Pneumonia
Definition :
An acute infection of the pulmonary parenchyma that is
associated with at least some symptoms of acute infection, accompanied
by an acute new infiltrate on CXR or auscultatory findings consistent
with pneumonia
Classification
:
1- Etiological :
A- Infection:
I-
Bacterial: pneumococci , hemophilis ,or other G+ve
bacteria & atypical legionella, chlamydia ,mycoplasma
II-
Viral
III-
Fungal
IV-
Other
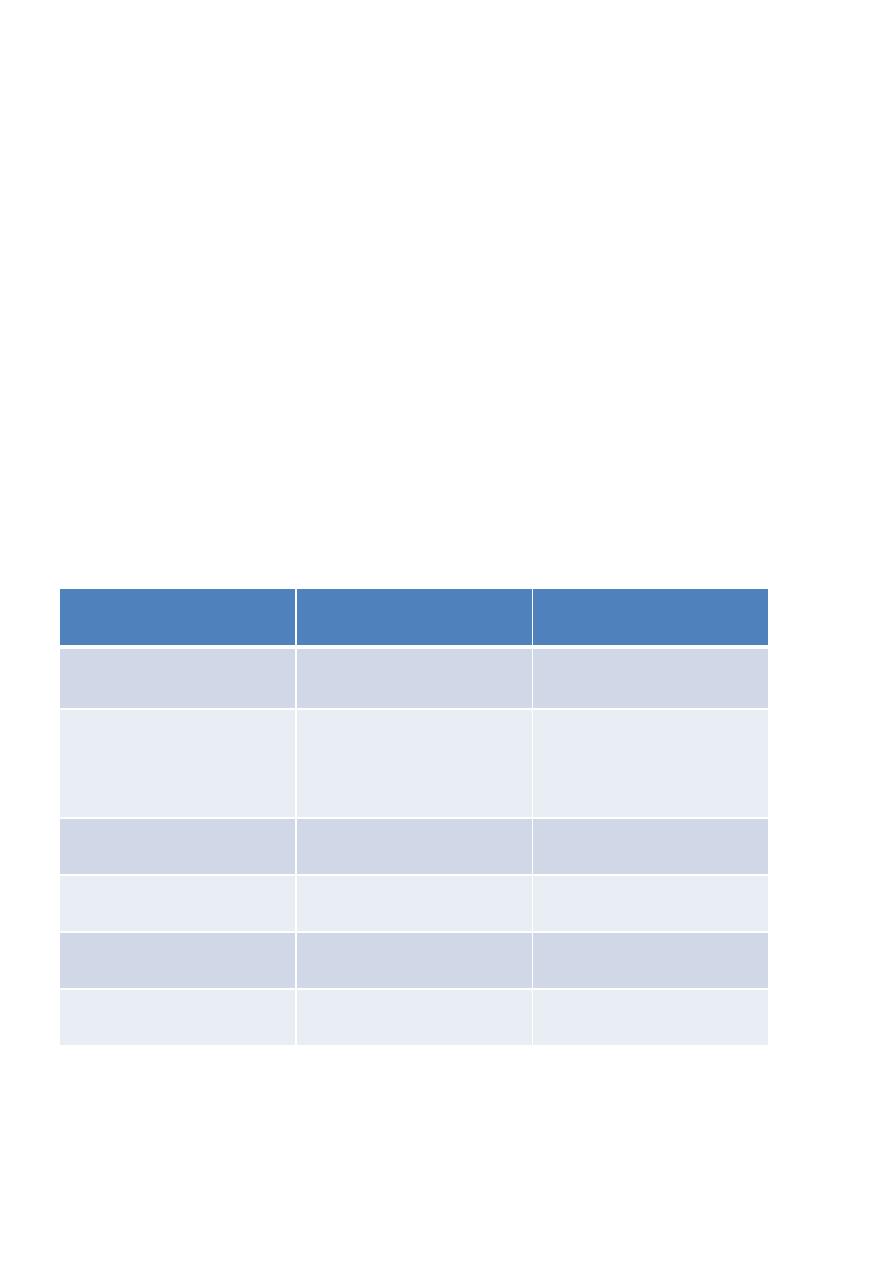
Typical verses atypical
atypical
Typical
Variable
Less acute proceeded by
flue or URTI
Acute
Onset
Mostly
Mycoplasma
Chlamydia
Legionella
Classical bacteria mostly
Pneumococcus
Cause
Less
High
Inflammatory markers
Interstitial
lobar
CXR
Teenage & young adult
any
age
Walking pneumonia
more
Severity
B- Chemical as drugs or occupational exposure
C- Inhalational as aspiration
D- Immune as cryptogenic organizing pneumonia or eosinophilic
pneumonia

2- Radiological :
A- Lobar : the consolidation involve the entire lobe or segment
limited by the fissure.
B- Bronchopneumonia the bronchial wall & the surrounding
alveoli are involved lead to bilateral consolidation nodules
isolated or confluent with inter-spacer normal lung tissue.
C- Interstitial pneumonia: the interstitial tissue is inflamed causing
reticular shadow mostly bilateral & basal
3- Location of acquiring :
A- Community acquired pneumonia: pneumonia acquired outside a
hospital or long-term care facility
B-
Hospital acquired pneumonia: or nosocomial pneumonia, is
a lower respiratory infection that was not incubating at the time of
hospital admission and that presents clinically 48 hours or more
after hospitalization.
C- Healthcare associated pneumonia: pneumonia in non-
hospitalized patients who had significant experience with the
healthcare system. Such contact could include (1) intravenous
antibiotics therapy within the preceding 30 days (2) residence in
a long-term care facility (3) hospitalization in an acute-care
hospital within the preceding 90 days (4) outpatient treatment in
a hospital or hemodialysis clinic within the preceding 30 days.
D- Ventilator associated pneumonia: as pneumonia that present
more than 48 hours after endotracheal intubation.
Clinical features :
Typical pneumonia:
Usual bacteria
– Sudden/subacute onset
– Fever with chills, rigors
– Productive cough, Mucopurulent sputum
– Tachypnea and tachycardia
– breathlessness

– Pleuritic chest pain
– Breath sound: crackles and rales
Atypical
– Gradual onset
– Afebrile
– Dry cough
– Breath sound: Rales
– Uni/bilateral patchy, infiltrates
– WBC: usual normal or slight high
– Sore throat, myalgia, fatigue, diarrhea
Diagnosis
:
1- Imaging studies:
A- X
‐Ray chest P/A & lateral view: very essential for diagnosis &
complications detection ,it may be normal too early or in obese patients
but not used for follow up as there is a time lag between the
clinical(earlier) & the radiological recovery as the CXR recovery may
take 4-6 weeks & up to 12 weeks in elderly or COPD patients
B- Compute tomography: not used routinely because of the radiational
hazards indicated only for non-resolving pneumonia or when there is a
suspicion of malignancy.
2- Lab. Tests
A- CBC with differential: neutrophilia –bacterial , lymphopenia—
atypical
B- BUN/Cr, electrolytes: hyponatremia –legionella & the BUN for
severity assessment
C- Glucose, liver enzymes: abnormal liver function---mycoplasma
D- Blood culture
3- Microbiological tests: to detect the causative agent not needed routinely
only for patients with severe CAP, need hospitalization or ICU or not
responding to treatment as:
1- sputum Gram stain
2- Sputum for culture
3- Sputum for Ziehl Neelsen stain
4- Sputum cytology
Sputum quality should be ensured by
•PMN’s>25/LPF
•Few epithelial cells<10/LPF
• Single predominant organism
5- Pneumococcal antigen test
6- Legionella antigen in urine: very good in diagnosis
4- Arterial oxygen saturation for hypoxemia patients or need ICU admission
Principles of management
•Prompt initiation of antibiotic therapy
•Pathogen directed antimicrobial therapy whenever possible
•Rational use of microbiology laboratory
•Decision to hospitalize based on prognostic criteria
Criteria for risk stratification (CURB
‐
65)
• Confusion
• Urea ≥7 mmol/L
• Respiratory rate ≥30/min
• Low blood pressure (diastolic blood pressure ≤60 mm Hg or systolic
blood pressure ≤90 mm Hg)
• Age ≥65 years
1 point outpat . treatment
2 -3 points inpat. Treatment
>3 points ICU treatment
Outpatient treatment
Emperic treatment

Amoxycillin, Amoxycillin + clavulanic acid, Macrolide,Doxycycline or
Fluoroquinolone
Single or combination therapy can be given
Inpatient management
Pathogen directed treatment/ Emperic
• Injectable drugs are used initially
• Combinations of drugs are preferred
• In elderly, diabetics, alcoholism, those with structural lung disease,
cephalosporins are preferred
ICU management
Pathogen directed treatment : use aggressive treatment as
3rd & 4th generation cephalosporins
Carbapenems
Vancomycin/Teicoplanin
Metronidazole/clindamycin
Antibiotic active against atypical organisms:
1- Erythromycin as azithromycin
2- Tetracycline as doxycycline
3- Respiratory quinolone as moxifloxacin , levofloxacine or ofloxacin
4- Rifampicine
Wait for 48
‐72 hrs for the drugs to act and before labeling treatment
failure
Criteria for clinical stability
• Temperature ≤37.8° C
• Heart rate ≤100 beats/minute
• Systolic blood pressure ≥90 mm Hg
• Respiratory rate ≤24 breaths/minute

• Oxyhemoglobin saturation ≥90% or PO2 ≥60 mm Hg
4 out of 5 criteria need to be fulfilled in stability criteria
Generally 7
‐10 days of antibiotics are sufficient except in:
1- Staph pneumonia
2- Atypical pneumonia
Where 21 days treatment is indicated
• Once the stability criteria are met, patient can be switched to oral
antibiotics ( same group)
Prevention
Pneumococcal vaccine: act agnost 23 variant given with recovery for all
patients older than 65 yreas old plus chronic respiratory , medical or
hematological diseases
Give protection for 5 years & can be booster in 2
nd
dose
Influenza vaccine: should be give annularly for risky patients from
September to October i.e. before the session
Complication
:
1- Local complications : due to lung affection by the infection as:
A- Lung abcess
B- Empyema
C- Parapneumonic effusion
2- Systemic complications due to systemic reactions as:
A- Bacteremia , sepsis & shock
B- Death
C- Distant infection & abscesses as meningitis & infective
endocarditis
D- Thromboembolism & thrombophlebitis
E- Antibiotics side effects
Failure to response:
Failure of clinical response within 96 hours not radiological , mostly due
to:

1- Incorrect diagnosis
2- Wrong or inappropriate antibiotic type or dose
3- Complications
4- Underlying cause as malignancy or embolism
5- Non-sensitive organisms as TB or fungus
Work up:
Imaging as new CXR & CT contrast or CT angio.
Bronchoscopy to exclude underlying causes as Cancer or FB
Microbiological studies to ensure the organisms & there sensitivity
