
1
Lec: 1
Dr. Mohammed Alhamdany
Peptic ulcer disease
Refers to an ulcer in the lower oesophagus, stomach or duodenum and part of
gut that expose to acid and pepsin.
Ulcers in the stomach or duodenum may be acute or chronic; both penetrate the
muscularis mucosae but the acute ulcer shows no evidence of fibrosis. Erosions
do not penetrate the muscularis mucosae.
Gastric and duodenal ulcer
The prevalence of peptic ulcer (0.1–0.2%) is decreasing in many Western
communities as a result of widespread use of Helicobacter pylori eradication
therapy, with male > female
Pathophysiology
A- H. pylori
Peptic ulceration is strongly associated with H. pylori infection. The prevalence
of the infection in developed nations rises with age and in the UK
approximately 50% of people over the age of 50 years are infected. In the
developing world infection is more common, affecting up to 90% of adults.
These infections are probably acquired in childhood by person-to-person
contact.
Around 90% of duodenal ulcer patients and 70% of gastric ulcer patients are
infected with H. pylori. The remaining 30% of gastric ulcers are caused by
NSAIDs.
It can cause:
1- Duodenal ulcer
2- gastric atrophy with ulcer
3- increase risk of Ca stomatch
4- MALTOMA ?
B- NSAIDs
Treatment with NSAIDs is associated with peptic ulcers due to impairment of
mucosal defences.
C- Smoking
Smoking confers an increased risk of gastric ulcer and, to a lesser extent,
duodenal ulcer. Once the ulcer has formed, it is more likely to cause
complications and less likely to heal if the patient continues to smoke.
D- Genetic factors and blood group O
Disease associate with peptic ulcer include:
(1) Advanced age
(2) Chronic pulmonary disease
(3) Chronic renal failure

2
(4) Cirrhosis
(5) Nephrolithiasis
(6) α1-antitrypsin deficiency
(7) Systemic mastocytosis
(8) Hyperparathyroidism
(9) Coronary artery disease
(10) Polycythemia vera
(11) Chronic pancreatitis
(12) Former alcohol use
(13) Obesity
Clinical features
Peptic ulcer disease is a chronic condition with spontaneous relapses and
remissions lasting for decades, if not for life. The most common presentation is
with recurrent abdominal pain that has three notable characteristics: localisation
to the epigastrium, relationship to food and episodic occurrence.
The typical pain pattern in DU occurs 90 min to 3 h after a meal and is
frequently relieved by antacids or food. Pain that awakes the patient from sleep
(between midnight and 3 a.m.) is the most discriminating symptom, with two-
thirds of DU patients describing this complaint.it also may presented with
hunger pain.
Occasional vomiting occurs in about 40% of ulcer subjects; persistent daily
vomiting suggests gastric outlet obstruction.
Physical examination: Epigastric tenderness is the most frequent finding in
patients with GU or DU.
Investigations
Endoscopy is the preferred investigation, Gastric ulcers may occasionally be
malignant and therefore must always be biopsied and followed up to ensure
healing. Patients should be tested for H. pylori infection.
3
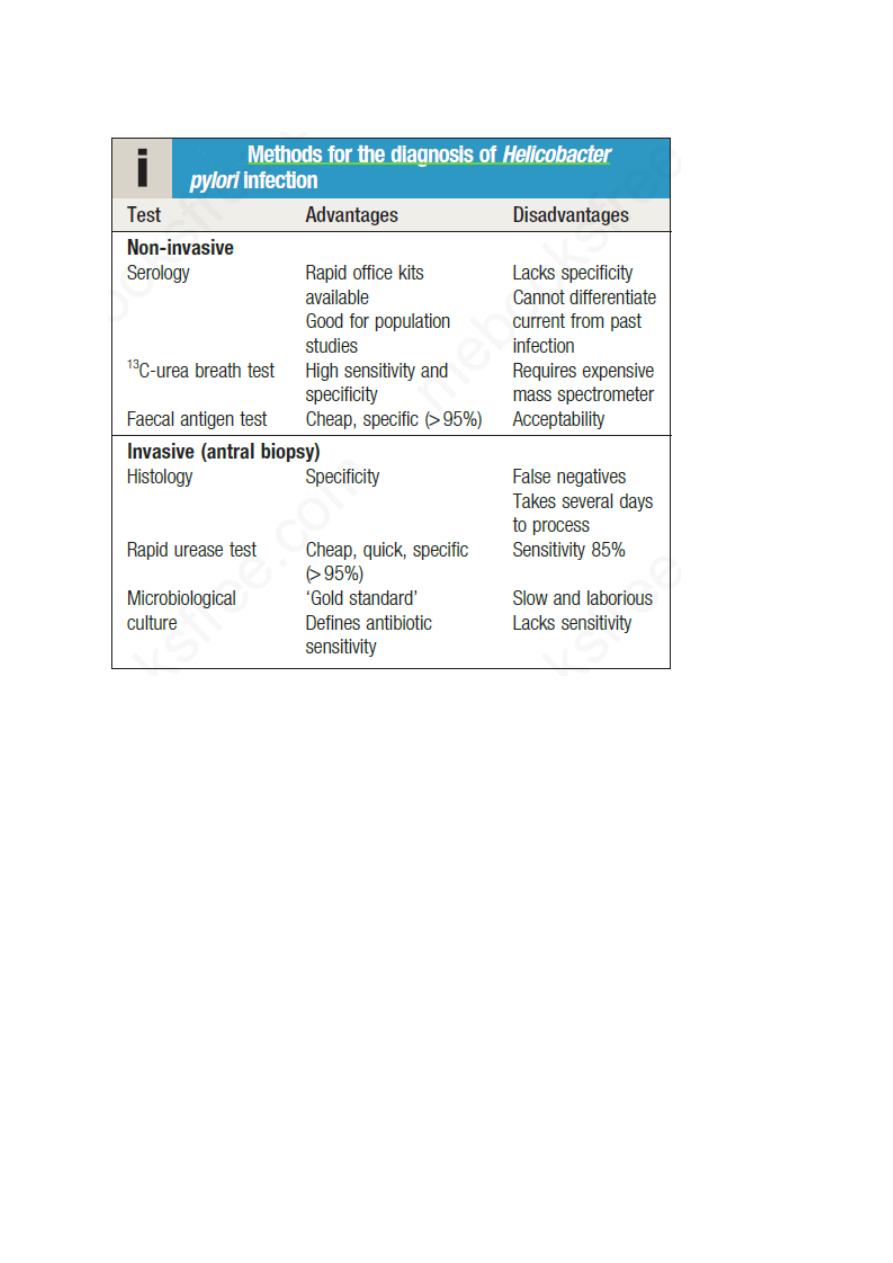
21.34 Methods for the diagnos
is of
Helicobacter
Management
The aims of management are to relieve symptoms, induce healing and prevent
recurrence. H. pylori eradication is the cornerstone of therapy for peptic ulcers,
as this will successfully prevent relapse and eliminate the need for long-term
therapy in the majority of patients.
ACID-NEUTRALIZING/INHIBITORY DRUGS
1- antacid:
Aluminum hydroxide can produce constipation and phosphate depletion;
magnesium hydroxide may cause loose stools.
2- H2 Receptor Antagonists Four of these agents are presently available
(cimetidine, ranitidine, famotidine, and nizatidine), and their structures share
homology with histamine.
3- Proton Pump (H+,K+-ATPase) Inhibitors Omeprazole, esomeprazole,
lansoprazole, rabeprazole, and pantoprazole are substituted benzimidazole
derivatives that covalently bind and irreversibly inhibit H+,K+-ATPase.

4
Sometime these drug use for longtime
Long-term acid suppression, especially with PPIs, has been associated with a
1-higher incidence of community-acquired pneumonia as well as community
and hospital acquired Clostridium difficile– associated disease.
2- long-term use of PPIs was associated with the development of hip fractures
in older women.
3- Long-term use of PPIs has also been implicated in the development of iron,
vitamin B12, and magnesium deficiency.
4- PPIs may exert a negative effect on the antiplatelet effect of clopidogrel.
Although the evidence is mixed and inconclusive, a small increase in mortality
and readmission rate for coronary events was seen in patients receiving a PPI
while on clopidogrel in earlier studies.
5- Additional concerning side effects with long-term PPI use include increased
cardiac risks independent of clopidogrel use, dementia, acute and chronic
kidney injury.
H. pylori eradication
All patients with proven ulcers who are H. pylori-positive should be offered
eradication as primary therapy. Treatment is based on a PPI taken
simultaneously with two antibiotics (from amoxicillin, clarithromycin and
metronidazole) for at least 7 days. High-dose, twice-daily PPI therapy increases
efficacy of treatment, as does extending treatment to 10–14 days. Success is
achieved in 80–90% of patients, although adherence, side-effects and antibiotic
resistance influence this.
Common side-effects of Helicobacter pylori eradication therapy
•
Diarrhoea: 30–50% of patients; usually mild but Clostridium difficile-
associated diarrhoea can occur
•
Flushing and vomiting when taken with alcohol (metronidazole)
•
Nausea, vomiting
•
Abdominal cramps
•
Headache
•
Rash
Indications for Helicobacter pylori eradication
Definite
1. Peptic ulcer
2. Extranodal marginal-zone lymphomas of MALT type

5
3. Family history of gastric cancer
4. Previous resection for gastric cancer
5. H. pylori-positive dyspepsia
6. Long-term NSAID or low-dose aspirin users
7. Chronic (> 1 year) PPI users
Not indicated
•
Gastro-oesophageal reflux disease
•
Asymptomatic people without gastric cancer risk factors
General measures
Cigarette smoking, aspirin and NSAIDs should be avoided. Alcohol in
moderation is not harmful and no special dietary advice is required.
Complications of peptic ulcer disease
1- Perforation
When perforation occurs, the contents of the stomach escape into the peritoneal
cavity, leading to peritonitis. This is more common in duodenal than in gastric
ulcers and is usually found with ulcers on the anterior wall. About one-quarter
of all perforations occur in acute ulcers and NSAIDs are often incriminated.
2- Gastric outlet obstruction
The presentation is with nausea, vomiting and abdominal distension. Large
quantities of gastric content are often vomited and food eaten 24 hours or more
previously may be recognised. Physical examination may show evidence of
wasting and dehydration. A succussion splash may be elicited 4 hours or more
after the last meal or drink.
3- Bleeding
Cause upper GIT bleeding causing hematemesis and melena
Zollinger–Ellison syndrome
This is a rare disorder characterised by the triad of severe peptic ulceration,
gastric acid hypersecretion and a neuro-endocrine tumour of the pancreas or
duodenum (‘gastrinoma’). It probably accounts for about 0.1% of all cases of
duodenal ulceration. The syndrome occurs in either sex at any age, although it is
most common between 30 and 50 years of age.
With best wishes
