Lec 4 GIT Dr.Hassan aljumaily
Oral cancer
CA esophagus
CA stomach &lymphoma
Colonic Polyps ,FAP& CA
colon
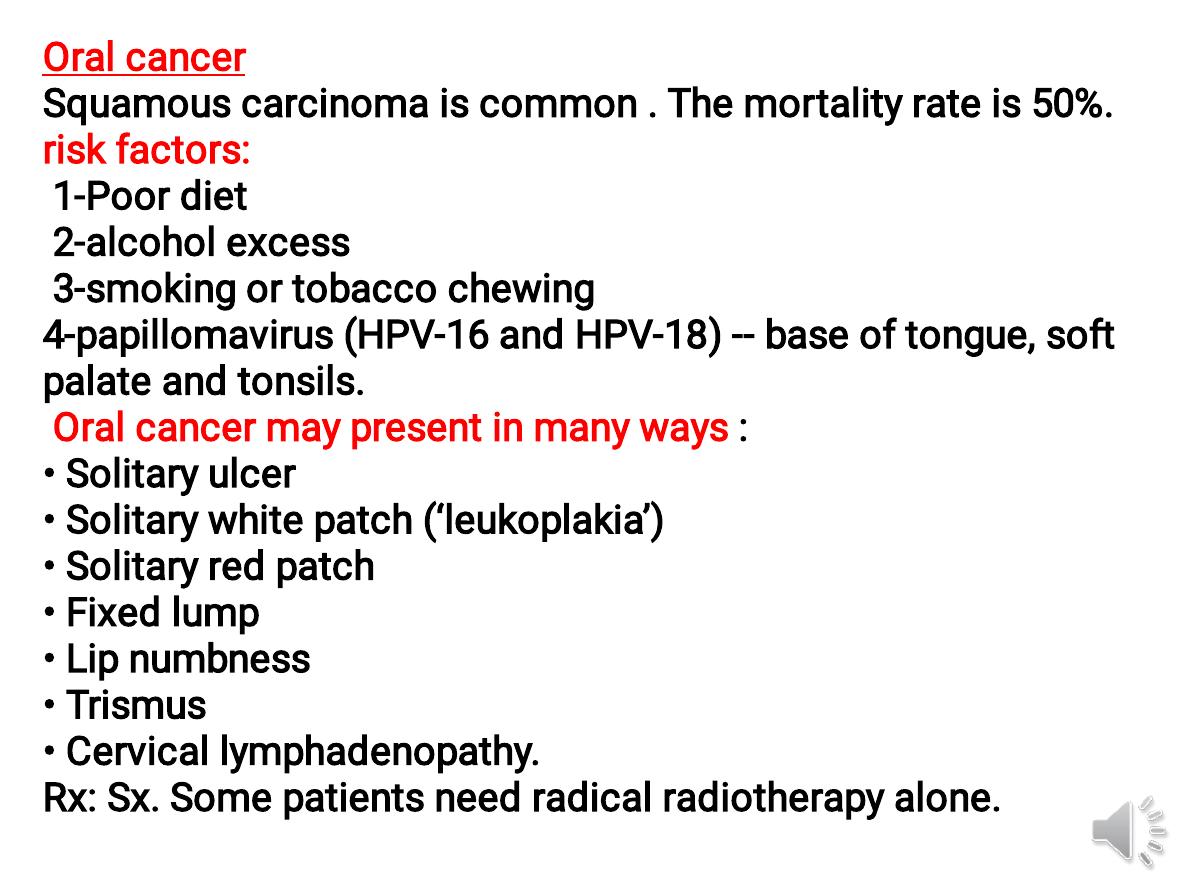
Oral cancer
Squamous carcinoma is common . The mortality rate is 50%.
risk factors:
1-Poor diet
2-alcohol excess
3-smoking or tobacco chewing
4-papillomavirus (HPV-16 and HPV-18) -- base of tongue, soft
palate and tonsils.
Oral cancer may present in many ways :
• Solitary ulcer
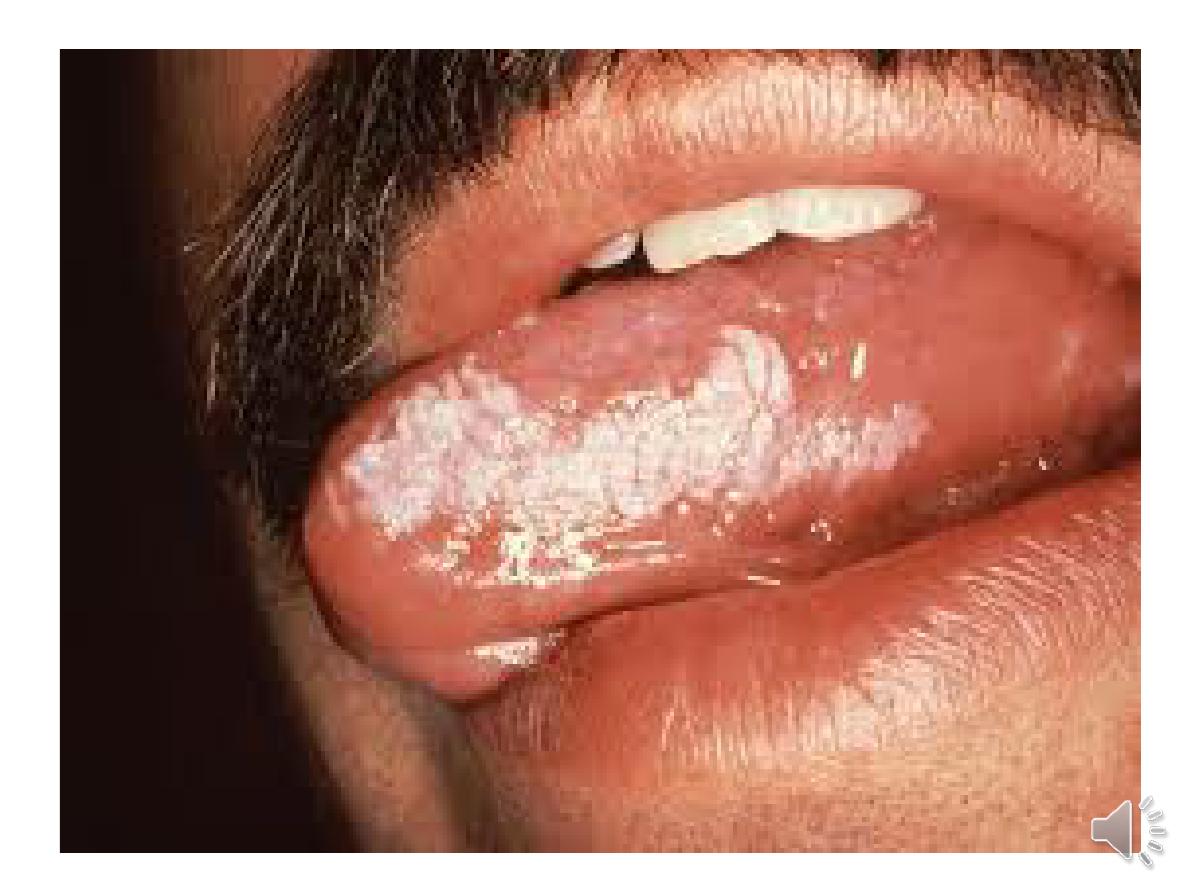
• Solitary white patch (‘leukoplakia’)
• Solitary red patch
• Fixed lump
• Lip numbness
• Trismus
• Cervical lymphadenopathy.
Rx: Sx. Some patients need radical radiotherapy alone.

Carcinoma of the oesophagus
aetiological factors
•
Smoking
• Alcohol excess
• Chewing betel nuts or tobacco
• Achalasia ,
Barrett
• Coeliac disease
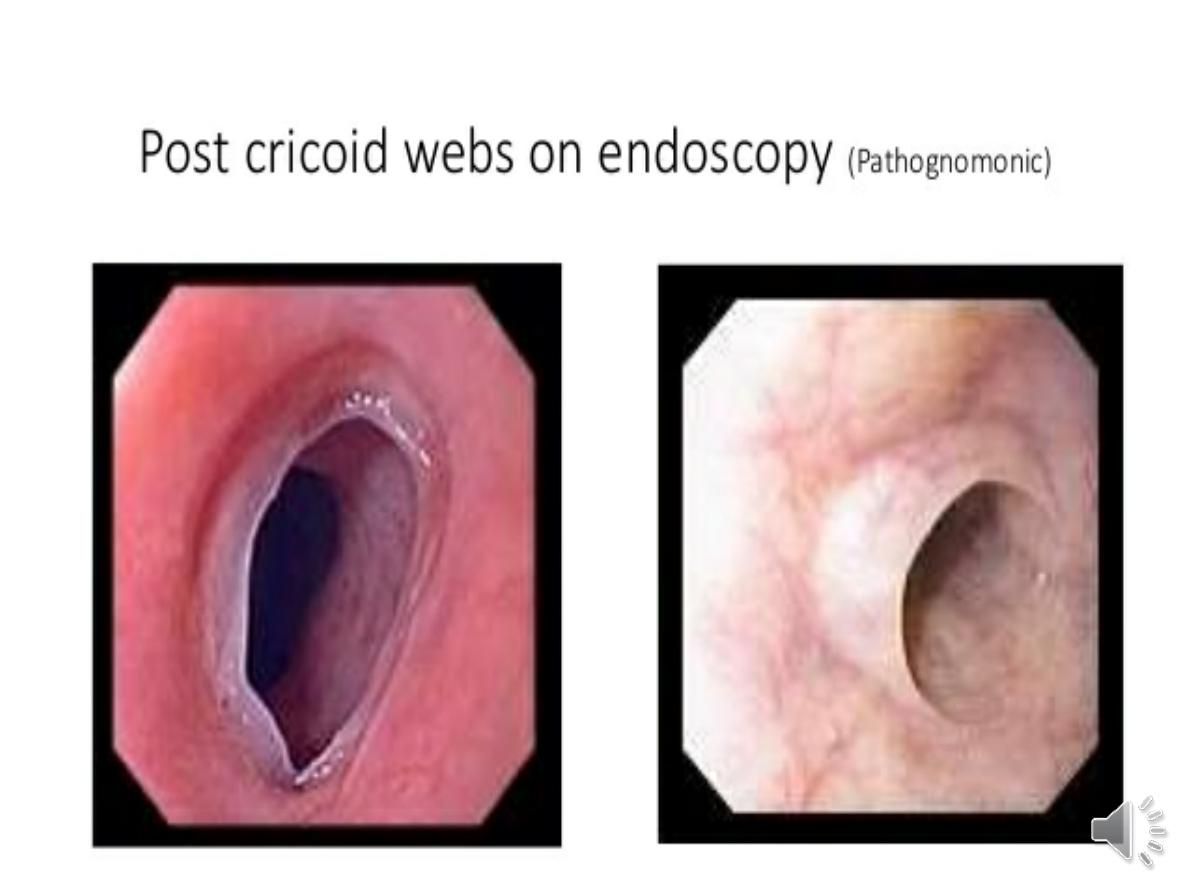
• Post-cricoid web
• Post-caustic stricture
• Tylosis
almost all tumours in the upper oesophagus are
squamous cancers. Adenocarcinomas typically arise
in the lower third of the oesophagus from Barrett’s
oesophagus. 5-year survival =13%.
Clinical features:
- dysphagia.
-In late stages, weight loss
-chest pain or hoarseness suggests mediastinal invasion.
- Fistulation between the oesophagus and the trachea--
coughing after swallowing.
- Physical signs may be absent or , cachexia, cervical LAP
Investigations
-OGD with biopsy.
-A barium swallow
-Thoracic and abdominal CT& PET--for metastatic spread and
local invasion.
- EUS : to determine the depth of penetration of the tumour
into the oesophageal.
These investigations will define the TNM stage of the disease .
Management
1-Sx
- Overall survival =30% at 5 years, but this
can be improved by neoadjuvant
chemotherapy.
2- squamous carcinomas are
radiosensitive
, radiotherapy alone is
associated with a 5-year survival of only
5%, but
combined chemoradiotherapy
achieve 5-year survival rates of 25–30%.
3- 70% of patients have
extensive
disease
--treatment is palliative
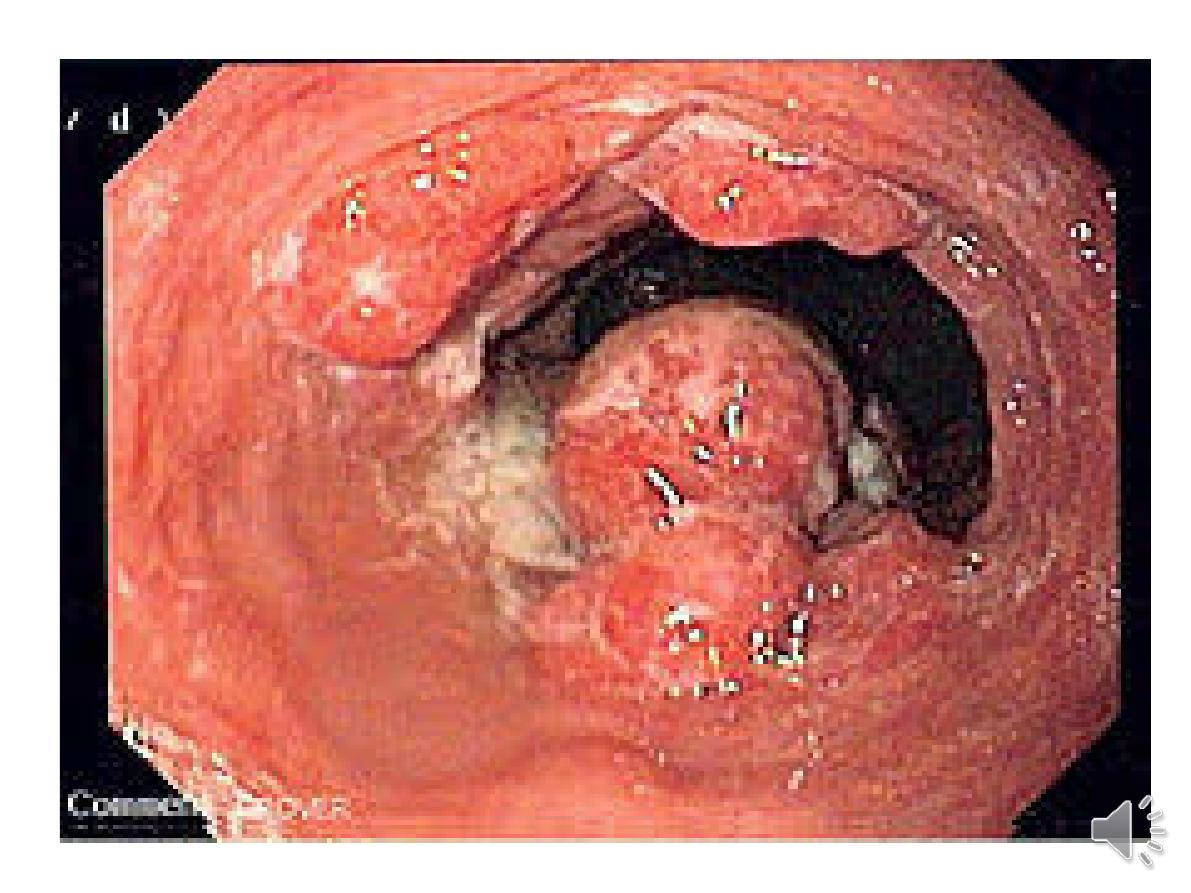
Gastric carcinoma
-fourth leading cause of cancer death.
-
50%
lower in women. In both sexes, it rises
sharply after 50 years of age. The overall
prognosis is poor, with
less than 30%
surviving 5 years,.
Pathophysiology
-Infection with
H. pylori
contribute to gastric
cancer in 60–70% of cases .
-
Diets
rich in salted, smoked foods and the
consumption of nitrites and nitrates may
increase cancer risk. Diets lacking fresh fruit
and vegetables, as well as vitamins C and A,
may also contribute
.
risk factors
•
H. pylori
• Smoking
• Alcohol
• Dietary associations
• Autoimmune gastritis (pernicious
anaemia)
• Adenomatous gastric polyps
• Previous partial gastrectomy (> 20 yrs)
• Hereditary diffuse gastric cancer
• FAP
.
-
cancer risk 2-3 fold in first-degree relatives of
patients, and links with blood group A
. Rarely,
gastric cancer may be inherited in an
AD
manner
in association with mutations of the
E-cadherin
(
CDH1
) gene.
-Virtually all tumours are adenocarcinomas.
-Cancers are either ‘intestinal’, arising from areas
of intestinal metaplasia with histological features
of intestinal epithelium, or ‘diffuse’, arising from
normal gastric tissue.
Diffuse submucosal infiltration by a scirrhous
cancer (
linitis plastica
) is uncommon.
Napoleon Bonaparte

Clinical features
-
asymptomatic
but may be discovered during
endoscopy for investigation of dyspepsia.
-2/3 with advanced cancers have
weight loss
and 50% have
ulcer-like pain
.
-
Anorexia and nausea
occur in 1/3
-
early satiety, haematemesis, melaena and
dyspepsia
alone are less common.
-
Dysphagia
occurs in tumours of the gastric
cardia which obstruct the gastro-oesophageal
junction.
-
Anaemia
from occult bleeding is also
common.
Examination:
- weight loss, anaemia and epigastric mass .
Jaundice or ascites signify metastatic spread.
-
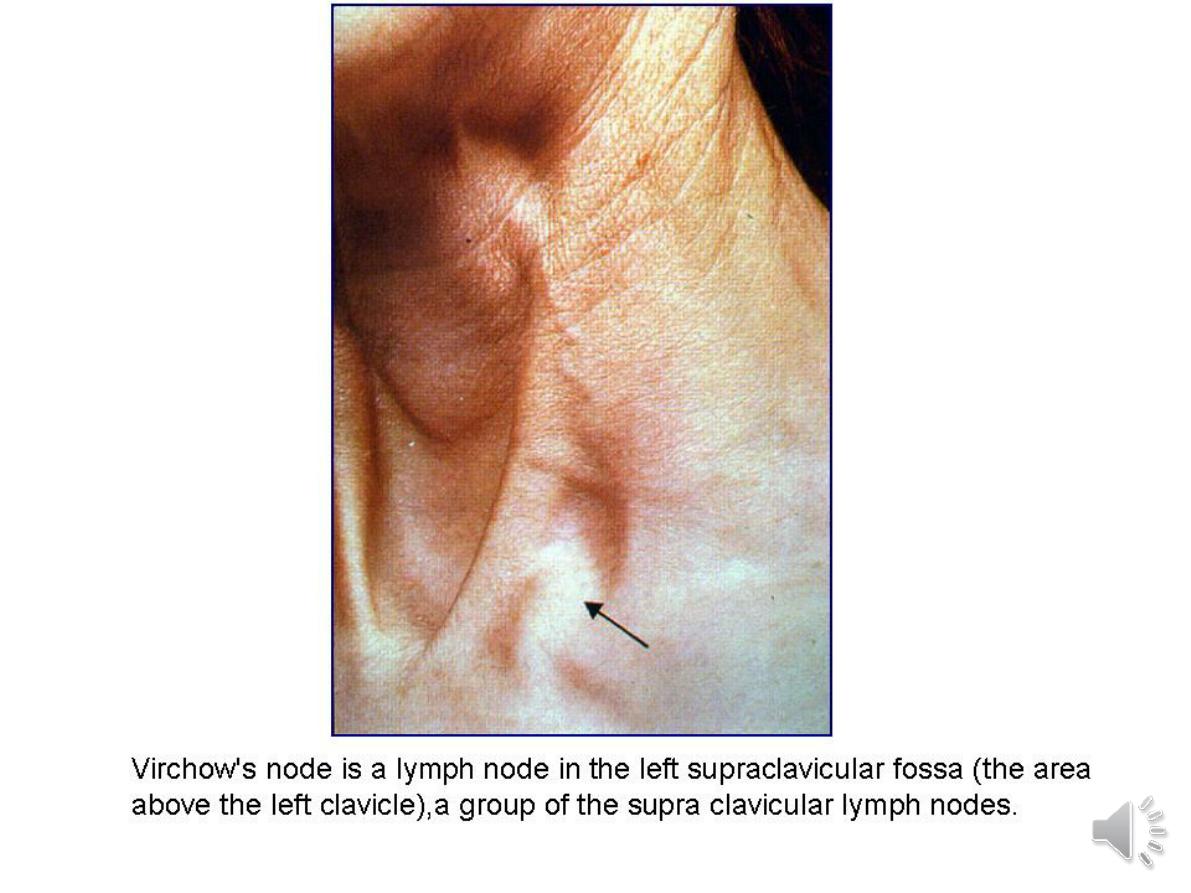
-supraclavicular lymph nodes
(Troisier’s sign
),
at umbilicus (
Sister Joseph’s nodule
) or
metastasis to ovaries (
Krukenberg tumour
).
-Paraneoplastic phenomena, such as
acanthosis nigricans,thrombophlebitis
(Trousseau’s sign).
-
Metastases arise most commonly in the liver,
lungs, peritoneum and bone marrow.




Investigations
1-
OGD
is the investigation of choice
‘alarm features’:
•
Weight loss
• Anaemia
• Vomiting
• Haematemesis and/or melaena
• Dysphagia
• Palpable abdominal mass
2-Barium meal
is a poor alternative .
3-CT
is necessary for staging & resectability.
4-laparoscopy
-detect peritoneal spread.

Management
Surgery
- cure, and this can be achieved in about
90%
of
patients with early gastric cancer.
-
Proximal tumours
involving the oesophago-gastric
junction also require a distal oesophagectomy.
-
Small, distally sited tumours
can be managed by a
partial gastrectomy with lymphadenectomy .
- complete removal of all macroscopic tumour
combined with lymphadenectomy will achieve a
50–60% 5-year survival.
Recent evidence suggests that perioperative
chemotherapy with epirubicin, cisplatin and fluorouracil
ECF) improves survival rates.
Gastric lymphoma
-less than
5
% of all gastric malignancies.
-
60%
of all primary gastrointestinal
lymphomas
-
H. pylori
infection is closely associated with
the development of a lowgrade lymphoma
Invex
: EUS ,OGD=ulcerating mass.
While initial treatment of low-grade lesions
confined to the superficial layers of the gastric
wall consists of
H. pylori
eradication
and close
observation, 25%
contain t(11 : 18)
chromosomal translocations
. In these cases,
additional radiotherapy or chemotherapy is
usually necessary.
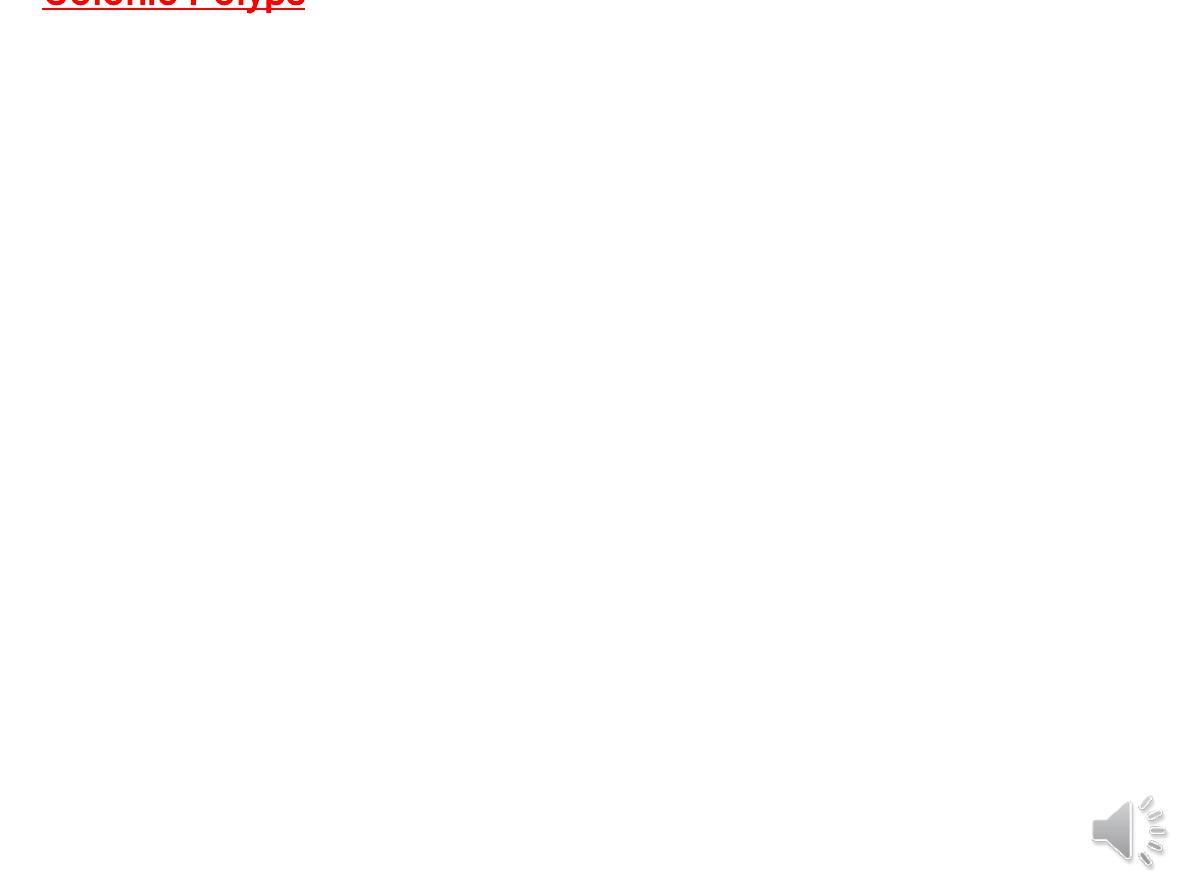
Colonic Polyps
Polyps may be neoplastic or non-neoplastic. The latter include
hamartomas, metaplastic (‘hyperplastic’) polyps and
inflammatory polyps. These have no malignant potential.
. Colorectal adenomas prevalence rises with age; 50% of
people over 60 years of age have adenomas. They are more
common in the rectum and distal colon .
all forms of colorectal carcinoma develop from adenomatous
polyps. Features associated with a higher risk of malignancy
are :
•
Large size (> 2 cm)
• Multiple polyps
• Villous architecture
• Dysplasia
Adenomas are usually asymptomatic and discovered
incidentally ,Or bleeding and anaemia. ..
Once all polyps have
been removed, surveillance colonoscopy should be
undertaken at 3–5-year intervals, as new polyps develop in
50% of patients.
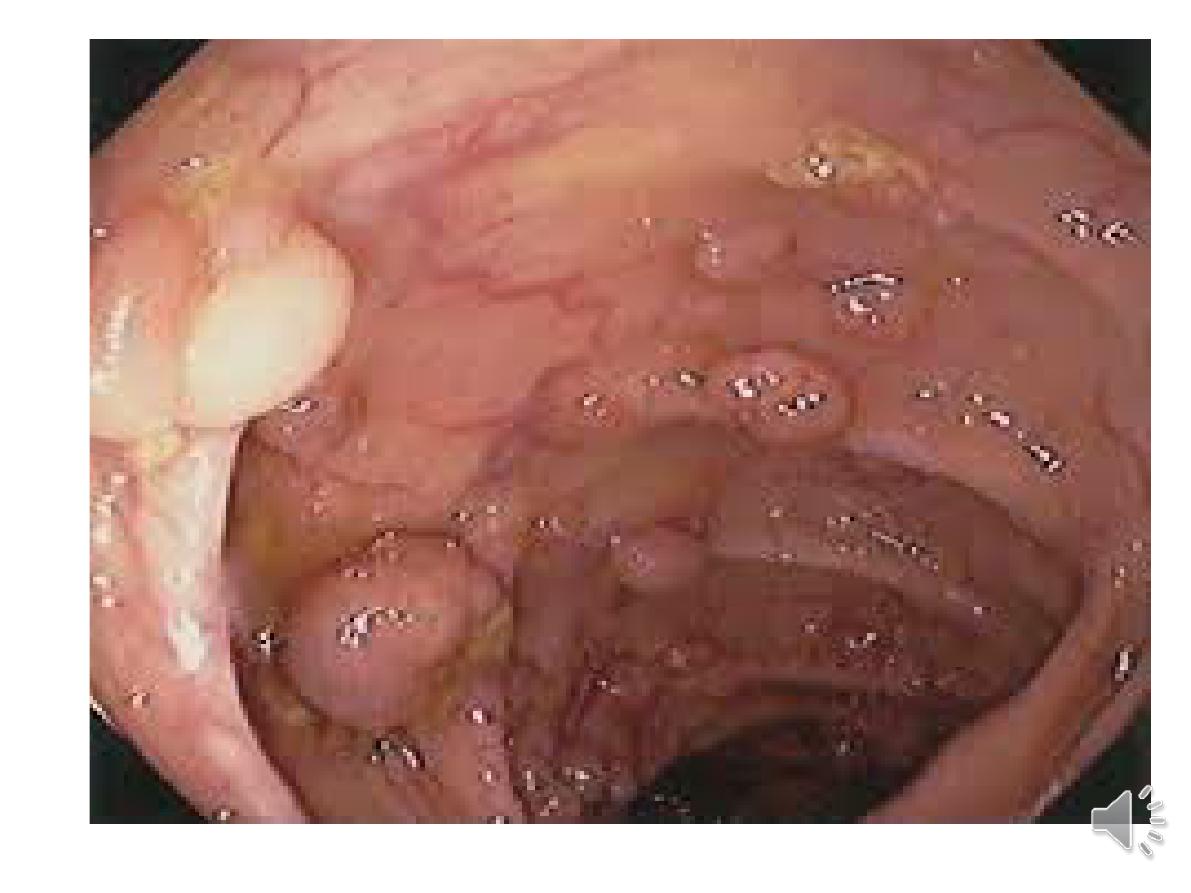
Familial adenomatous polyposis
- AD disorder
→1% of all colorectal cancers.
germline mutation of the tumour suppressor
APC
gene.
20%
of cases
→ have no family history.
-cancer will develop within
10–15 years
of the
appearance of adenomas and
90% of
patients will
develop colorectal cancer by the age of 50 years.
Despite surveillance, 25% with FAP have cancer by the
time they undergo colectomy.
-
Other polyps
in the stomach.
Duodenal adenomas
occur
in over 90% and are most common around the ampulla of
Vater.
Malignant transformation to adenocarcinoma
occurs in 10% and is the leading cause of death in those
who have had prophylactic colectomy
.


-
sometimes respond to hormonal therapy with
tamoxifen, and the NSAID sulindac may lead to
regression in some, by unknown mechanisms.
-
members should undergo mutation testing at
13–14 years of age and patients who are found
to have the mutation should be offered
colectomy after school or college education
has been completed. The operation of choice is
total proctocolectomy with ileal pouch–anal
anastomosis
.
Periodic OGD every 1–3 years to detect
duodenal and periampullary adenomas
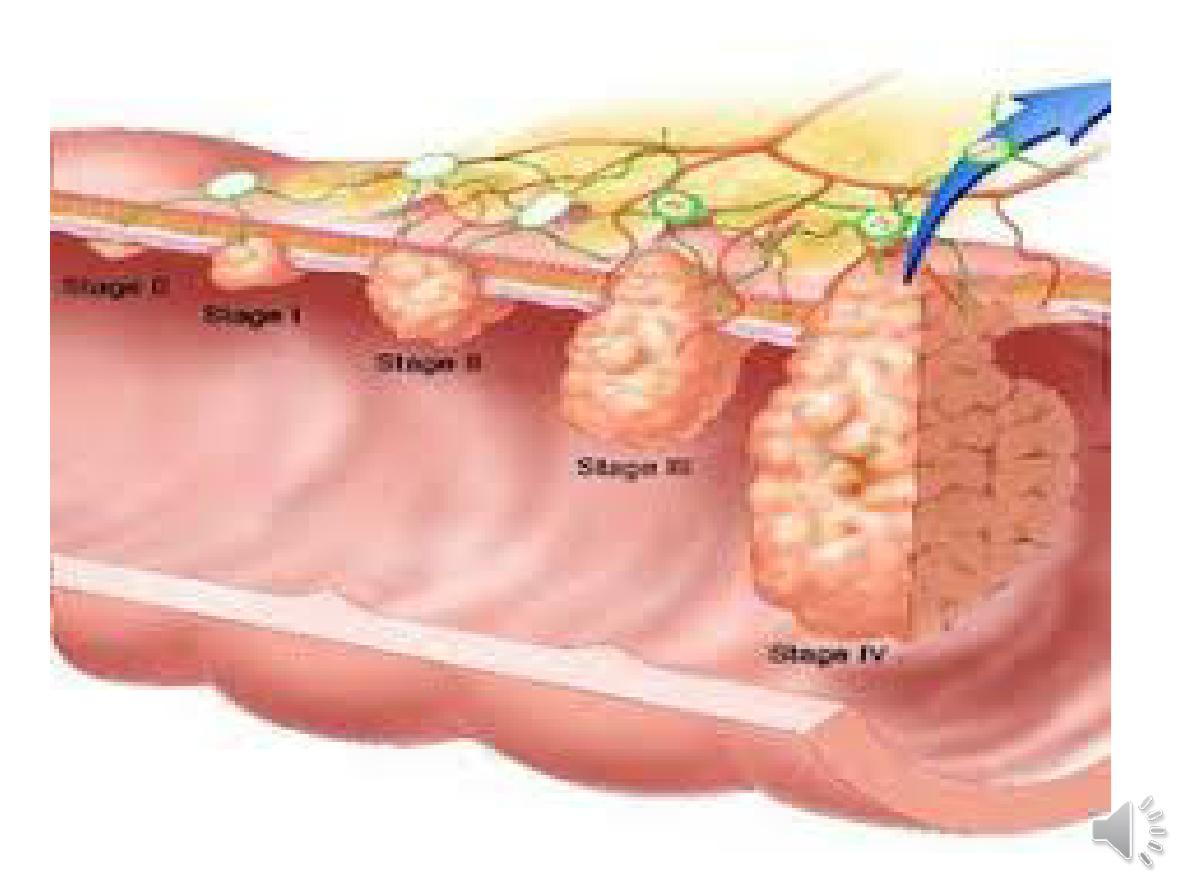
Colorectal cancer
common over the age of 50 years.
Pathophysiology
environmental and genetic & dietary factors
other:
Medical conditions
• Colorectal adenoma
• UC or Crohn’s colitis
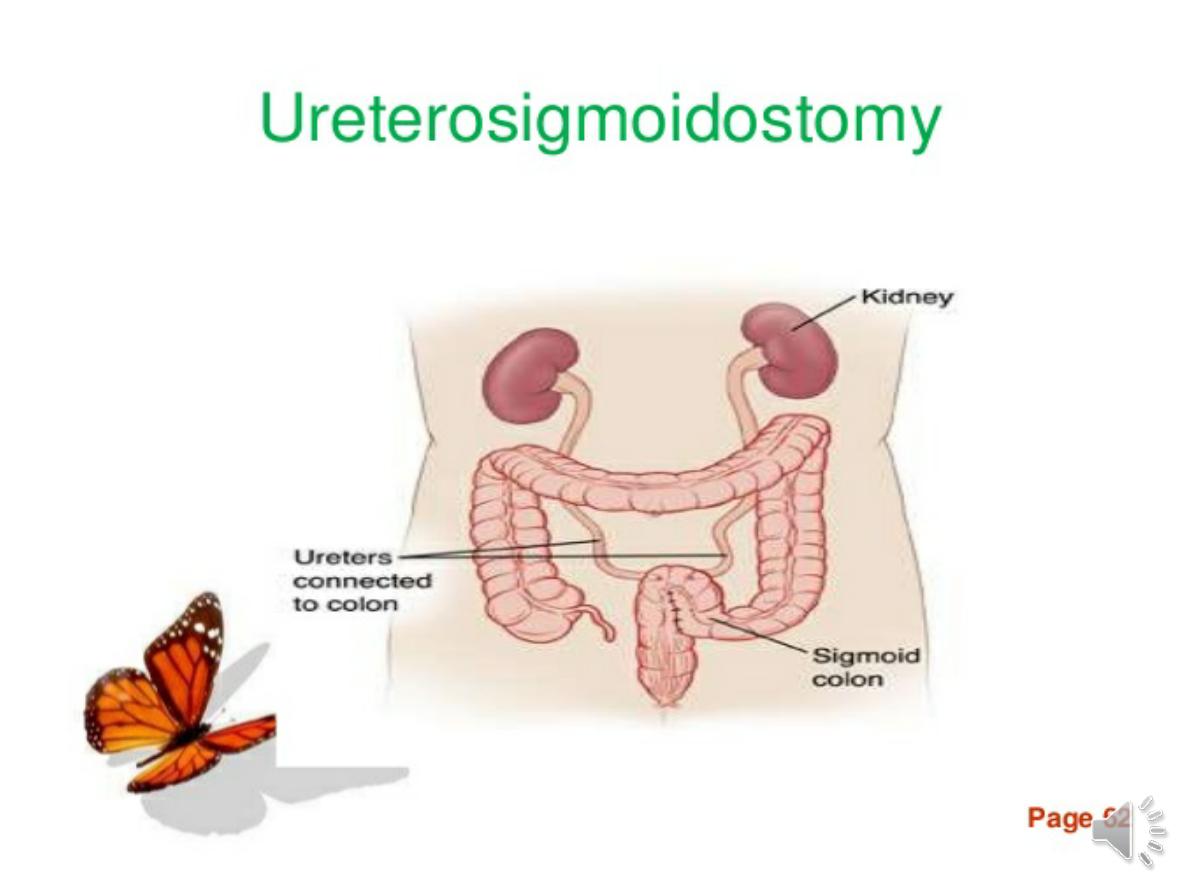
• Ureterosigmoidostomy
• Acromegaly
• Pelvic radiotherapy
Others
•
Obesity and sedentary lifestyle – may be related to diet
• Smoking
• Alcohol (weak association)
• Cholecystectomy (effect of bile acids in right colon)
• Type 2 DM (hyperinsulinaemia)
• Use of aspirin or NSAIDs and statins associated with
reduced
risk
.

-
About 5–10% of colon cancers are
caused by
hereditary non-polyposis
colon cancer
(HNPCC). AD , positive
family history of colon cancer occurring
at a young age.
Most tumors arise from malignant
transformation of a benign
adenomatous polyp
. 65%
→rectosigmoid ,
15%
→caecum or ascending colon.
Clinical features
-In left colon
, fresh rectal bleeding &obstruction.
-
In right colon
anaemia from occult bleeding or with
altered bowel habit, but obstruction is a late feature.
Colicky lower abdominal pain
is present in 2/3 of
patients and
rectal bleeding occurs in 50%
.
. Carcinoma of the rectum usually causes early
bleeding, mucus discharge or a feeling of incomplete
emptying.
Between 10 and 20% of patients present
with iron deficiency anaemia or weight loss.
On examination, there may be a palpable mass, signs
of anaemia or hepatomegaly from metastases. Low
rectal tumours may be palpable on digital examination
.
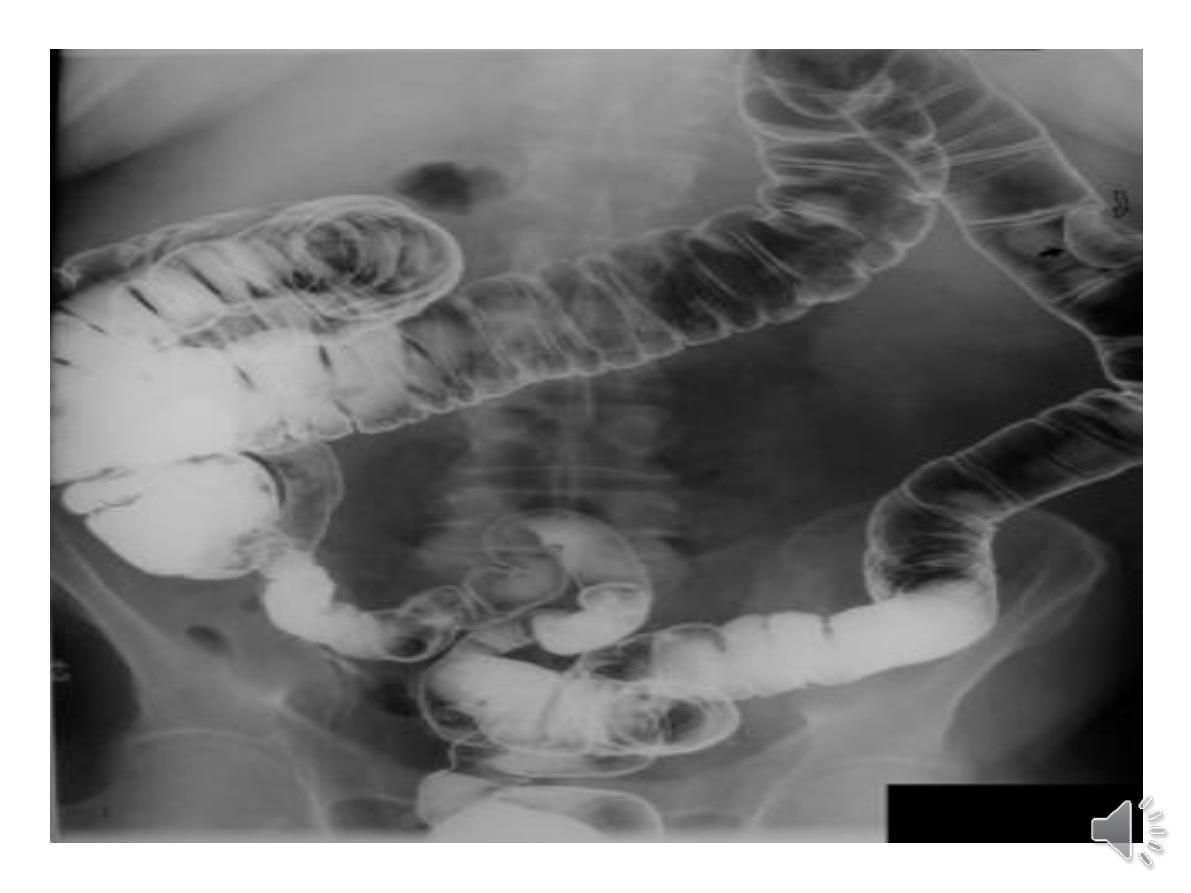
Investigations
1-
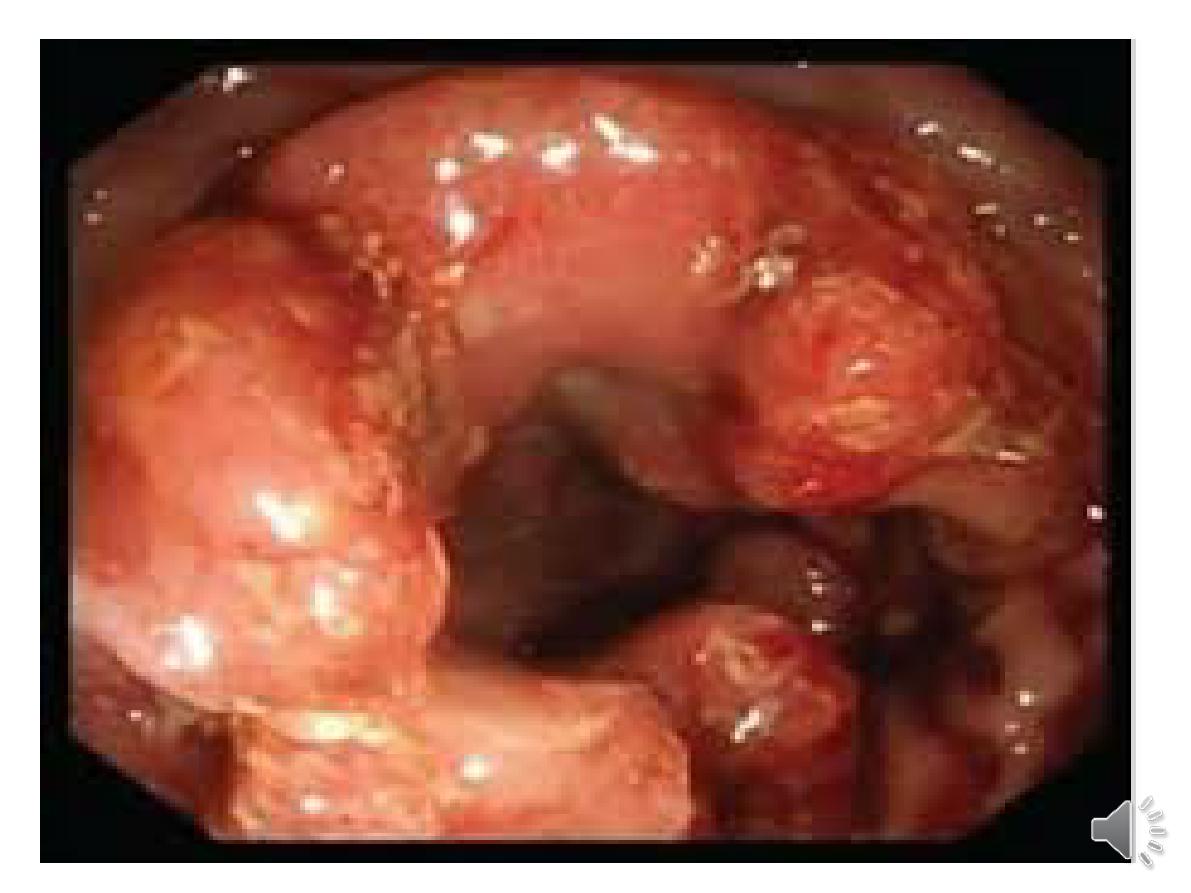
Colonoscopy
is sensitive and specific
than
barium enema
2- Patients in whom colonoscopy is
incomplete and those who are at high
risk of complications
→
CT colonography
.
This is a sensitive and non-invasive
technique for diagnosing tumours and
polyps of more than 6 mm diameter.
3-
CEA.
Surgery:
1-locally advanced rectal cancer should be
offered neoadjuvant radiotherapy or
chemoradiotherapy to increase the
subsequent chance of a complete surgical
resection
.
2-Carcinomas within 2 cm of the anal verge
may require abdominoperineal resection and
formation of a colostomy
.
3-Post-operatively, patients should undergo
colonoscopy after 6–12 months and then at 5
years to search for local recurrence or
development of new lesions, which occur in
6% of cases..
Prevention and screening :
Secondary
prevention aims to detect and remove lesions
at an early or pre-malignant stage.
1• people over the age of 50 years screened by
regular
faecal occult blood (FOB)
testing
reduces colorectal cancer mortality
2•
Colonoscopy
remains the gold standard but
is expensive and carries risks.
3•
Flexible sigmoidoscopy
is an alternative
option and has been shown to reduce overall
colorectal cancer mortality by approximately
35% .
