
ACUTE DIABETIC
COMPLICATIONS
1
-
hypoglycemia(COMMON)
2-DKA(COMMON)
3-hyperosmolar hyperglycemia(LESS COMMON)
4-lactic acidosis(VERY RARE
)
HYPOGLYCEMIA
GLODEN RULES
1
-
NO
CHART=
NO
TREATMENT
2
-
D
=DIRECT OBSERVATION BY YOURSELF
3
-
K
=KIND REDUCTION OF GLUCOSE
4
-
A
=ALWAYS RECHEK
5
-ADMITION IS
MUST
6
-I.V
N/S
IS THE MOST IMPORTANT
7
-ANTIBIOTIC COVER IF INFECTION
SUSPECTED
8
-I.V SOD.BICRAB
RARELY NEEDED
ONLY IF SEVER
ACIDOSIS

9
-K REPLACEMENT DONE
ONLY IF
=GOOD
U.O.P
+
URINE CATHETER PLACED
+
SLOW I.V
INFUSION
+
EVIDENCE OF HYPOK.BY ECG
OR
LAB
10-
DON’T
DISCHAGE BEFOR
48H
11
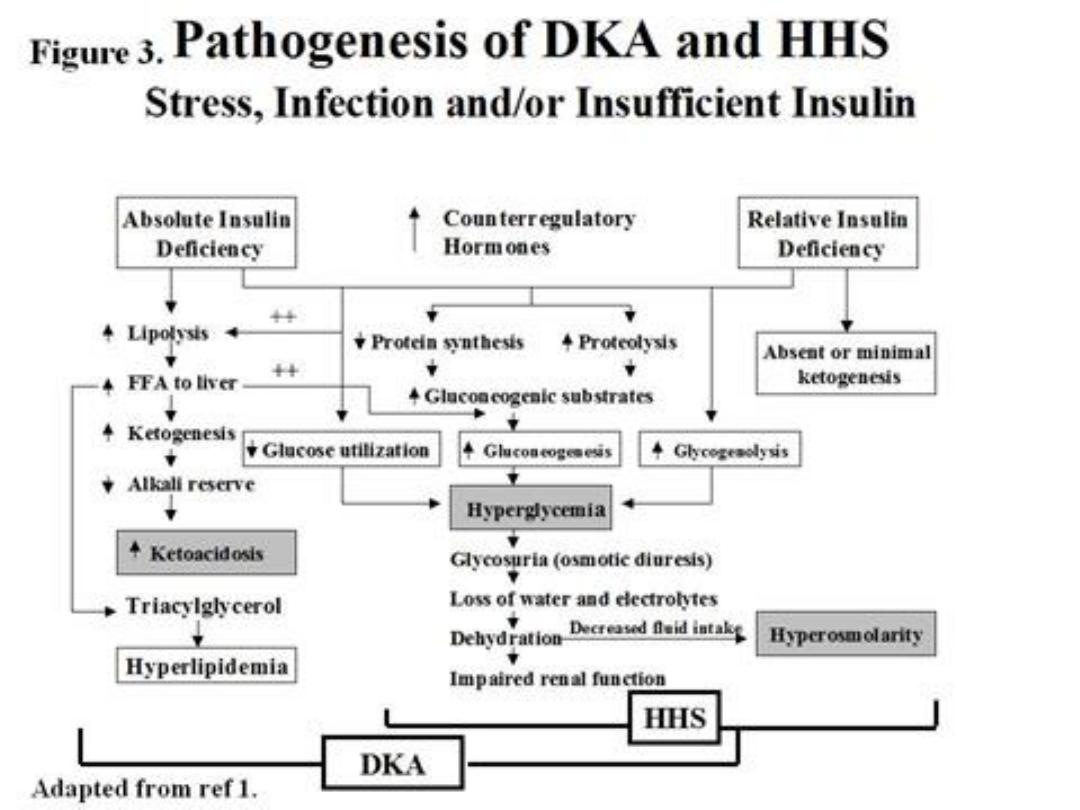
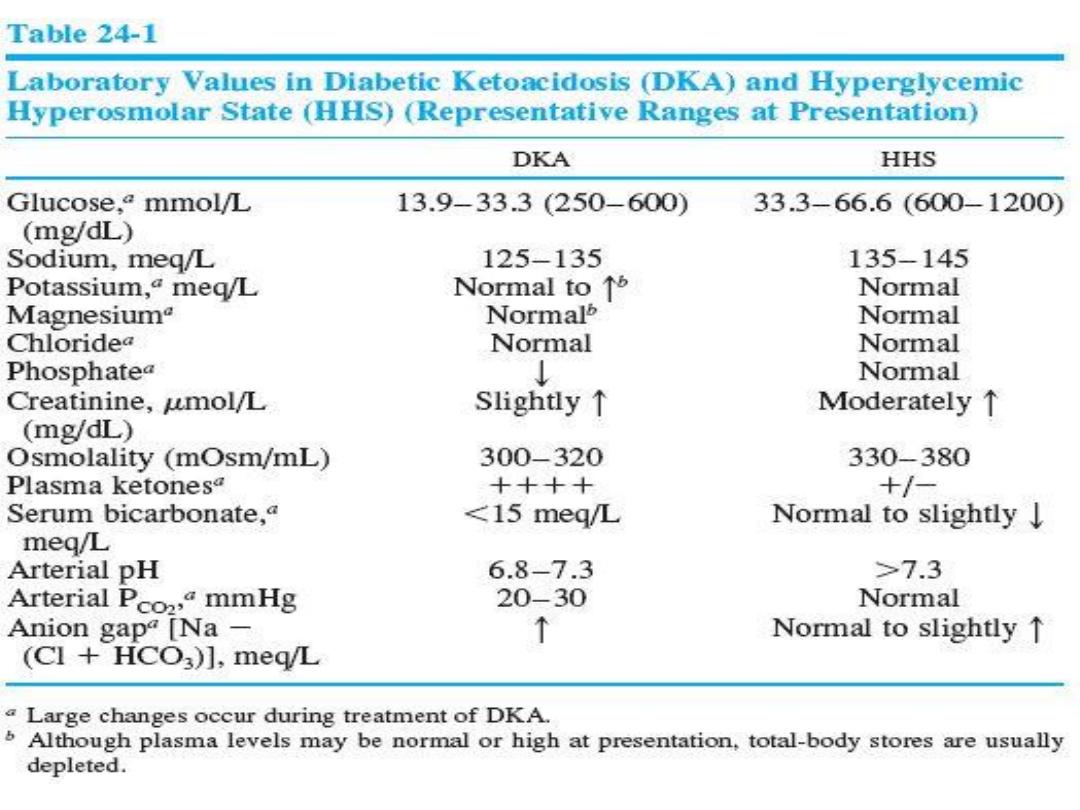
-HHS DIFFER FROM DKA IN=
NO
SIGNIFICANT
KETONEURIA
OR
ACIDOSIS
+
SEVER
HYPERGLYCEMIA
+
MORE
DEHYDRATION
+
MORE
THROMBOSIS
+
MORE
SENSITIVE TO
INSULIN
+
0,45
N/S IS NEEDED
12
-DKA PATIENT MAY WALK TO THE E,R

13
-DKA OCCURE
MAINLY
IN TYPE 1
RARELY
IN
TYPE2…HHS
ONLY
IN TYPE 2
14
-MORTALITY OF DKA=
5-10
%...HHS=
40
%
25
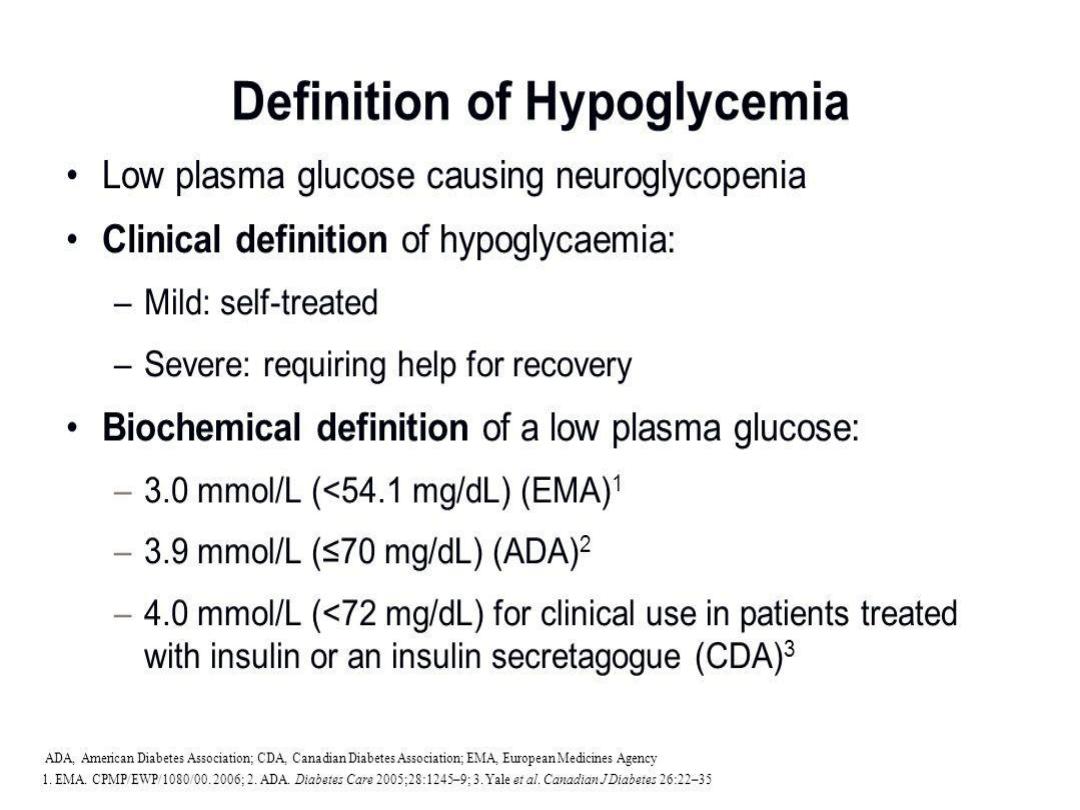
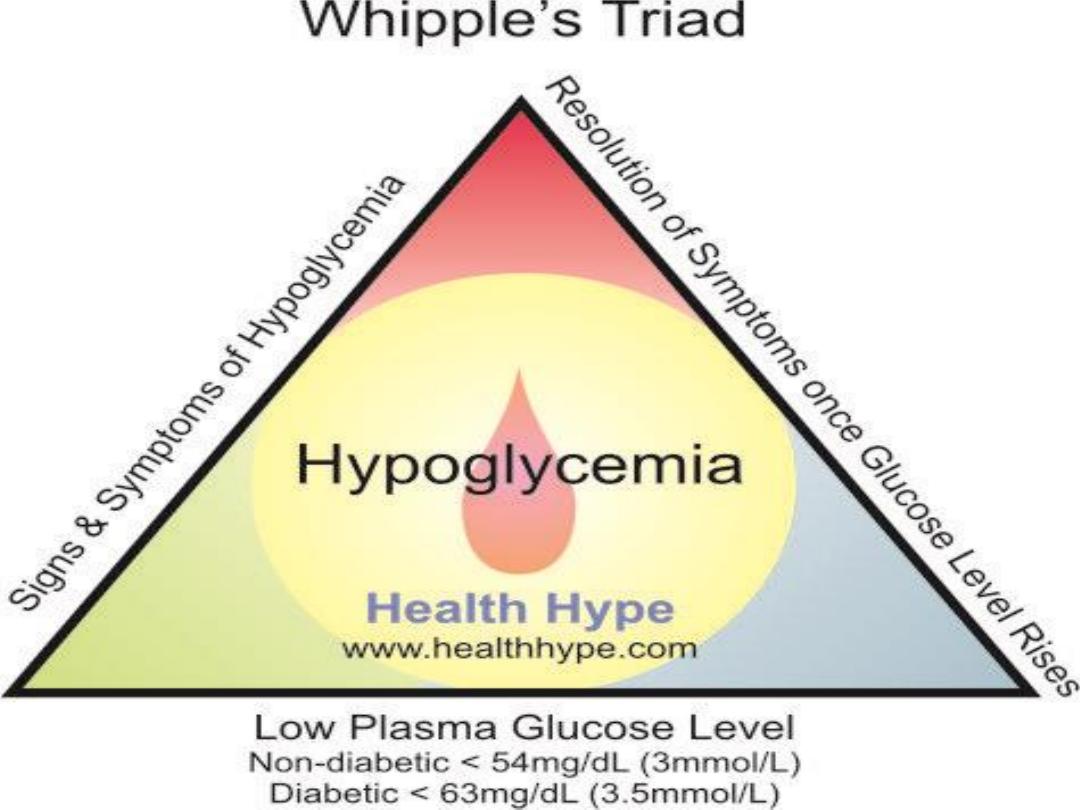
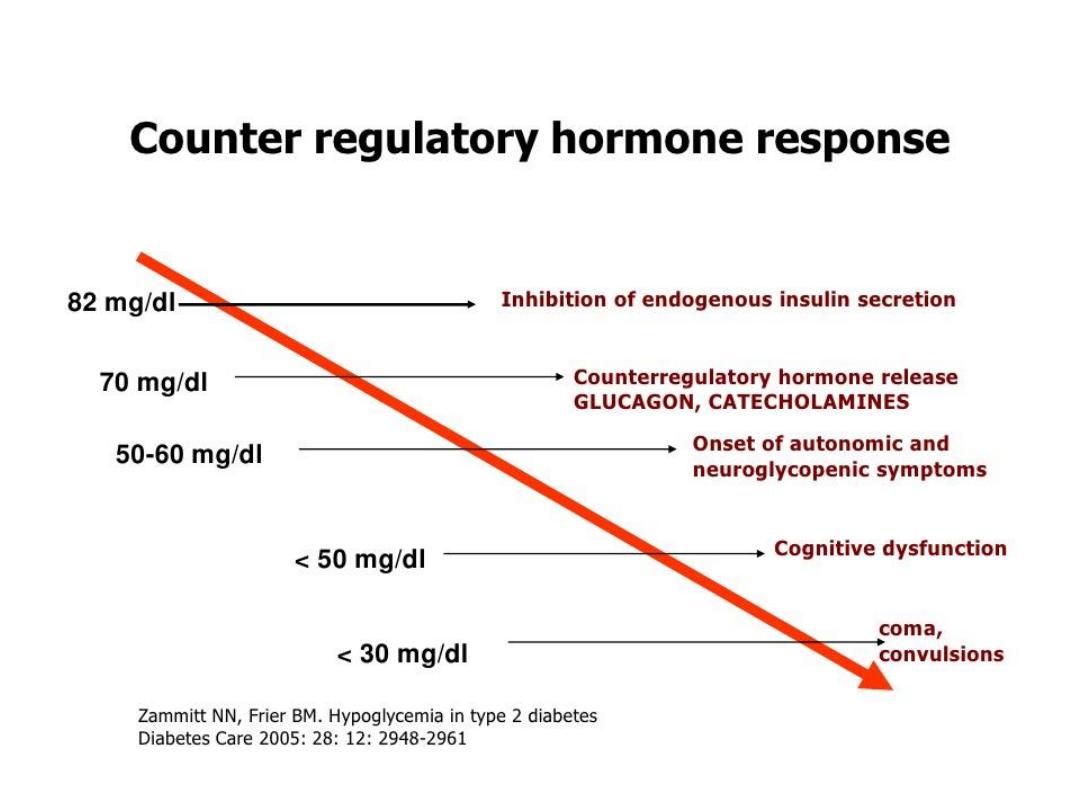
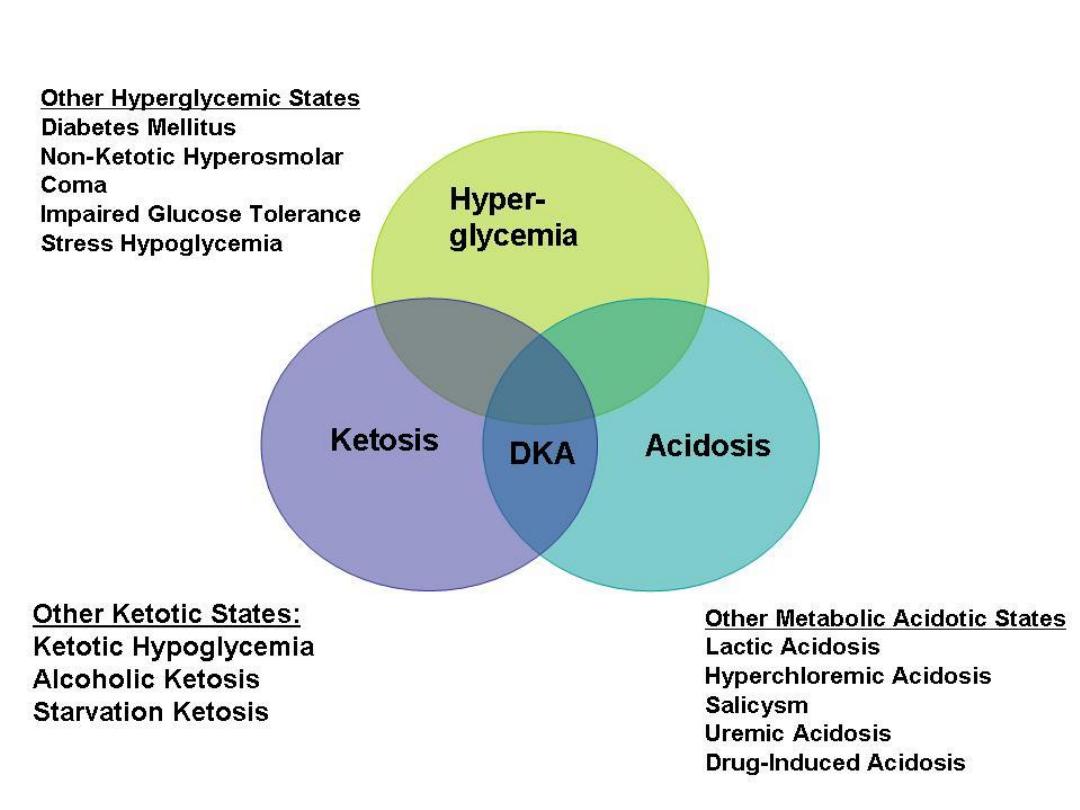
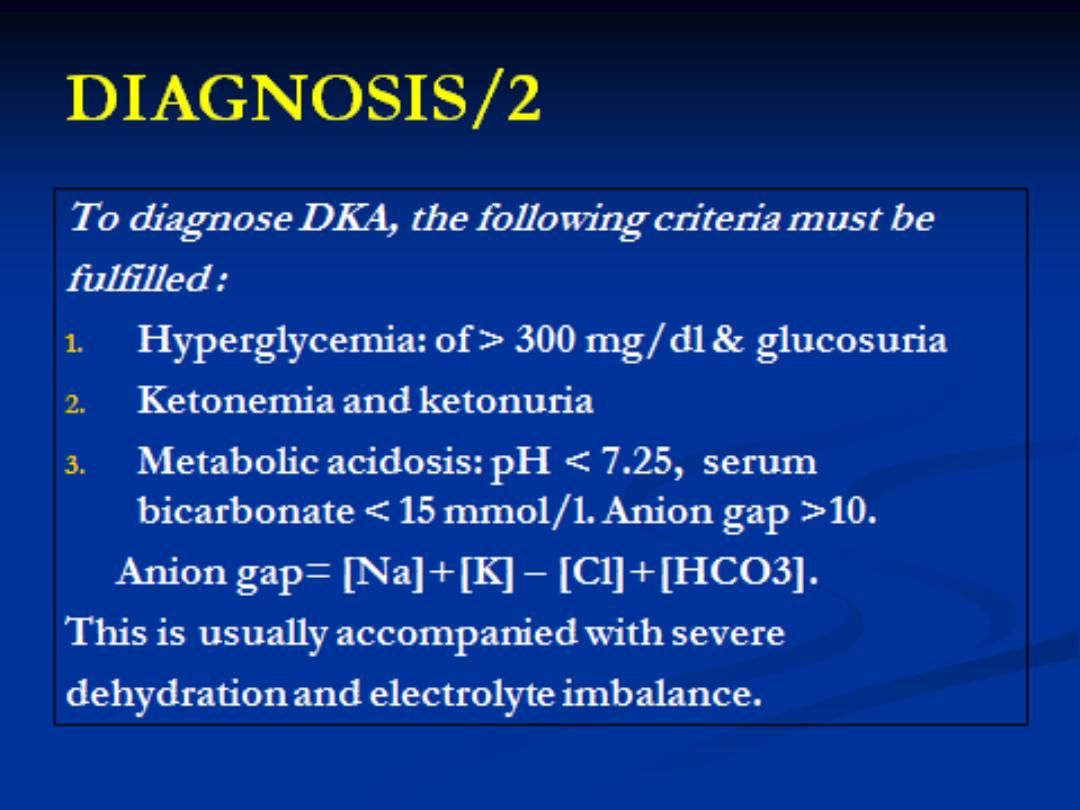
DEFINITION
Exact definition is variable
Most consistent is:
Blood glucose level greater than
250
mg/dL
Bicarbonate less than
15
mEq/L
Arterial pH less than
7.3
Moderate ketonemia

31
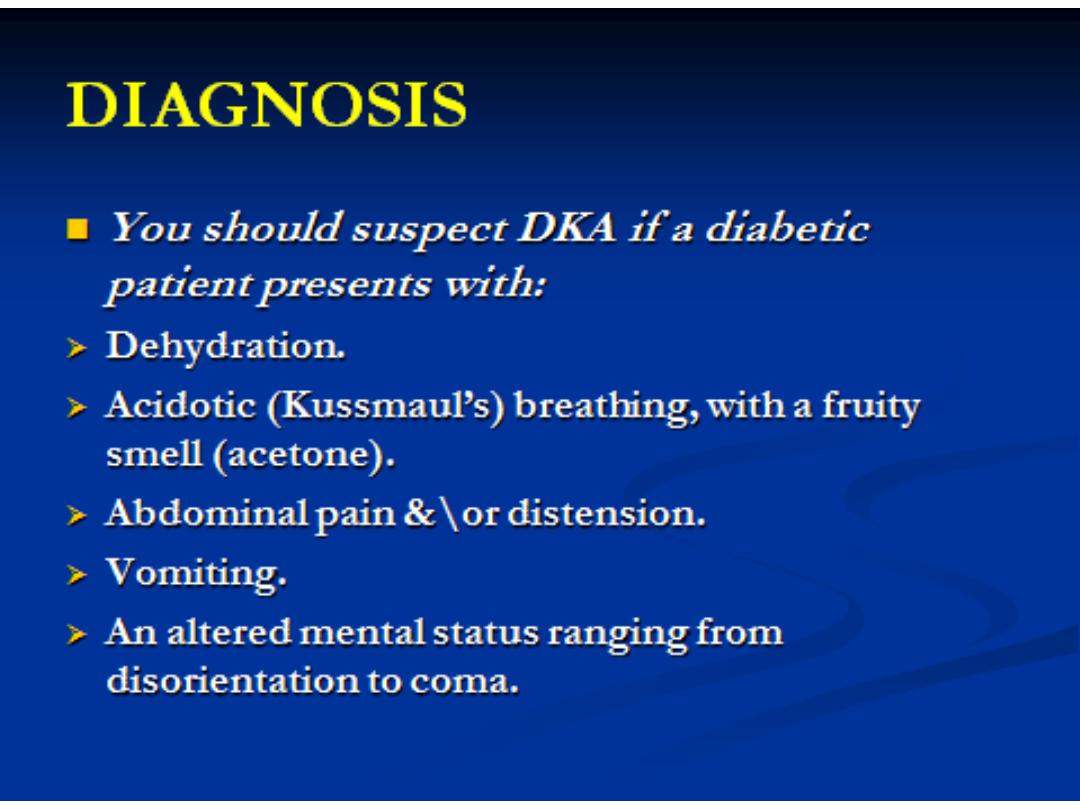
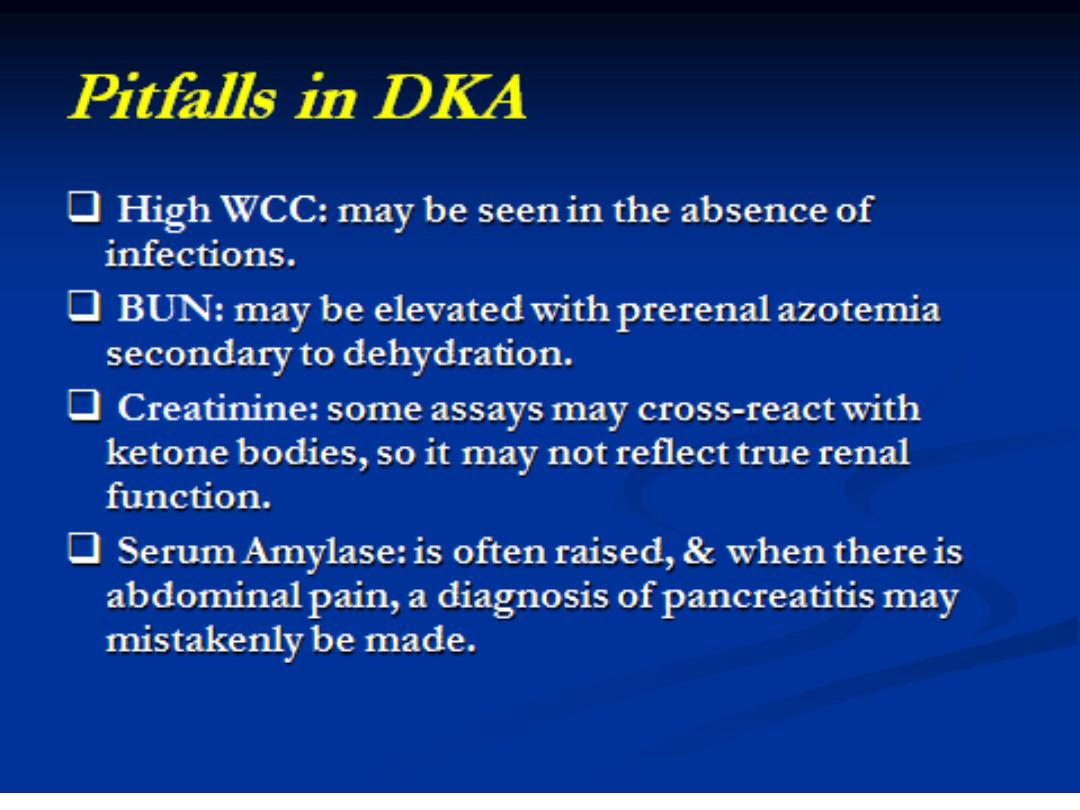
Acetone presents with odor in some patients
Absence of fever does not exclude infection as a
source of the ketoacidosis
Hypothermia may occur due to peripheral
vasodilatation
Abdominal pain and tenderness may occur with
gastric distension, ileus or pancreatitis
Abdominal pain and elevated amylase in those with
DKA or pancreatitis may make differentiation difficult
Lipase is more specific to pancreatitis

32
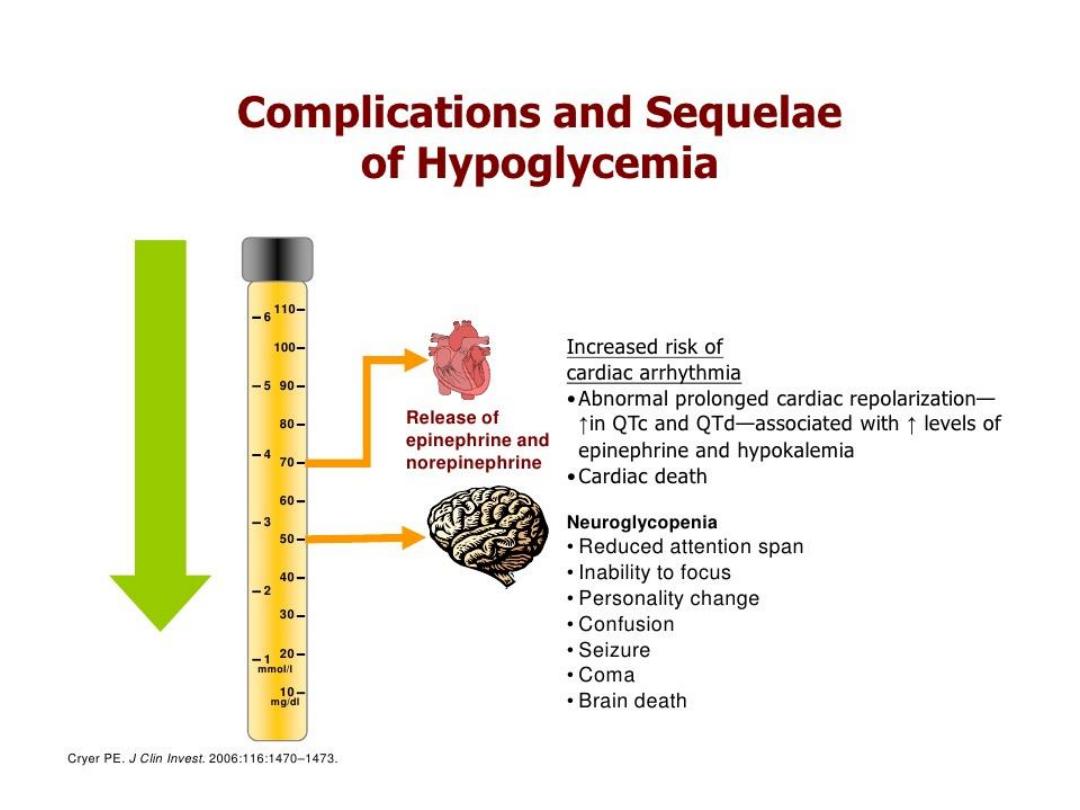
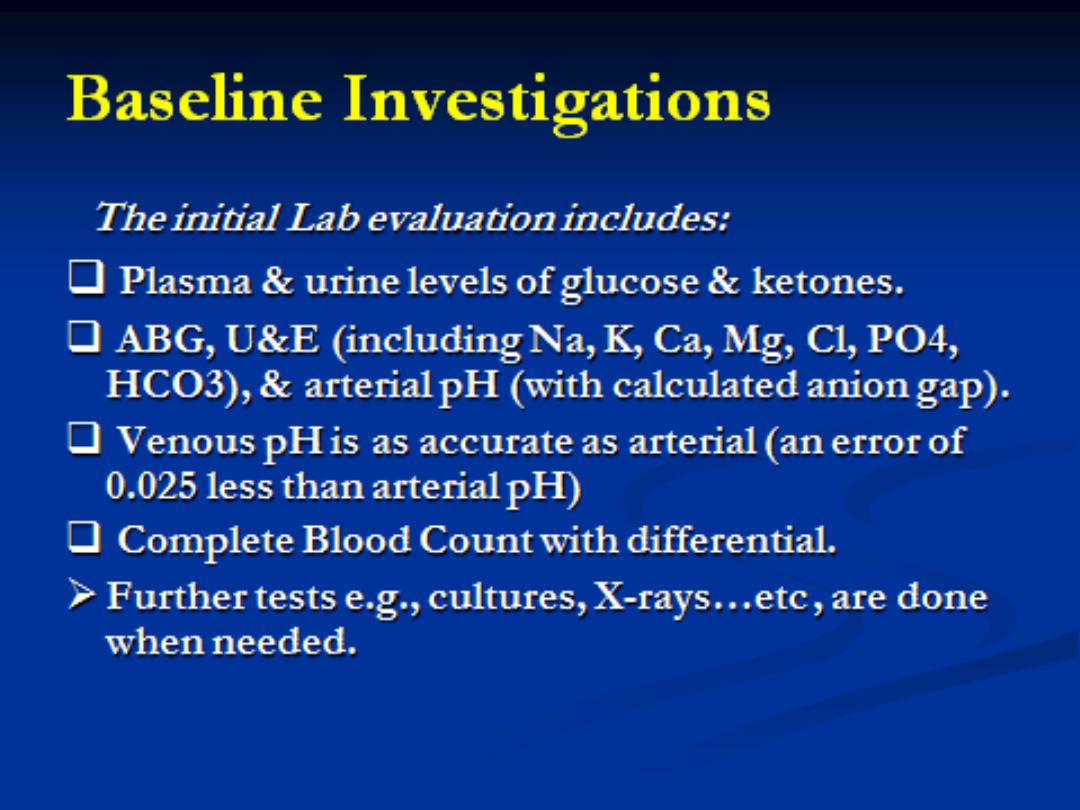
ECG CHANGES
Underlying rhythm is sinus tachycardia
Changes of hypo/hyperkalemia
Transient changes due to rapidly changing metabolic
status
Evaluate for ischemia because MI may precipitate DKA

33
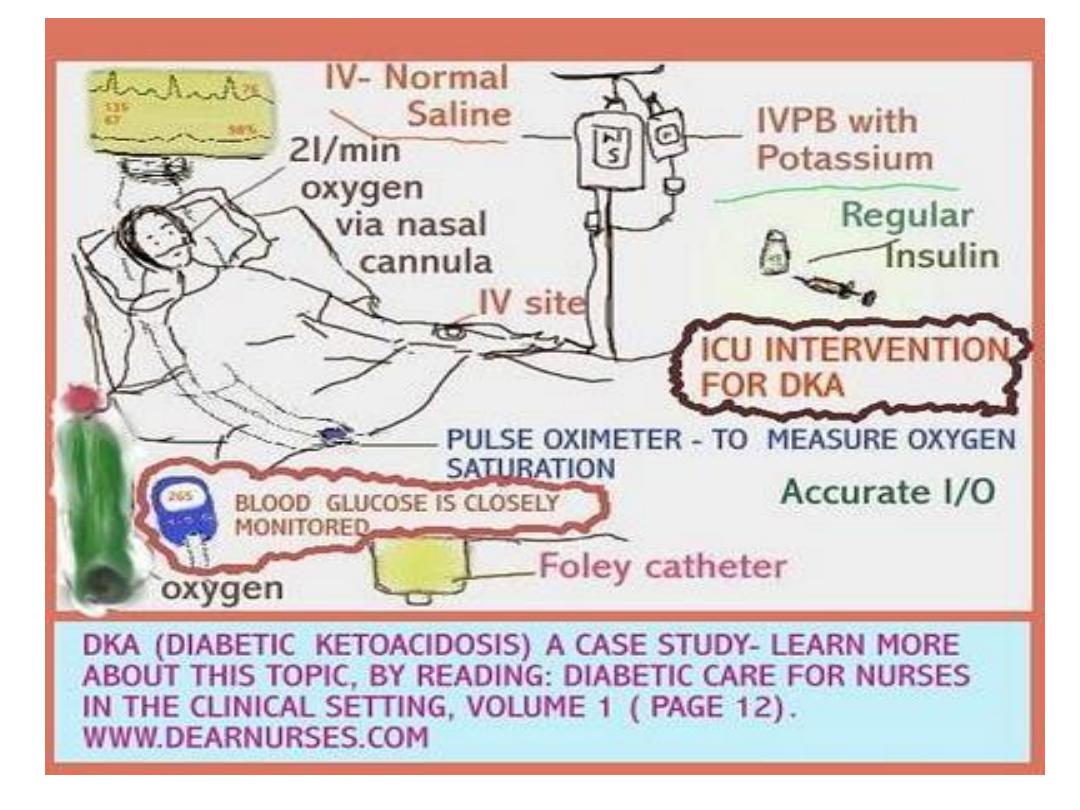
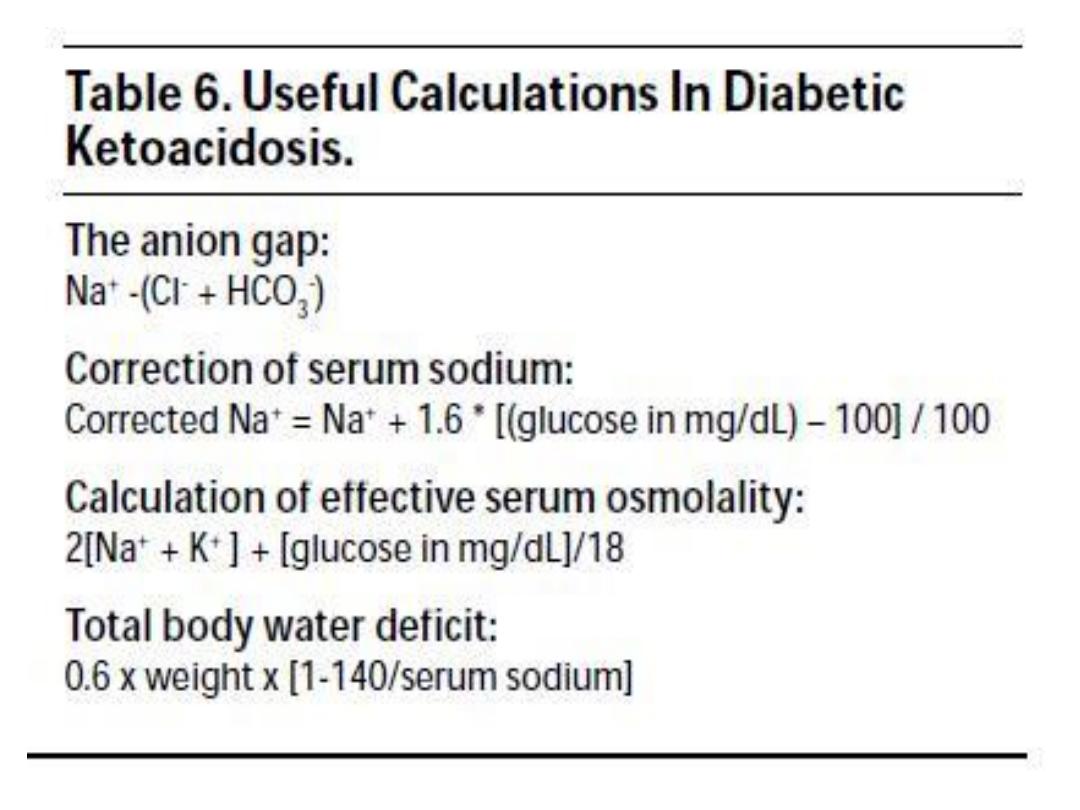
TREATMENT
Order of therapeutic priorities is volume first, then insulin and/or
potassium, magnesium and bicarbonate
Monitor glucose, potassium and anion gap, vital signs, level of
consciousness, volume input/output until recovery is well
established
Need frequent monitoring of electrolytes (every 1-2 hours) to meet
goals of safely replacing deficits and supplying missing insulin
Resolving hyperglycemia alone is not the end point of therapy
Need resolution of the metabolic acidosis or inhibition of ketoacid
production to signify resolution of DKA
Normalization of anion gap requires 8-16 hours and reflects clearance of
ketoacids
34
FLUID ADMINISTRATION
Rapid administration is single most important step in treatment
Restores:
Intravascular volume
Normal tonicity
Perfusion of vital organs
Improve glomerular filtration rate
Lower serum glucose and ketone levels
Average adult patient has a 100 ml/Kg (5-10 L) water deficit and a
sodium deficit of 7-10 mEq/kg
Normal saline is most frequently recommended fluid for initial
volume repletion

35
Recommended regimen:
First L of NS within first 30 minutes of presentation
First 2 L of NS within first 2 hours
Second 2 L of NS at 2-6 hours
Third 2 L of NS at 6-12 hours
Above replaces 50% of water deficit within first 12
hours with remaining 50% over next 12 hours
Glucose and ketone concentrations begin to fall
with fluids alone

36
Add D
5
to solution when glucose level is
between 250-300 mg/dL
Change to hypotonic ½ NS or D
5
½ NS if
glucose below 300 mg/dL after initially
using NS
If no extreme volume depletion, may
manage with 500 ml/hr for 4 hours
May need to monitor CVP or wedge pressure in
the elderly or those with heart disease and may
risk ARDS and cerebral edema
37
INSULIN
Recommended dose is 0.1 unit/kg/hr
Effect begins almost immediately after initiation
of infusion
Loading dose not necessary and not
recommended in children
38
POTASSIUM
Patients usually with profound total body hypokalemia
3-5 mEq/kg deficient
Created by insulin deficiency, metabolic acidosis, osmotic diuresis,
vomiting
2% of total body potassium is intravascular
Initial serum level is normal or high due to:
Intracellular exchange of potassium for hydrogen ions during acidosis
Total body fluid deficit
Diminished renal function
Initial hypokalemia indicates severe total-body potassium depletion and
requires large amounts of potassium within first 24-36 hours

39
During initial therapy the serum potassium
concentration may fall rapidly due to:
Action of insulin promoting reentry into cells
Dilution of extracellular fluid
Correction of acidosis
Increased urinary loss of potassium
Early potassium replacement is a standard modality
of care
Not given in first L of NS as severe hyperkalemia may
precipitate fatal ventricular tachycardia and ventricular
fibrillation

40
Fluid and insulin therapy
alone
usually lowers the
potassium level rapidly
For each 0.1 change in pH, serum potassium
concentration changes by 0.5 mEq/L inversely
Goal is to maintain potassium level within
4-5
mEq/L and avoid life threatening
hyper/hypokalemia
Oral
potassium is
safe and effective
and should be
used as soon as patient can tolerate po fluids
During
first 24 hours
, KCl
100-200 mEq
usually is
required
41
COMPLICATIONS AND MORTALITY
Complications related to acute disease
Main contributors to mortality are MI and infection
Old age, severe hypotension, prolonged and severe
coma and underlying renal and cardiovascular
disease
Severe volume depletion leaves elderly at risk for
vascular stasis and DVT
Airway protection for critically ill and lethargic patients
at risk for aspiration
42
COMPLICATIONS RELATED TO THERAPY
Hypoglycemia
Hypophosphatemia
ARDS
Cerebral edema
43
COMPLICATIONS RELATED TO THERAPY
Cerebral edema
Occurs between 4 and 12 hours after onset of therapy but
may occur as late as 48 hours after start treatment
Estimated incidence is 0.7 to 1.0 per 100 episodes of DKA in
children
Mortality rate of 70%
No specific presentation or treatment variables predict
development of edema
Young age and new-onset diabetes are only identified potential
risk factors
44
CEREBRAL EDEMA
Symptoms include:
Severe headache
Incontinence
Change in arousal or behavior
Pupillary changes
Blood pressure changes
Seizures
Bradycardia
Disturbed temperature regulation
Treat with Mannitol
Any change in neurologic function early in therapy should
prompt immediate infusion of mannitol at 1-2 g/kg
