Lec: 3
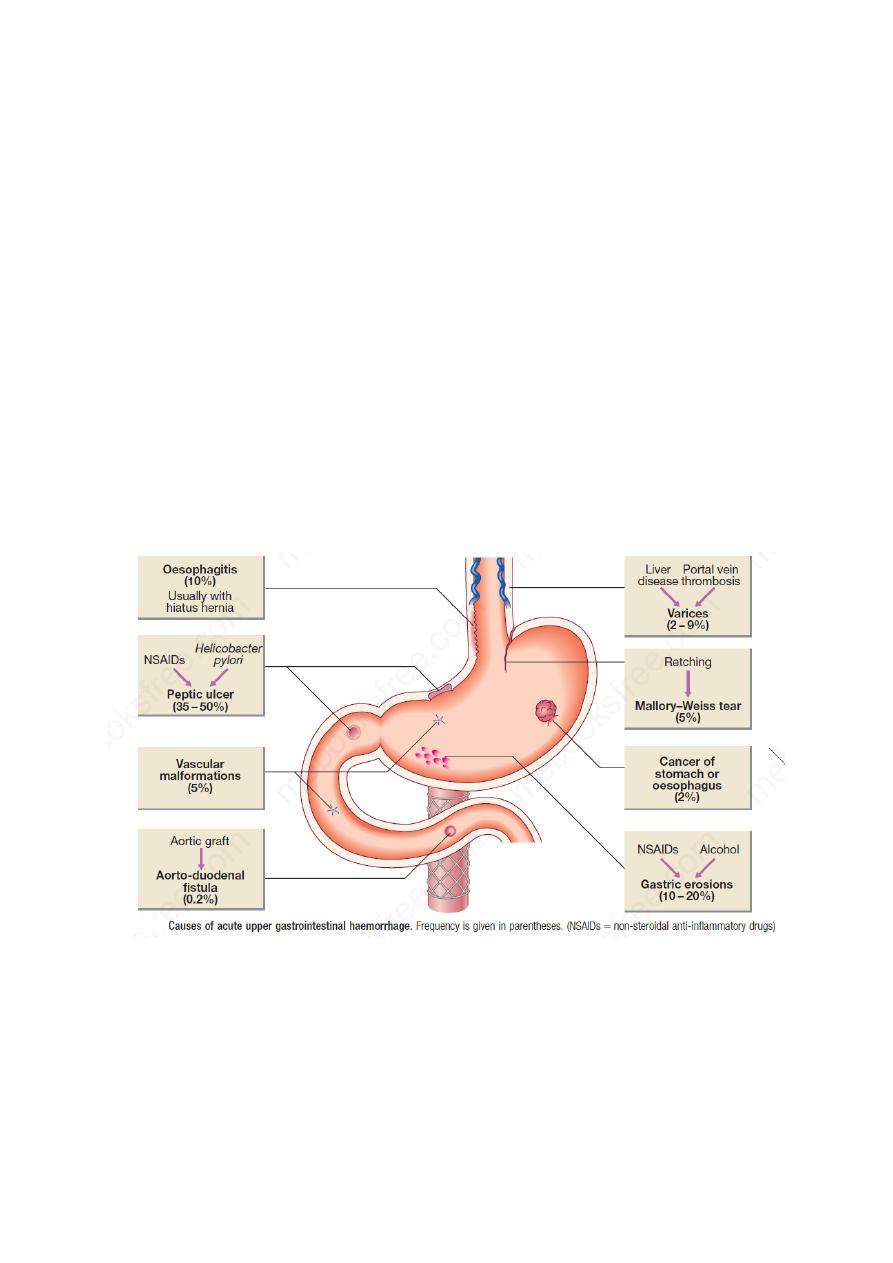
Acute upper gastrointestinal haemorrhage
The common causes:
Esophagus
1- Oesophagitis (10%) Usually with hiatus hernia
2- Variceal bleeding (2 – 9%)
3- Mallory–Weiss tear (5%)
Stomach and duodenum
1- Peptic ulcer (35 – 50%)
2- Gastric erosions (10 – 20%)
3- Vascular malformations (5%)
Combine
Cancer of stomach or oesophagus (2%)
Clinical assessment
1- Haematemesis is red with clots when bleeding is rapid and profuse, or black
(‘coffee grounds’) when less severe.
2- Syncope may occur and is caused by hypotension from intravascular volume
depletion.
1
3- Symptoms of anaemia suggest chronic bleeding.
4- Melaena is the passage of black, tarry stools containing altered blood; it is
usually caused by bleeding from the upper gastrointestinal tract, although
haemorrhage from the right side of the colon is occasionally responsible. The
characteristic colour and smell are the result of the action of digestive enzymes
and of bacteria on haemoglobin. Other causes include Iron suplimentation,
Bismuth, blueberry, black liquorice and beetroot
5- Hematochezia
:
Severe acute upper gastrointestinal bleeding can sometimes
cause maroon or bright red stool.
Management
1. Intravenous access: The first step is to gain intravenous access using at least
one large-bore cannula.
2. Initial clinical assessment
• Define circulatory status. Severe bleeding causes tachycardia, hypotension ,
postural hypotension and oliguria. The patient is cold and sweating, and may be
agitated.
• Seek evidence of liver disease. Jaundice, cutaneous stigmata,
hepatosplenomegaly and ascites may be present in decompensated cirrhosis.
• Identify comorbidity. The presence of cardiorespiratory, cerebrovascular or
renal disease is important, both because these may be worsened by acute
bleeding and because they increase the hazards of endoscopy and surgical
operations.
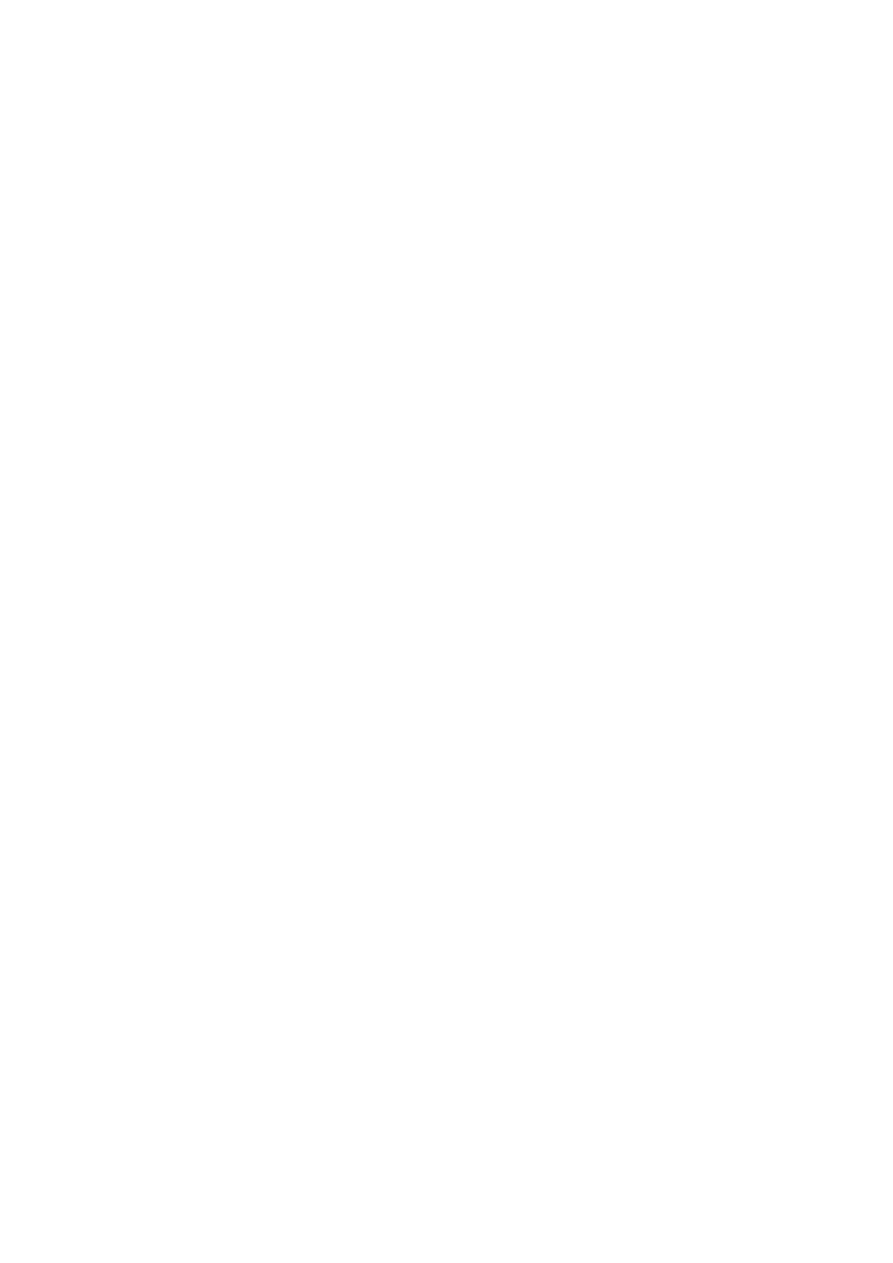
• Blatchford score: which can be calculated at the bedside. A score of 2 or less is
associated with a good prognosis, while progressively higher scores are
associated with poorer outcomes.
3. Basic investigations
• Full blood count. Chronic or subacute bleeding leads to anaemia but the
haemoglobin concentration may be normal after sudden, major bleeding until
haemodilution occurs. Thrombocytopenia may be a clue to the presence of
hypersplenism in chronic liver disease.
• Urea and electrolytes.
• Liver function tests.
• Prothrombin time.
• Cross-matching. At least 2 units of blood should be cross-matched if a
significant bleed is suspected.
4. Resuscitation
Intravenous crystalloid fluids should be given to raise the blood pressure, and
blood should be transfused when the patient is actively bleeding with low blood
pressure and tachycardia. Comorbidities should be managed as appropriate.
Patients with suspected chronic liver disease should receive broad-spectrum
antibiotics.
2
5. Oxygen: this should be given to all patients in shock.
6. Endoscopy
This should be carried out after adequate resuscitation, ideally within 24 hours,
and will yield a diagnosis in 80% of cases.
Treatment include:
A- ‘heater probe’
B- endoscopic clips,
C- usually combined with injection of dilute adrenaline (epinephrine) into the
bleeding point (‘dual therapy’).
D- A biologically inert haemostatic mineral powder (TC325, ‘haemospray’) can
be used as rescue therapy when standard therapy fails.
E- This may stop active bleeding and, combined with intravenous proton pump
inhibitor (PPI) therapy, may prevent re-bleeding.
3

F- Patients found to have bled from varices should be treated by band ligation;
if this fails,
G- Balloon tamponade.
H- transjugular intrahepatic portosystemic shunt (TIPSS).
9. Eradication
Following treatment for ulcer bleeding, all patients should avoid non-steroidal
anti-inflammatory drugs (NSAIDs) and those who test positive for H. pylori
infection should receive eradication therapy. Successful eradication should be
confirmed by urea breath or faecal antigen testing.
Lower gastrointestinal bleeding
Causes of lower gastrointestinal bleeding
Severe acute
1. Diverticular disease
2. Angiodysplasia
3. Ischaemia
4. Meckel’s diverticulum
5. Inflammatory bowel disease (rarely)
Moderate, chronic/subacute
1. Fissure
2. Solitary rectal ulcer
3. Haemorrhoids
4. Inflammatory bowel disease
5. Angiodysplasia
6. Carcinoma
7. Large polyps
8. Radiation enteritis
Severe acute lower gastrointestinal bleeding
This presents with profuse red or maroon diarrhoea and with shock. Diverticular
disease is the most common cause and is often due to erosion of an artery within
the mouth of a diverticulum.
Subacute or chronic lower gastrointestinal bleeding
This can occur at all ages and is usually due to haemorrhoids or anal fissure.
Haemorrhoidal bleeding is bright red and occurs during or after defecation.
Proctoscopy can be used to make the diagnosis, but subjects who have altered
bowel habit and those who present over the age of 40 years should undergo
colonoscopy to exclude coexisting colorectal cancer. Anal fissure should be
suspected when fresh rectal bleeding and anal pain occur during defecation.
Ischemic gut injury
Acute small bowel ischaemia
Causes
4
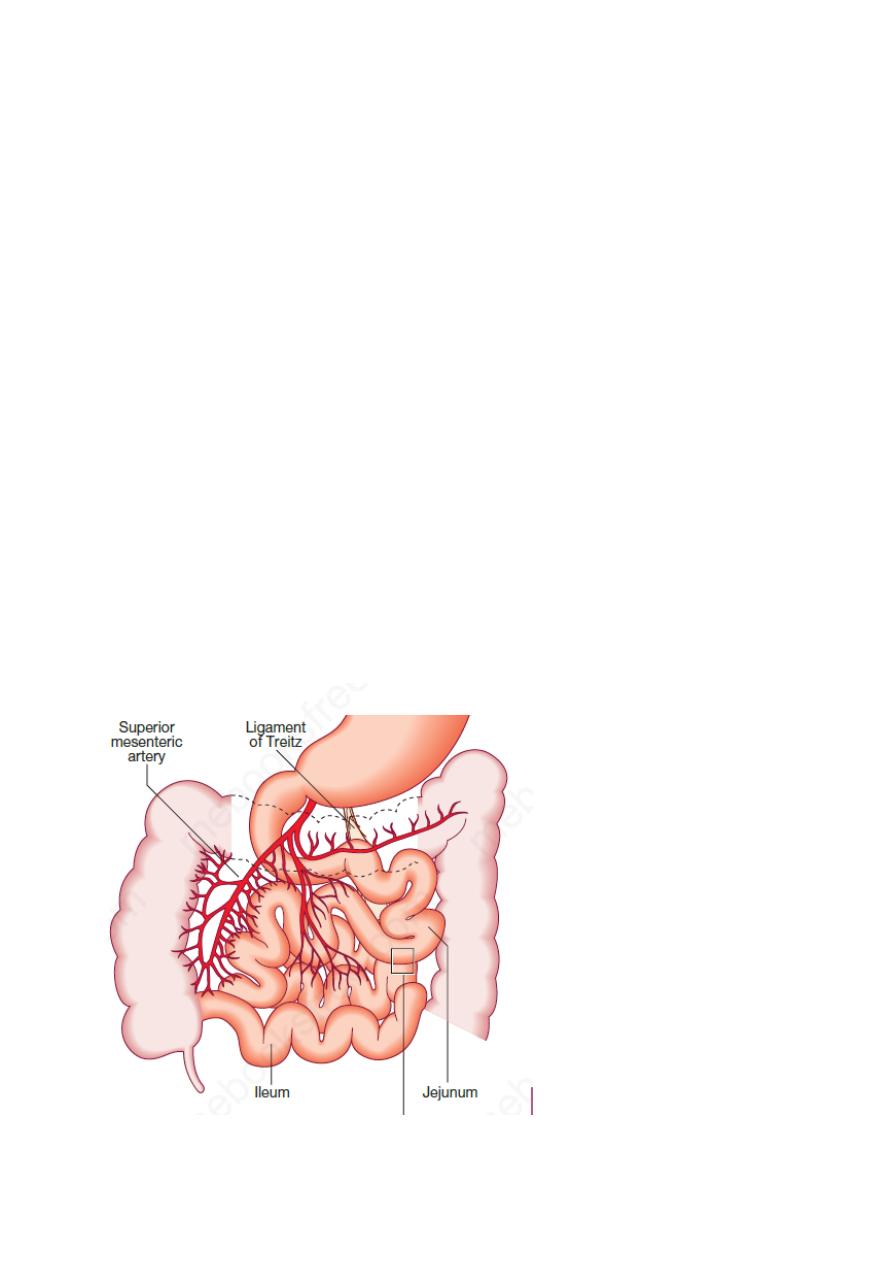
1- An embolus from the heart ( specially in patient with AF)or aorta to the
superior mesenteric artery is responsible for 40–50% of cases.
2- thrombosis of underlying atheromatous disease for approximately 25%.
3- ischaemia due to hypotension complicating myocardial infarction, heart
failure, arrhythmias or sudden blood loss for approximately 25%
4- Vasculitis (rare)
Clinical feature: include diarrhea, lower GIT bleeding, and Almost all develop
abdominal pain that is more impressive than the physical findings.
Signs: In the early stages, the only physical signs may be a silent, distended
abdomen or diminished bowel sounds, with peritonitis developing only later.
Ix: Leucocytosis, metabolic acidosis, hyperphosphataemia and
hyperamylasaemia are typical. Plain abdominal X-rays show ‘thumb-printing’
due to mucosal oedema. Mesenteric or CT angiography reveals an occluded or
narrowed major artery with spasm of arterial arcades.
Investigations for underlying prothrombotic disorders should be performed.
Management:
Resuscitation, management of cardiac disease and intravenous antibiotic
therapy, followed by laparotomy and bowel resection, are key steps. If treatment
is instituted early, embolectomy and vascular reconstruction may salvage some
small bowel.
In patients at high surgical risk, thrombolysis may sometimes be effective. The
results of therapy depend on early intervention; patients treated late have a 75%
mortality rate.
Investigations for underlying prothrombotic disorders should be performed.
5

Acute colonic ischaemia:
The splenic flexure and descending colon have little collateral circulation and
lie in ‘watershed’ areas of arterial supply.
Causes
1- Arterial thromboembolism (main cause).
2- severe hypotension.
3- colonic volvulus.
4- strangulated hernia.
5- systemic vasculitis.
6- hypercoagulable states.
7- complication of abdominal aortic aneurysm surgery (where the inferior
mesenteric artery is ligated).
Clinical feature:
The patient is usually elderly and presents with sudden onset of cramping, left-
sided, lower abdominal pain and rectal bleeding. Symptoms usually resolve
spontaneously over 24–48 hours and healing occurs in 2 weeks.
Complication:
fibrous stricture or segment of colitis. A minority develop gangrene and
peritonitis.
Diagnosis: colonoscopy within 48 hour
Treatment: self-limit disease, Resection is required for peritonitis.
Chronic mesenteric ischaemia
This results from atherosclerotic stenosis of the coeliac axis, superior
mesenteric artery and inferior mesenteric artery. The typical presentation is with
dull but severe mid- or upper abdominal pain developing about 30 minutes after
eating. Weight loss is common because patients are reluctant to eat and some
experience diarrhoea. Physical examination shows
evidence of generalised arterial disease. An abdominal bruit is sometimes
audible but is non-specific. The diagnosis is made by mesenteric angiography.
Treatment is by vascular reconstruction or percutaneous angioplasty, if the
patient’s clinical condition permits. The condition is frequently complicated by
intestinal infarction, if left untreated.
With best wishes
6
