Infective endocarditis

Pathophysiology
•
typically occurs at sites of preexisting endocardial damage
•
virulent or aggressive organisms (e.g.
Staphylococcus aureus
) can cause
endocarditis in a previously normal heart
•
Many acquired and congenital cardiac lesions are vulnerable to endocarditis,
particularly areas of endocardial damage caused by a high-pressure jet of blood
•
•
The avascular valve tissue and presence of fibrin and platelet aggregates help to
protect proliferating organisms from host defence mechanisms
•
vegetations composed of organisms, fibrin and platelets grow and may become
large enough to cause obstruction or embolism
•
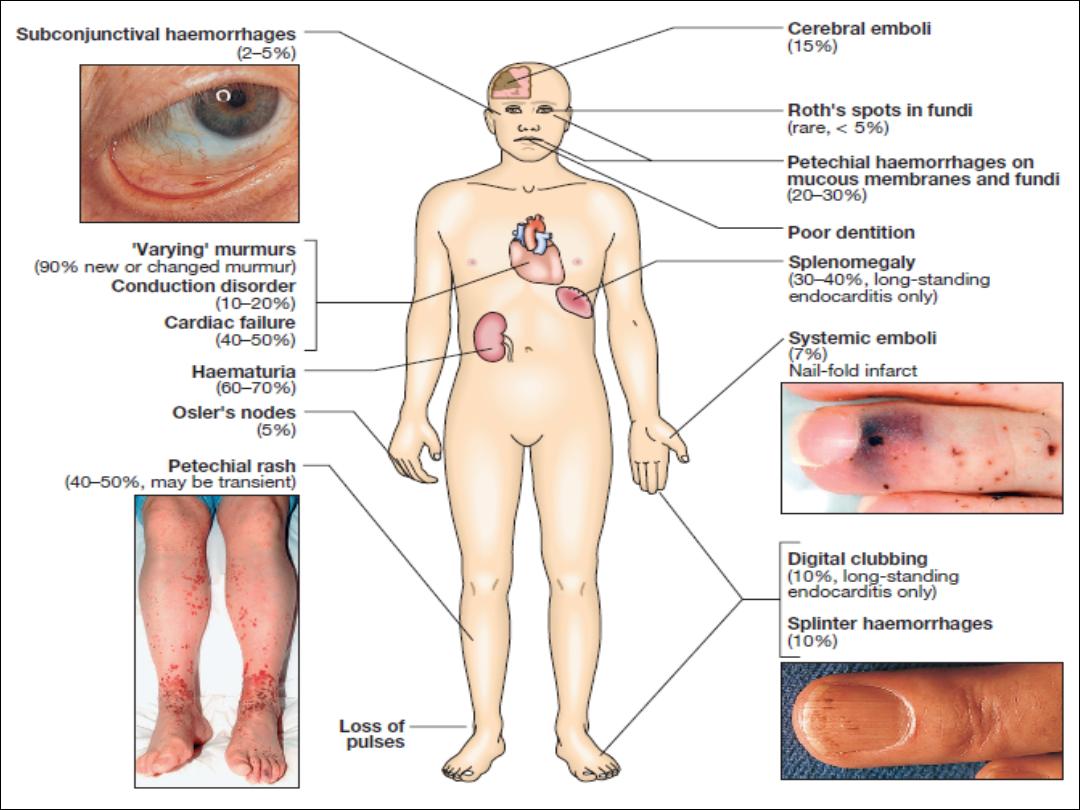
Extracardiac manifestations, such as vasculitis and skin lesions, are due to emboli
or immune complex deposition
Microbiology
• Over three-quarters of cases are caused by streptococci or staphylococci
•
Strep. milleri
and
Strep. bovis
endocarditis is associated with large-bowel
neoplasms.
•
Staph. aureus
has now overtaken streptococci as the most common
cause of acute endocarditis
• Post-operative endocarditis .The most common organism is a coagulase-
negative staphylococcus (
Staph. epidermidis
)
• Q fever endocarditis due to
Coxiella burnetii
, : contact with farm animals.
The aortic valve is usually affected and there may also be hepatitis,
pneumonia and purpura. Life-long antibiotic therapy may be required.
• HACEK are slow-growing, fastidious organisms that are only revealed
after prolonged culture and may be resistant to penicillin.
•
Brucella
• Yeasts and fungi (
Candida, Aspergillus
)
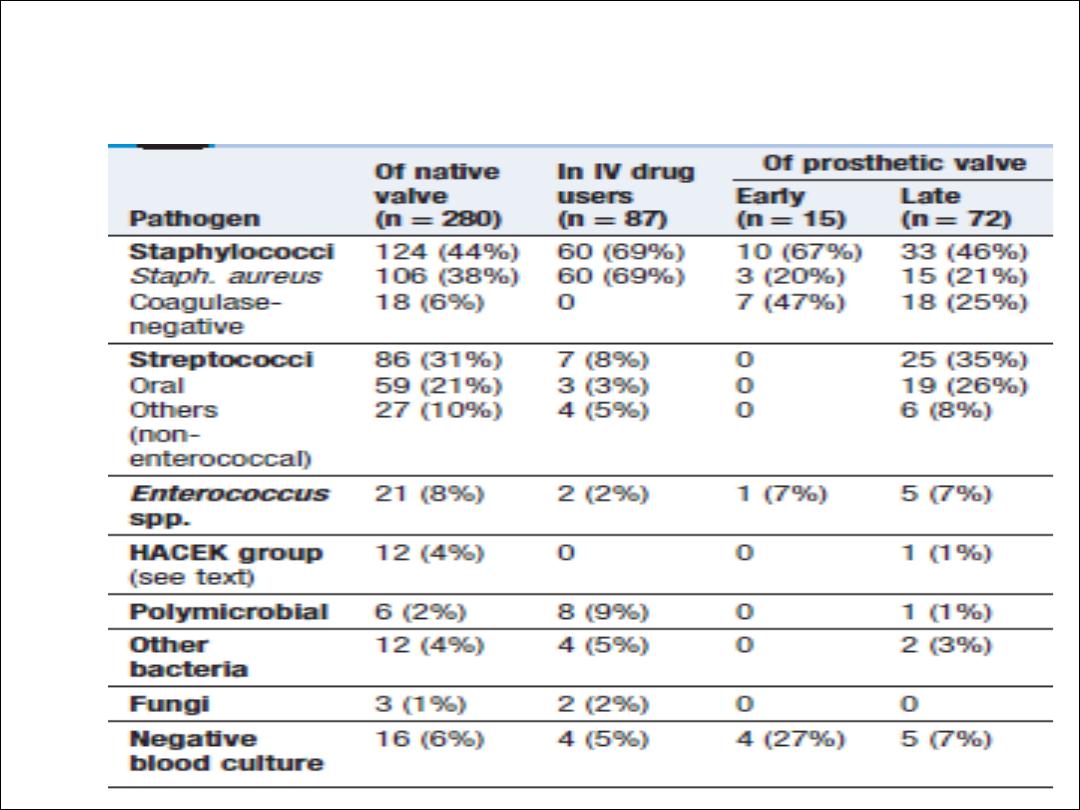
Microbiology of infective endocarditis
Incidence
• 5 to 15 cases per 100 000 per annum
• 50% of patients are over 60 years
• rheumatic heart disease in 24%
• congenital heart disease in 19%
• other cardiac abnormalities (calcified aortic valve, floppy mitral valve) in
25%
• 32% were not thought to have a pre-existing cardiac abnormality
Clinical features
•
Subacute endocarditis
•
Acute endocarditis
•
Post-operative endocarditis
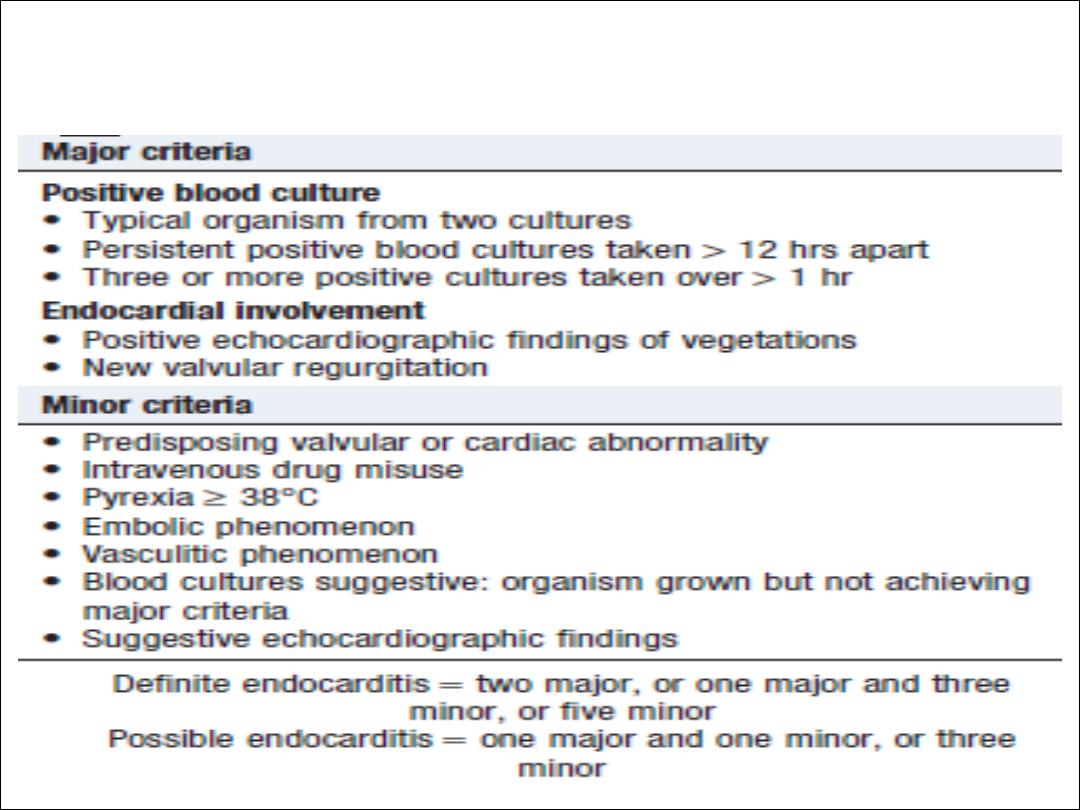
modified Duke criteria

Investigations
• Blood culture
• Echocardiography
• ESR , CRP , CBC
• ECG
• CXR

Management
• The case fatality of bacterial endocarditis is approximately 20 %
• A multidisciplinary approach increases the chance of better outcome
• Empirical treatment depends on the mode of presentation, the
suspected organism, and whether the patient has a prosthetic valve or
penicillin allergy
• If the presentation is acute, flucloxacillin and gentamicin are
recommended, while for a subacute or indolent presentation, benzyl
penicillin and gentamicin are preferred
• In those with penicillin allergy, a prosthetic valve or suspected meticillin-
resistant Staph. aureus (MRSA) infection, triple therapy with
vancomycin, gentamicin and oral rifampicin should be considered
• A 2-week treatment regimen may be sufficient for fully sensitive strains
of Strep. viridans and Strep. bovis, provided specific conditions are met

Conditions for the short-course treatment
of
Strep. viridans/bovis
endocarditis
Ø
• Native valve infection
Ø
• MIC ≤ 0.1 mg/L
Ø
• No adverse prognostic factors (e.g. heart failure,
aortic regurgitation, conduction defect)
Ø
• No evidence of thromboembolic disease
Ø
• No vegetations > 5 mm diameter
Ø
• Clinical response within 7 days
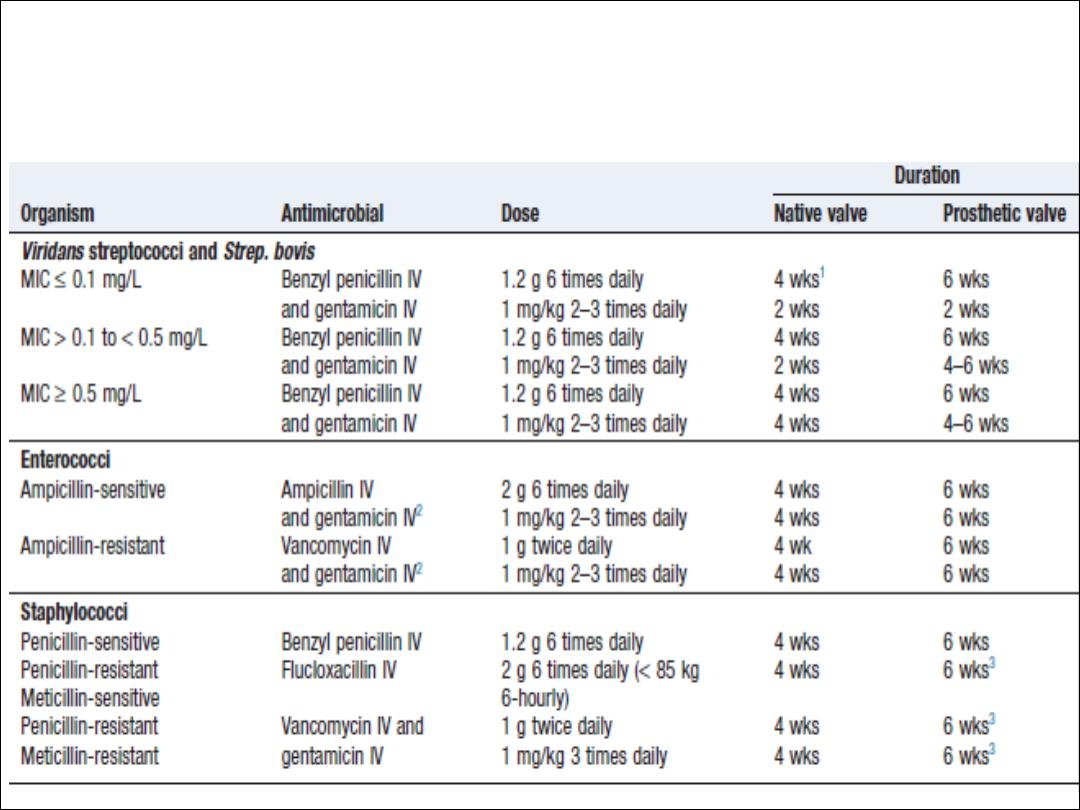
Antimicrobial treatment of common causative
organisms in infective endocarditis

Indications for cardiac surgery in
infective endocarditis
Ø
• Heart failure due to valve damage
Ø
• Failure of antibiotic therapy (persistent/uncontrolled
infection)
Ø
• Large vegetations on left-sided heart valves with
evidence or‘high risk’ of systemic emboli
Ø
• Abscess formation
N.B. Patients with prosthetic valve endocarditis or fungal endocarditis often require
cardiac surgery.
CONGENITAL HEART DISEASE
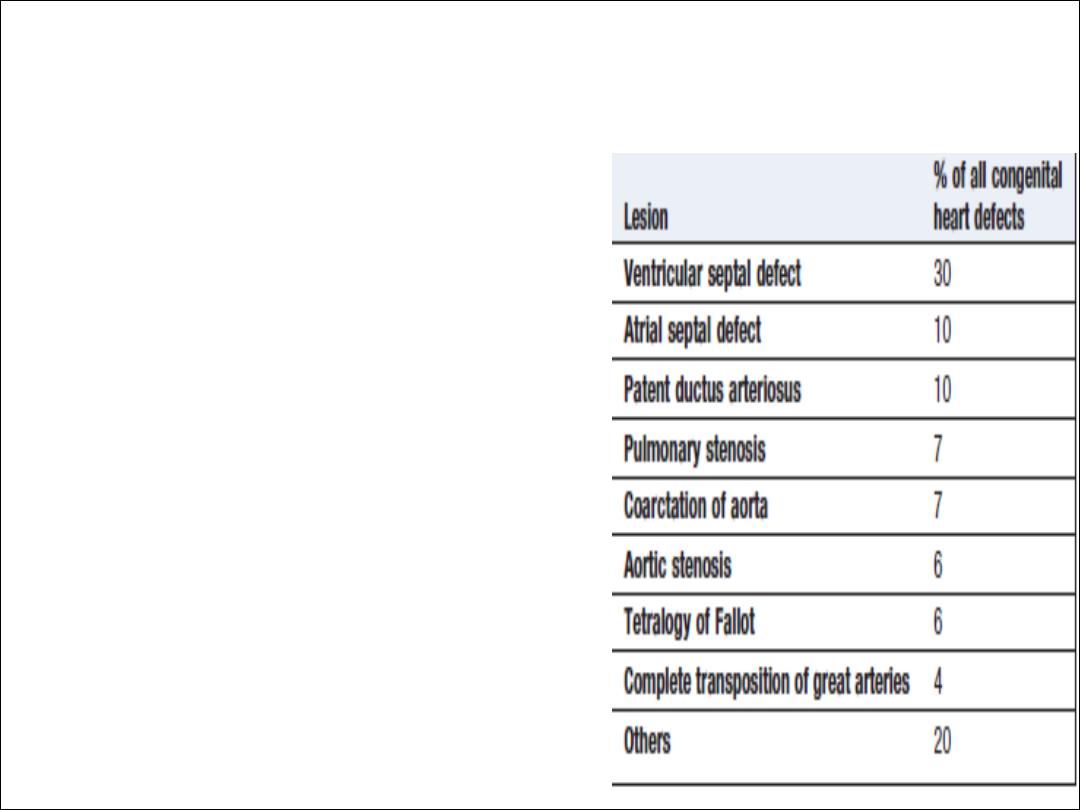
Aetiology and incidence
• 0.8% of live births
• Maternal infection or exposure to
drugs or toxins may cause congenital
heart disease.
Rubella , alcohol , SLE
• Genetic or chromosomal
abnormalities, such as Down’s
syndrome , Marfan syndrom and
Digeorge syndrom
Clinical features
• Clinical signs vary with the anatomical lesion
• Symptoms may be absent, or the child may be breathless
or fail to attain normal growth and development
• Some defects are not compatible with extrauterine life
• Features of other congenital conditions, such as Marfan’s
syndrome or Down’s syndrome, may also be apparent
• Early diagnosis is important because many types of
congenital heart disease are amenable to surgery

•
Central cyanosis and digital clubbing
•
Growth retardation and learning difficulties
•
Syncope
•
Pulmonary hypertension and Eisenmenger’s
syndrome
Pregnancy
• Obstructive lesions (e.g. severe aortic stenosis): poorly
tolerated and associated with significant maternal morbidity and
mortality.
• Cyanotic conditions (e.g. Eisenmenger’s syndrome):
especially poorly tolerated and pregnancy should be avoided.
• Surgically corrected disease: patients often tolerate
pregnancy well.
• Children of patients with congenital heart disease: 2–5%
will be born with cardiac abnormalities, especially if the mother is
affected.
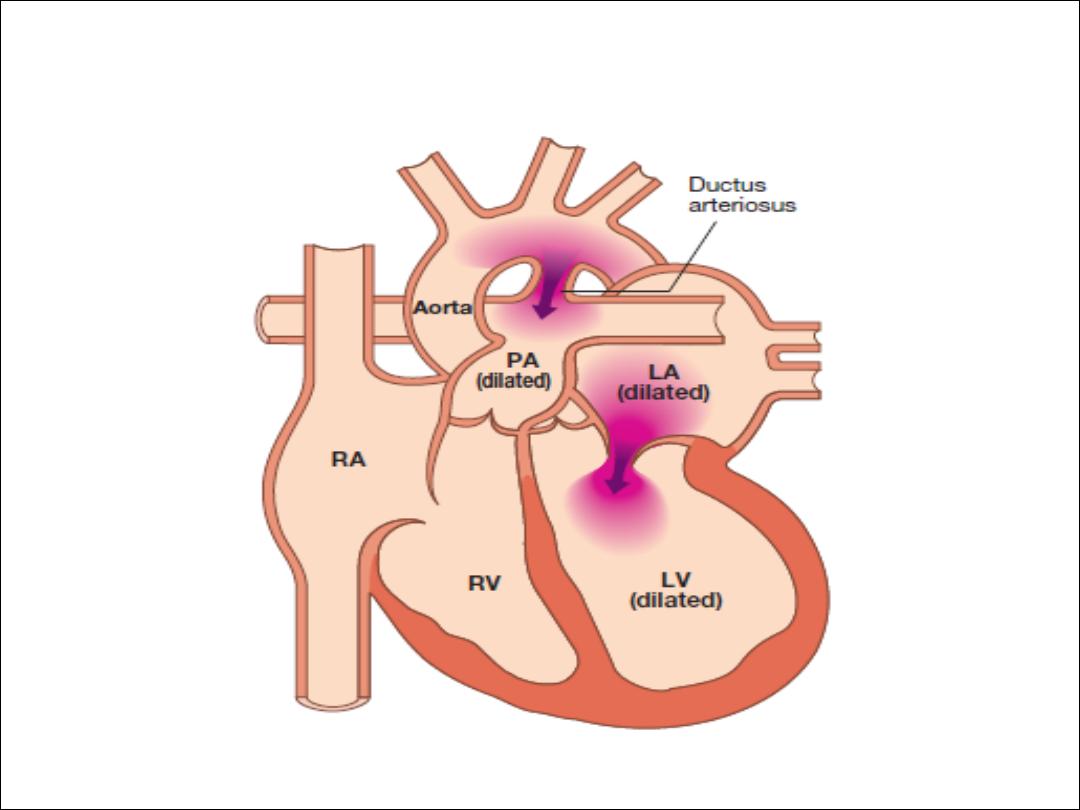
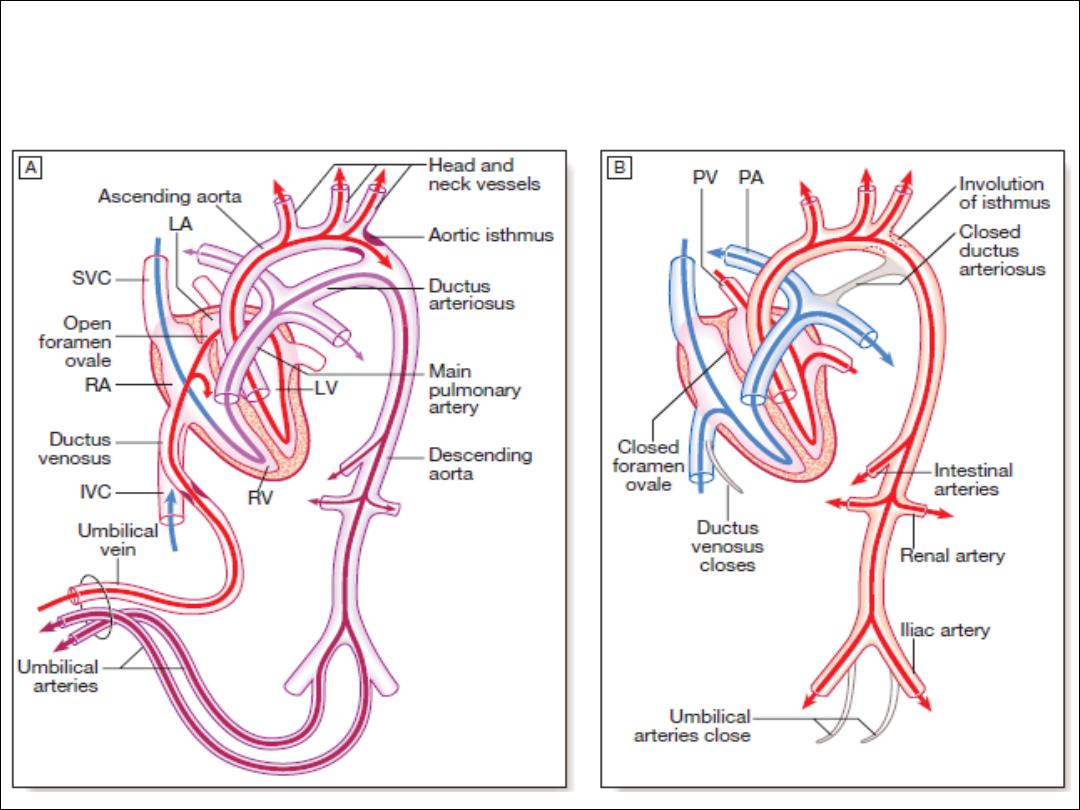
Persistent ductus arteriosus

Aetiology
• Normally, the ductus closes soon after birth but sometimes
fails to do so
• Persistence of the ductus is associated with other
abnormalities and is more common in females.
• there will be a continuous arteriovenous shunt
• 50% of the left ventricular output is recirculated through the
lungs

Clinical features
• small shunts there may be no symptoms for years
• when the ductus is large, growth and development may be
retarded
• cardiac failure may eventually ensue, dyspnoea being the first
symptom
• continuous ‘machinery’ murmur is heard
•
Persistent ductus with reversed shunting

Management
• A patent ductus is closed at cardiac catheterisation
with an implantable occlusive device
•
Pharmacological treatment in the neonatal period
(
prostaglandin synthetase inhibitor (indometacin or
ibuprofen)
Coarctation of the aorta
Aetiology
• occurs in the region where the ductus arteriosus joins the aorta, i.e. at
the isthmus just below the origin of the left subclavian artery
• twice as common in males and occurs in 1 in 4000 children
• associated with other abnormalities, most frequently bicuspid aortic valve
and ‘berry’ aneurysms of the cerebral circulation
• Acquired coarctation of the aorta is rare but may follow trauma or occur
as a complication of a progressive arteritis (Takayasu’s disease)

Clinical features and investigations
• coarctation is an important cause of cardiac failure in the newborn
• symptoms are often absent when it is detected in older children or adults
• Headaches , weakness or cramps in the legs , BP is raised in the upper
body
• Radiofemoral delay , systolic murmur may be be heard posteriorly or in the
aortic area with ejection click due to bicuspid AV
• CXR …… 3 sign and rib notching
• ECG ….LVH
• Echo. …..Confirm the diagnosis
• MRI is the best imaging modality

Management
• In untreated cases, death may occur from left ventricular failure,
dissection of the aorta or cerebral haemorrhage.
• Surgical correction is advisable in most cases
• Patients repaired in late childhood or adult life often remain
hypertensive or develop recurrent hypertension later on
• Recurrence of stenosis may occur as the child grows and this
may be managed by balloon dilatation and sometimes stenting
• Coexistent bicuspid aortic valve, which occurs in over 50% of
cases, may lead to progressive aortic stenosis or regurgitation,
and also requires long-term follow-up.

Atrial septal defect
• one of the most common congenital heart defects
• twice as frequently in females
• Most are ‘ostium secundum’ defects
• Ostium primum’ defects result from a defect in the
atrioventricular septum and are associated with a ‘cleft mitral
valve’ (split anterior leaflet).
• Pulmonary hypertension and shunt reversal sometimes
complicate atrial septal defect, but are less common and tend
to occur later in life
Clinical features and investigations
Symptoms
• Asymptomatic
• Dyspnea
• Chest infection
• HF
• Arrythmias , AF
Signs
• Wide fixed splitting S2
• Systolic flow murmur
• Diastolic flow murmur
Investigations
• ECG :- RBBB , RAD and in case of primum defect
LAD
• CXR : cardiomegaly ; pul plethora , prominent PA
• Echo :- shows the defect , RV and PA dilatation
• TEE
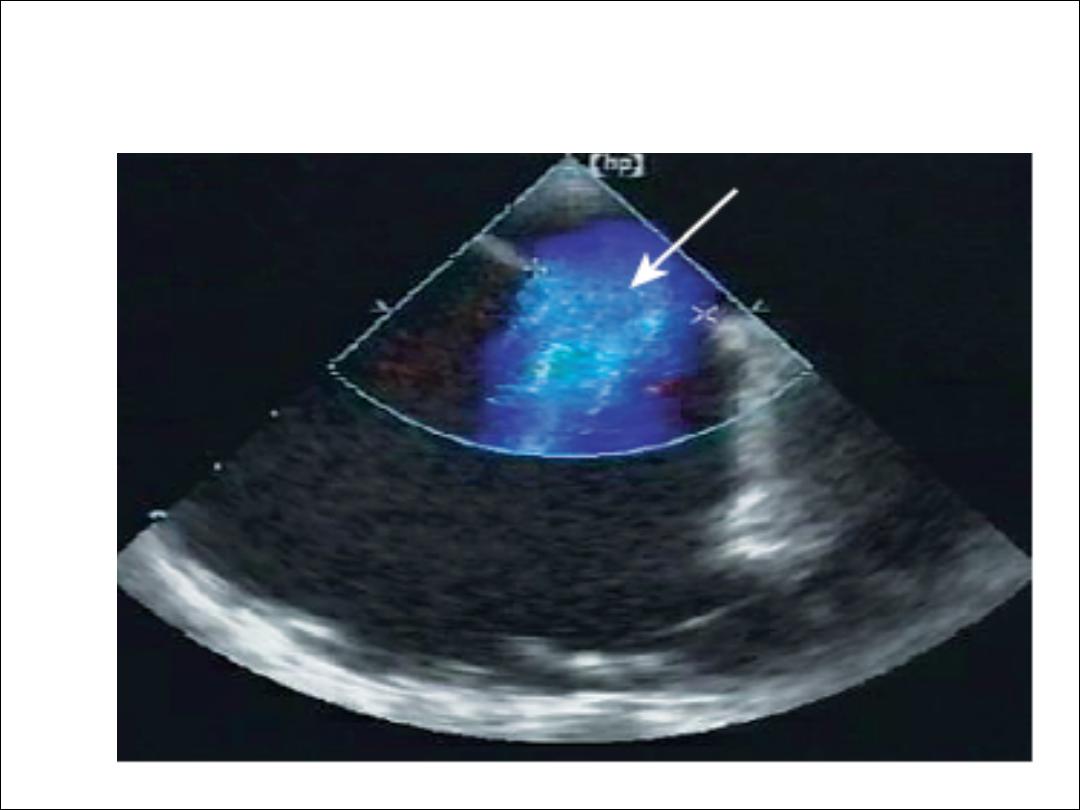
TEE

Management
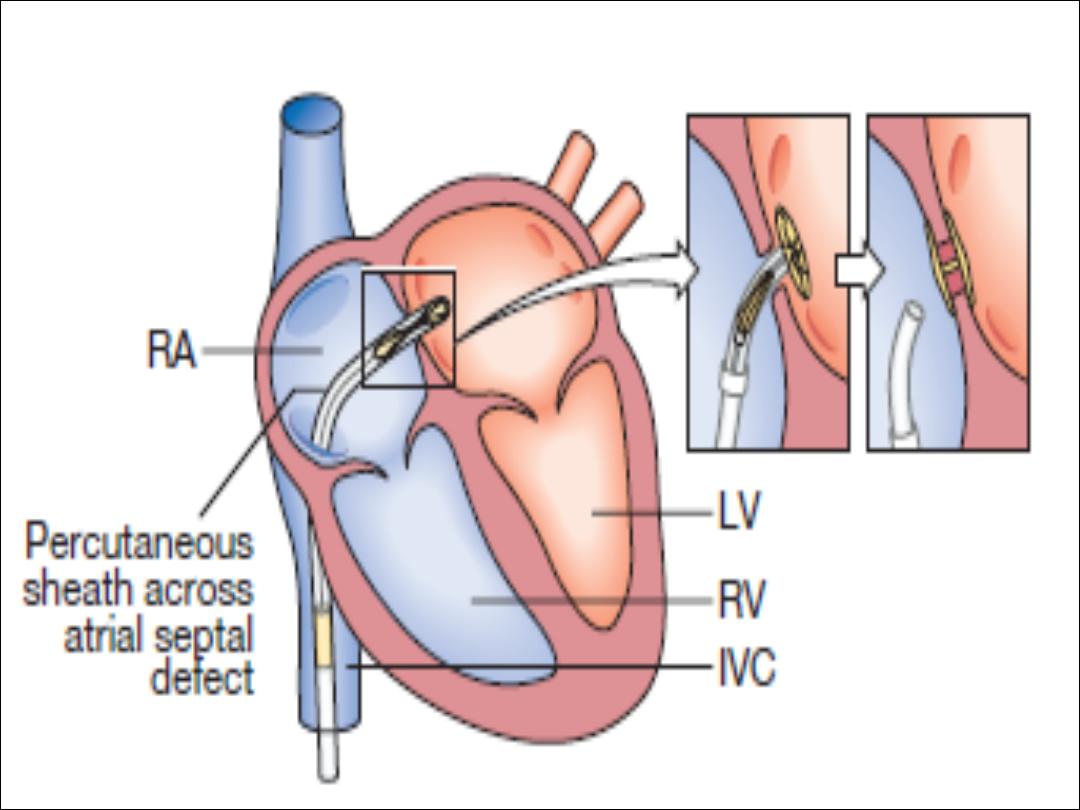
• Atrial septal defects in which pulmonary flow is
increased 50% above systemic flow (i.e. flow ratio of
1.5 : 1) are often large enough to be clinically
recognisable and should be closed
• Cath or surgery
• Severe pulmonary hypertension and shunt reversal
are both contraindications to closure
Ventricular septal defect
Aetiology
• Congenital and acquired
• Embryologically, the interventricular septum has a
membranous and a muscular portion
• Most congenital defects are ‘perimembranous
• the most common congenital cardiac defect, occurring once
in 500 live births.
• Acquired ventricular septal defect may result from rupture as
a complication of acute MI or, rarely, from trauma.

Clinical features
• pansystolic murmur, usually heard best at the left sternal edge but
radiating all over the precordium
• maladie de Roger :- small defect producing loud murmur in the absence
of other haemodynamic disturbance
• Congenital ventricular septal defect may present as cardiac failure in
infants, as a murmur with only minor haemodynamic disturbance in older
children or adults, or, rarely, as Eisenmenger’s syndrome
• If cardiac failure complicates a large defect, it only becomes apparent in
the first 4–6 weeks of life
• The chest X-ray shows pulmonary plethora and the ECG shows bilateral
ventricular hypertrophy.
• Echo .

Management and prognosis
• Small ventricular septal defects require no specific
treatment
• HF : digoxin and diuretics
• Persisting failure is an indication for closure of the defect by
cath. or surgery
• Except in Eisenmenger’s syndrome, long-term prognosis is
very good in congenital ventricular septal defect
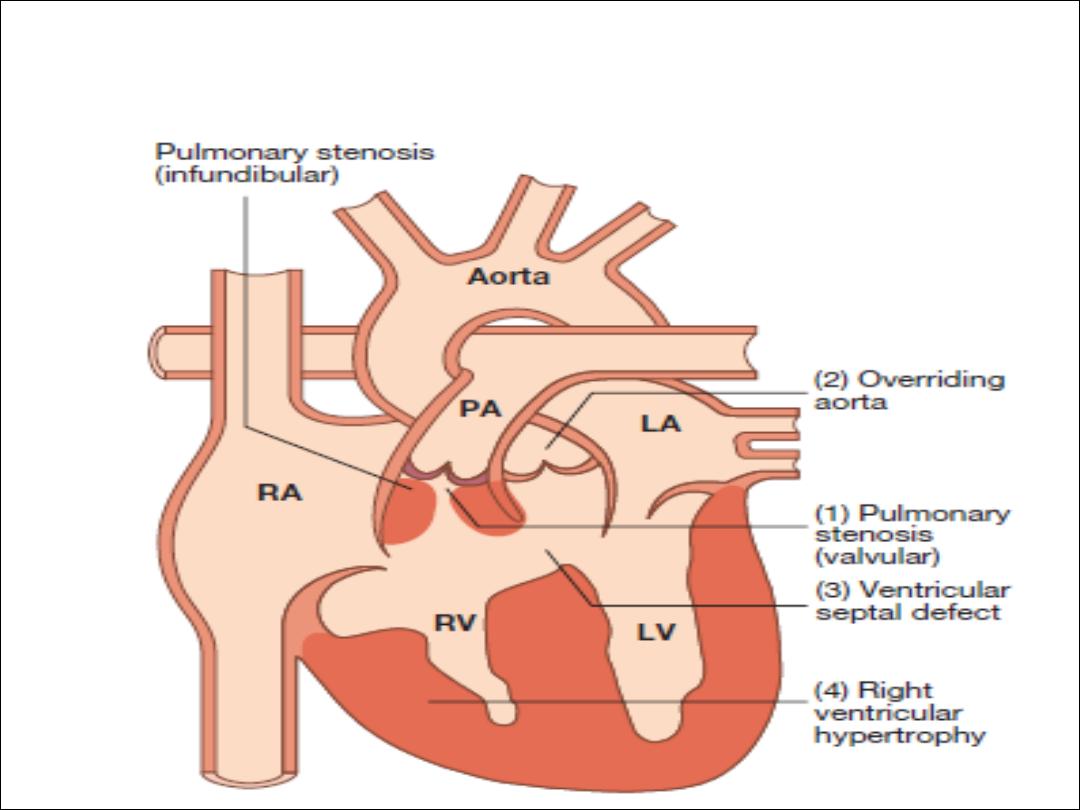
Tetralogy of Fallot

Aetiology
• The embryological cause is abnormal development of
the bulbar septum that separates the ascending aorta
from the pulmonary artery
• The defect occurs in about 1 in 2000 births and is the
most common cause of cyanosis in infancy after the
first year of life.

Clinical features
• Children are usually cyanosed but this may not be the case in the neonate
• The subvalvular component of the RV outflow obstruction is dynamic and
may increase suddenly under adrenergic stimulation
• Fallot’s spells
• In older children, Fallot’s spells are uncommon but cyanosis becomes
increasingly apparent, with stunting of growth, digital clubbing and
polycythaemia
• Fallot’s sign : Some children characteristically obtain relief by squatting after
exertion
• On examination, cyanosis with a loud ejection systolic murmur in the
pulmonary area
• cyanosis may be absent in the newborn or in patients with only mild right
ventricular outflow obstruction (‘acyanotic tetralogy of Fallot’)

Investigations and management
• ECG … RVH
• CXR … boot shaped heart
• Echo … Dx
• The definitive management is total surgical correction
• If the pulmonary arteries are too hypoplastic, then palliation in
the form of a Blalock–Taussig shunt
• The prognosis after total correction is good
• ICD is sometimes recommended in adulthood.
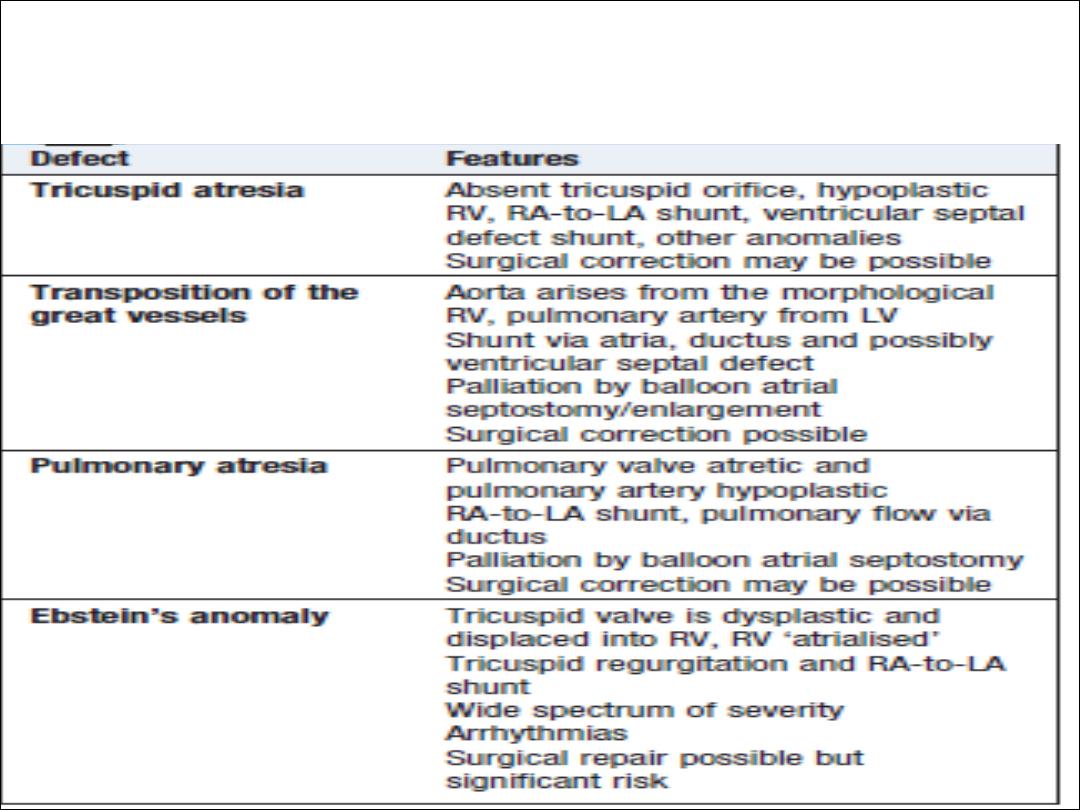
Other causes of cyanotic
congenital heart disease