
ATHEROSCLEROSIS
ATHEROSCLEROSIS
Atherosclerosis can affect any artery in the body
Occult coronary artery disease is common in those
who present with other forms of atherosclerotic
vascular disease

PATHOPHYSIOLOGY
Type I ( initial lesion)
: isolated macrophage ,foam
cells
Type II ( fatty streak)
: intracellular lipid
Type III (intermediate lesion
); type II+ small
extracellular lip[id pool
Type IV (atheroma lesion)
:type II + core of
extracellular lipid pool
Type V (fibroatheroma
): Lipid core + fibrotic layer
Type VI (complicated
): surface defect , hematoma
;hemorrhage ; thrombus

EARLY ATHEROSCLEROSIS
Atherosclerosis begins early in life
Early atherosclerotic lesions have been found in the
arteries of victims of accidental death in the second
and third decades of life
Fatty streaks tend to occur at sites of altered arterial
shear stress
They develop when inflammatory cells, predominantly
monocytes, bind to receptors expressed by
endothelial cells, migrate into the intima, take up
oxidised low-density lipoprotein (LDL) particles and
become lipid-laden macrophages or foam cells
ADVANCED
ATHEROSCLEROSIS
In an established atherosclerotic plaque,
macrophages mediate inflammation and smooth
muscle cells promote repair.
Any breach in the integrity of the plaque will
expose its contents to blood, and trigger platelet
aggregation and thrombosis that extend into the
atheromatous plaque and the arterial lumen

'Vulnerable' plaques are characterised by a lipid-rich
core, a thin fibrocellular cap and an increase in
inflammatory cells that release specific enzymes to
degrade matrix proteins. In contrast, stable plaques are
typified by a small lipid pool, a thick fibrous cap,
calcification and plentiful collagenous cross-struts
Atherosclerosis may induce complex changes in the
media that lead to arterial remodelling ( posative and
negative)

RISK FACTORS
Age and sex.
Family history.
Smoking.
Hypertension
Hypercholesterolaemia
Diabetes mellitus.
Haemostatic factors.
Physical activity.
Obesity
Alcohol.
Other dietary factors.
Personality.
Social deprivation.

PREVENTION
Primary prevention
Secondary prevention
CORONARY ARTERY DISEASE
Coronary artery disease (CAD) is the most common form
of heart disease
By 2020, it is estimated that it will be the major
cause of death in all regions of the world.
Occasionally, the coronary arteries are involved in other
disorders such as aortitis, polyarteritis and other
connective tissue disorders.
CORONARY ARTERY DISEASE: CLINICAL
MANIFESTATIONS AND PATHOLOGY
Stable angina Ischaemia due to fixed atheromatous
stenosis of one or more coronary arteries
Unstable angina Ischaemia caused by dynamic
obstruction of a coronary artery due to plaque rupture or
erosion with superimposed thrombosis
Myocardial infarction Myocardial necrosis caused by
acute occlusion of a coronary artery due to plaque rupture
or erosion with superimposed thrombosis
Heart failure Myocardial dysfunction due to infarction or
ischaemia
Arrhythmia Altered conduction due to ischaemia or
infarction
Sudden death Ventricular arrhythmia, asystole or massive
myocardial infarction

STABLE ANGINA
is the symptom complex caused by transient
myocardial ischaemia and constitutes a clinical
syndrome rather than a disease.
imbalance between myocardial oxygen supply and
demand
may be a manifestation of other forms of heart
disease, particularly aortic valve disease and
hypertrophic cardiomyopathy
FACTORS INFLUENCING MYOCARDIAL OXYGEN SUPPLY AND
DEMAND
Oxygen demand: cardiac work
Heart rate
BP
Myocardial contractility
Left ventricular hypertrophy
Valve disease, e.g. aortic stenosis
Oxygen supply: coronary blood flow
Duration of diastole
Coronary perfusion pressure (aortic diastolic minus coronary sinus or right
atrial diastolic pressure)
Coronary vasomotor tone
Oxygenation
Haemoglobin
Oxygen saturation

ACTIVITIES PRECIPITATING
ANGINA
Common
Physical exertion
Cold exposure
Heavy meals
Intense emotion
Uncommon
Lying flat (decubitus angina)
Vivid dreams (nocturnal angina)

INVESTIGATIONS
Resting ECG
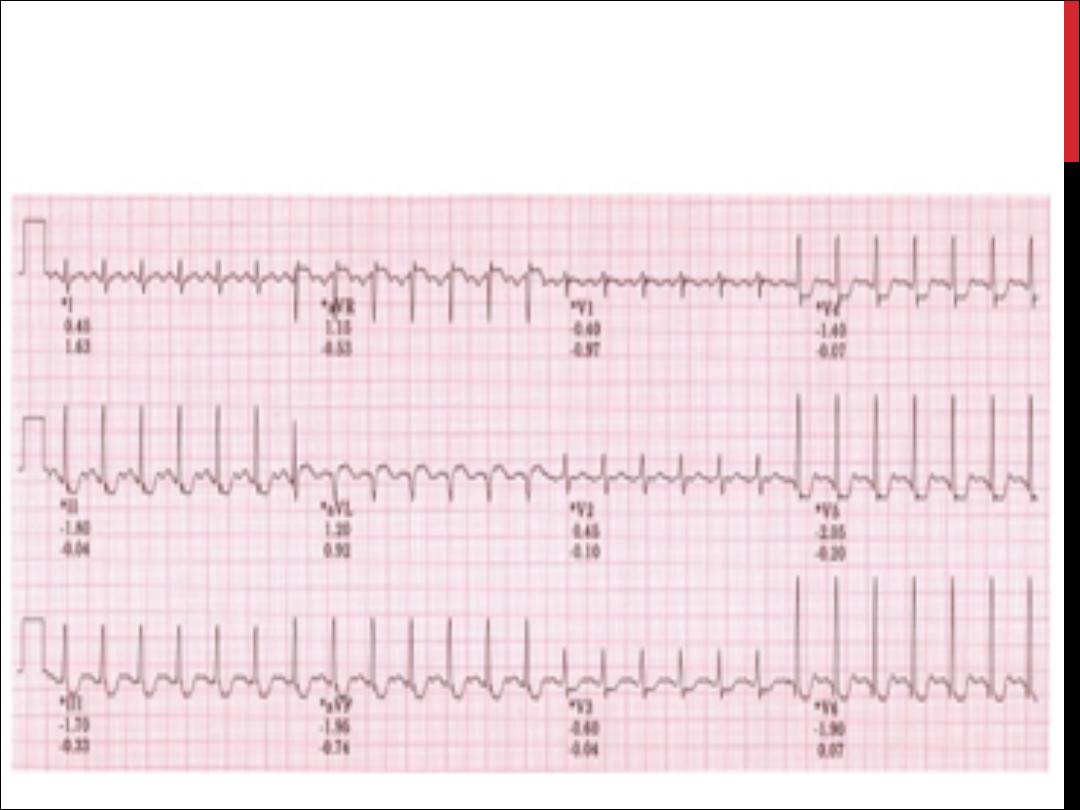
Exercise ECG
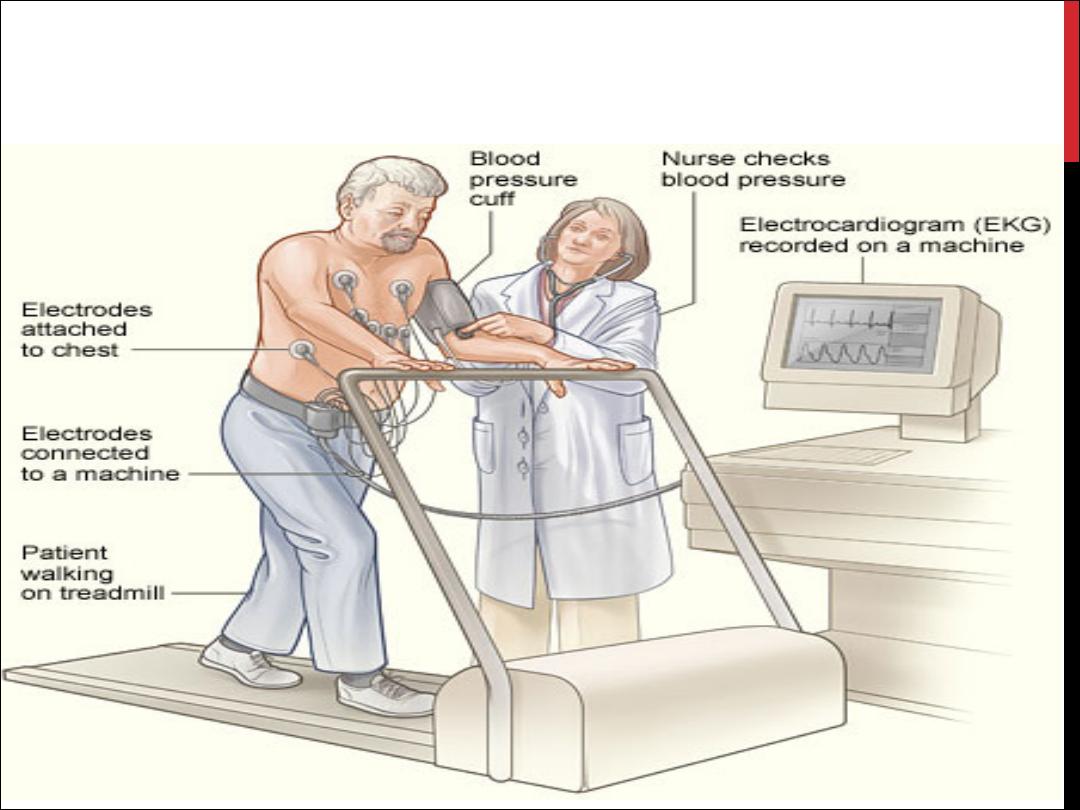
EXERCISE ECG

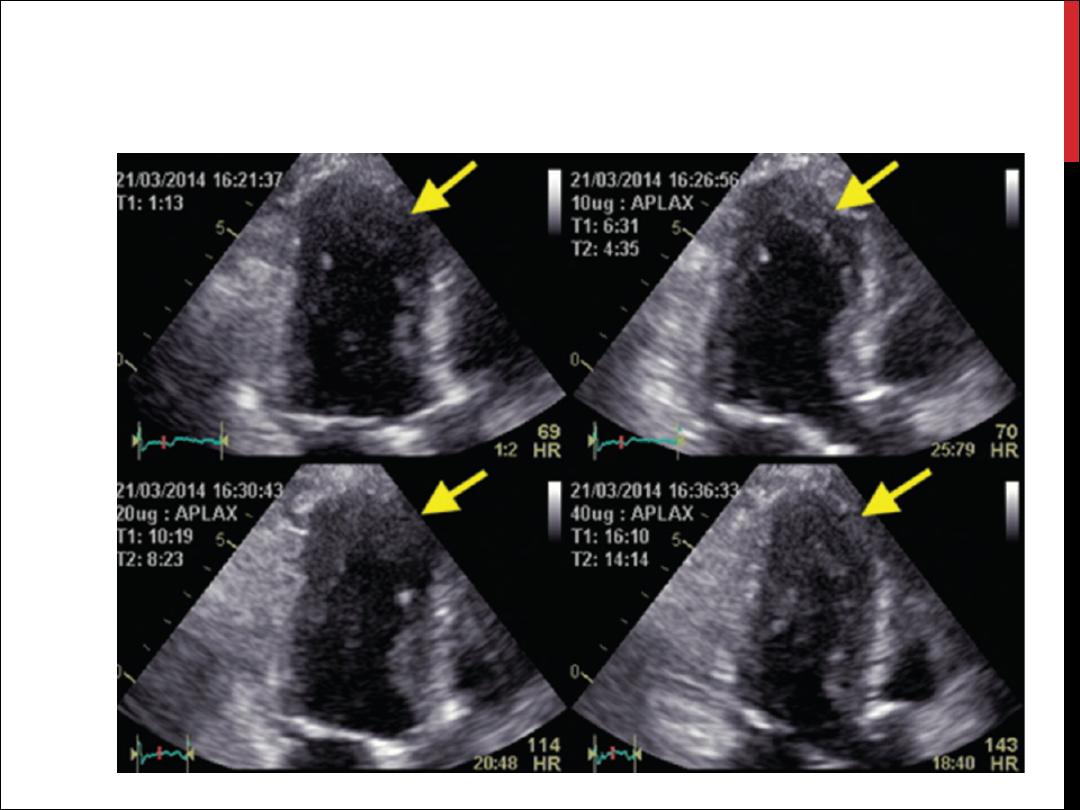
OTHER FORMS OF STRESS
TESTING
Stress echocardiography
Myocardial perfusion scanning
Coronary arteriography
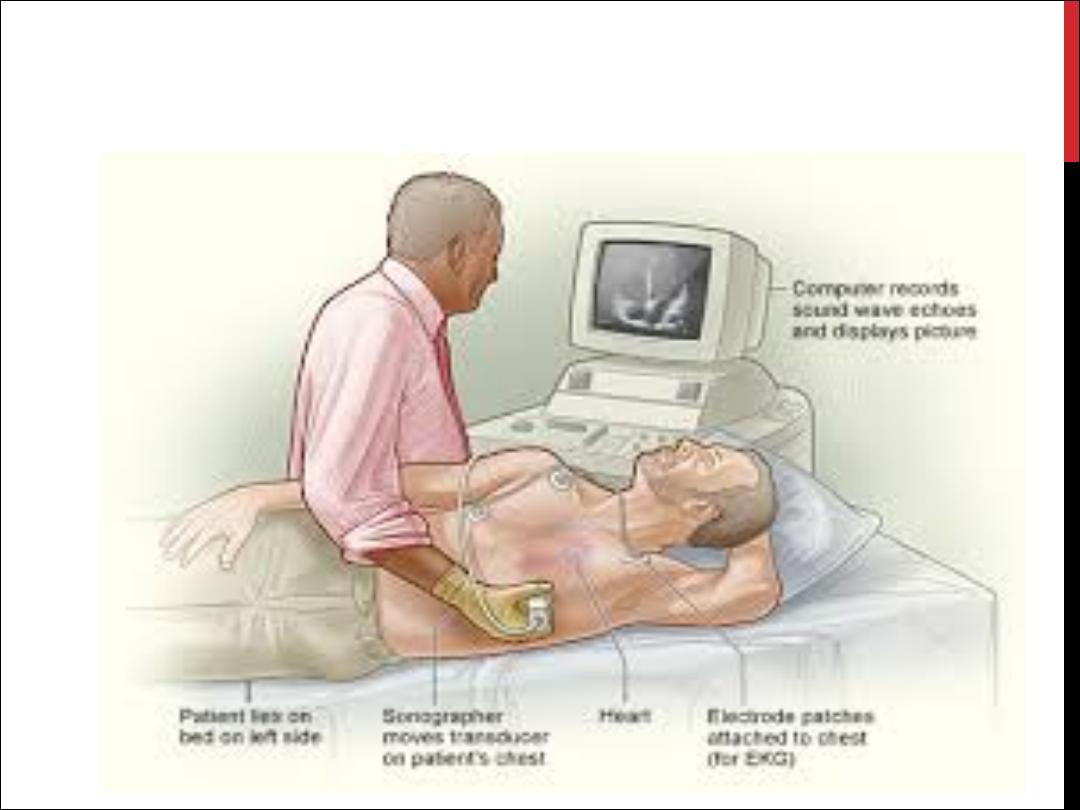
STRESS ECHO
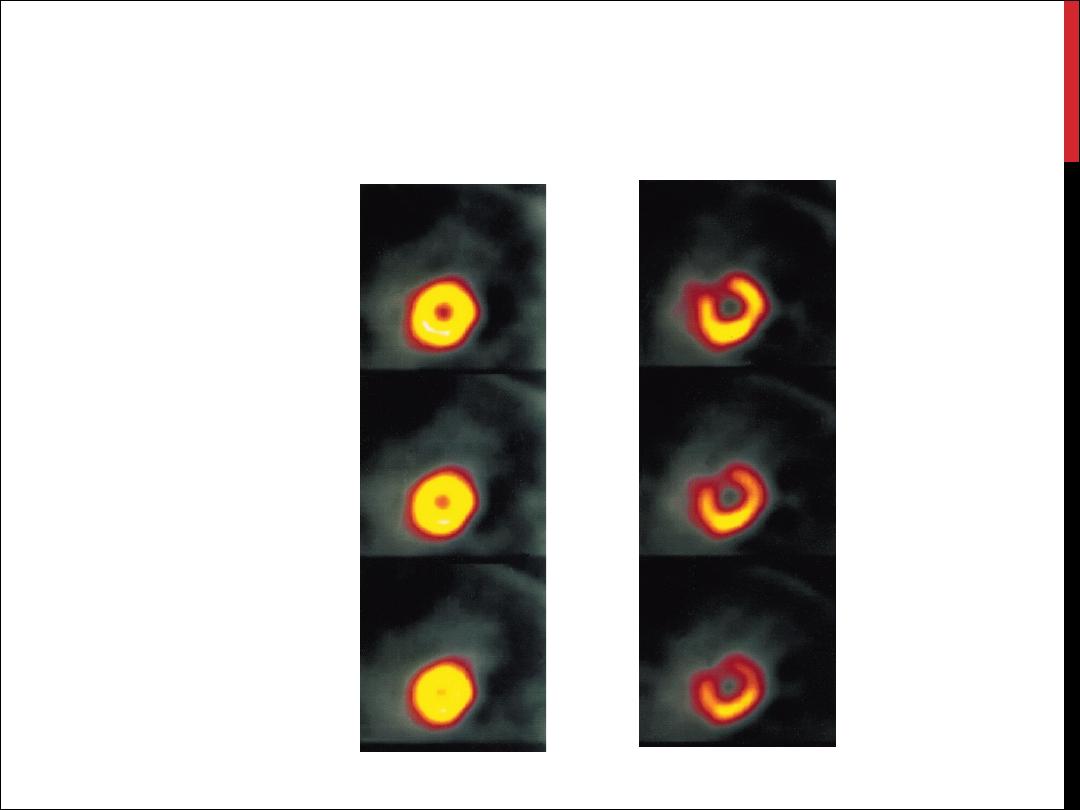
MYOCARDIAL PERFUSION
SCANNING
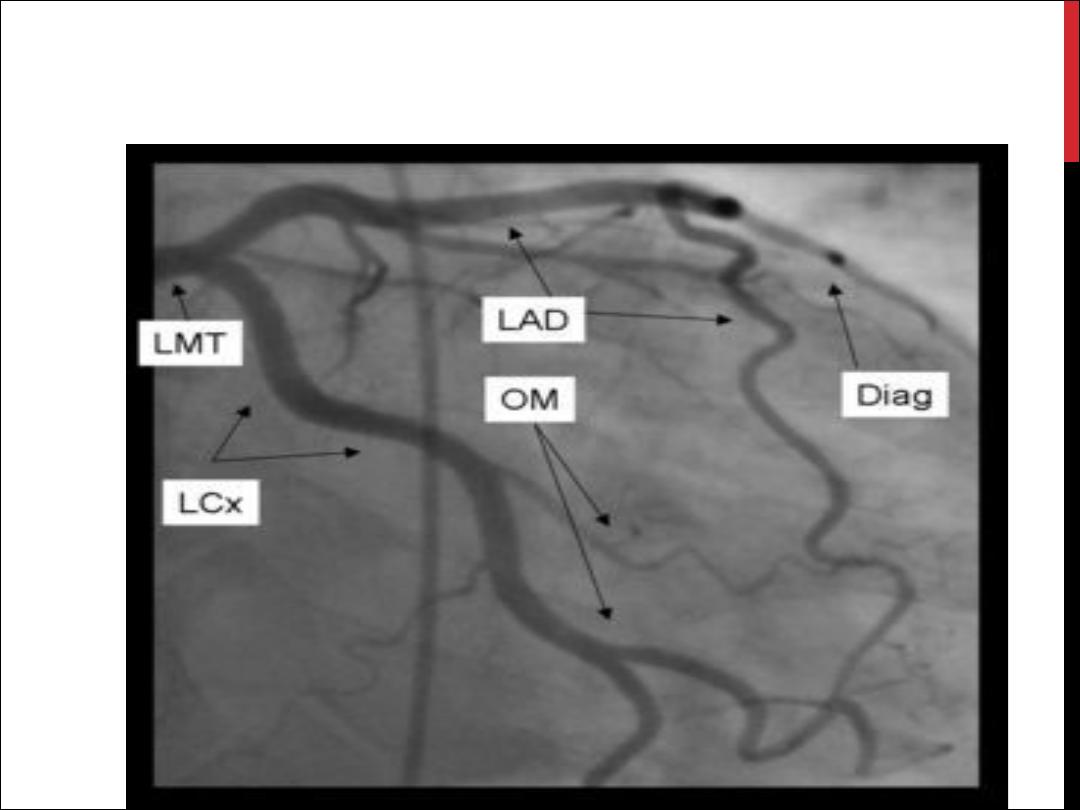
CORONARY ANGIO.

RISK STRATIFICATION IN STABLE ANGINA
High risk
Low risk
Post-infarct angina
Predictable exertional angina
Poor effort tolerance
Good effort tolerance
Ischaemia at low workload
Ischaemia only at high workload
Left main or three-vessel disease
Single-vessel or two-vessel disease
Poor LV function
Good LV function

MANAGEMENT: GENERAL
MEASURES
a careful assessment of the likely extent and
severity of arterial disease
the identification and control of risk factors
such as smoking, hypertension and
hyperlipidaemia
the use of measures to control symptoms
the identification of high-risk patients for
treatment to improve life expectancy.
ADVICE TO PATIENTS WITH STABLE
ANGINA
Ø
Do not smoke
Ø
Aim for ideal body weight
Ø
Take regular exercise (exercise up to, but not
beyond, the point of chest discomfort is beneficial
and may promote collateral vessels)
Ø
Avoid severe unaccustomed exertion, and
vigorous exercise after a heavy meal or in very
cold weather
Ø
Take sublingual nitrate before undertaking
exertion that may induce angina

PHARMACOLOGICAL THERAPY
Antiplatelet therapy
Anti-anginal drug treatment
Nitrates
Beta-blockers
Calcium channel antagonists
Potassium channel activators
I
f
channel antagonist
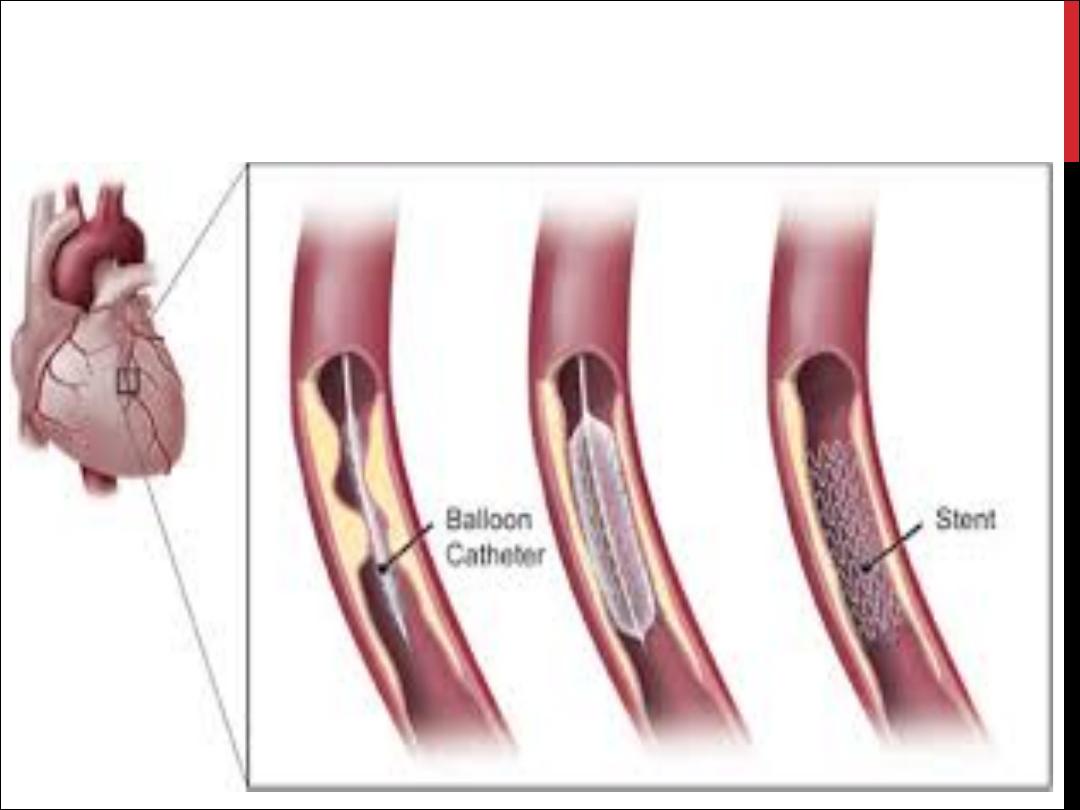
INVASIVE THERAPY : PCI AND CABG
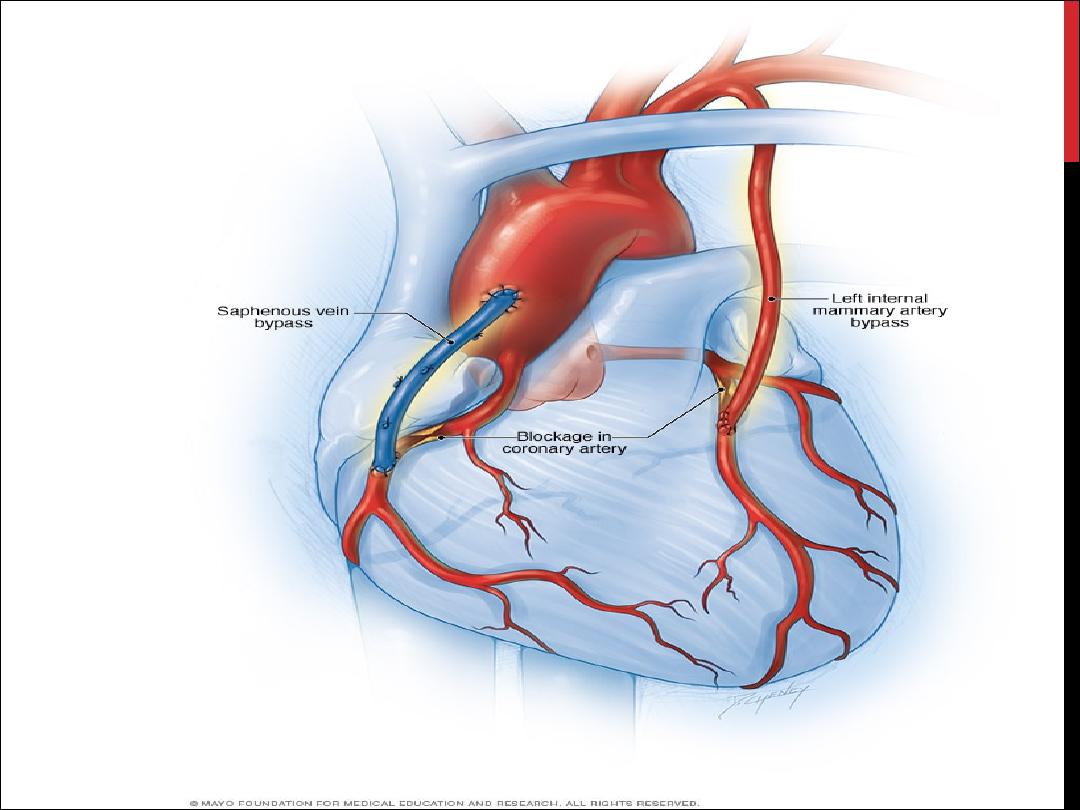
COMPARISON OF PCI AND CABG
PCI
CABG
Death
>
0.5
%
>
1.5
%
Myocardial infarction*
2
%
10
%
Hospital stay
12-36 hrs
5-8 days
Return to work
2-5 days
6-12 wks
Recurrent angina
15-20% at 6 mths
10% at 1 yr
Repeat revascularisation
10-20% at 2 yrs
2% at 2 yrs
Neurological complications Rare
Common (see text)
Other complications
Emergency CABG
Vascular damage related to
access site
Diffuse myocardial damage
Infection (chest, wound)
Wound pain

PROGNOSIS
Symptoms are a poor guide to prognosis
Exercise testing and other forms of stress testing
are much more powerful predictors of mortality
In general, the prognosis of coronary artery
disease is related to the number of diseased
vessels and the degree of left ventricular
dysfunction.

ANGINA WITH NORMAL CORONARY
ARTERIES
Coronary artery spasm
Syndrome X

ACUTE CORONARY SYNDROME
Unstable Angina
MI
The culprit lesion is usually a complex ulcerated or
fissured atheromatous plaque with adherent platelet-rich
thrombus and local coronary artery spasm

CLINICAL FEATURES
Symptoms
Prolonged cardiac pain: chest, throat, arms, epigastrium or back
Anxiety and fear of impending death
Nausea and vomiting
Breathlessness
Collapse/syncope
Physical signs
Signs of sympathetic activation: pallor, sweating, tachycardia
Signs of vagal activation: vomiting, bradycardia
Signs of impaired myocardial function
•
Hypotension, oliguria, cold peripheries
•
Narrow pulse pressure
•
Raised JVP
•
Third heart sound
•
Quiet first heart sound
•
Diffuse apical impulse
•
Lung crepitations
Signs of tissue damage: fever
Signs of complications: e.g. mitral regurgitation, pericarditis

DIAGNOSIS AND RISK
STRATIFICATION
The differential diagnosis is wide
The assessment of acute chest pain depends heavily on an
analysis of the character of the pain and its associated
features
ECG and Biochemical markers
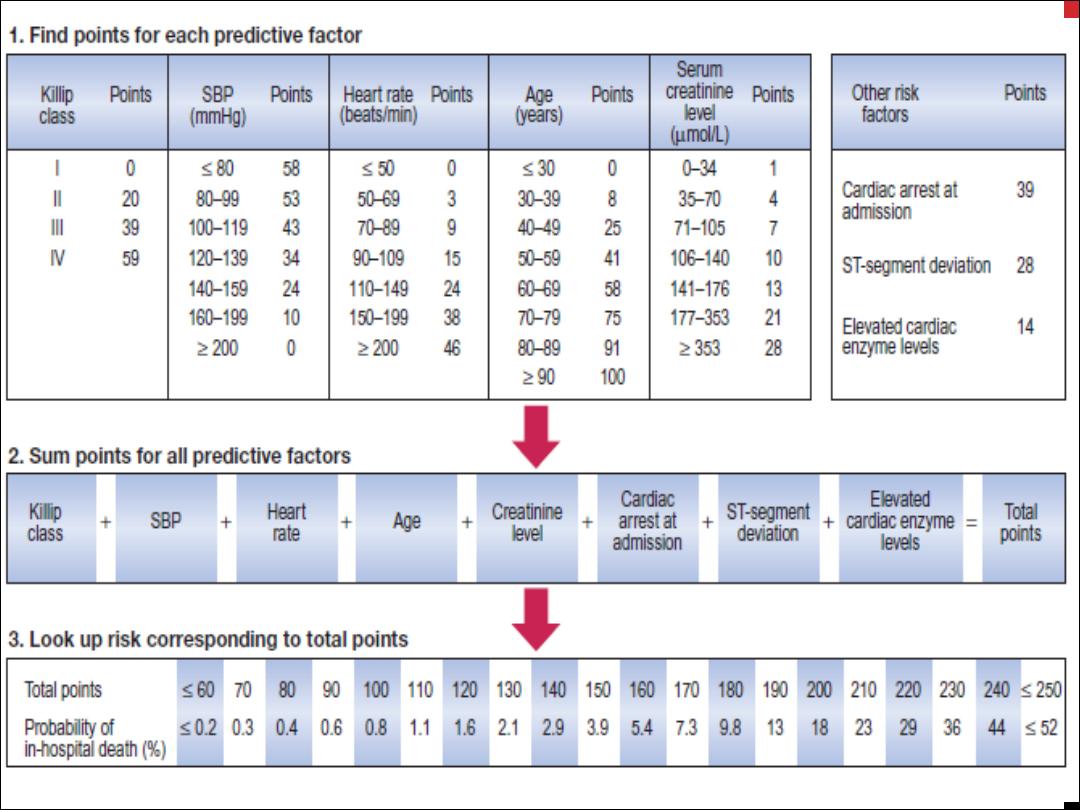
Risk stratification is important because it guides the use of
more complex pharmacological and interventional
treatment (
GRACE
)
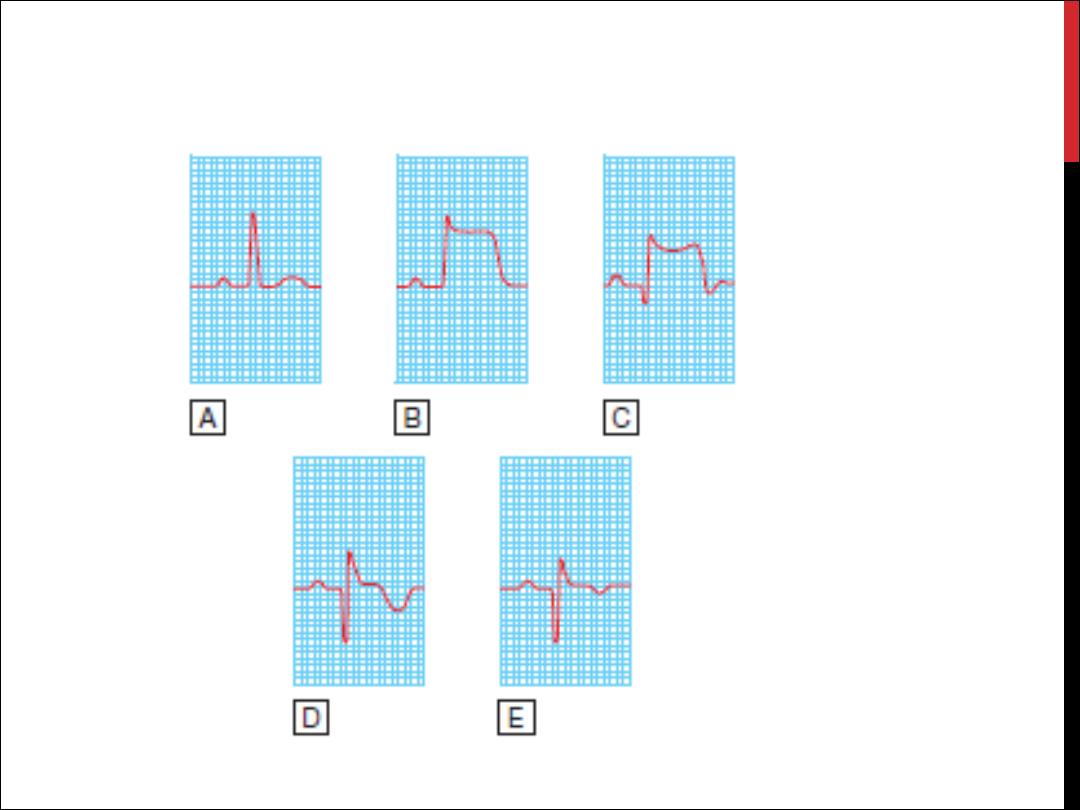
INVESTIGATIONS : ECG
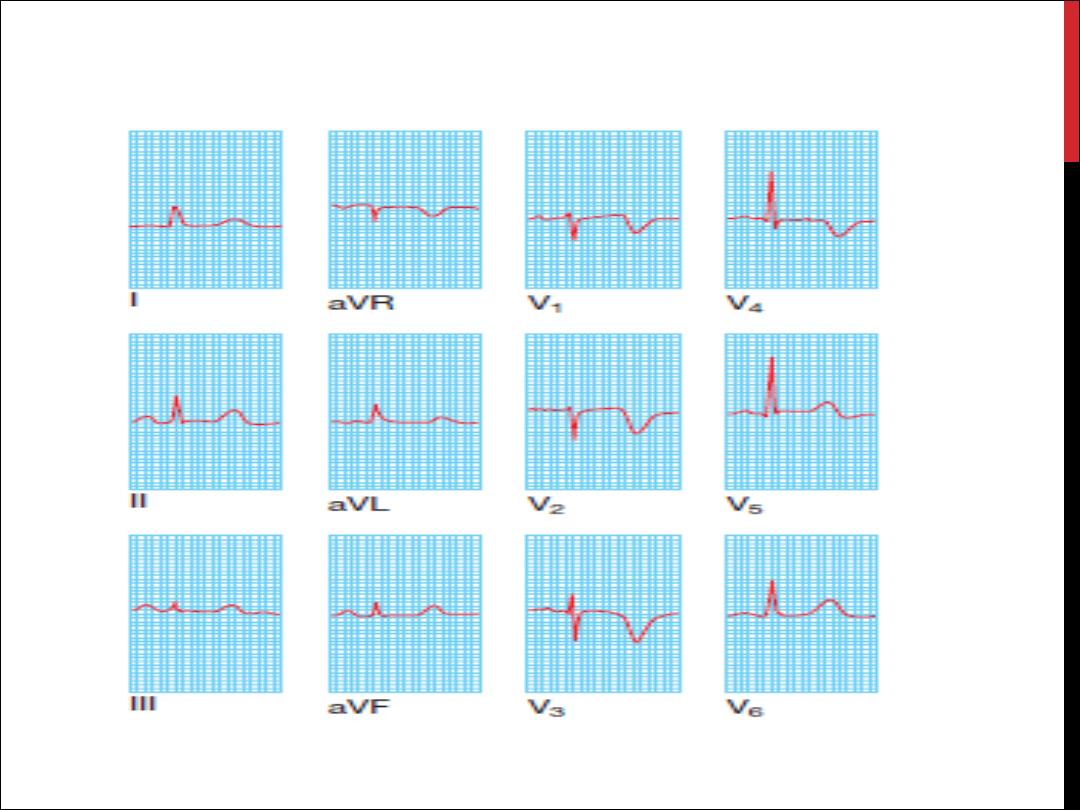
NON STEMI
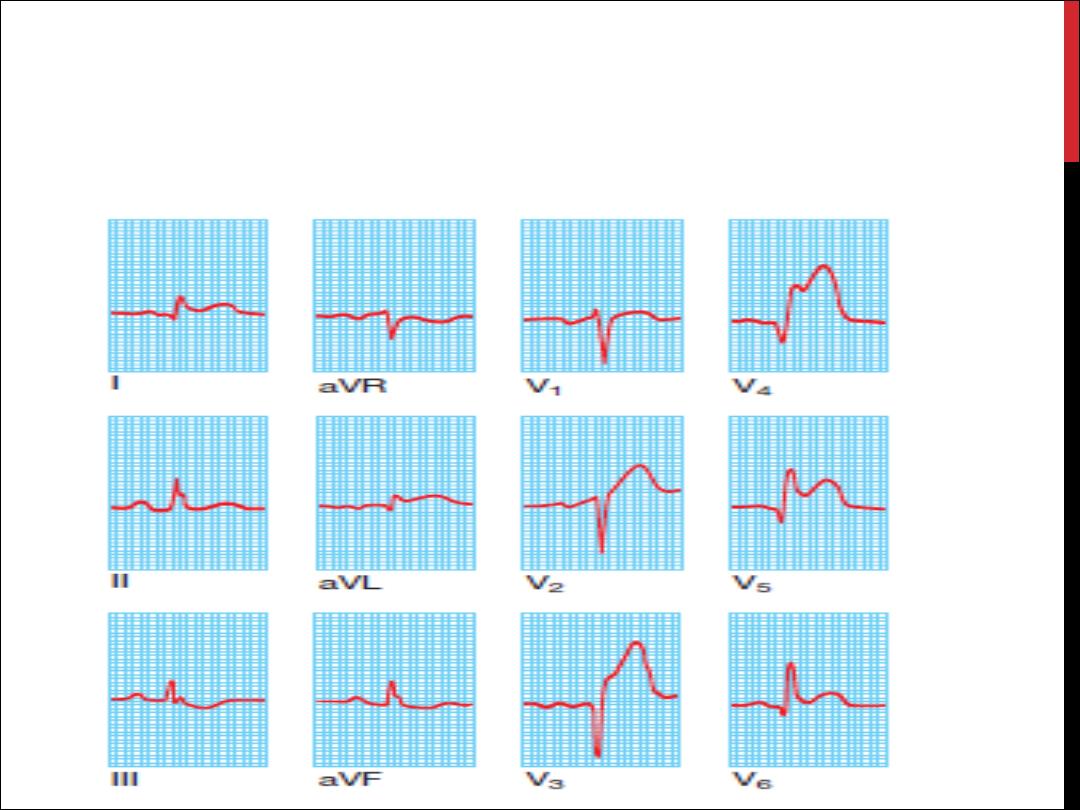
ANTERIOR STEMI
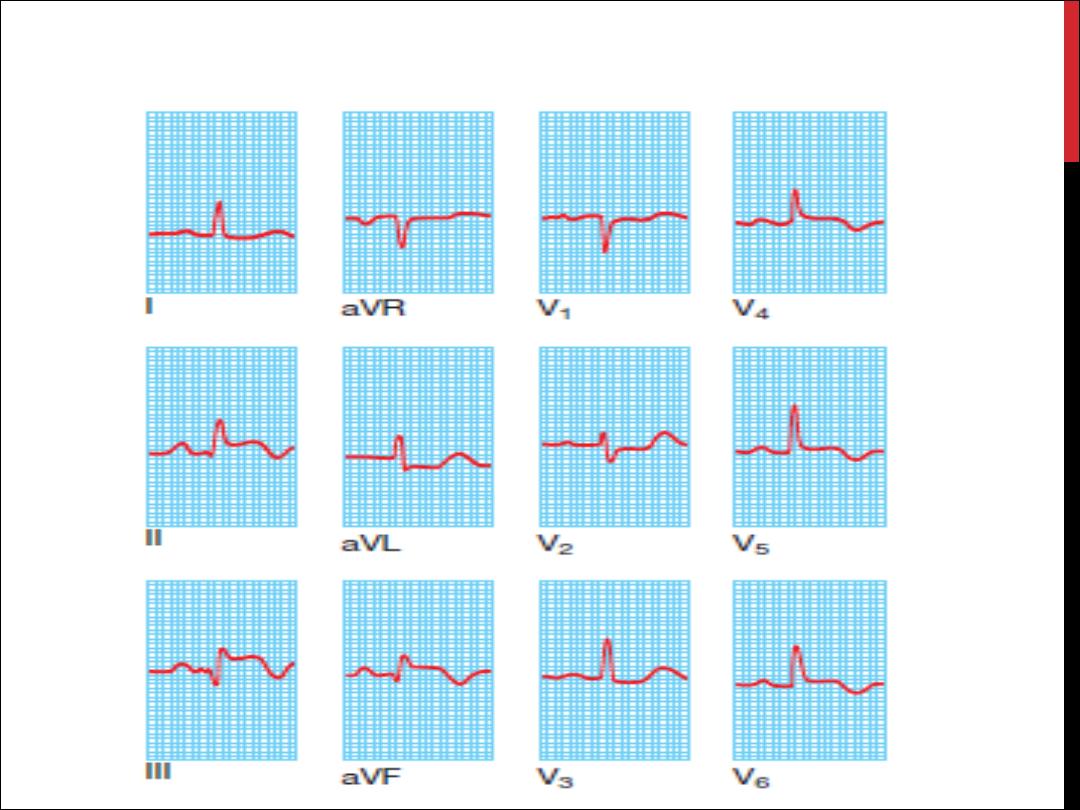
INFEROLATERAL STEMI
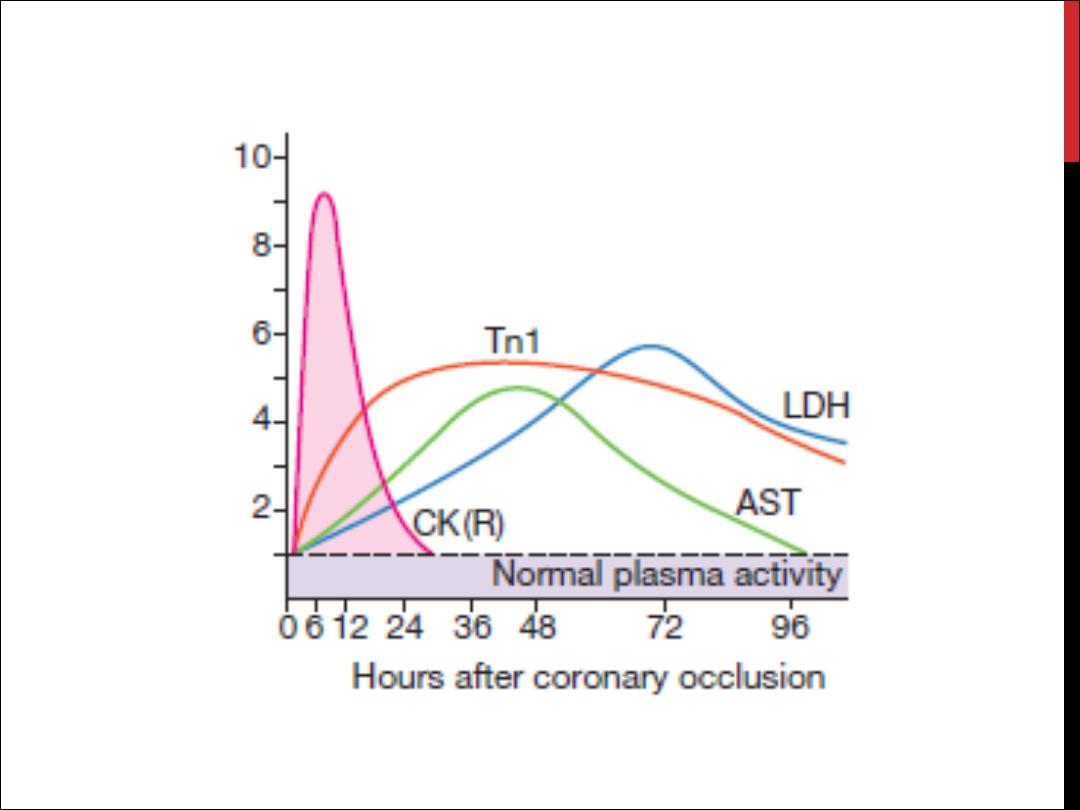
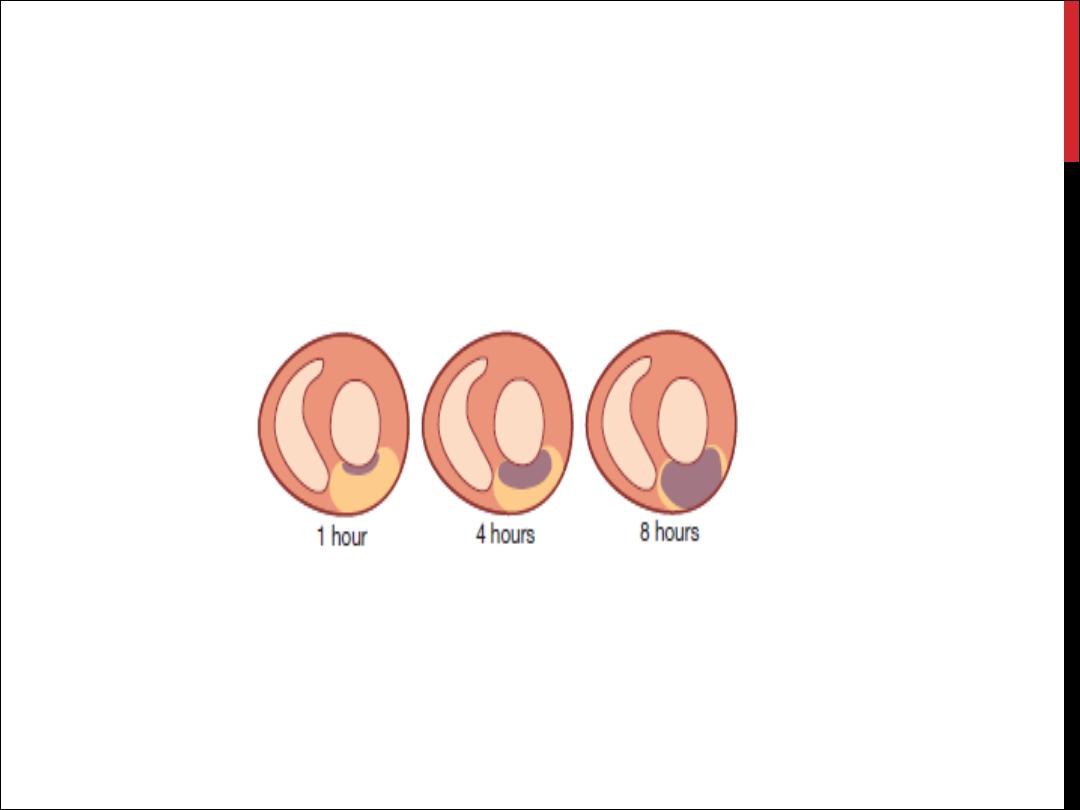
PLASMA CARDIAC BIOMARKERS
Other blood tests
Chest X-ray
Echocardiography

IMMEDIATE MANAGEMENT: THE
FIRST
12 HOURS
Addmission
Analgesia
Antithrombotic therapy
Anti-anginal therapy
Reperfusion therapy
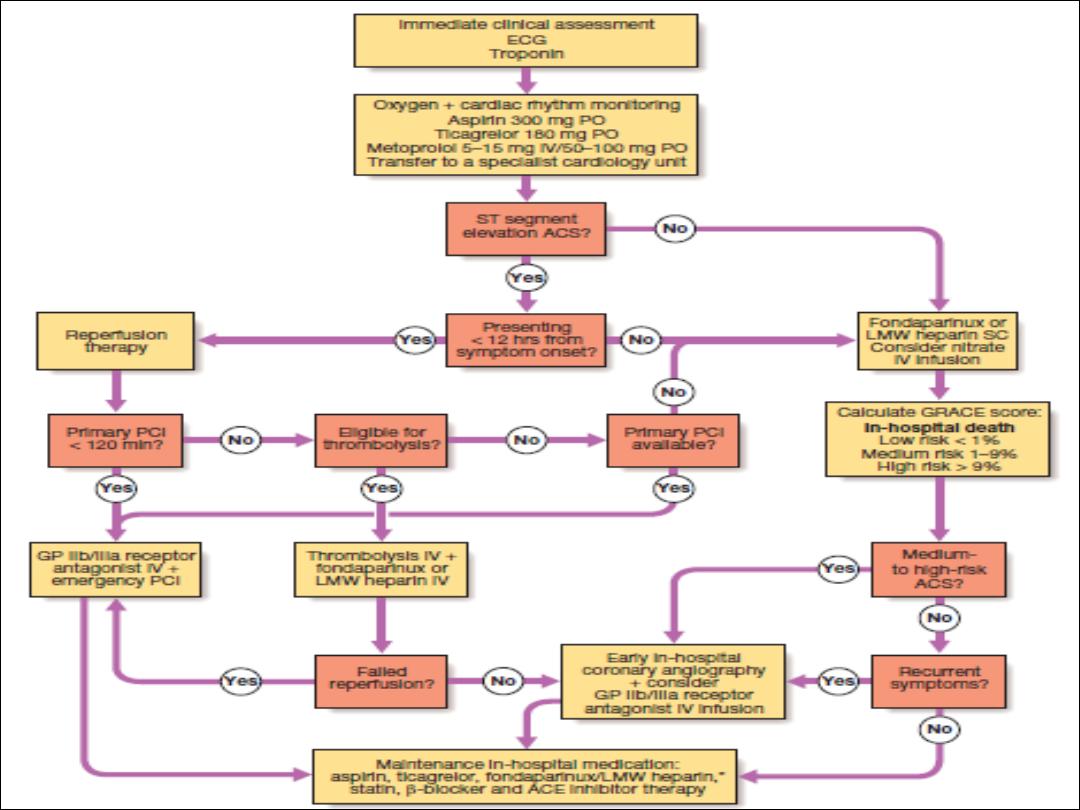
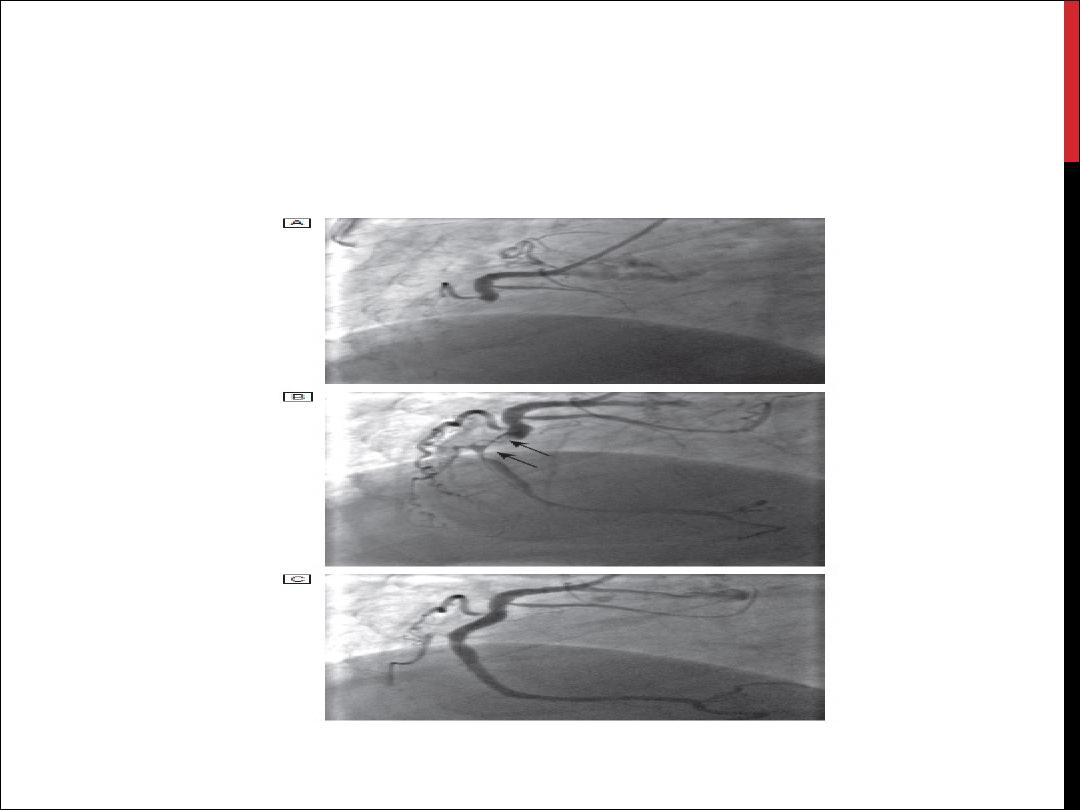
PRIMARY PCI
CONTRAINDICATIONS
Absolute
•
ICH
•
Structural cerebral vascular lesion
•
Ischaemic strok within 3 months
•
Malig. Intracranial neoplasm
•
Active bleeding and bleeding diathesis
•
Aortic dissection
•
Significant closed –head or facial trauma within 3 months
Relative
•
Poorly controlled HT. ( SBP ≥ 180)
•
Ischaemic strok ≥ 3 months
•
Dementia
•
Prolonged traumatic resuscitation ( ≥ 10 min)
•
Recent internal bleeding ( within 2-4 weeks)
•
Non compressible vascular puncture
•
Active peptic ulcer
•
Current use of anticoagulants
•
Pregnancy
•
Prior exposure ( for streptokinase)

COMPLICATIONS OF ACUTE
CORONARY SYNDROME
Arrhythmias
Ischaemia
Acute circulatory failure
Pericarditis
Mechanical complications
Embolism
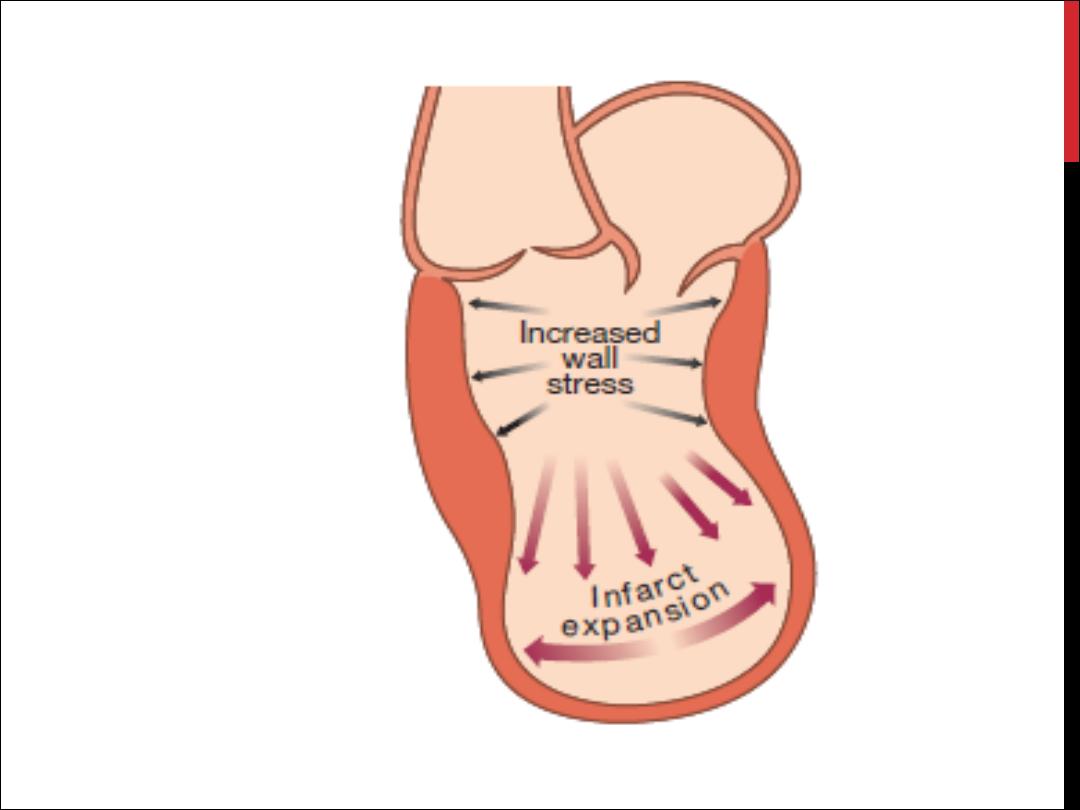
Impaired ventricular function, remodelling and ventricular aneurysm
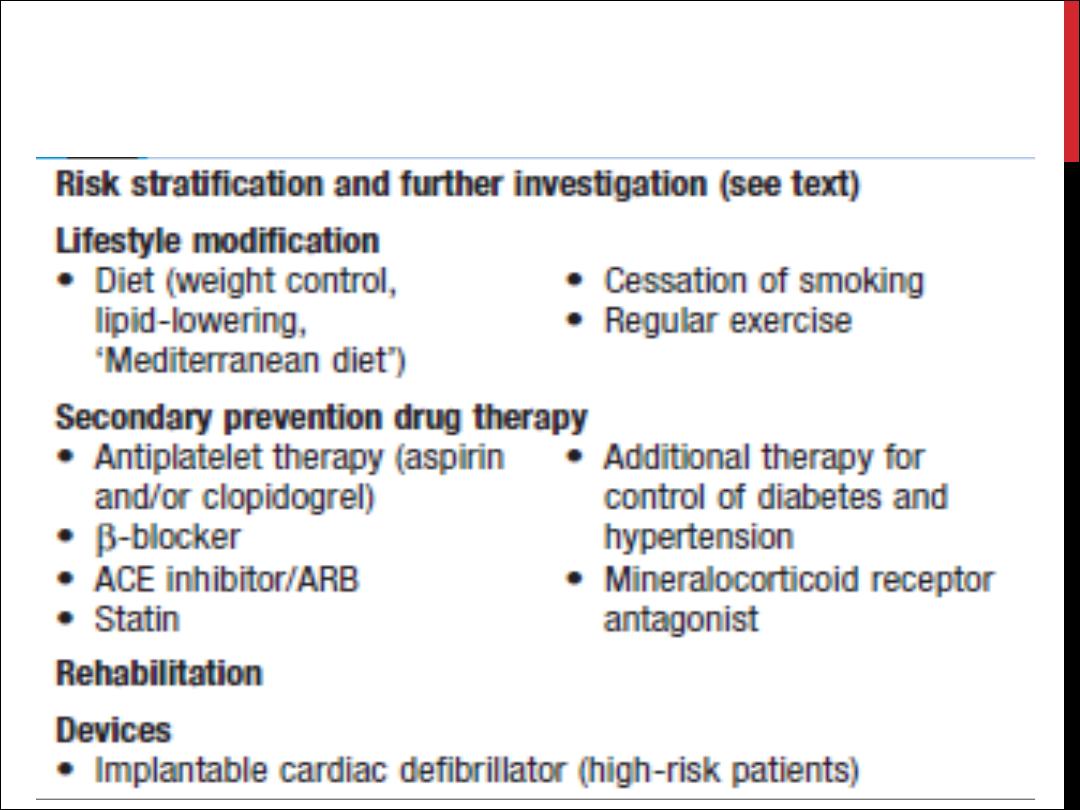
LATE MANAGEMENT OF ML
Valvular heart
diseases

Mitral Stenosis

AETIOLOGY
1- Congenital
2- acquired
Rheumatic
Degenerative

pathophysiology
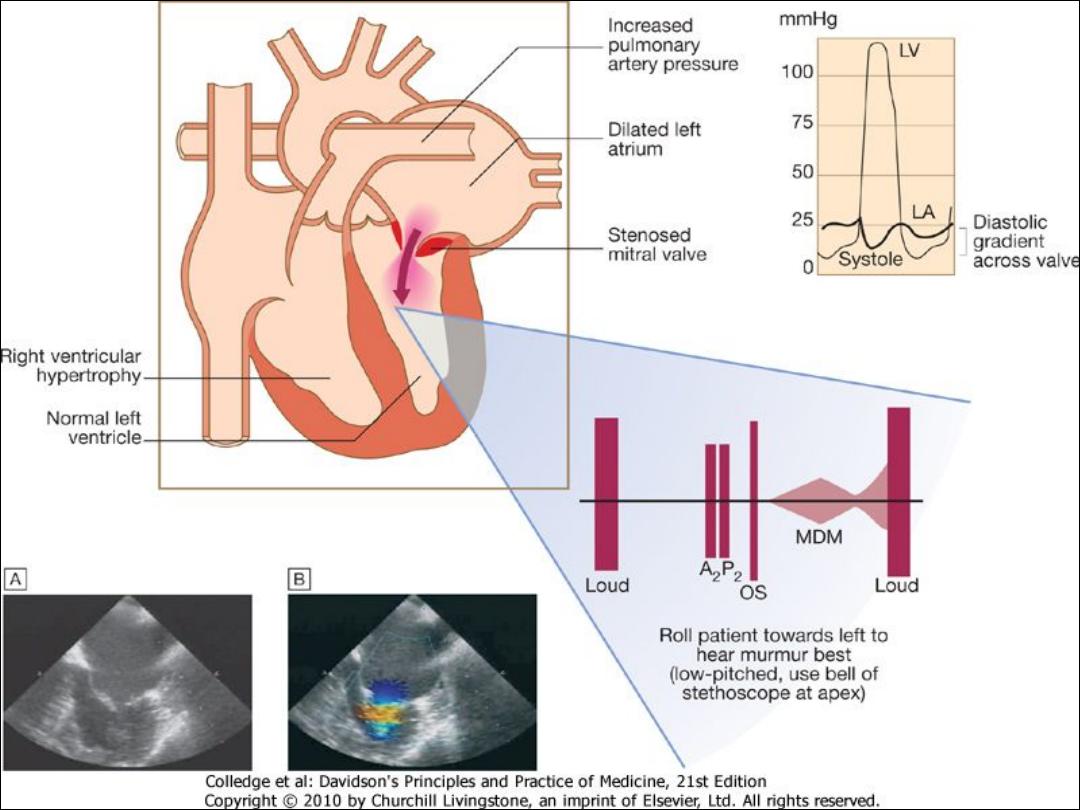
PATHOPHYSIOLOGY
DEFINITIONS OF SEVERITY OF
MITRAL STENOSIS
Valve Area:
•
<1.0 cm2 è Severe
•
1.0-1.5 cm2 è Moderate
•
>1.5-2.5 cm2 è Mild
Mean gradient:
•
>10 mmHg è Severe
•
5-10 mmHg è Moderate
•
<5 mmHg è Mild

CLINICAL FEATURES
Symptoms
Breathlessness (pulmonary congestion)
Fatigue (low cardiac output)
Oedema, ascites (right heart failure)
Palpitation (atrial fibrillation)
Haemoptysis (pulmonary congestion, pulmonary embolism)
Cough (pulmonary congestion)
Chest pain (pulmonary hypertension)
Thromboembolic complications (e.g. stroke, ischaemic limb)
Signs
Atrial fibrillation
Mitral facies
Auscultation
Loud first heart sound, opening snap
Mid-diastolic murmur
Crepitations, pulmonary oedema, effusions (raised PCWP)
RV heave, loud P2 (pulmonary hypertension)

Investigations

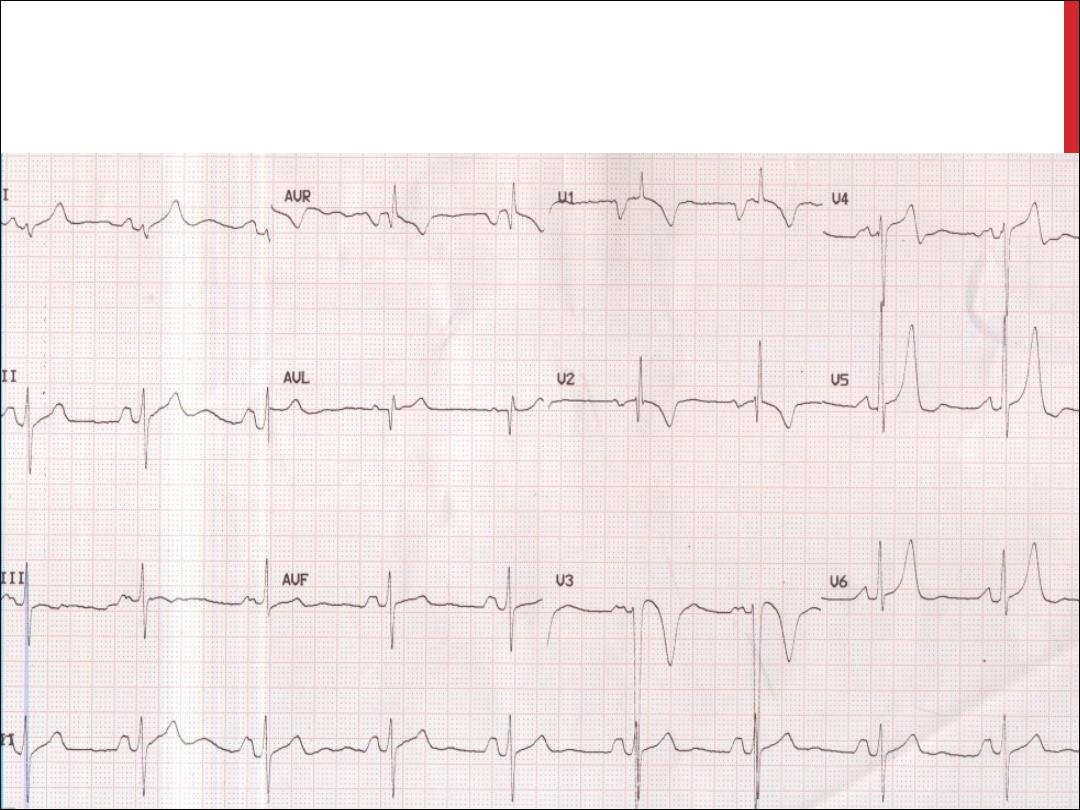
ECG
P mitrale or atrial fibrillation
Right ventricular hypertrophy: tall R waves in V1-V3
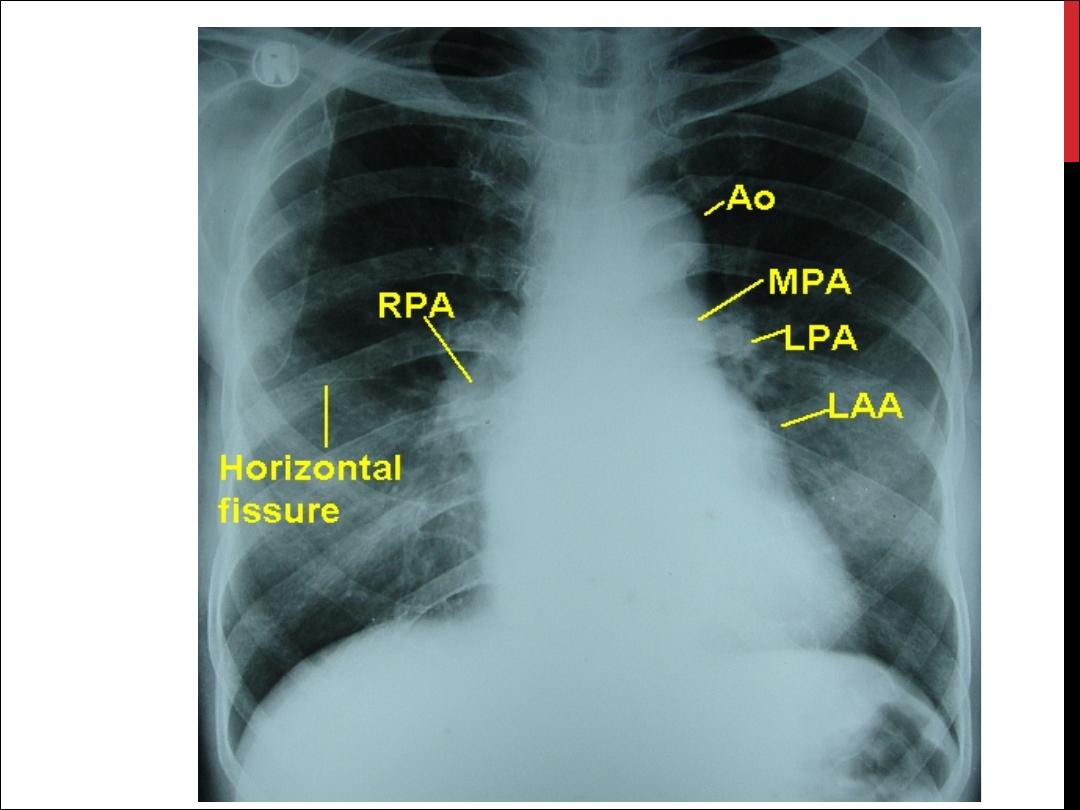
CXR
Enlarged LA and appendage
Signs of pulmonary venous congestion
Echo
Thickened immobile cusps
Reduced valve area
Reduced rate of diastolic filling of LV
Enlarged LA
Doppler
Pressure gradient across mitral valve
Pulmonary artery pressure
Left ventricular function
Cath
Coronary artery disease
Mitral stenosis and regurgitation
Pulmonary artery pressure

Echocardiogram in mitral
\
Desktop
\
SHOKRY
\
Users
\
C:
YouTube.flv
-
stenosis

MANAGEMENT
1- Medical management
Anticoagulation
Rate control
Diuretics
2- Mitral balloon valvuloplasty
Significant symptoms
Isolated mitral stenosis
No (or trivial) mitral regurgitation
Mobile, non-calcified valve ( Wilkins score )
LA free of thrombus
3- Valvotomy and Valve replacement

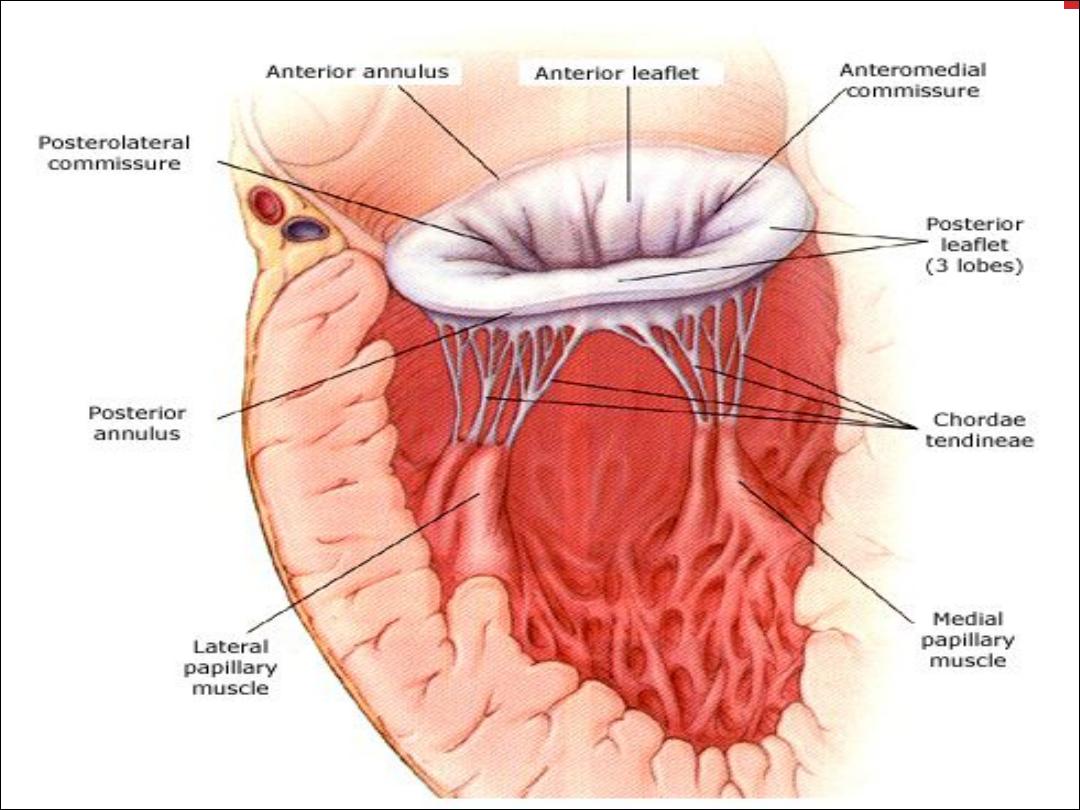
MITRAL REGURGITATION
Causes of mitral regurgitation
Mitral valve prolapse
Dilatation of the LV and mitral valve ring (e.g.
coronary artery disease,cardiomyopathy)
Damage to valve cusps and chordae (e.g. rheumatic heart
disease,endocarditis)
Ischaemia or infarction of the papillary muscle
MI

MITRAL VALVE
PROLAPSE
Congenital anomalies
Degenerative myxomatous changes
Marfan syndrom
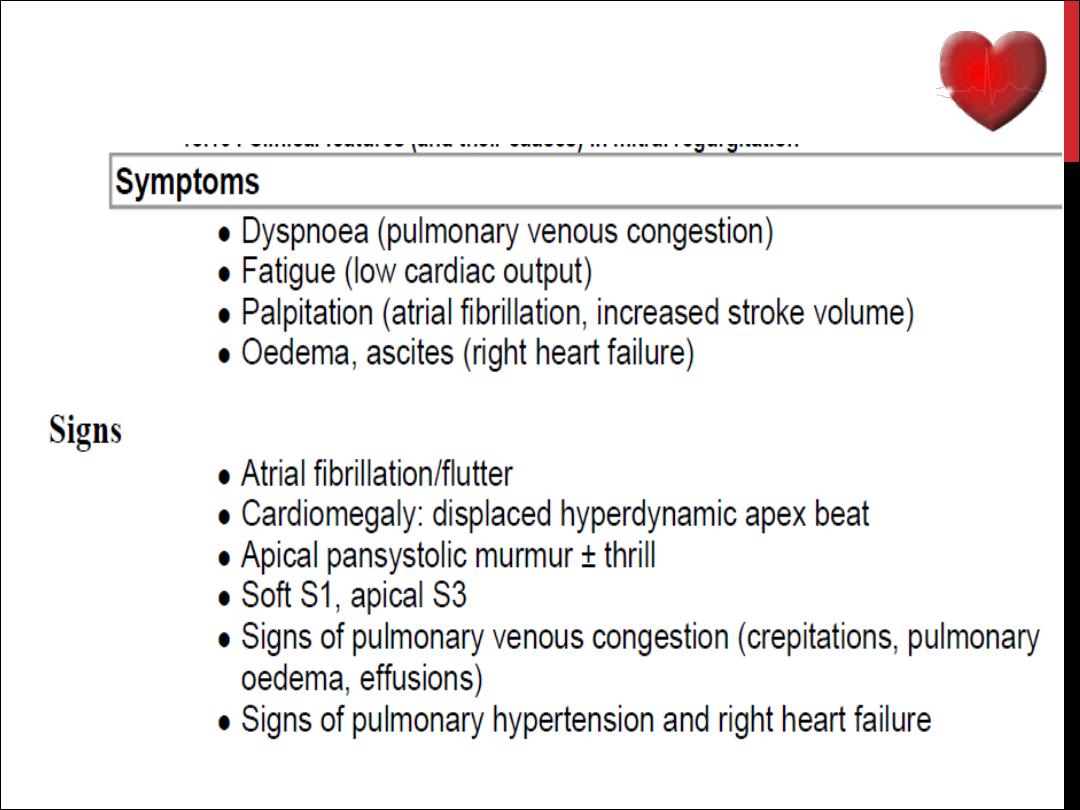
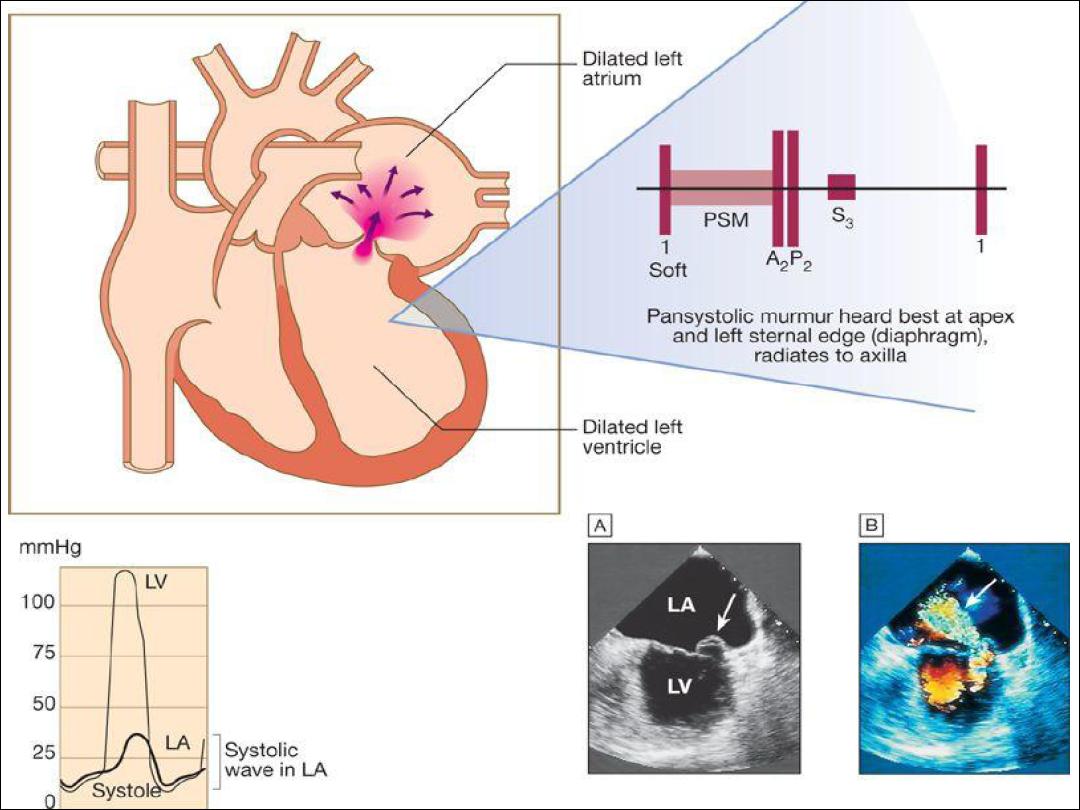
CLINICAL FEATURES
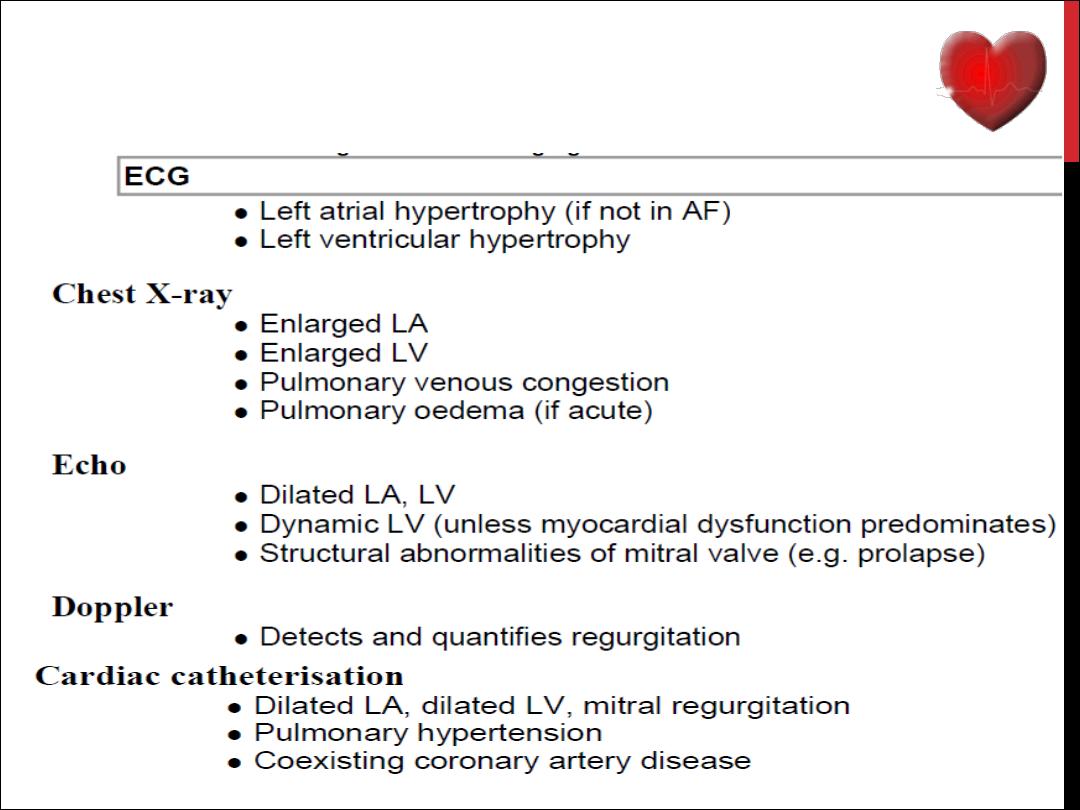
INVESTIGATIONS

MANAGEMENT
Medical management of MR
Diuretics
Vasodilators, e.g. ACE inhibitors
Digoxin if atrial fibrillation is present
Anticoagulants if atrial fibrillation is present
Surgical management
Repair
Replacement

AORTIC STENOSIS
Infants, children, adolescents
Congenital aortic stenosis
Congenital subvalvular aortic stenosis
Congenital supravalvular aortic stenosis
Young adults to middle-aged
Calcification and fibrosis of congenitally bicuspid aortic valve
Rheumatic aortic stenosis
Middle-aged to elderly
Senile degenerative aortic stenosis
Calcification of bicuspid valve
Rheumatic aortic stenosis

CLINICAL FEATURES
Symptoms
Mild or moderate stenosis: usually asymptomatic
Exertional dyspnoea
Angina
Exertional syncope
Sudden death
Episodes of acute pulmonary oedema
Signs
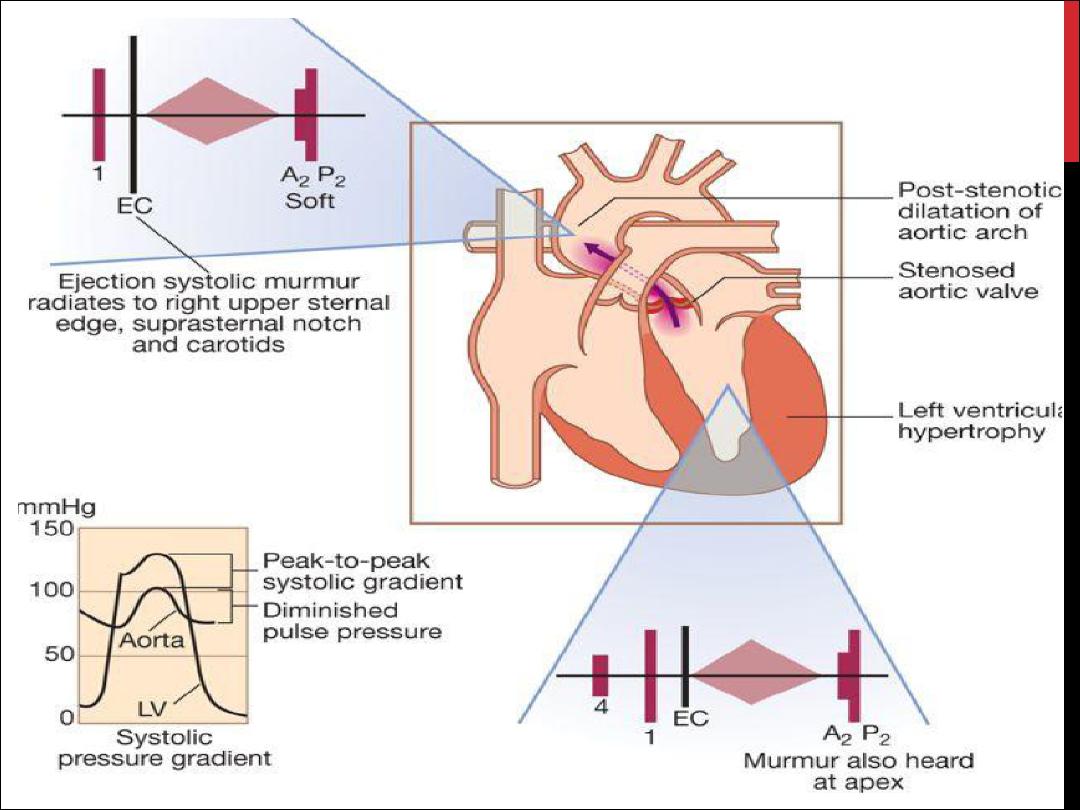
Ejection systolic murmur
Slow-rising carotid pulse
Narrow pulse pressure
Thrusting apex beat (LV pressure overload)
Signs of pulmonary venous congestion (e.g. crepitations)

INVESTIGATIONS IN AORTIC STENOSIS
ECG
Left ventricular hypertrophy (usually)
Left bundle branch block
Chest X-ray
May be normal; sometimes enlarged LV and dilated ascending aorta on PA view,
calcified valve on lateral view
Echo
Calcified valve with restricted opening, hypertrophied Left ventricle
Doppler
Measurement of severity of stenosis
Detection of associated aortic regurgitation
Cardiac catheterisation
Mainly to identify associated coronary artery disease
May be used to measure gradient between LV and aorta

MANAGEMENT
Conservative
AVR
Balloon dilatation
TAVI

AORTIC REGURGITATION
Congenital
Bicuspid valve or disproportionate cusps
Acquired
Rheumatic disease
Infective endocarditis
Trauma
Aortic dilatation (Marfan's syndrome, aneurysm, dissection,
syphilis,ankylosing spondylitis)
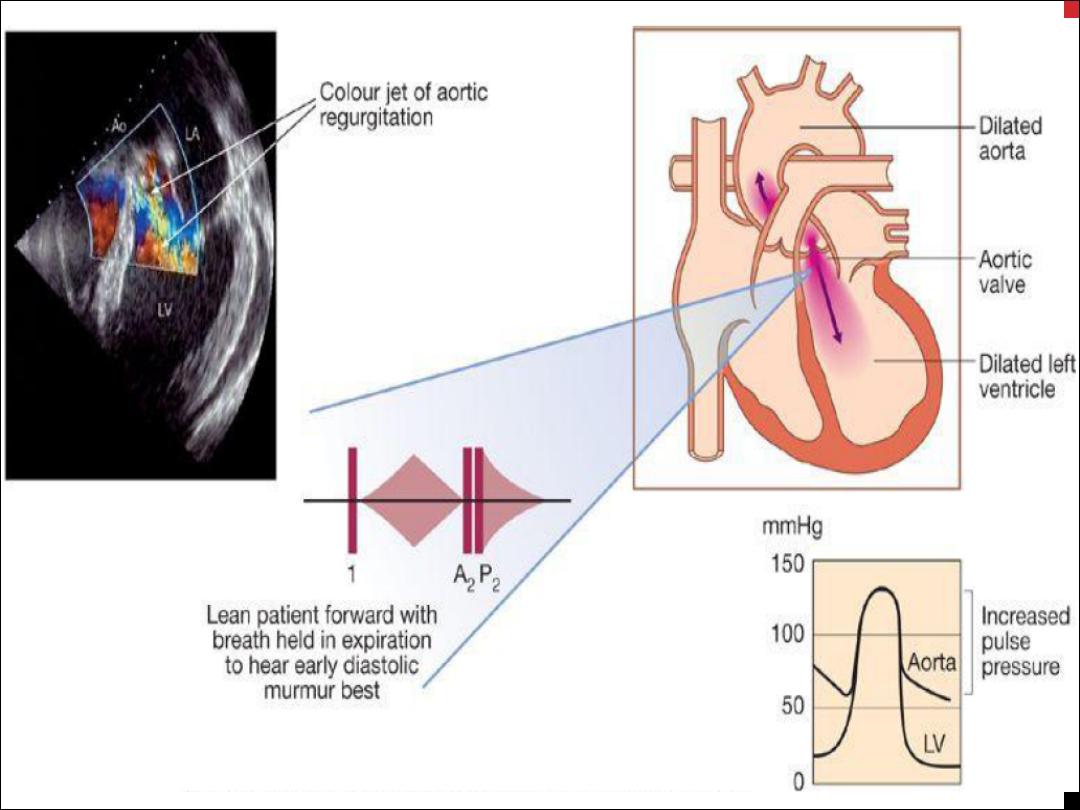

CLINICAL FEATURES
Mild to moderate AR
Often asymptomatic
Awareness of heart beat, 'palpitations'
Severe AR
Breathlessness
Angina
Signs Pulses
Large-volume or 'collapsing' pulse
Low diastolic and increased pulse pressure
Bounding peripheral pulses
Capillary pulsation in nail beds: Quincke's sign
Femoral bruit ('pistol shot'): Duroziez's sign
Head nodding with pulse: de Musset's sign
Murmurs
Early diastolic murmur
Systolic murmur (increased stroke volume)
Austin Flint murmur (soft mid-diastolic)
Other signs

INVESTIGATIONS
ECG
Initially normal, later left ventricular hypertrophy and T-wave inversion
Chest X-ray
Cardiac dilatation, maybe aortic dilatation
Features of left heart failure
Echo
Dilated LV
Hyperdynamic LV
Fluttering anterior mitral leaflet
Doppler detects reflux
Cardiac catheterisation (may not be required)
Dilated LV
Aortic regurgitation
Dilated aortic root

MANAGEMENT
underlying conditions
Systolic BP should be controlled with vasodilating
drugs such as nifedipine or ACE inhibitors
Surgery

INFECTIVE ENDOCARDITIS
This is due to microbial infection of a heart
valve (native or prosthetic), the lining of a
cardiac chamber or blood vessel, or a
congenital anomaly
PATHOPHYSIOLOGY
occurs at sites of pre-existing endocardial damage
Many acquired and congenital cardiac lesions are
vulnerable to endocarditis
Infection tends to occur at sites of endothelial damage
vegetations composed of organisms, fibrin and platelets
grow and may become large enough to cause obstruction
or embolism
Valve regurgitation may develop or increase
Extracardiac manifestations such as vasculitis and skin
lesions are due to emboli or immune complex deposition
Mycotic aneurysms may develop in arteries at the site of
infected emboli

MICROBIOLOGY
Over three-quarters of cases are due to streptococci or
staphylococci (viridans group )
Other organisms Enterococcus faecalis, E. faecium and
Strep. Bovis
Staph. aureus has now overtaken streptococci
Post-operative endocarditis: coagulase-negative
staphylococcus (Staph. epidermidis , Staph. Lugdenensis )
Q fever endocarditis due to Coxiella burnetii
HACEK group and Brucella
Yeasts and fungi (Candida, Aspergillus)

INCIDENCE
5 to 15 cases per 100 000 per annum
rheumatic heart disease in 24%
congenital heart disease in 19%
other cardiac abnormality (e.g. calcified aortic
valve, floppy mitral valve) in 25%.
32% not have a pre-existing cardiac
abnormality

CLINICAL FEATURES
Subacute endocarditis
Acute endocarditis
Post-operative endocarditis

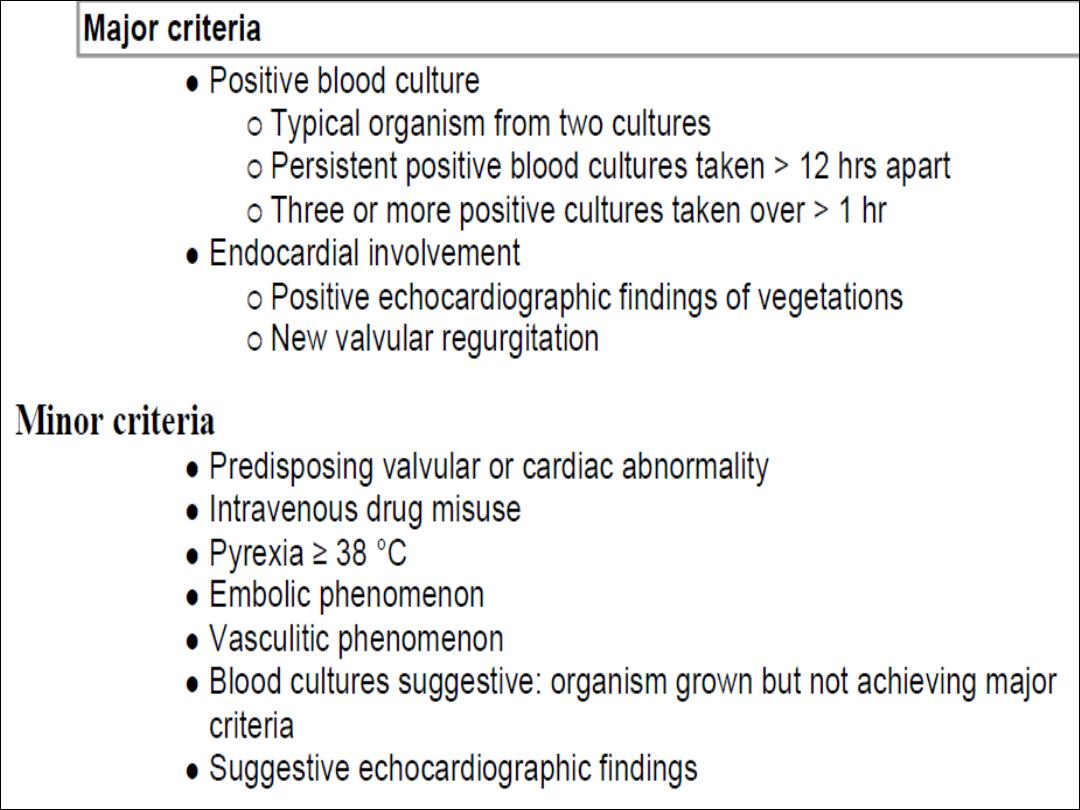
INVESTIGATIONS
Blood culture
Echocardiography
ESR, anaemia, and leucocytosis
CRP ; Proteinurea ; microscopic haematuria
ECG
CXR
MANAGEMENT
The case fatality 20%
A multidisciplinary approach
Empirical treatment
A 2-week treatment regimen may be sufficient for fully
sensitive strains of Strep. viridans and Strep. Bovis
Cardiac surgery
Heart failure due to valve damage
Failure of antibiotic therapy
Large vegetations on left-sided heart valves
Abscess formation
