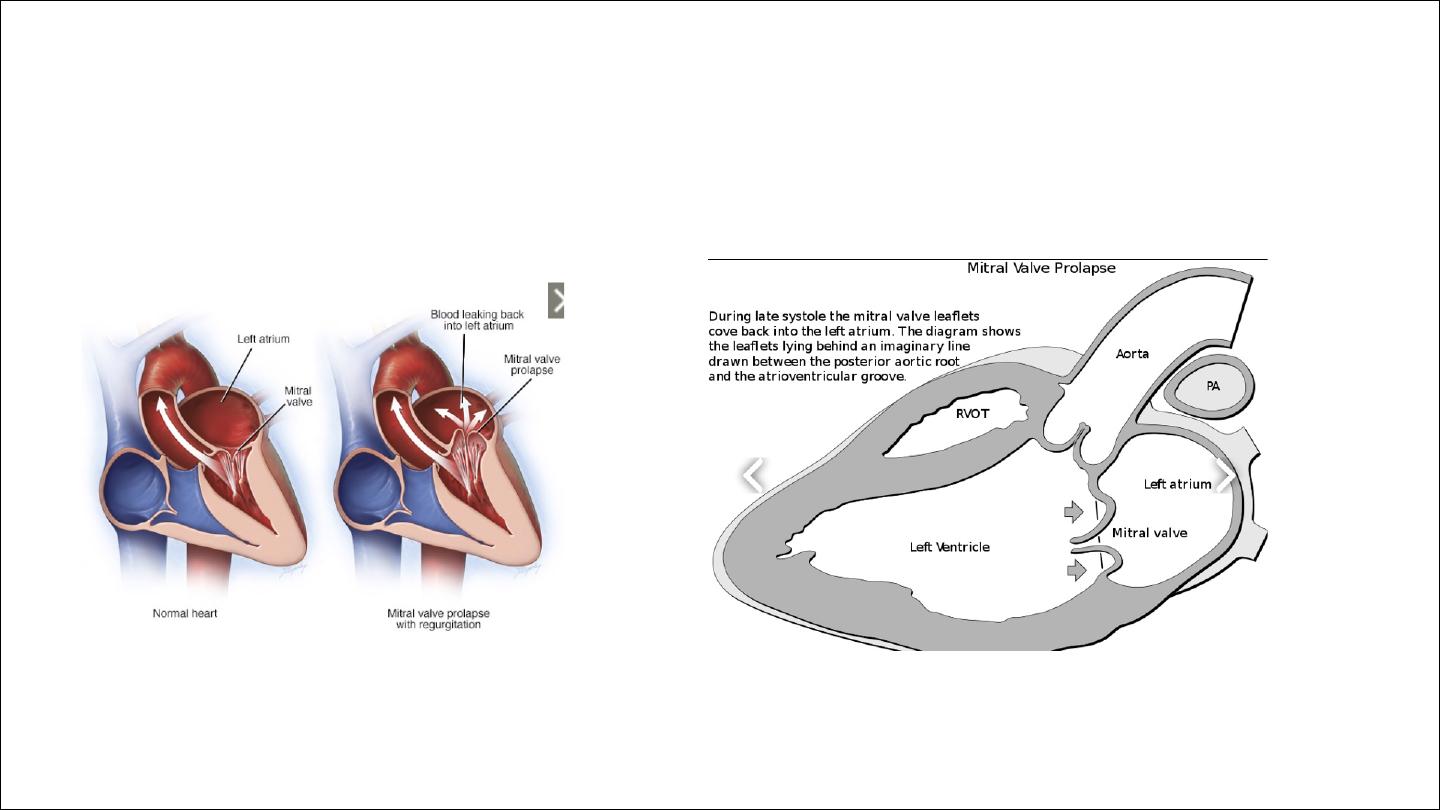
Mitral valve prolapse
This is also known as ‘floppy’ mitral valve and is one of the more
common causes of mild mitral regurgitation. It is caused by congenital
anomalies or degenerative myxomatous changes, and is sometimes a
feature of connective tissue disorders such as Marfan’s syndrome.
In its mildest forms, the valve remains competent but bulges back into
the atrium during systole, causing a mid-systolic click but no murmur.
If regurgitation occur, click followed by murmur

A click is not always audible and the physical signs may vary with both
posture and respiration. Progressive elongation of the chordae
tendineae leads to increasing mitral regurgitation, and if chordal
rupture occurs, regurgitation suddenly becomes severe. This is rare
before the fifth or sixth decade of life.
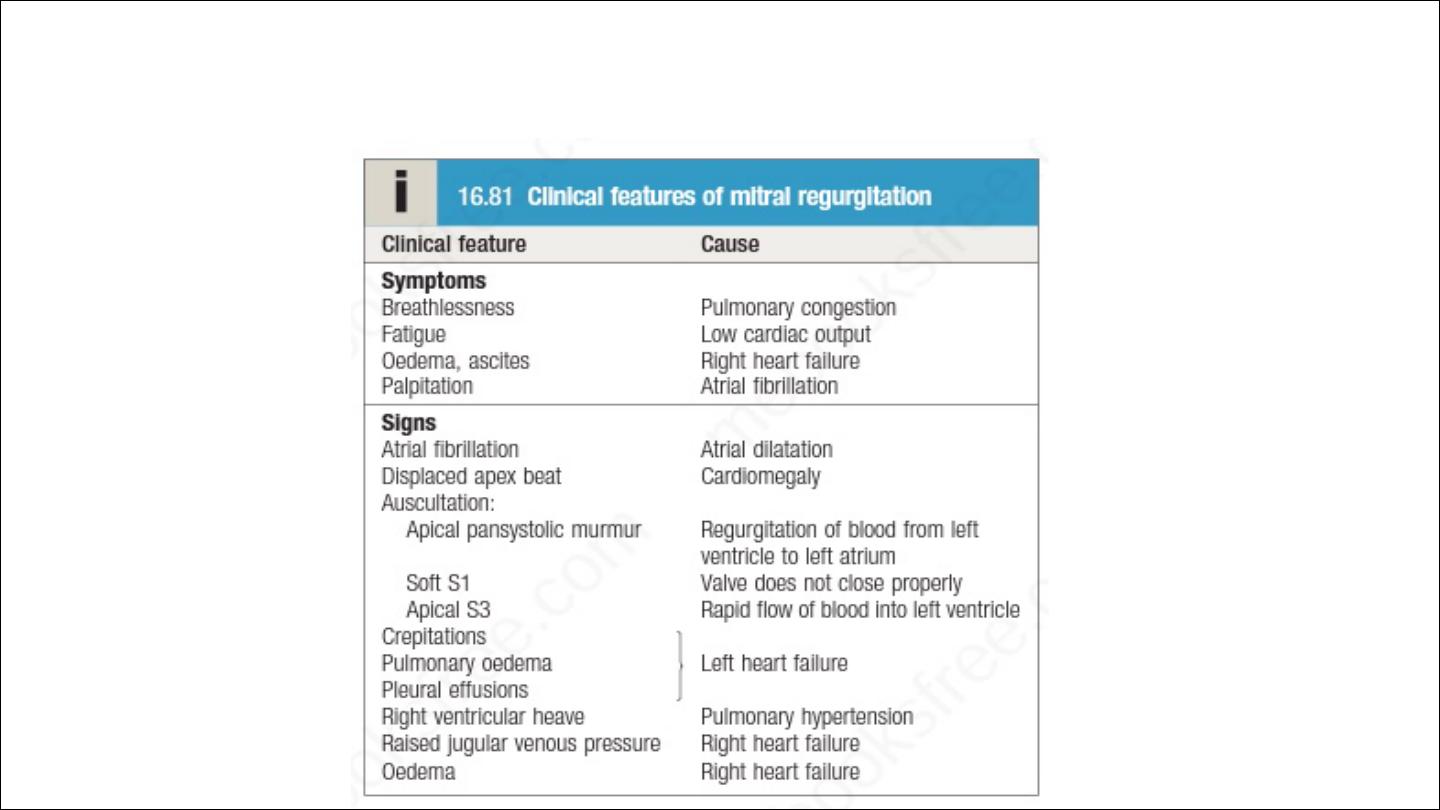
Clinical features
Symptoms depend on how suddenly the regurgitation develops
management
•
Diuretics
•
Vasodilators, e.g. ACE inhibitors
•
Digoxin if atrial fibrillation is present
•
Anticoagulants if atrial fibrillation is present
•
Surgery : repair or replacement

valve repair is used to treat mitral valve prolapse and offers many advantages
when compared to mitral valve replacement, such that it is now advocated
for severe regurgitation, even in asymptomatic patients, because results are
excellent and early repair prevents irreversible left ventricular damage
Mitral regurgitation often accompanies the ventricular dilatation and
dysfunction that are concomitants of coronary artery disease. If such
patients are to undergo coronary bypass graft surgery, it is common practice
to repair the valve and restore mitral valve function by inserting an
annuloplasty ring to overcome annular dilatation and to bring the valve
leaflets closer together.
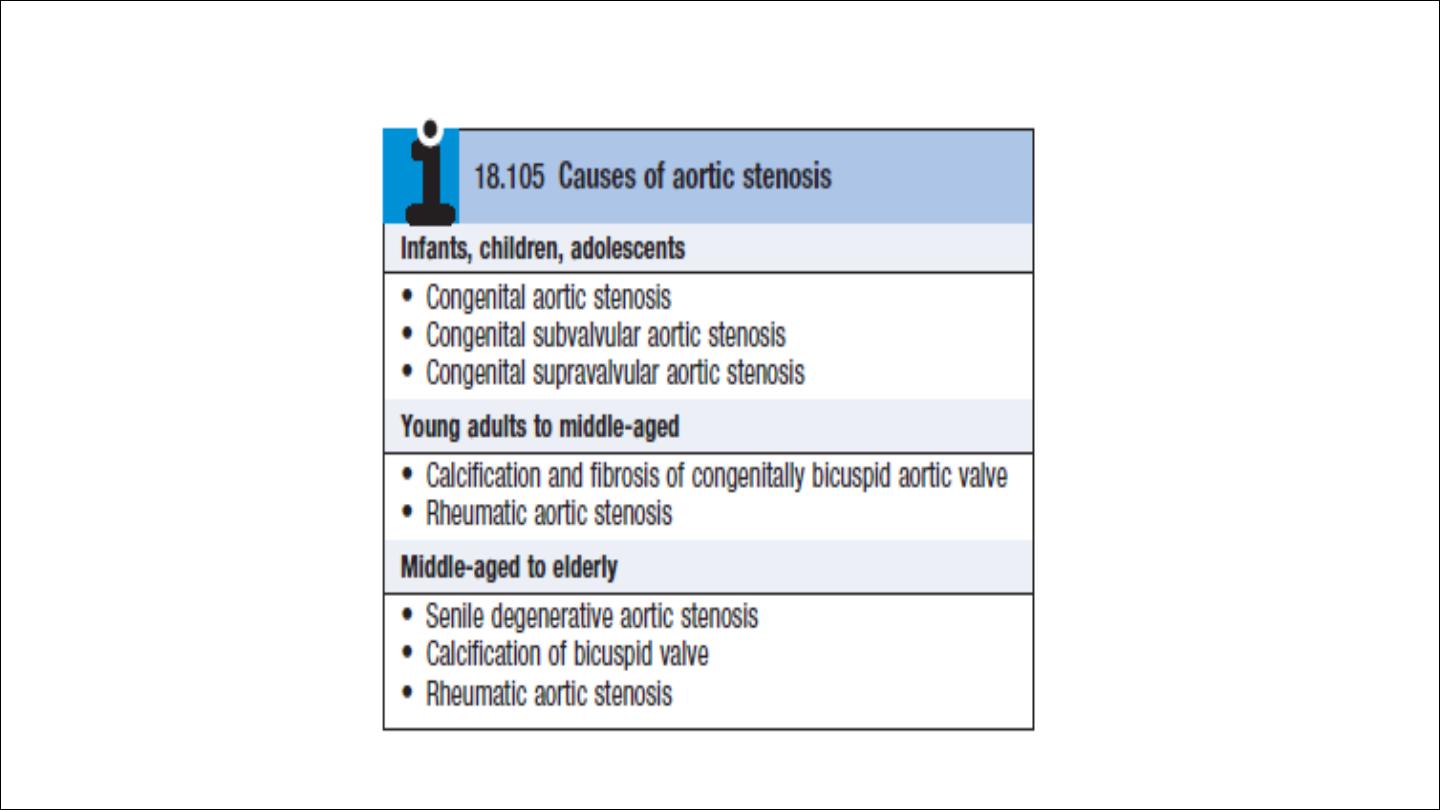
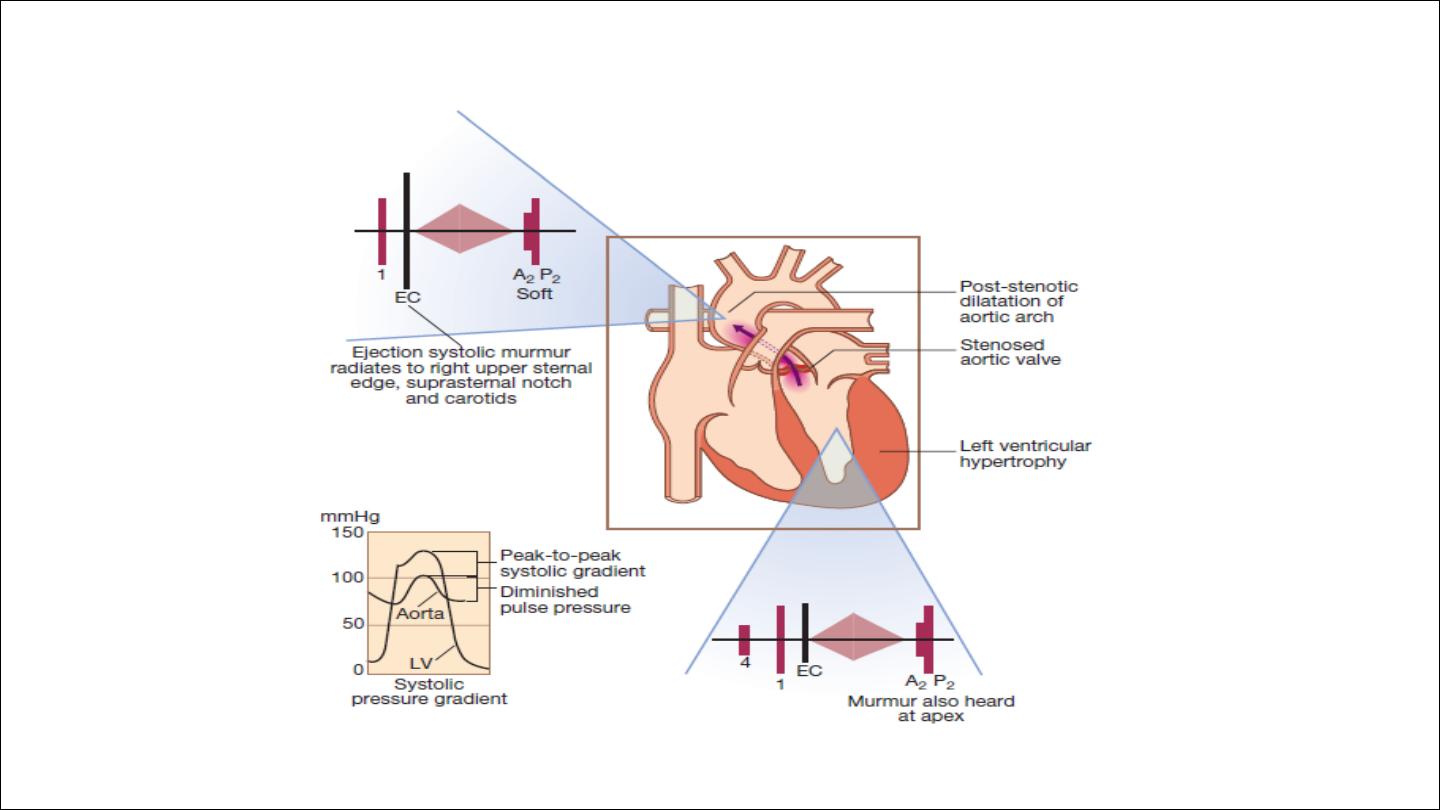
Aortic stenosis

AETIOLOGY AND PATHOPHYSIOLOGY
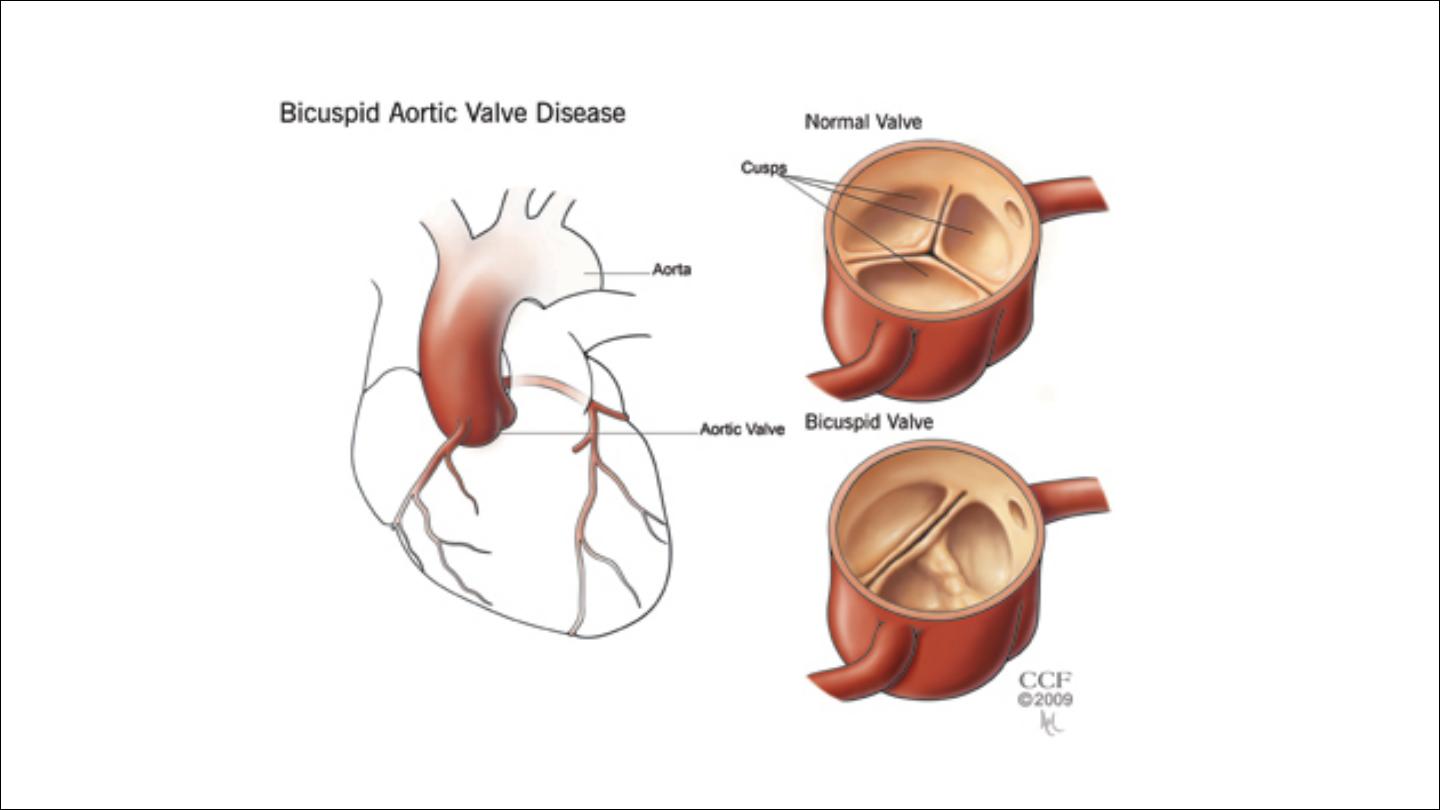
The likely aetiology depends on the age of the patient . In congenital
aortic stenosis, obstruction is present from birth or becomes apparent
in infancy. With bicuspid aortic valves, obstruction may take years to
develop as the valve becomes fibrotic and calcified.
The aortic valve is the second most frequently affected by rheumatic
fever and, commonly, both the aortic and mitral valves are involved. In
older people, a structurally normal tricuspid aortic valve may be
affected by fibrosis and calcification, in a process that is histologically
similar to that of atherosclerosis affecting the arterial wall.

Cardiac output is initially maintained at the cost of a steadily increasing
pressure gradient across the aortic valve. The LV becomes increasingly
hypertrophied and coronary blood flow may then be inadequate.
patients may therefore develop angina, even in the absence of
concomitant coronary disease. The fixed outflow obstruction limits the
increase in cardiac output required on exercise.
Eventually, the LV can no longer overcome the outflow tract
obstruction and pulmonary oedema supervenes.

Haemodynamically significant stenosis develops slowly, typically
occurring at 30–60 years in those with rheumatic disease, 50–60 in
those with bicuspid aortic valves and 70–90 in those with degenerative
calcific disease.
In contrast to patients with mitral stenosis, which tends to progress
very slowly, those with aortic stenosis typically remain asymptomatic
for many years but deteriorate rapidly when symptoms develop, and
death usually ensues within 3–5 years of these.
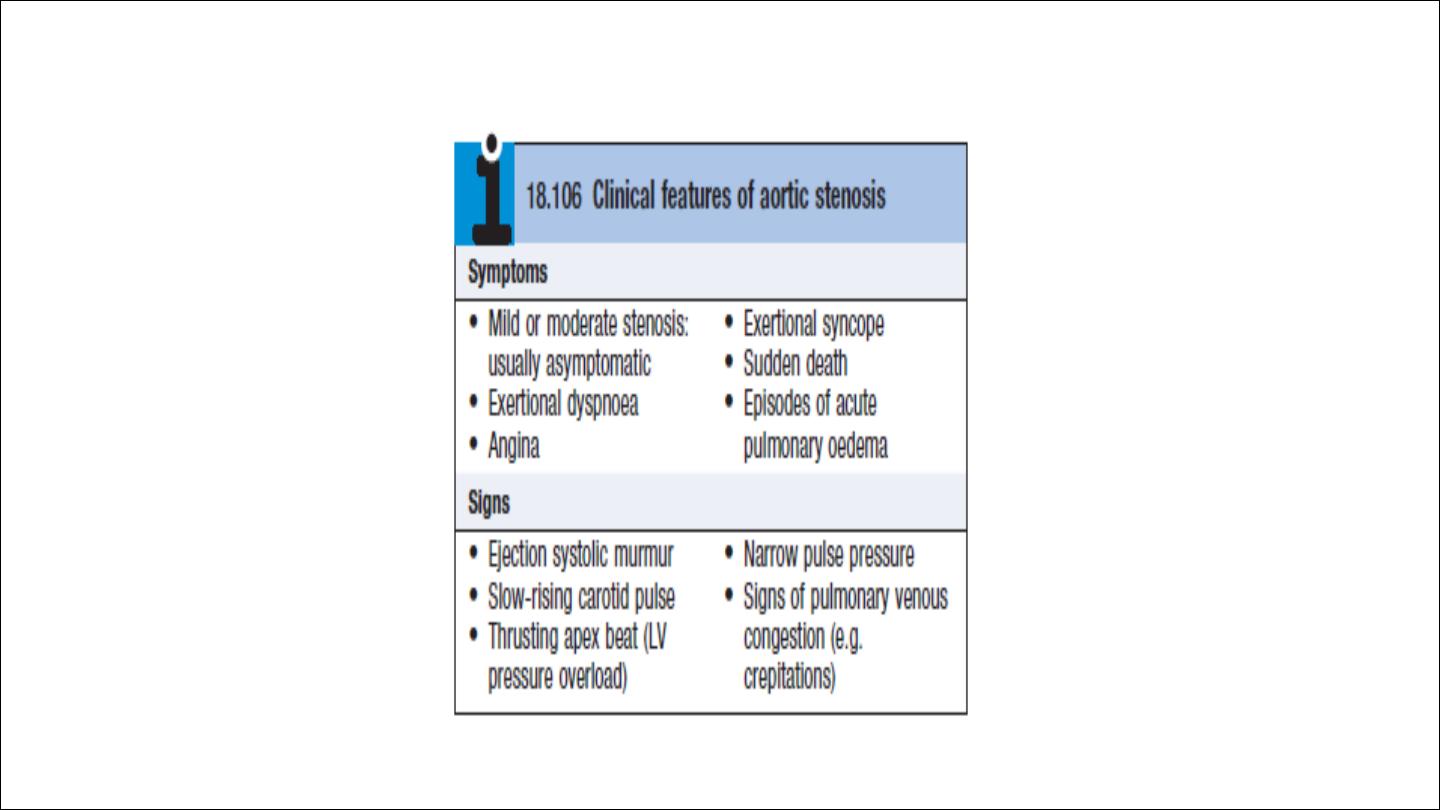

Clinical features
Mild and moderate are usually asymptomatic
Sever can be asymptomatic or symptomatic
Symptoms include
Angina : oxygen mismatch or coexistent CAD (50 %)
exertional Syncope: inability of CO to increase in the presence of fixed
LVOT obstruction

Pulse in AS in elderly can be normal because of stiff non compliant
arteries.
The murmur is often likened to a saw cutting wood and may (especially
in older patients) have a musical quality like the ‘mew’ of a seagull.
Clinical signs of severity
Loud murmur, thrill , soft A2, S4, heaving apex beat
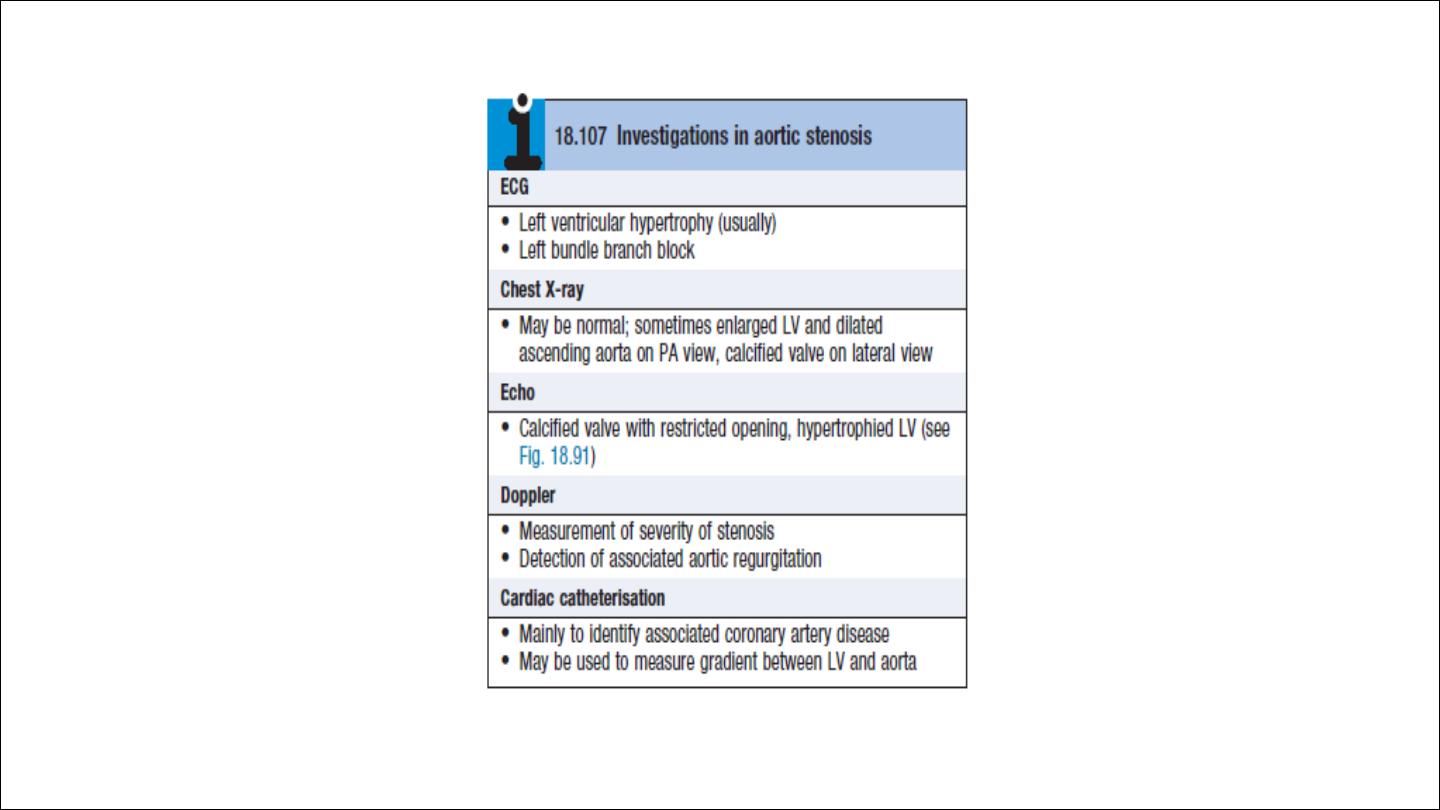

Management
Mild and moderate → asymptomatic
Sever if asymptomatic need only follow up every 1 year, consider
exercise testing
Symptomatic, death occur within 2 to 3 years so its an indication to
surgery.
Age is not a contraindication to valve replacement and results are very
good in experienced centers, even for those in their eighties.
Aortic balloon valvuloplasty is useful in congenital aortic stenosis but is
of no value in older patients with calcific aortic stenosis.

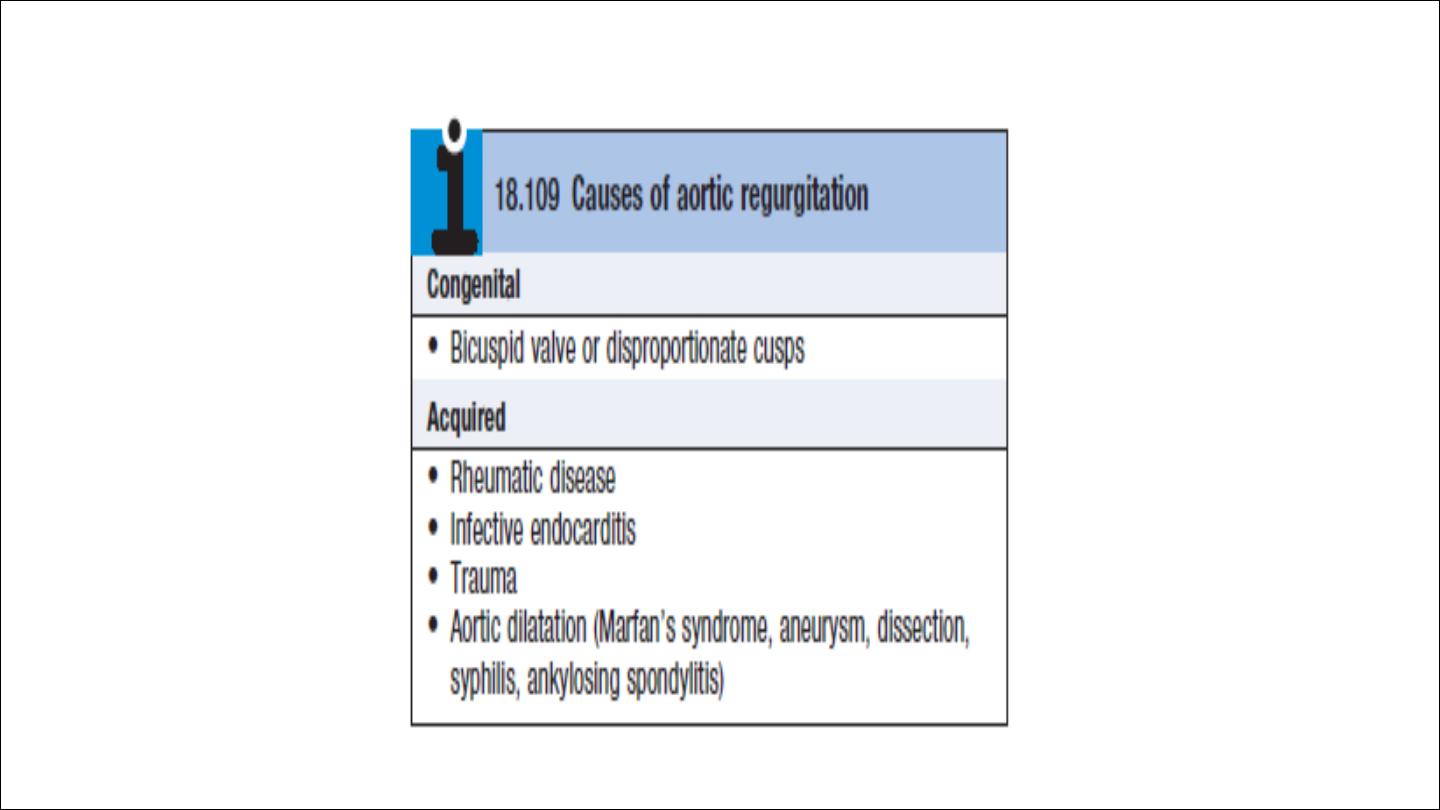
Aortic regurgitation
Aetiology and pathophysiology
This condition is due to disease of the aortic valve cusps
or dilatation of the aortic root.
The LV dilates and hypertrophies to compensate for the
regurgitation.
The stroke volume of the LV may eventually be doubled or
trebled, and the major arteries are then conspicuously
pulsatile.
As the disease progresses, left ventricular diastolic
pressure rises and breathlessness develops.
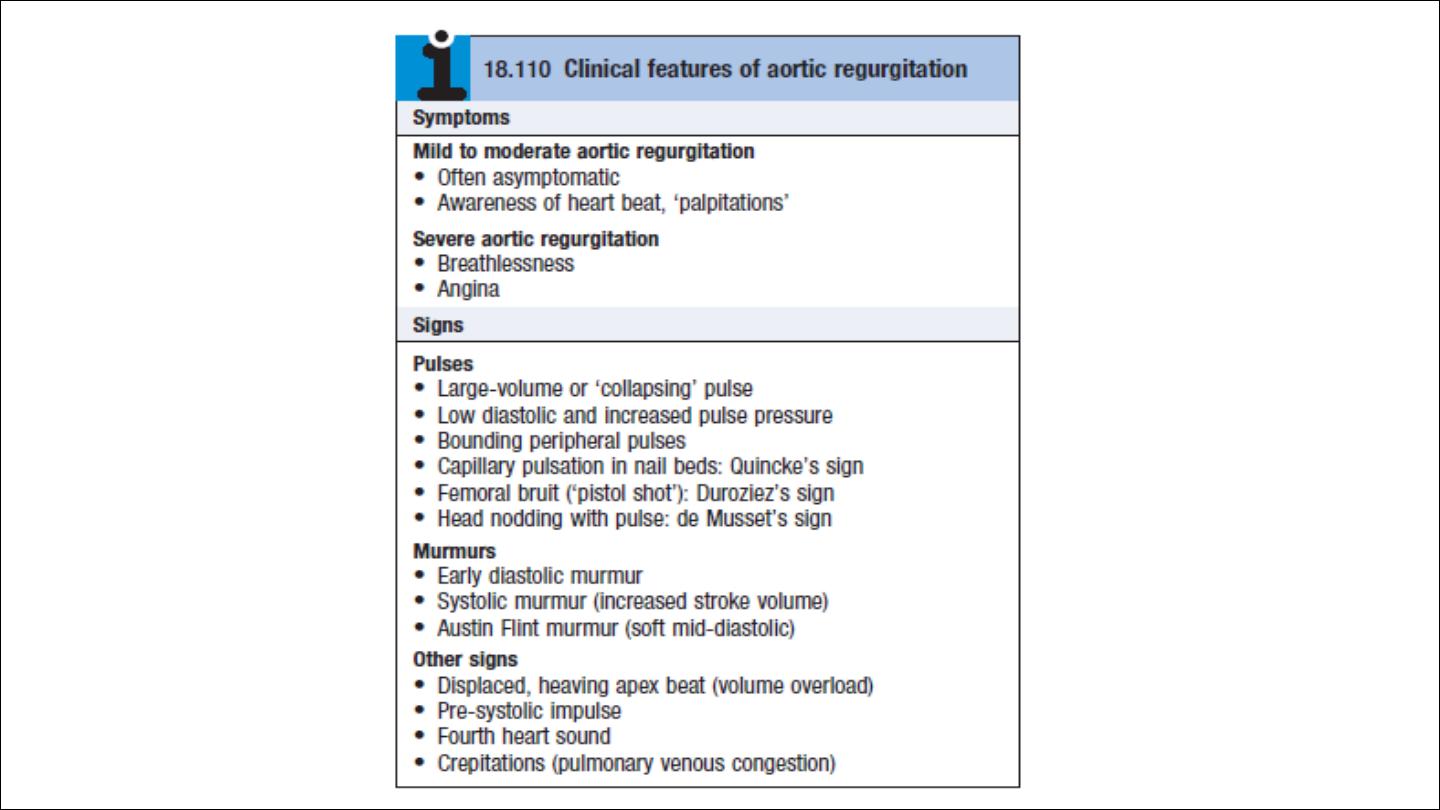
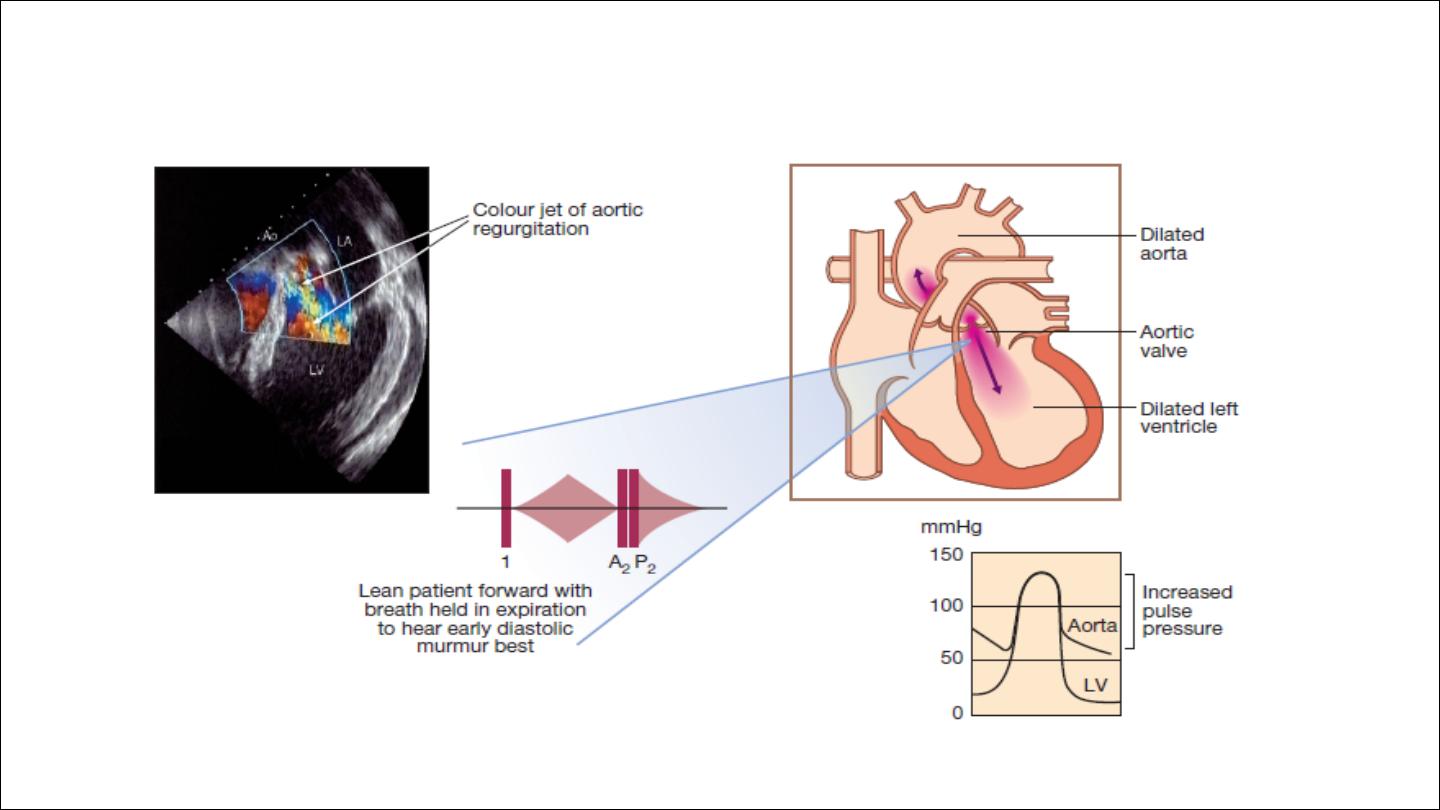
The regurgitant jet causes fluttering of the mitral valve and, if
severe, causes partial closure of the anterior mitral leaflet,
leading to functional mitral stenosis and a soft mid-diastolic
(Austin Flint) murmur.
In acute severe regurgitation (e.g. perforation of aortic cusp in
endocarditis), there may be no time for compensatory left
ventricular hypertrophy and dilatation to develop and the
features of heart failure may predominate. In this situation,
the classical signs of aortic regurgitation may be masked by
tachycardia and an abrupt rise in left ventricular end-diastolic
pressure thus, the pulse pressure may be near normal and the
diastolic murmur may be short or even absent.
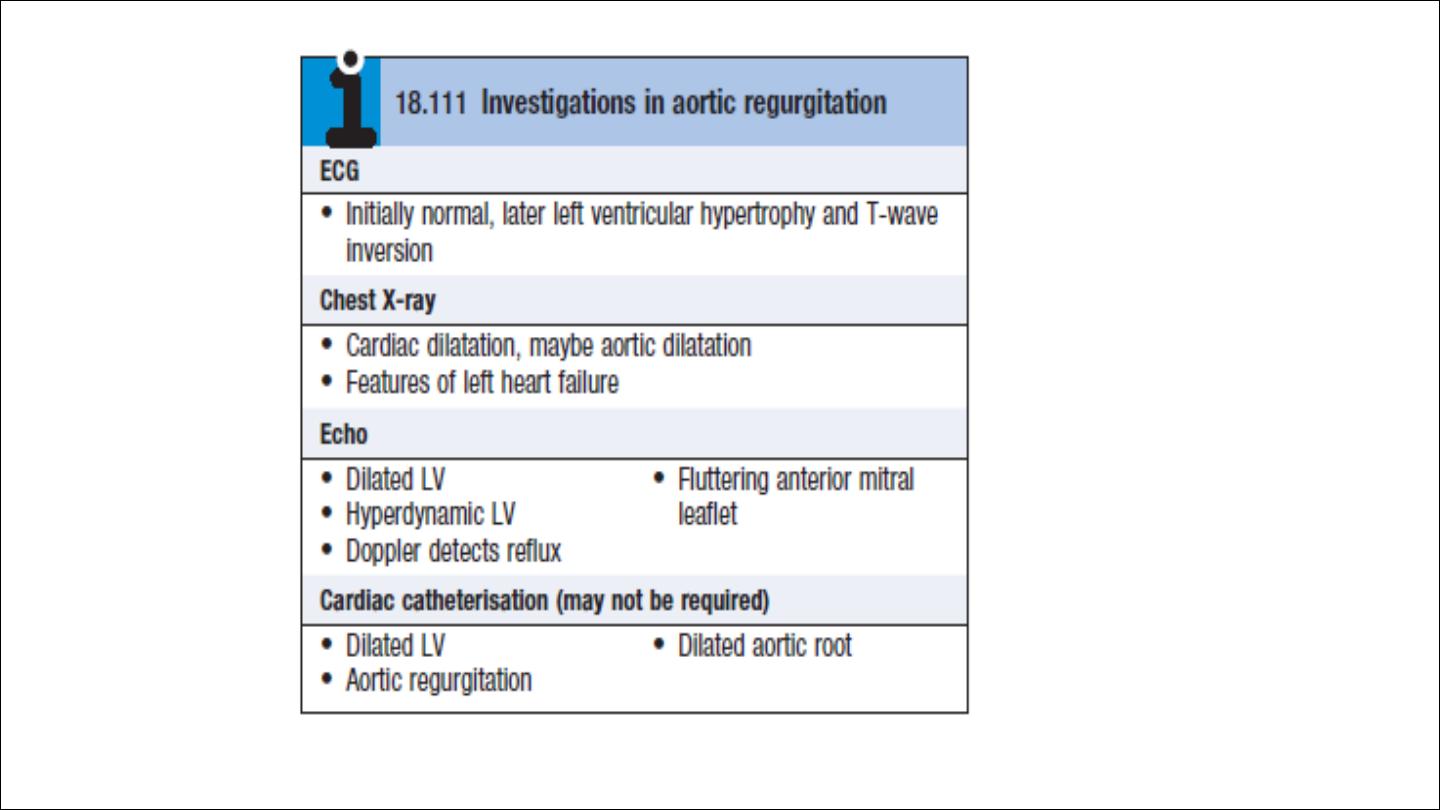

Management
Mild and moderate AR → asymptomatic → follow up
Severe asymptomatic → follow up
Severe symptomatic → AVR
AVR IN ASYMPTOMATIC PATIENTS
1. EF LESS THAN 50 %
2. LVESD MORE THAN 55 MM
3. LVEDD MORE THAN 65 MM

Tricuspid stenosis
Usually rheumatic in origin
Almost always associated with aortic and mitral valve disease
Clinical feature
Symptoms of right sided heart failure
Prominent a wave, slow y descent
Mid diastolic murmur higher pitch than MS, increase with inspiration.
Presystolic hepatic pulsation
Mangement
Surgery
Balloon valvoplasty
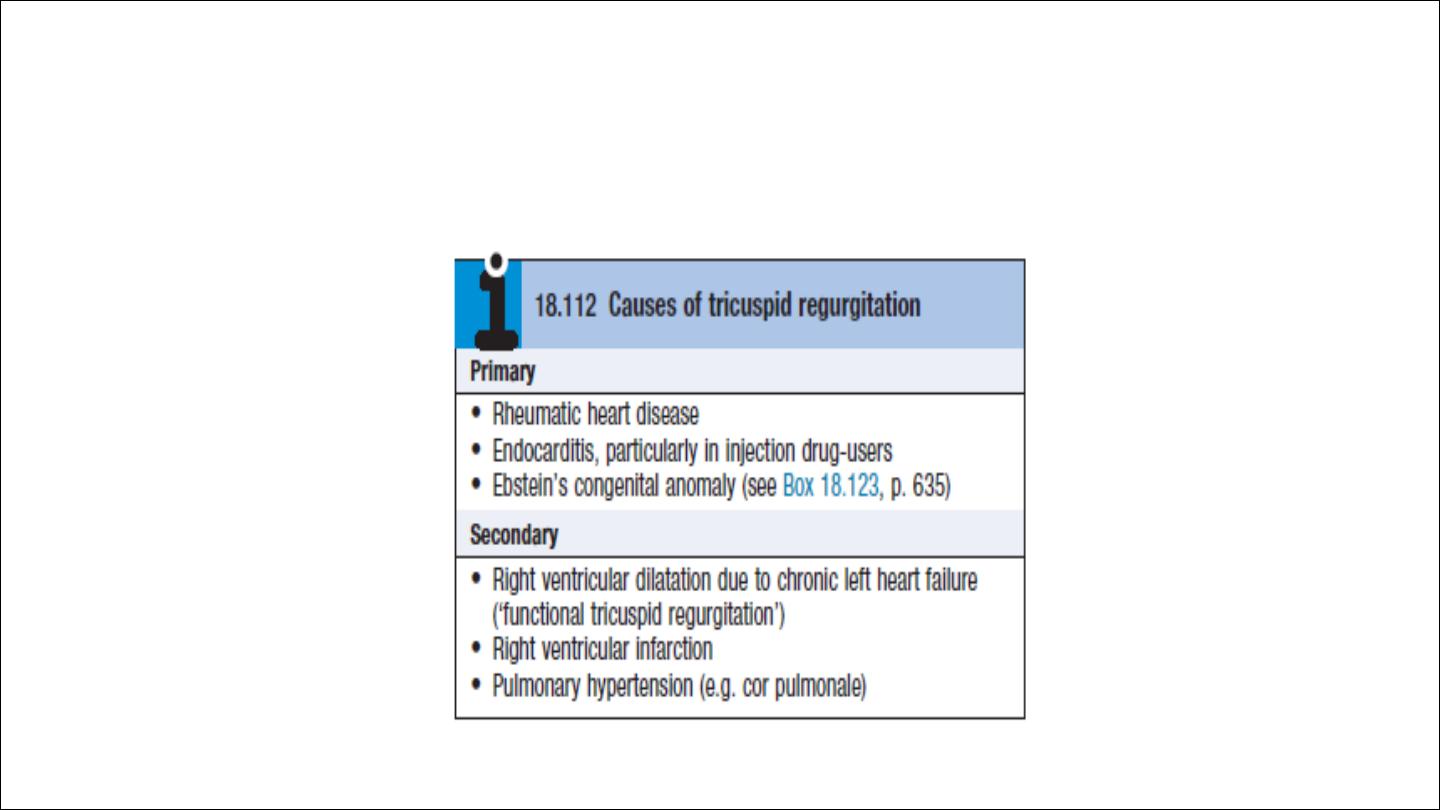
Tricuspid regurgitation
Tricuspid regurgitation is common, and is most frequently ‘functional’
as a result of right ventricular dilatation.

Management
•
Tricuspid regurgitation due to right ventricular dilatation often
improves when the cardiac failure is treated. Patients with a
normal pulmonary artery pressure tolerate isolated tricuspid reflux
well, and valves damaged by endocarditis do not usually need to
be replaced.
•
Patients undergoing mitral valve replacement, who have tricuspid
regurgitation due to marked dilatation of the tricuspid annulus,
benefit from valve repair with an annuloplasty ring to bring the
leaflets closer together. Those with rheumatic damage may require
tricuspid valve replacent

Pulmonary stenosis
Usually congenital, or associated with carcinoid syndrome
Clinical features:
Ejection systolic murmur, loudest at the left upper sternum and radiating
towards the left shoulder. There may be a thrill, best felt when the patient leans
forward and breathes out. The murmur is often preceded by an ejection sound
(click).
Management:
Mild to moderate PS need no treatment. Severe pulmonary stenosis (resting
gradient > 50 mmHg with a normal cardiac output) is treated by percutaneous
pulmonary balloon valvuloplasty or, if this is not available, by surgical
valvotomy. Long-term results are very good. Post-operative pulmonary
regurgitation is common but benign.
