GIT
Lec 2 Dr.Hassan aljumaily
candidiasis
parotitis
aphthus ulcer
GERD
Achalasia
DES,NCE
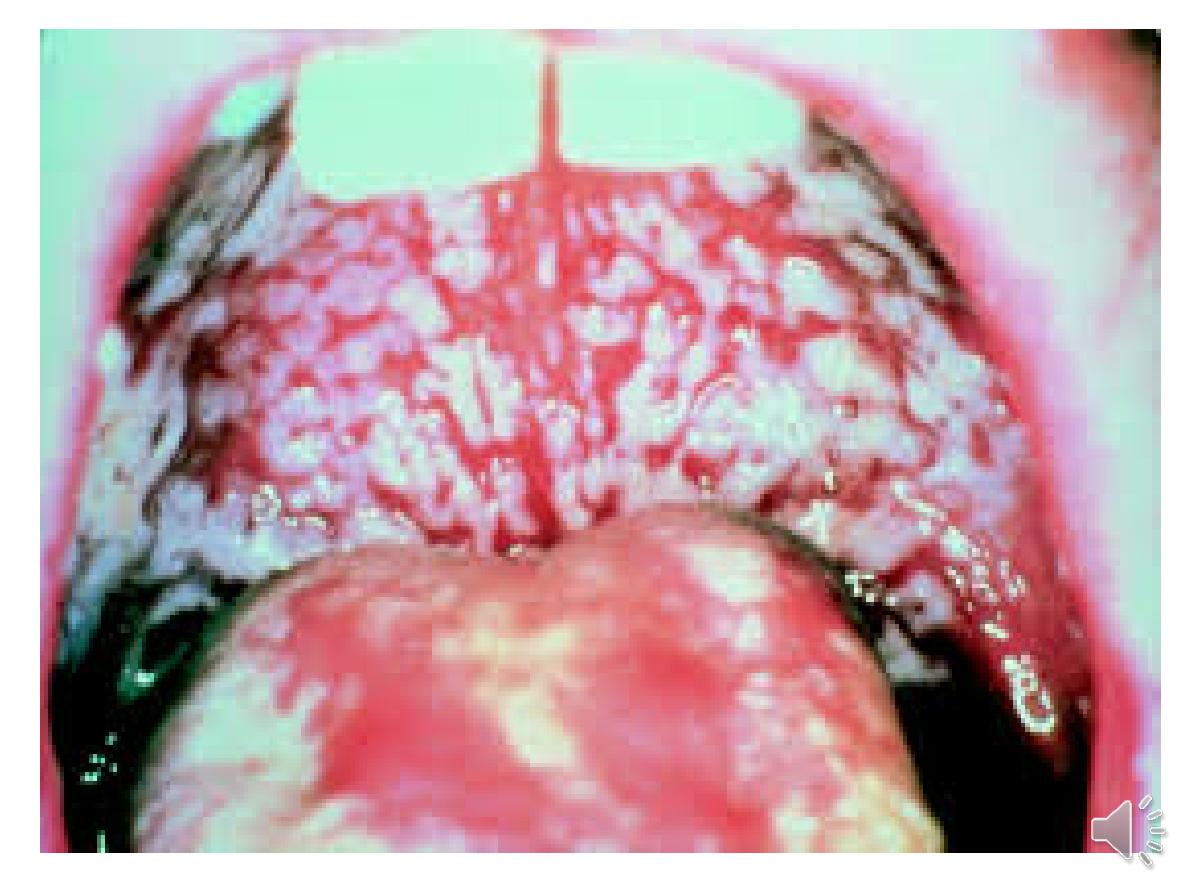
Candidiasis
Candida albicans
--- thrush.
babies, debilitated patients, patients on
steroid or AB therapy, DM &
immunosuppressed patients
White patches
.Odynophagia or dysphagia
suggests pharyngeal ,oesophageal candidiasis.
A clinical diagnosis or brushings or biopsies
can be obtained for mycological examination.
treated using
nystatin or amphotericin
.
Resistant cases or immunosuppressed
patients may require
oral fluconazole
.
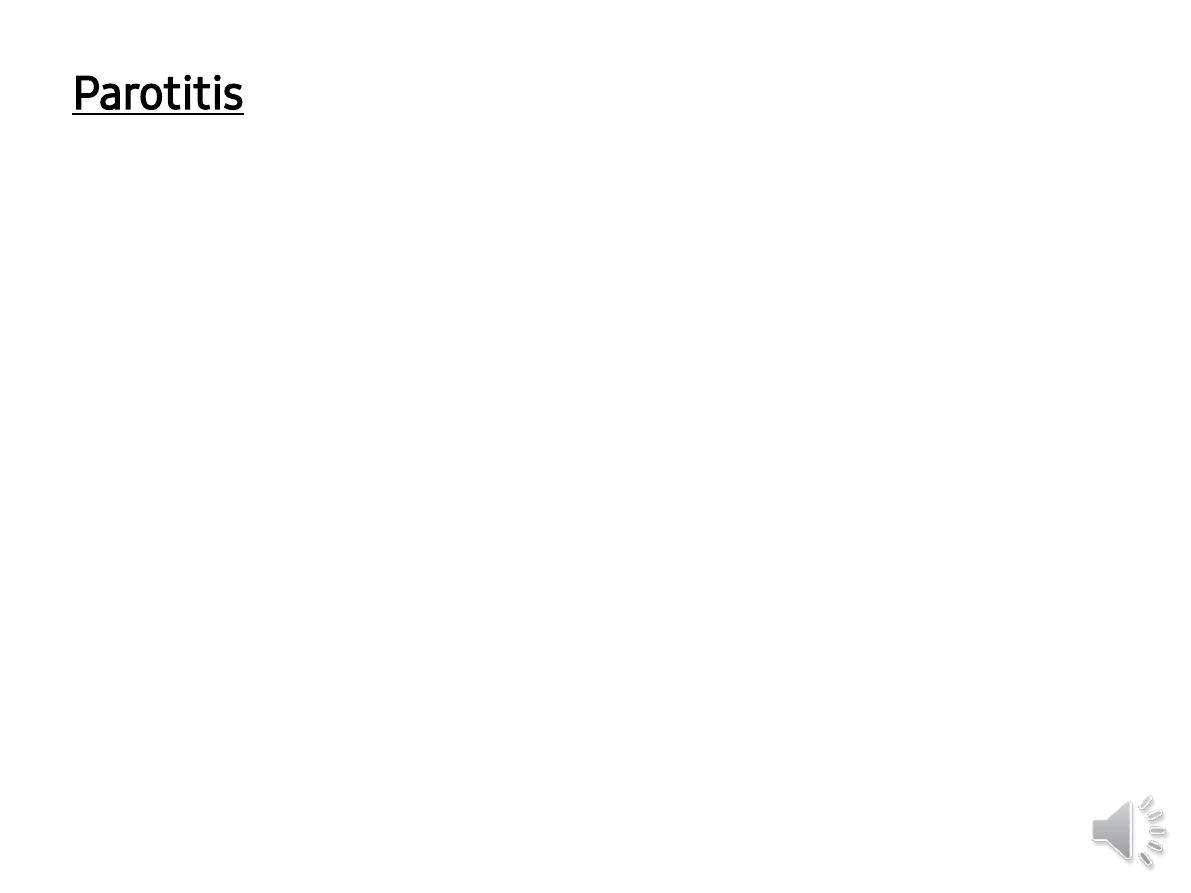
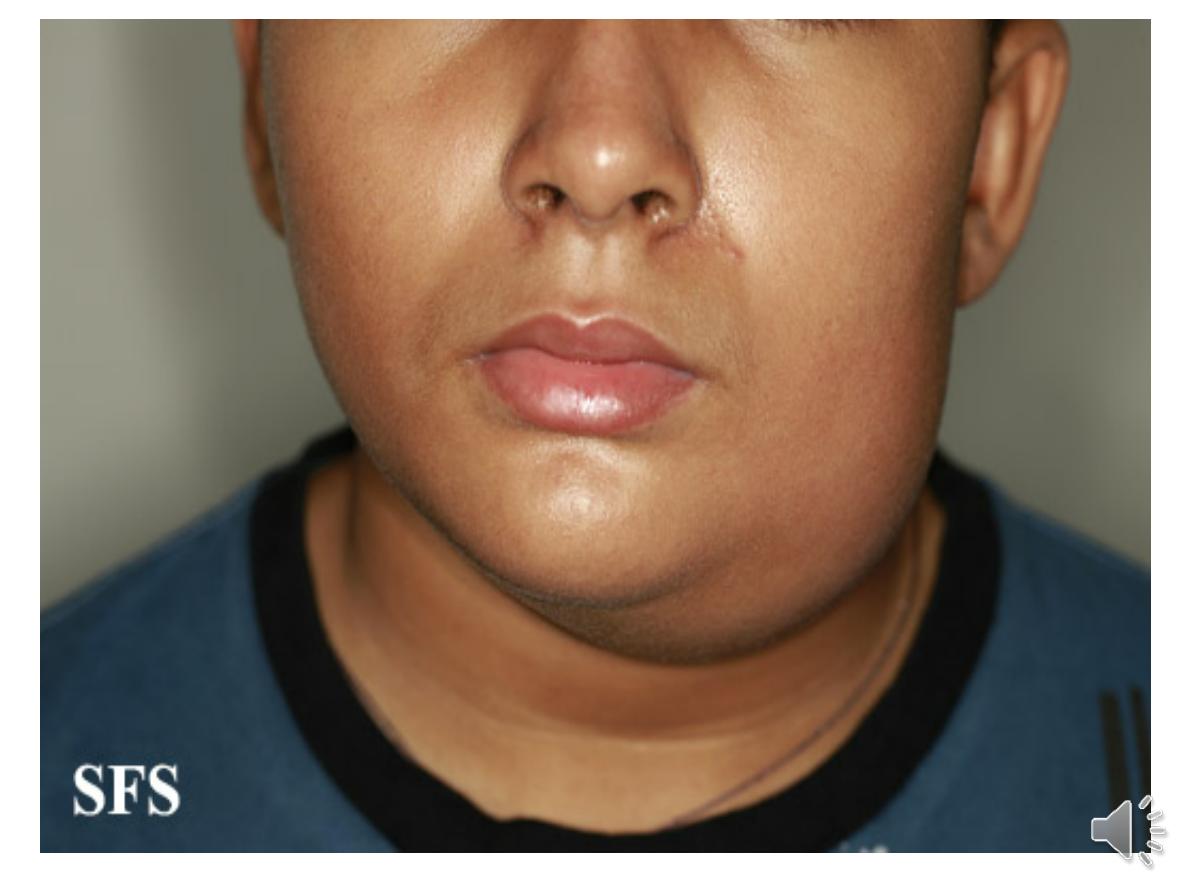
Parotitis
Parotitis is due to viral or bacterial infection.
Bacterial parotitis
Cx of major surgery. Enhanced by
dehydration and poor oral hygiene.
Patients present with painful parotid swelling and
this can be complicated by abscess formation.
antibiotics are required, whilst surgical drainage is
necessary for abscesses.
Other causes of salivary Calculi ,Sj
ِgren’s syndrome
Sarcoidosis …Tumours
Benign: pleomorphic adenoma (95% of cases)
Intermediate: mucoepidermoid tumour
Malignant: carcinoma
.
Aphthous ulceration
superficial
and
painful
Recurrent 30%
common in
women
prior to menstruation.
The cause is unknown.
Mx:
topical steroids
Symptomatic →local anaesthetic
mouthwashes.
Rarely, patients with very severe,
recurrent aphthous ulcers may need oral
steroids .
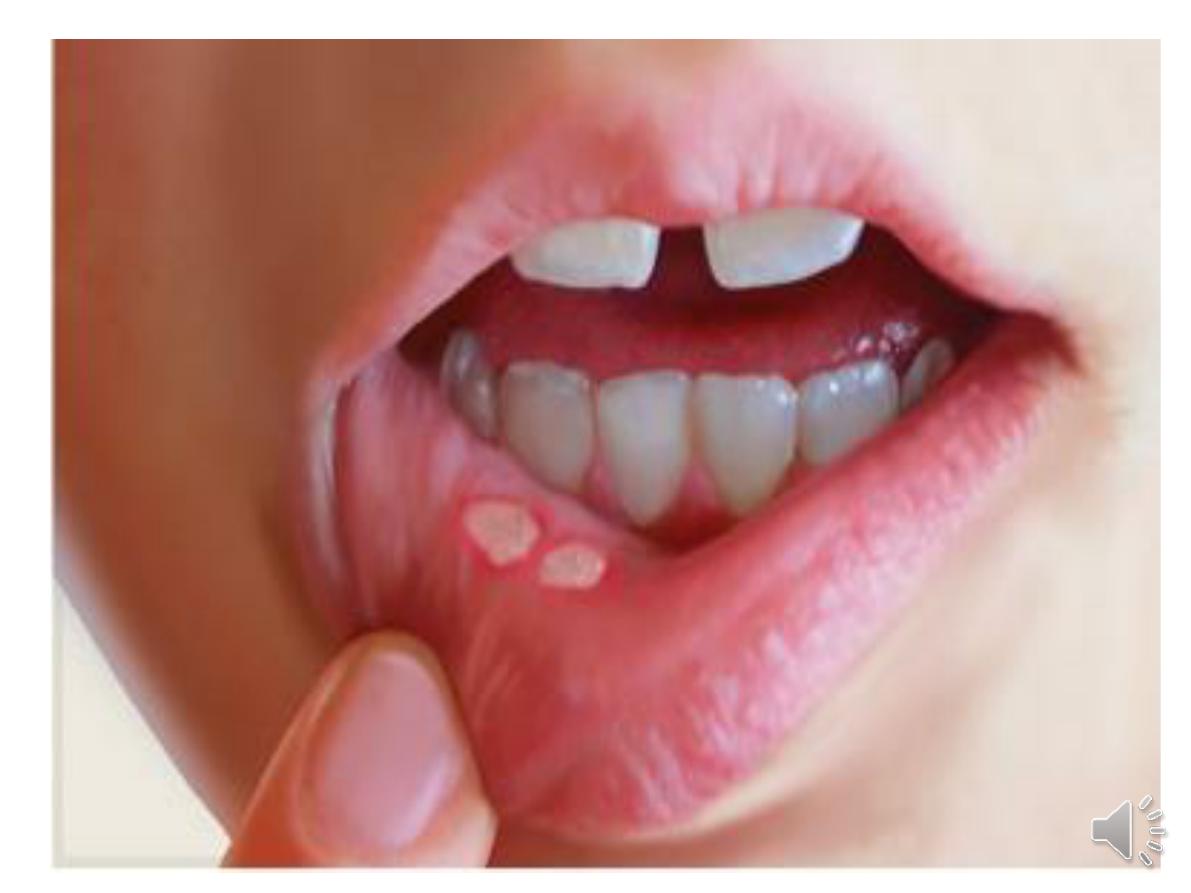
other causes of oral ulceration:
Infection
• Fungal (candidiasis) • Viral (herpes simplex, HIV) • Bacterial,
including syphilis, tuberculosis
Gastrointestinal diseases
• Crohn’s disease • Coeliac disease
Dermatological conditions
• Lichen planus•• Dermatitis herpetiformis • Erythema
multiforme
Drugs
•, NSAIDs, methotrexate, penicillamine, losartan, ACE
inhibitors • Cytotoxic drugs
Systemic diseases
• Systemic lupus erythematosus • Behçet’s syndrome
Neoplasia
• Carcinoma • Leukaemia • Kaposi’s sarcoma
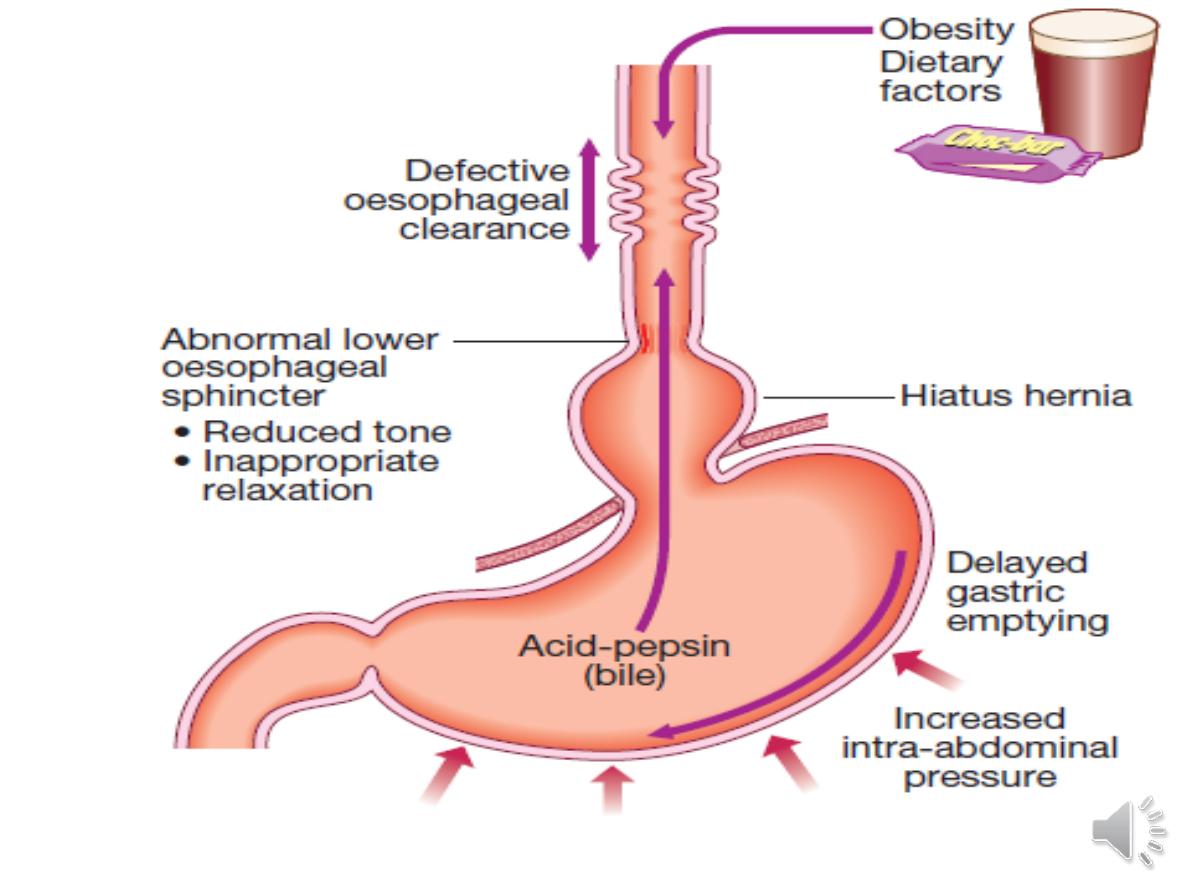
GERD
heartburn and regurgitation
, often provoked
by bending, straining or lying down.
‘
Waterbrash
’, The patient is often overweight.
Some patients are woken at night by choking
as refluxed fluid irritates the larynx
.
--odynophagia or dysphagia.
other :
atypical chest pain
which may be severe
and can mimic angina, and may be due to
reflux-induced oesophageal spasm.
Others include
hoarseness
(‘acid laryngitis’),
recurrent chest infections, chronic cough
Investigations
1- if age >50
2-if symptoms are atypical or complication is
suspected((worrying features such as
dysphagia,
weight loss or anaemia
)) →
OGD is indicated.
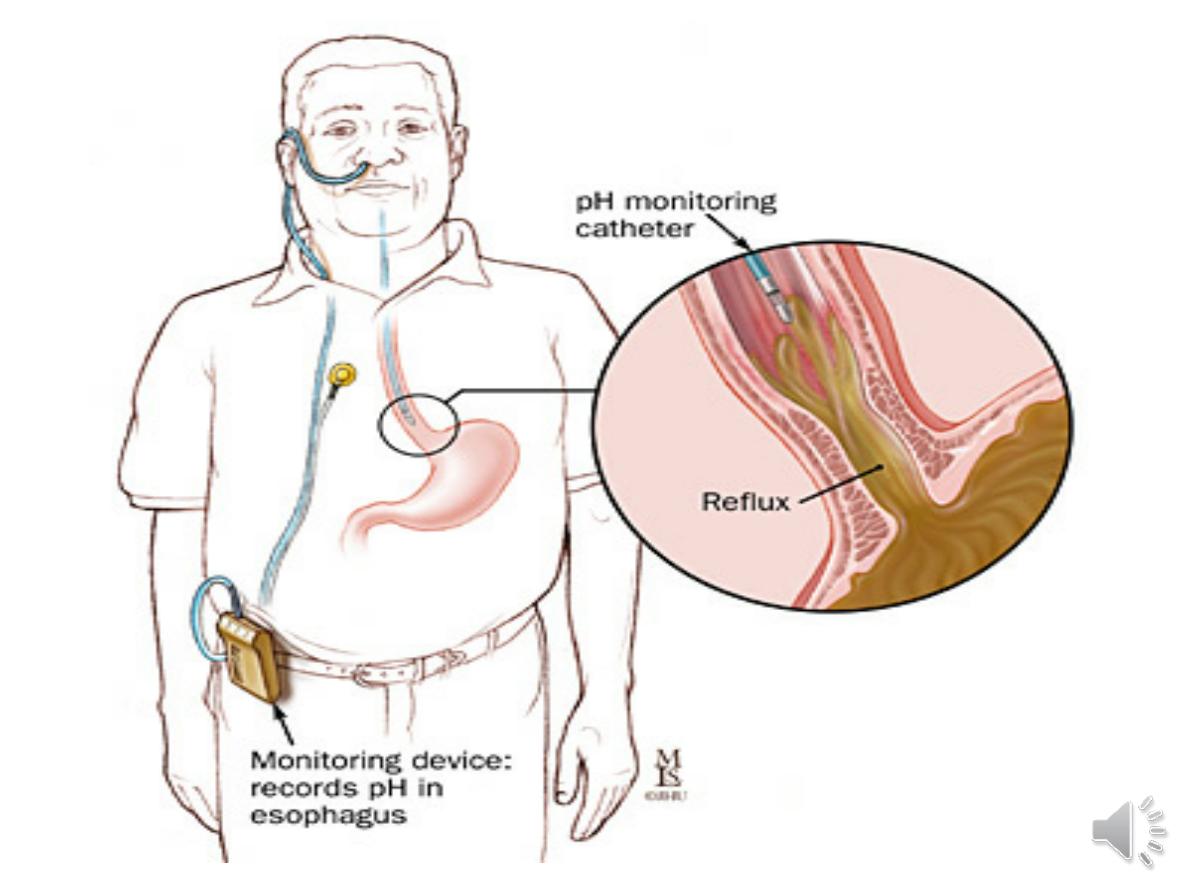
** 24 hr pH monitoring.
** 24 hr pH monitoring.
This involves tethering a slim catheter with a
terminal radiotelemetry pH-sensitive probe
above the gastro-oesophageal junction. The
intraluminal pH is recorded whilst the patient
undergoes normal activities, and episodes of
symptoms are noted and related to pH
. A pH of
less than 4 for more than 6–7% of the study time
is diagnostic of reflux
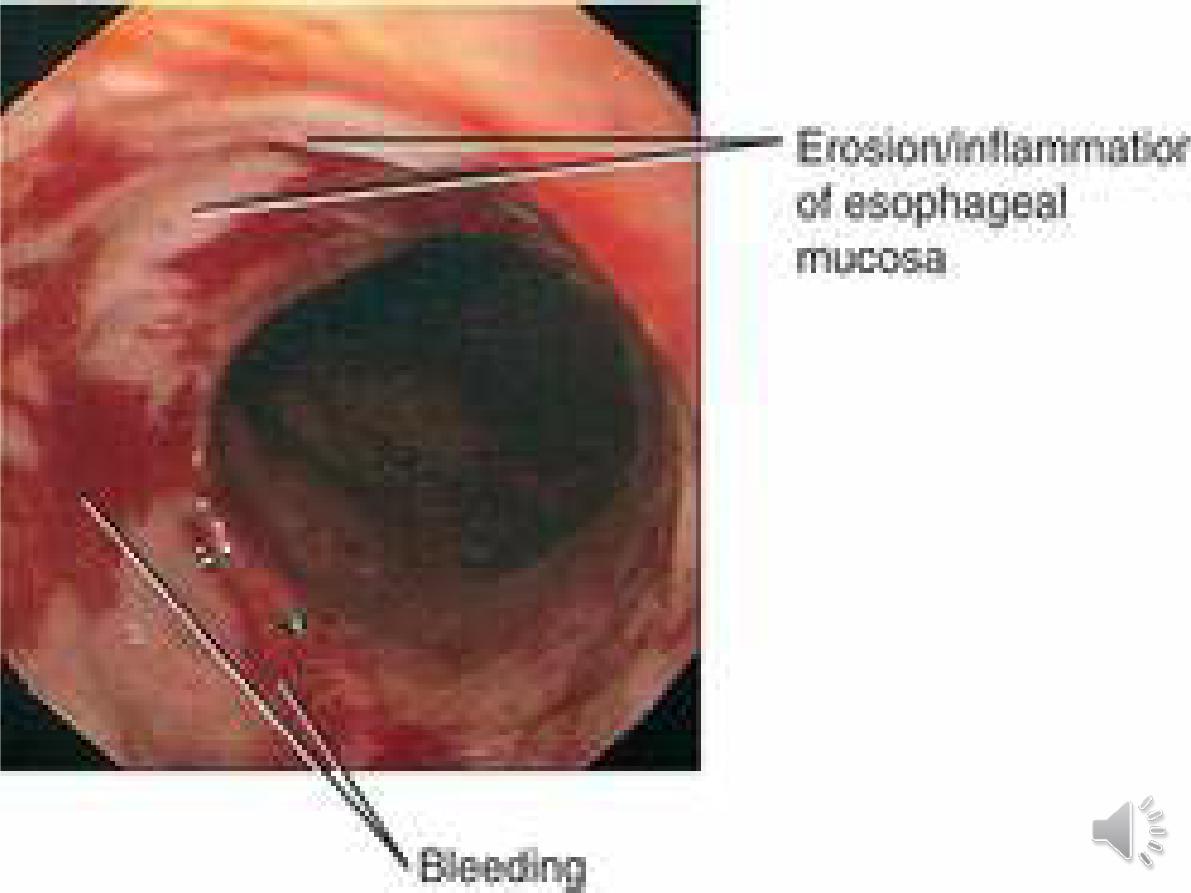
Complications
Oesophagitis
A range of endoscopic findings, from mild redness to severe,
bleeding ulceration
Anaemia
Iron deficiency anaemia.
Gastric volvulus
oesophageal or gastric obstruction and the patient presents
with severe chest pain, vomiting and dysphagia. The diagnosis
is made by chest X-ray (air bubble in the chest) and barium
swallow.
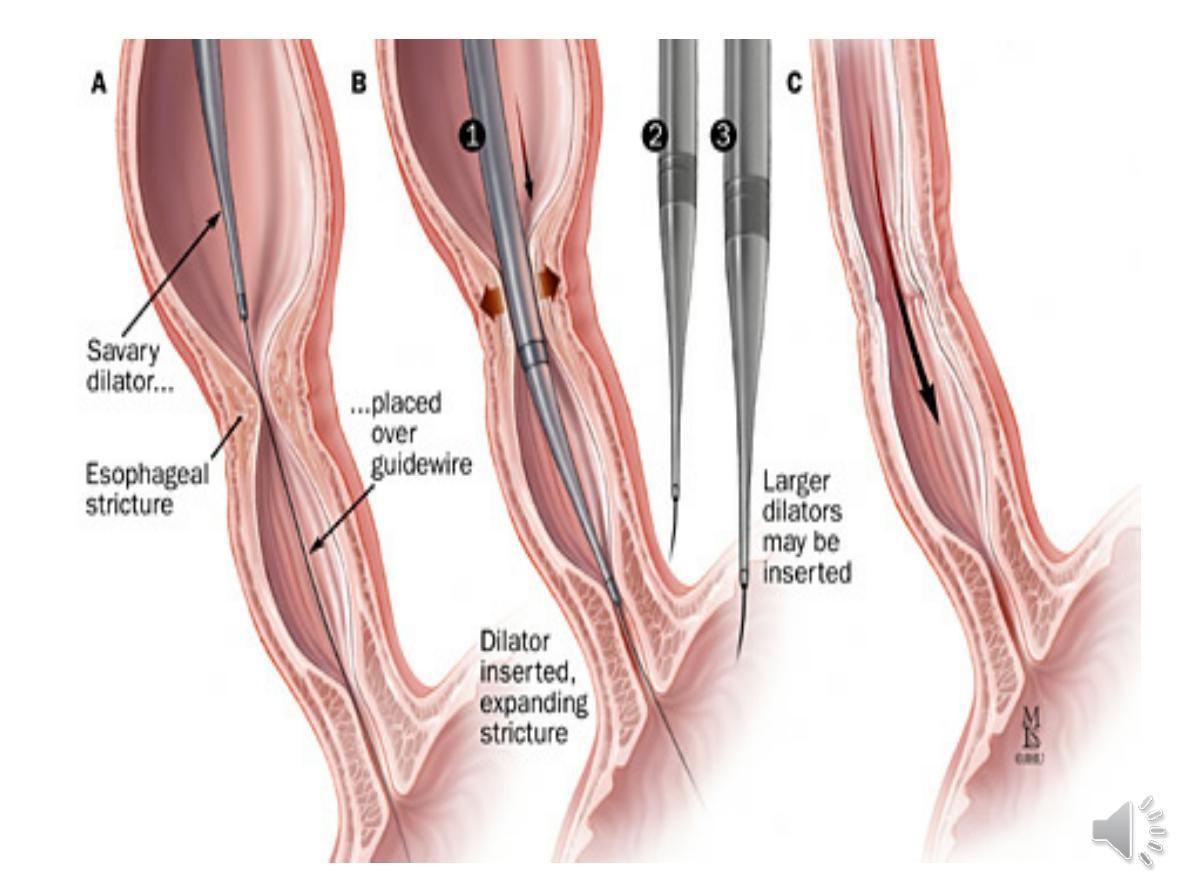
Benign oesophageal stricture
Fibrous strictures especially in the elderly. dysphagia for
solids than for liquids .many elderly patients presenting with
strictures have no preceding heartburn. Diagnosis is by
endoscopy, when biopsies of the stricture can be taken to
exclude malignancy. Endoscopic balloon dilatation helpful
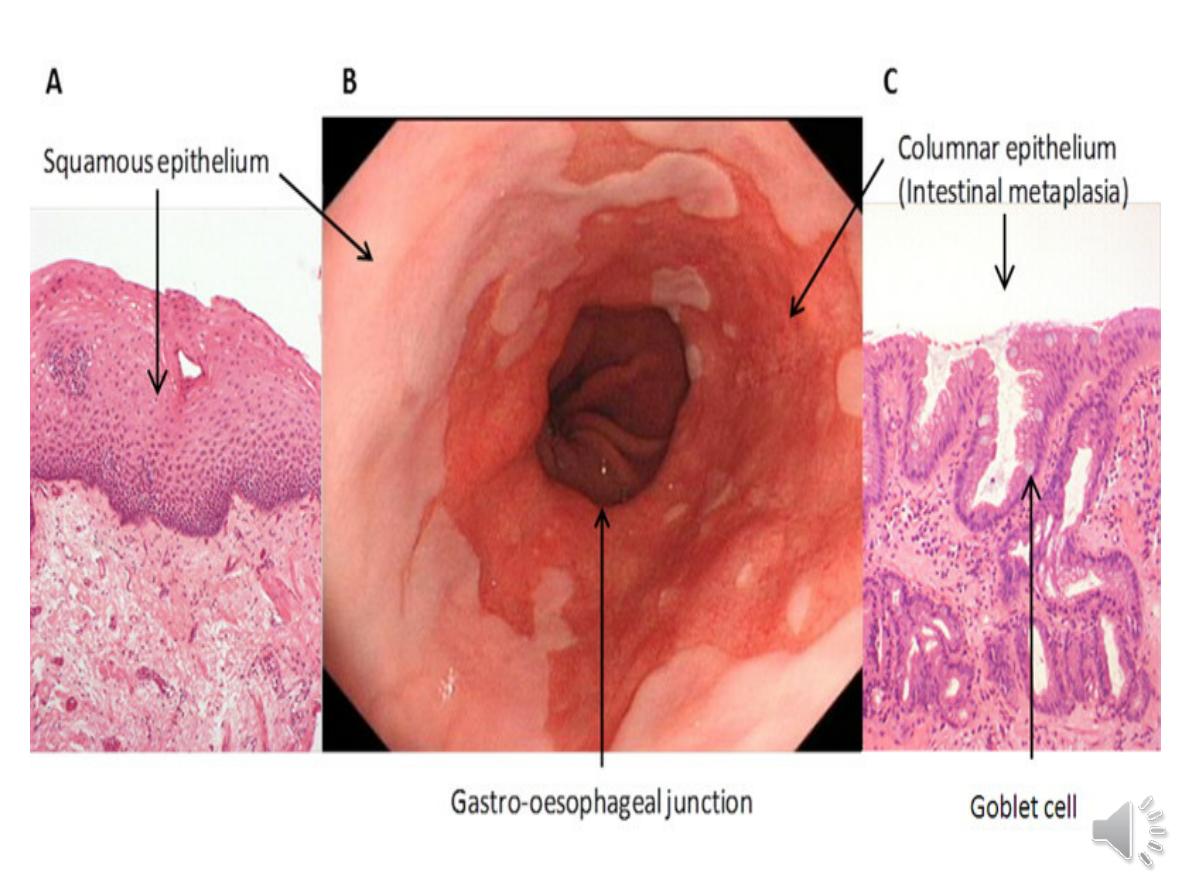
Barrett’s oesophagus
▲ Barrett’s oesophagus is a
pre-malignant condition
, in which
the normal squamous lining of the lower oesophagus is replaced
by columnar mucosa (
columnar lined oesophagus; CLO
) that may
contain areas of intestinal metaplasia .
▲ 10% of patients undergoing gastroscopy for reflux symptoms.
▲ 1.5–5% of the population, as the condition is often
asymptomatic
until discovered when the patient presents with oesophageal
cancer.
▲ more common in
men (
especially white), the
obese
and those
over
50 years of age
. It is weakly associated with smoking but
not alcohol intake.
The risk of cancer seems to relate to the
severity and duration of reflux rather than the presence of CLO
per se
.
▲ inactivation of the tumour suppression protein p16 followed
by somatic inactivation of p53, which promotes tumour
progression.
Diagnosis.
Bx
Management.
Neither potent acid suppression nor antireflux surgery stops
progression or induces regression of CLO,
Endoscopic therapies, such as
radiofrequency ablation or
photodynamic therapy
, can induce regression but, at present, are
used only for those with dysplasia or intramucosal cancer. Regular
endoscopic surveillance can detect dysplasia at an early stage and
may improve survival but, because most CLO is undetected until
cancer develops, surveillance strategies are unlikely to influence
the overall mortality rate of oesophageal cancer
.
Surveillance
1-patients with CLO without dysplasia should undergo endoscopy at
3–5-yearly intervals
2- those with low grade dysplasia at 6–12-monthly intervals.
3- those with high-grade dysplasia (HGD) or intramucosal
carcinoma, the treatment options are either
oesophagectomy
or
endoscopic therapy
with a combination of
endoscopic resection (ER) of any visibly abnormal
areas and radiofrequency ablation (RFA) of the remaining Barrett’s
mucosa
Management of GERD:
♠
Lifestyle advice: weight loss, avoidance of diet worsen
symptoms, elevation of the bed head , avoidance of late meals
and giving up smoking.
♠
PPI.
♠
When dysmotility features are prominent, domperidone can
be helpful
.
♠There is no evidence that
H. pylori
eradication has any
therapeutic value.
♠
Proprietary antacids and alginates can also provide
symptomatic benefit. H2-receptor antagonist drugs also help
symptoms
♠Patients who fail to respond to medical therapy, those who
are unwilling to take long-term PPIs and those whose major
symptom is severe regurgitation should be considered for
laparoscopic anti-reflux surgery
. small minority develop
complications, such as inability to vomit and abdominal
bloating (‘gas-bloat’ syndrome’).

Other causes of oesophagitis
Infection
Corrosives
Suicide attempt by bleach or battery acid
--extensive erosive oesophagitis. Cx =oesophageal
perforation with mediastinitis and by stricture
formation. Rx=conservative, based upon analgesia
and nutritional support;
vomiting and endoscopy should be avoided because
of the high risk of oesophageal perforation.
a barium swallow ---stricture
. Endoscopic dilatation is usually necessary but it is
difficult and hazardous because strictures are often
long, tortuous and easily perforated
• a hypertonic lower oesophageal sphincter, whichfails to
relax
• failure of propagated oesophageal contraction, leading to
progressive dilatation of the gullet.
The cause is unknown.
Defective release of nitric oxide
degeneration of ganglion cells
within the sphincter and the
body .
Loss of the dorsal vagal nuclei within the brainstem
dysphagia
.--slowly, is initially intermittent, and is worse for
solids
and eased by drinking liquids, and by standing and moving
around after eating.
Heartburn does
not occur because the closed oesophageal
sphincter
chest pain
due to oesophageal spasm.
As the disease progresses worsens, the oesophagus empties
poorly and
nocturnal pulmonary aspiration
develops
. Achalasia predisposes to
squamous carcinoma of the
oesophagus
.
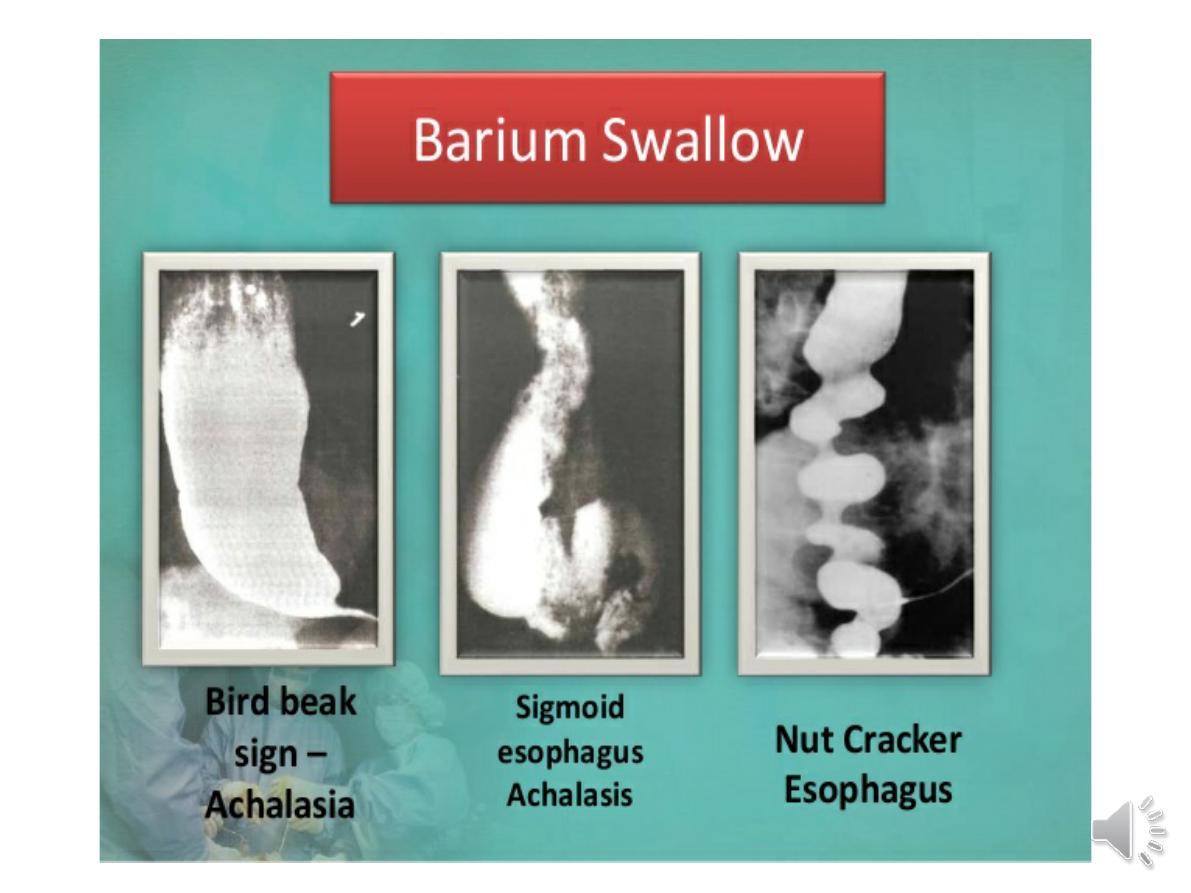
Investigations
1-
Endoscopy
should always be carried out
because carcinoma of the cardia can mimic the
presentation and radiological and manometric
features of achalasia (‘pseudo-achalasia’).
2-A
barium swallow
shows tapered
narrowing of the lower oesophagus
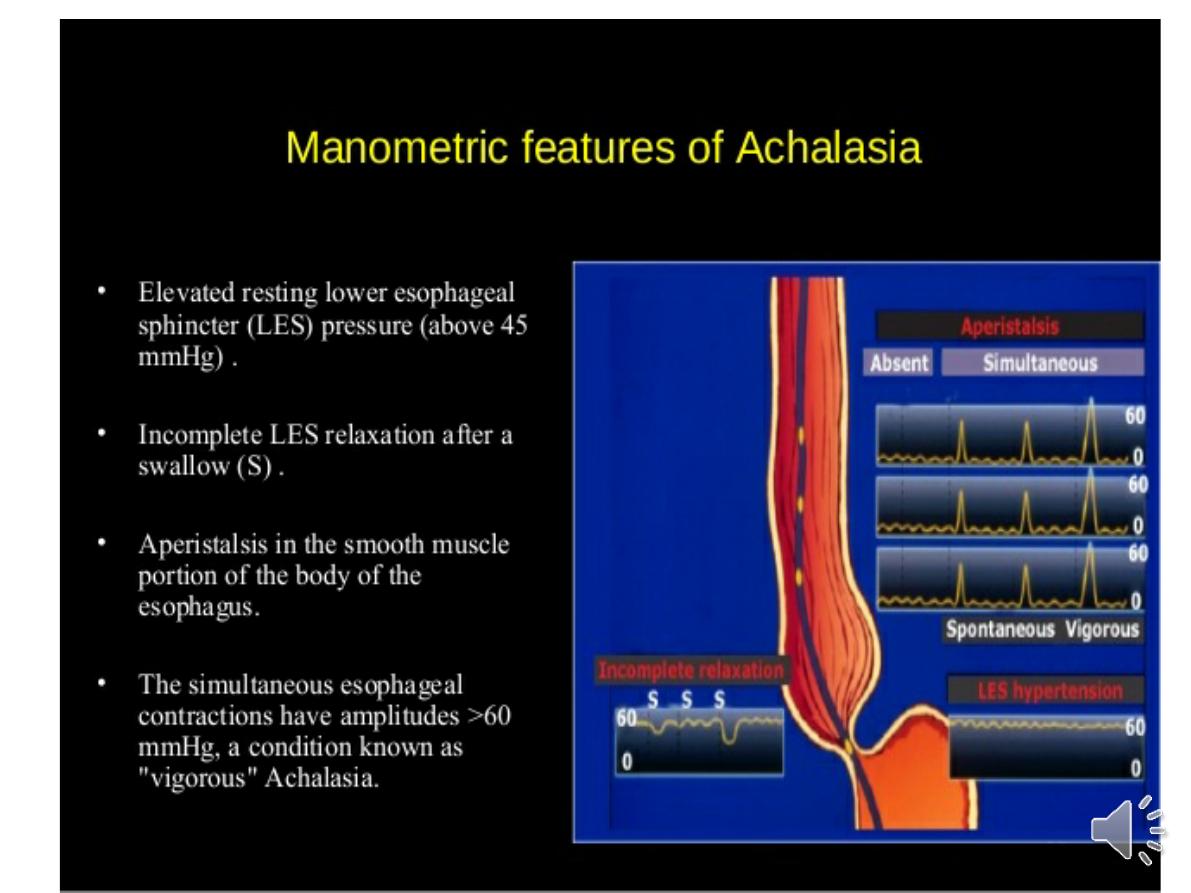
3-
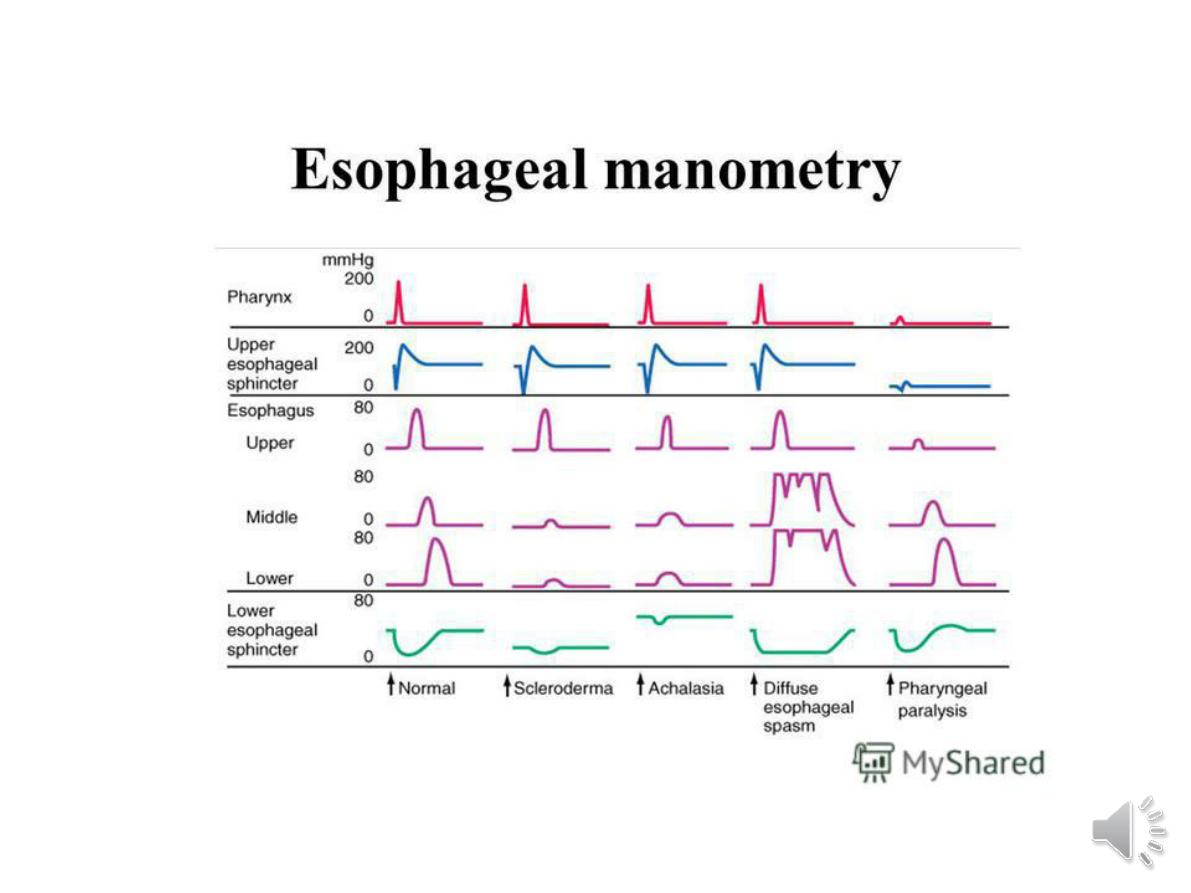
Manometry
confirms the highpressure,
non-relaxing lower oesophageal sphincter
with poor contractility of the oesophageal
body
Management
Endoscopic
-Forceful pneumatic dilatation using a 30–35-
mm diameter fluoroscopically positioned
balloon disrupts the oesophageal sphincter
and improves symptoms in 80% of patients..
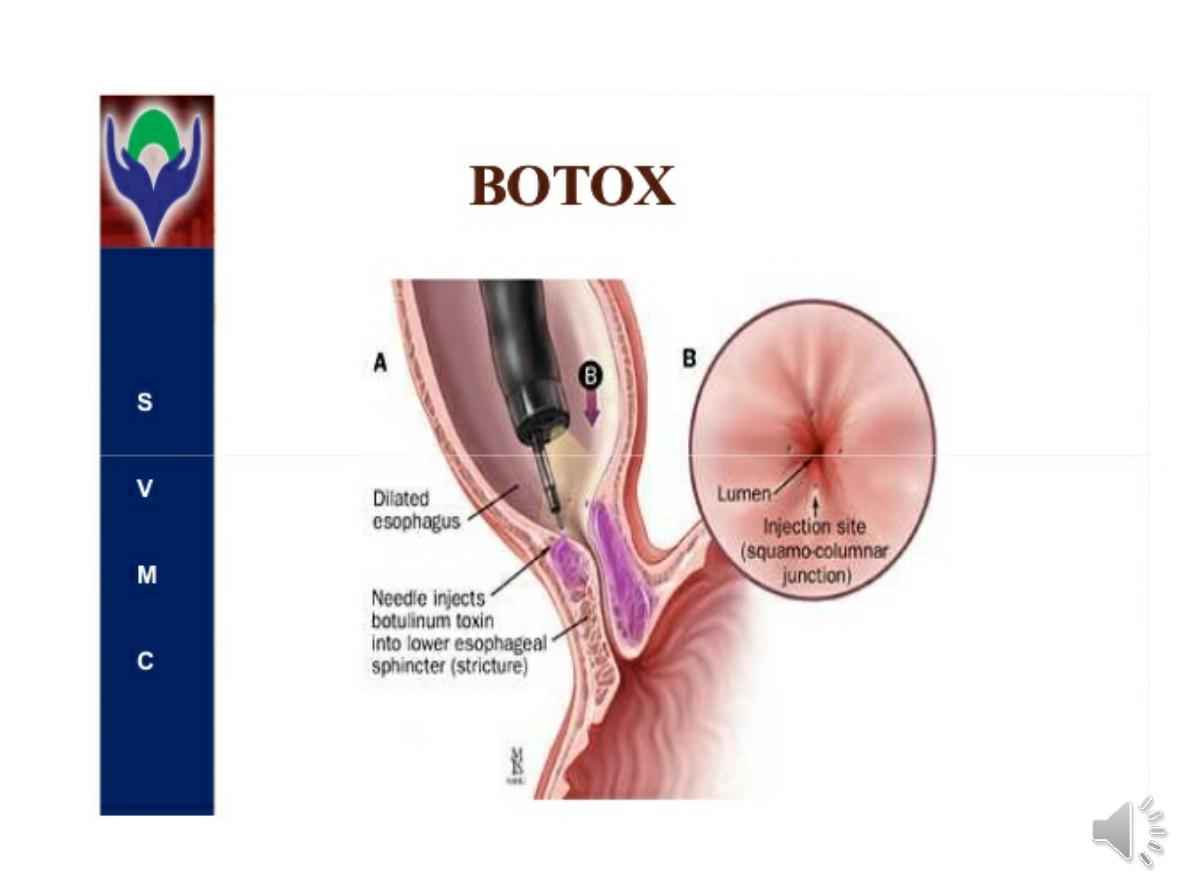
-Endoscopically directed injection of
botulinum toxin
into the lower oesophageal
sphincter induces clinical remission but
relapse is common.
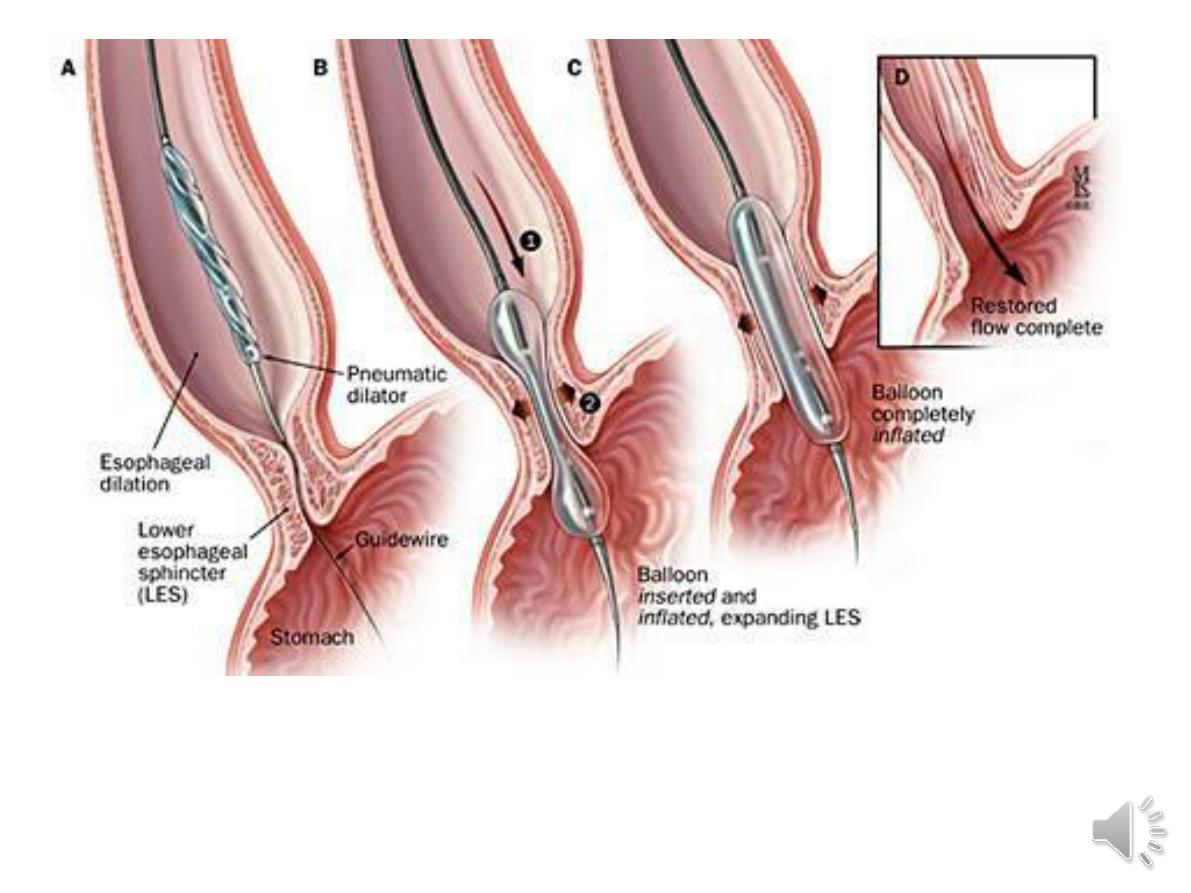

Surgical
Surgical myotomy (Heller’s operation),
performed either laparoscopically or as an open
operation, is effective but is more invasive than
endoscopic dilatation. Both pneumatic
dilatation and myotomy may be complicated by
GERD
, and this can lead to severe oesophagitis
because oesophageal clearance is so poor.
For this reason, Heller’s myotomy is
accompanied by a
partial fundoplication
anti-
reflux procedure.-----PPI therapy is often
necessary after surgery
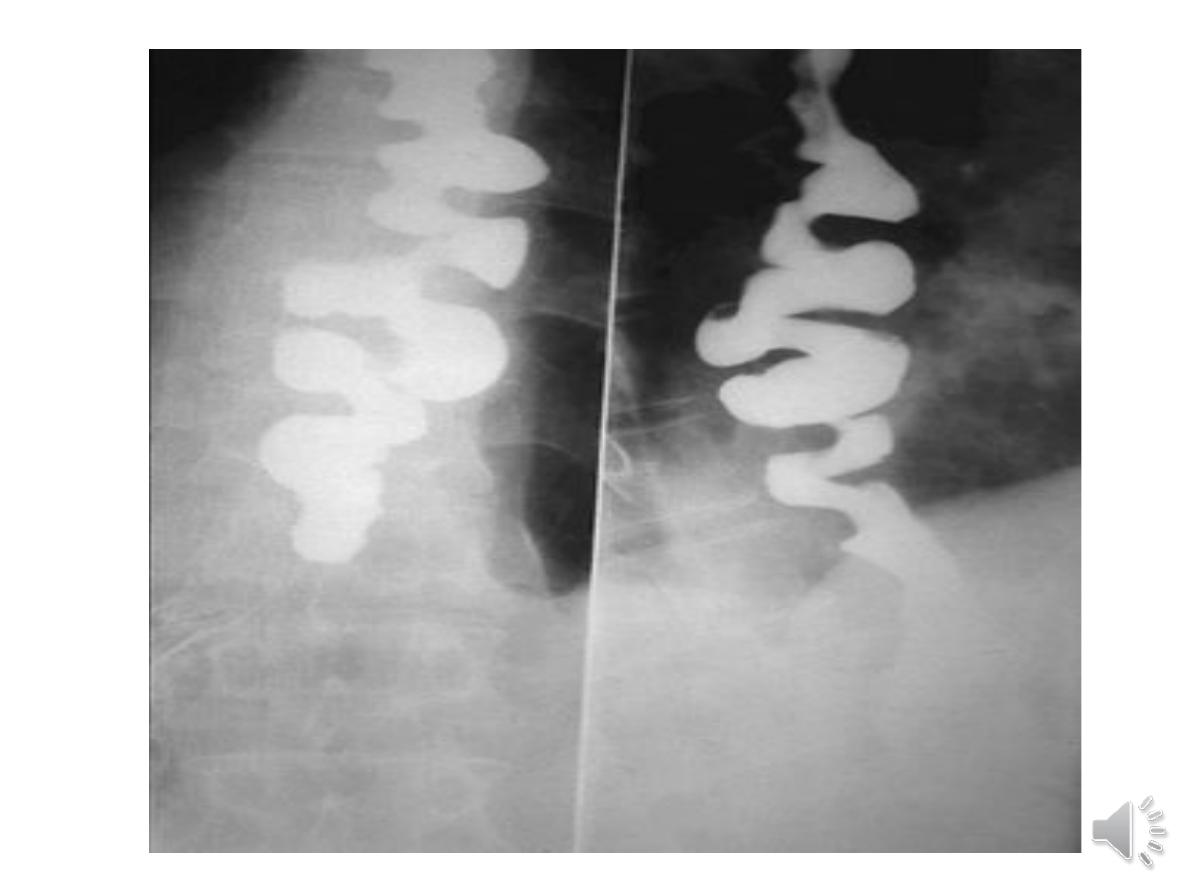
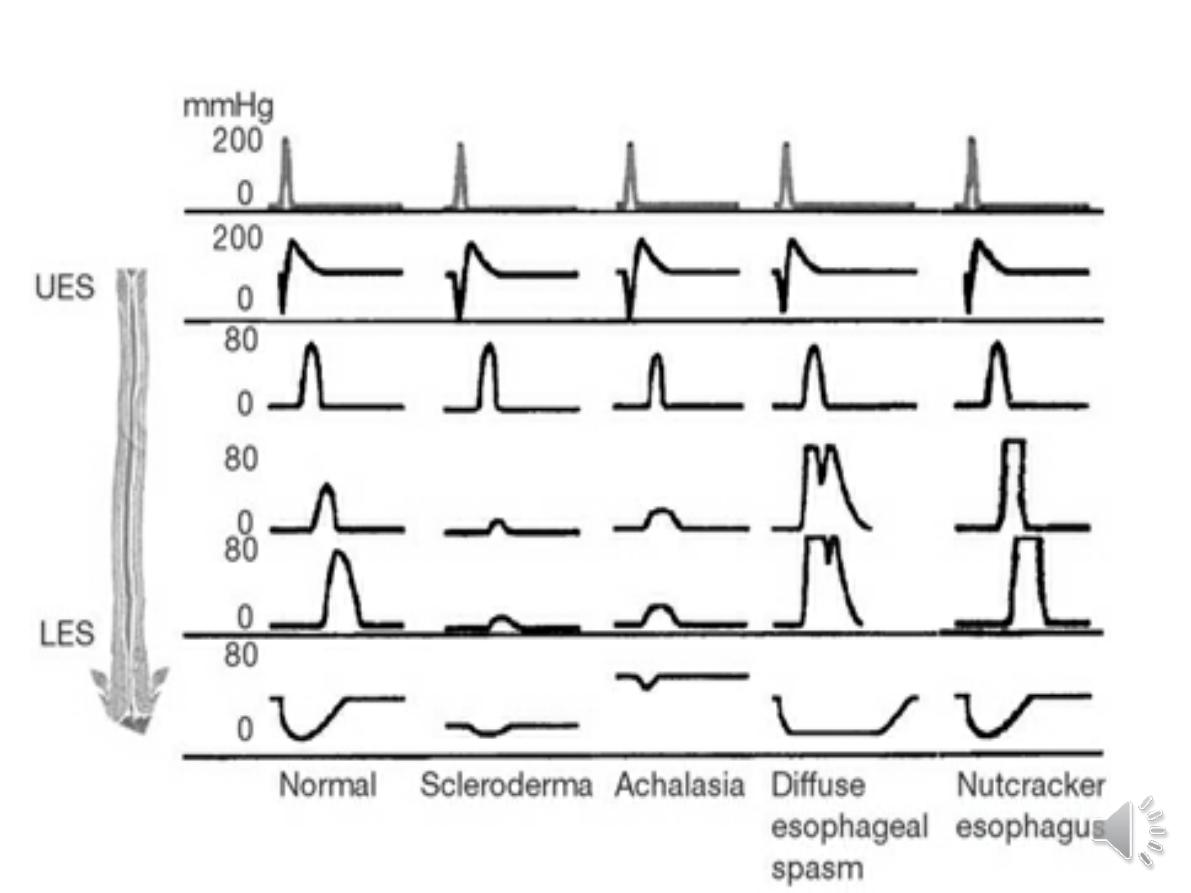
Diffuse oesophageal spasm
late middle age with episodic
chest
pain
that may mimic angina. sometimes
dysphagia
Some cases occur in response to GERD
Treatment is based upon the use of
PPI
drugs when GERD is present.
Oral or sublingual
nitrates or nifedipine
may relieve attacks of pain.
the alternatives:
pneumatic dilatation
and surgical myotomy
.
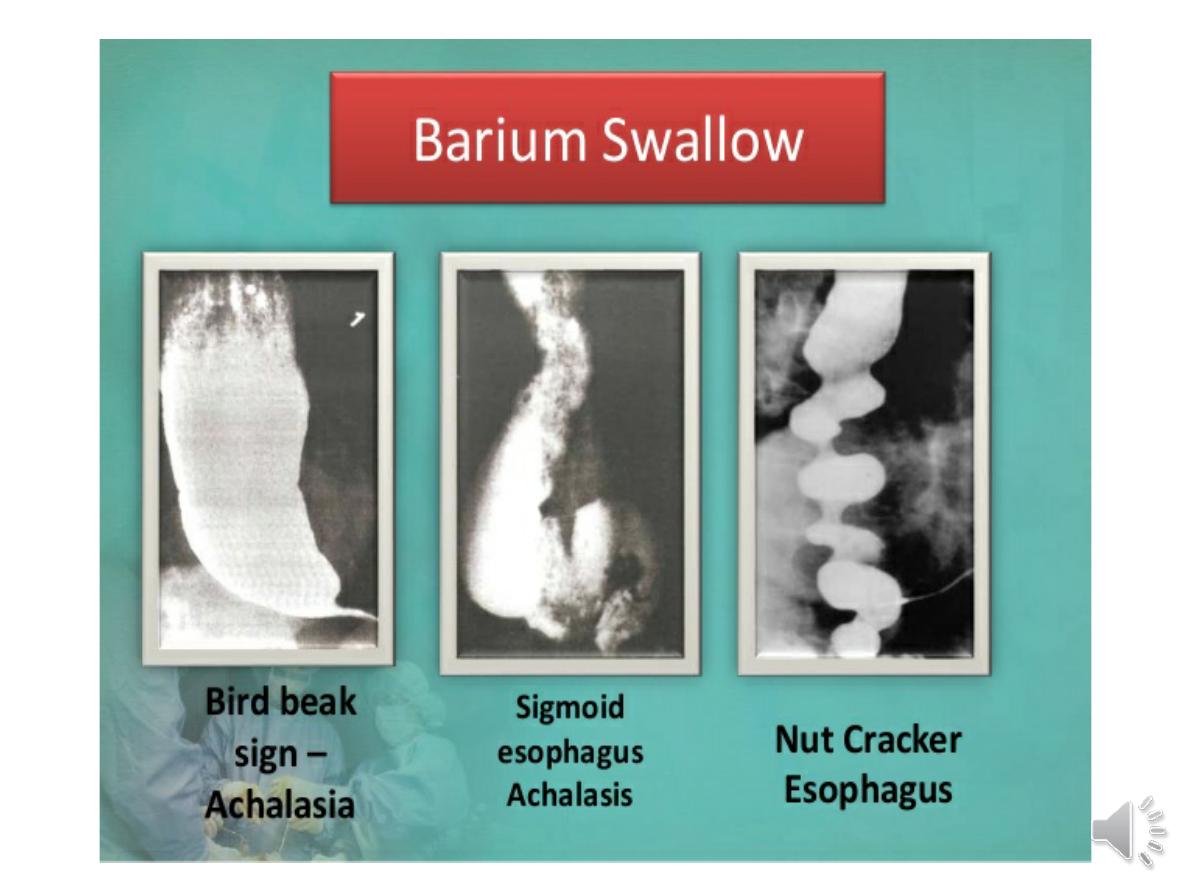
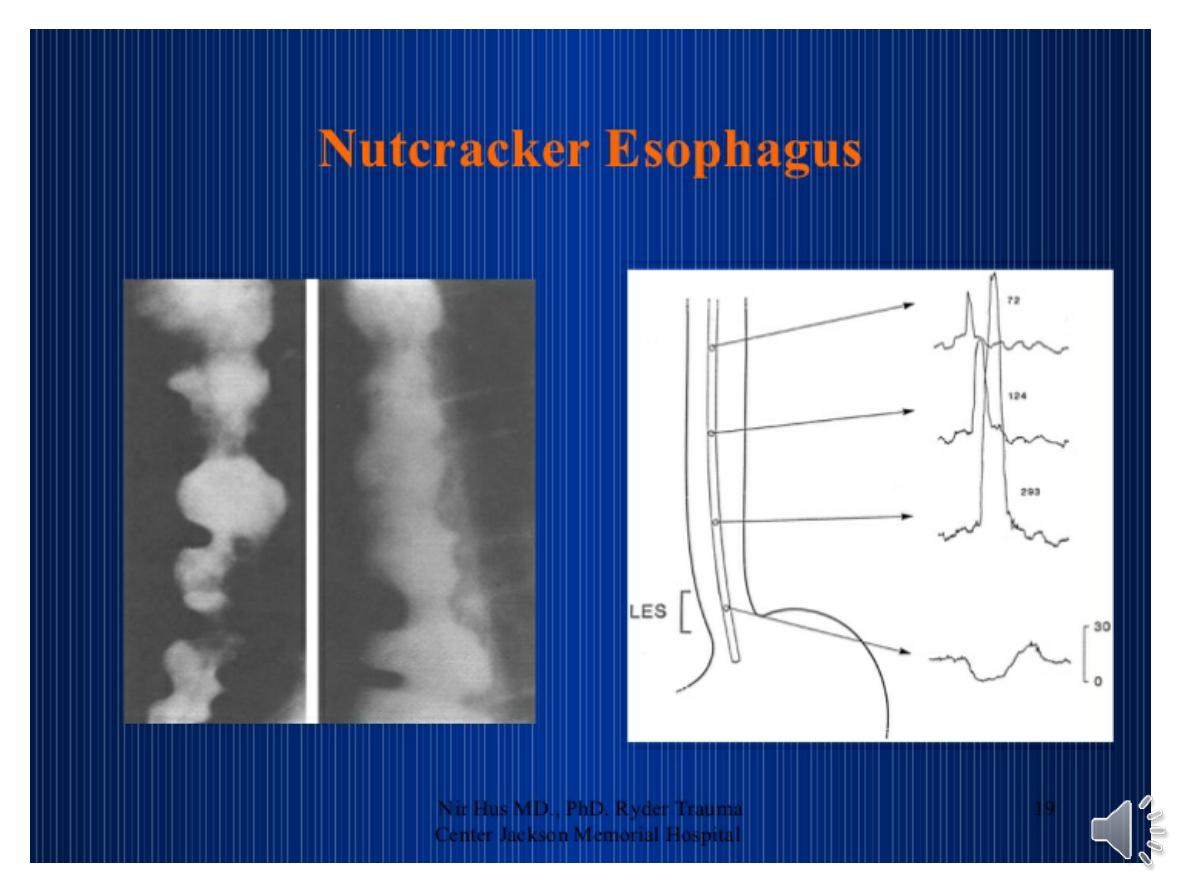
Nutcracker’ oesophagus
extremely forceful peristaltic activity
leads to episodic
chest pain
and
dysphagia
. Treatment is --
nitrates or
nifedipine
.
The patients are usually elderly.
Manometric abnormalities
, ranging
from poor peristalsis to spasm, occur.
Treatment is with
dilatation and/or
vasodilators for chest pain
.