Lec .4 Dr. Nihad Abdallah Al-jeboori /Subspecialty Endocrinology &Diabetes
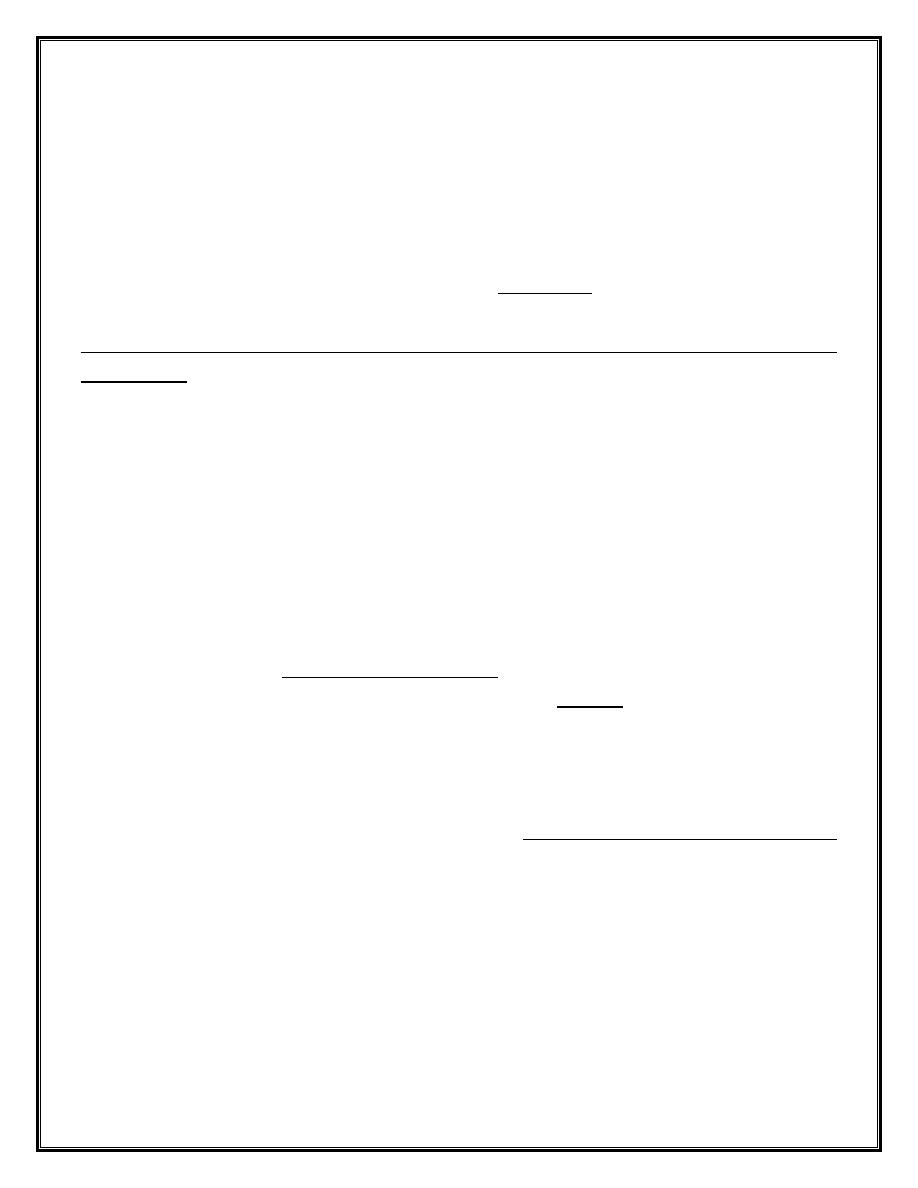
Thyroid lump or swelling
A lump or swelling in the thyroid gland can be a source of considerable anxiety for
patients. There are numerous causes but, broadly speaking, a thyroid swelling is either
a solitary nodule, a multinodular goitre or a diffuse goitre . Nodular thyroid disease is
more common in women and occurs in approximately 30% of the adult female
population. The majority of thyroid nodules are impalpable but may be identified when
imaging of the neck is performed for another reason, such as during Doppler
ultrasonography of the carotid arteries or computed tomographic pulmonary
angiography. Increasingly, thyroid nodules are identified during staging of patients with
cancer with computed tomography (CT), magnetic resonance imaging (MRI) or positron
emission tomography (PET) scans.
Palpable thyroid nodules occur in 4–8% of adult women and 1–2% of adult men, and
classically present when the individual (or a friend or relative) notices a lump in the
neck. Multinodular goitre and solitary nodules sometimes present with acute painful
enlargement due to haemorrhage into a nodule. Patients with thyroid nodules often
worry that they have cancer but the reality is that only 5–10% of thyroid nodules are
malignant.
A nodule presenting in childhood or adolescence, particularly if there is a past history of
head and neck irradiation, or one presenting in an elderly patient should heighten
suspicion of a primary thyroid malignancy . The presence of cervical lymphadenopathy
also increases the likelihood of malignancy.
Rarely, a secondary deposit from a renal, breast or lung carcinoma presents as a painful,
rapidly growing, solitary thyroid nodule. Thyroid nodules identified on PET scanning
have an approximately 33% chance of being malignant.
Lec .4 Dr. Nihad Abdallah Al-jeboori /Subspecialty Endocrinology &Diabetes
Clinical assessment and investigations
Swellings in the anterior part of the neck most commonly originate in the thyroid and
this can be confirmed by demonstrating that the swelling moves on swallowing . It is
often possible to distinguish clinically between the three main causes of thyroid
swelling. There is a broad differential diagnosis of anterior neck swellings, which
includes lymphadenopathy, branchial cysts, dermoid cysts and thyroglossal duct cysts
(the latter are classically located in the midline and move on protrusion of the tongue).
An ultrasound scan should be performed urgently, if there is any doubt as to the
aetiology of an anterior neck swelling. Serum T3, T4 and TSH should be measured in all
patients with a goitre or solitary thyroid nodule. The finding of biochemical
thyrotoxicosis or hypothyroidism (both of which may be subclinical) should lead to
investigations, as already described in previous lectures.
Lec .4 Dr. Nihad Abdallah Al-jeboori /Subspecialty Endocrinology &Diabetes
Thyroid scintigraphy
Thyroid scintigraphy with 99m technetium should be performed in an individual with a
low serum TSH and a nodular thyroid to confirm the presence of an autonomously
functioning (‘
hot
’) nodule .In such circumstances, further evaluation is not necessary.
‘
Cold
’ nodules on scintigraphy have a much higher likelihood of malignancy, but the
majority are benign and so scintigraphy is not routinely used in the evaluation of thyroid
nodules when TSH is normal.
Toxic adenoma
A solitary toxic nodule is the cause of less than 5% of all cases of thyrotoxicosis. The
nodule is a follicular adenoma, which autonomously secretes excess thyroid hormones
and inhibits endogenous TSH secretion, with subsequent atrophy of the rest of the
thyroid gland. The adenoma is usually greater than 3 cm in diameter.
Most patients are female and over 40 years of age. Although many nodules are
palpable, the diagnosis can be made with certainty only by thyroid scintigraphy . The
thyrotoxicosis is usually mild and in almost 50% of patients the plasma T3 alone is
elevated (T3 thyrotoxicosis). 131I (400–800 MBq (10–20 mCi)) is highly effective and is
an ideal treatment since the atrophic cells surrounding the nodule do not take up iodine
and so receive little or no radiation. For this reason, permanent hypothyroidism is
unusual. Hemithyroidectomy is an alternative management option.
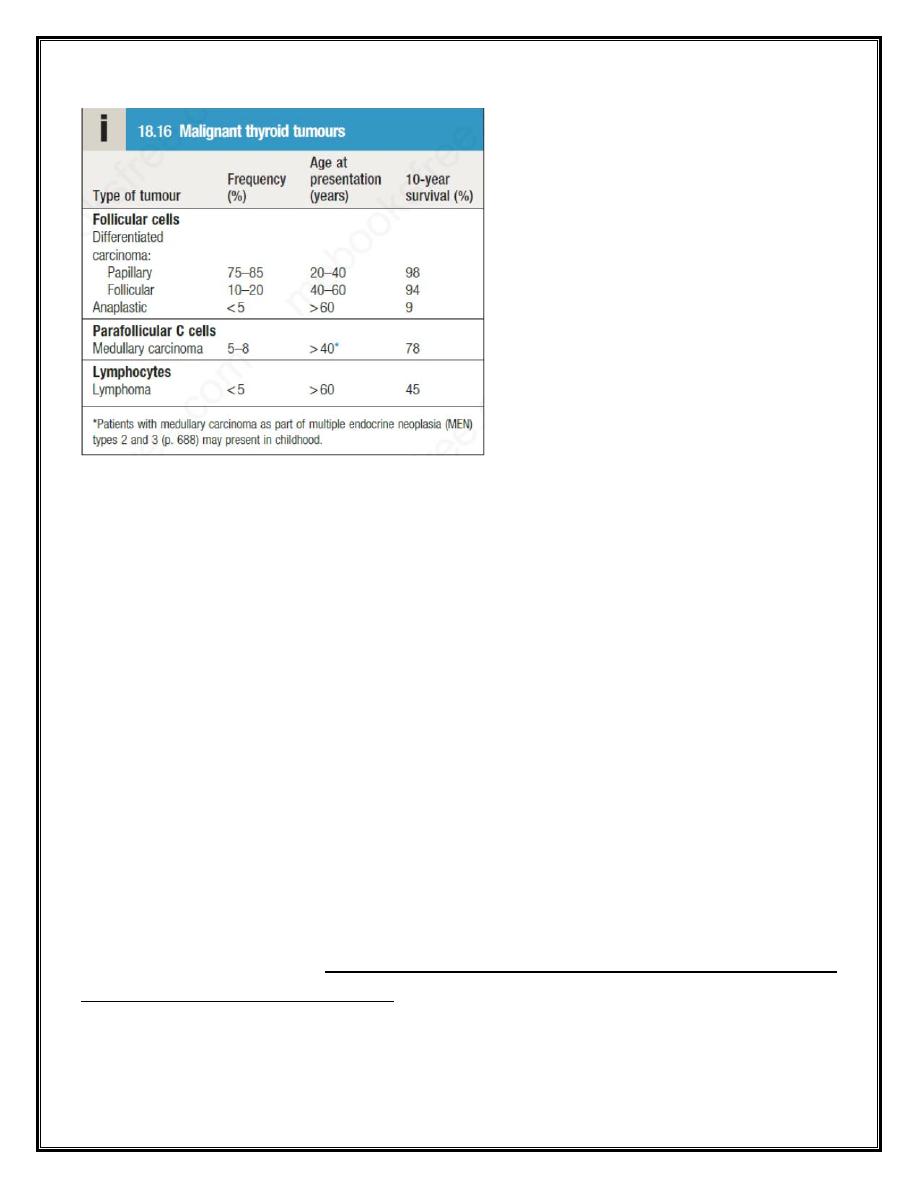
Thyroid neoplasia
Patients with thyroid tumours usually present with a solitary nodule . Most are benign
and a few of these, called ‘toxic adenomas’, secrete excess thyroid hormones. Primary
thyroid malignancy is rare, accounting for less than 1% of all carcinomas, and has an
incidence of 25 per million per annum. It can be classified according to the cell type of
origin. With the exception of medullary carcinoma, thyroid cancer is more common in
females.
Lec .4 Dr. Nihad Abdallah Al-jeboori /Subspecialty Endocrinology &Diabetes
Differentiated carcinoma
Papillary carcinoma
This is the most common of the malignant thyroid tumours and accounts for 90% of
radiation-induced thyroid cancer. It may be multifocal and spread is initially to regional
lymph nodes. Some patients present with cervical lymphadenopathy and no apparent
thyroid enlargement; in such instances, the primary lesion may be less than 10 mm in
diameter.
Follicular carcinoma
This is usually a single encapsulated lesion. Spread to cervical lymph nodes is rare.
Metastases are blood-borne and are most often found in bone, lungs and brain.
Management
The management of thyroid cancers should be individualized and planned in
multidisciplinary team meetings that include all specialists involved in the service; this
should include thyroid surgeons, endocrinologists, oncologists, pathologists,
radiologists and nurse specialists. Large tumours, those with adverse histological
features and/or tumours with metastatic disease at presentation are usually managed
by total thyroidectomy followed by a large dose of
131
I ( (approximately 30 or 100 mCi))
Lec .4 Dr. Nihad Abdallah Al-jeboori /Subspecialty Endocrinology &Diabetes
to ablate any remaining normal or malignant thyroid tissue. Thereafter, long-term
treatment with levothyroxine in a dose sufficient to suppress TSH (usually 150–200 μg
daily) is given, as there is evidence that growth of differentiated thyroid carcinomas is
TSH-dependent. Smaller tumours with no adverse histological features may require only
thyroid lobectomy.
Follow-up involves measurement of serum thyroglobulin, which should be undetectable
in patients whose normal thyroid has been ablated and who are taking a suppressive
dose of levothyroxine. Thyroglobulin antibodies may interfere with the assay and,
depending on the method employed, may result in a falsely low or high result.
Detectable thyroglobulin, in the absence of assay interference, is suggestive of tumour
recurrence or metastases, particularly if the thyroglobulin titre is rising across serial
measurements. Local recurrence or metastatic disease may be localised by ultrasound,
CT, MRI and/or whole-body scanning with
131
I, and may be treated with further surgery
and/or
131
I therapy.
Those with locally advanced or metastatic papillary and follicular carcinoma that is
refractive to
131
I may be considered for therapy with sorafenib or lenvatinib. These
drugs are multi-targeted tyrosine kinase inhibitors and have been shown in trials to
prolong progression-free survival by between 5 and 14 months.
Prognosis
Most patients with papillary and follicular thyroid cancer will be cured with appropriate
treatment. Adverse prognostic factors include older age at presentation, the presence
of distant metastases, male sex and certain histological subtypes.
Anaplastic carcinoma and lymphoma
These two conditions are difficult to distinguish clinically but are distinct cytologically
and histologically. Patients are usually over 60 years of age and present with rapid
thyroid enlargement over 2–3 months. The goitre is hard and there may be stridor due
to tracheal compression and hoarseness due to recurrent laryngeal nerve palsy. There is
no effective treatment for anaplastic carcinoma, although surgery and radiotherapy may
be considered in some circumstances. In older patients, median survival is only 7
months.
Lec .4 Dr. Nihad Abdallah Al-jeboori /Subspecialty Endocrinology &Diabetes
The prognosis for lymphoma, which may arise from preexisting Hashimoto’s thyroiditis,
is better , with a median survival of 9 years. Some 98% of tumours are non-Hodgkin’s
lymphomas, usually the diffuse large B-cell subtype. Treatment is with combination
chemotherapy and external beam radiotherapy .
Medullary carcinoma
This tumour arises from the parafollicular C cells of the thyroid. In addition to calcitonin,
the tumour may secrete 5-hydroxytryptamine (5-HT, serotonin), various peptides of the
tachykinin family, adrenocorticotrophic hormone (ACTH) and prostaglandins. As a
consequence, carcinoid syndrome and Cushing’s syndrome may occur.
Patients usually present in middle age with a firm thyroid mass. Cervical lymph node
involvement is common but distant metastases are rare initially. Serum calcitonin levels
are raised and are useful in monitoring response to treatment.
Treatment
is by total thyroidectomy with removal of regional cervical lymph nodes.
Since the C cells do not concentrate iodine and are not responsive to TSH, there is no
role for 131I therapy or TSH suppression with levothyroxine. External beam
radiotherapy may be considered in some patients at high risk of local recurrence.
Vandetanib and cabozantinib are tyrosine kinase inhibitors licensed for patients with
progressive advanced medullary cancer. The prognosis is less good than for papillary
and follicular. Medullary carcinoma of the thyroid occurs sporadically in 70–90% cases;
in 10–30% of cases, there is a genetic predisposition that is inherited in an autosomal
dominant fashion and is due to an activating mutation in the RET gene. This inherited
tendency normally forms part of one of the MEN syndromes (MEN 2 (also known as
MEN 2a) or MEN 3 (also known as MEN 2b), but, occasionally, susceptibility to
medullary carcinoma is the only inherited trait (familial medullary thyroid cancer).
Riedel’s thyroiditis
This is not a form of thyroid cancer but the presentation is similar and the
differentiation can usually be made only by thyroid biopsy. It is an exceptionally rare
condition of unknown aetiology, in which thereis extensive infiltration of the thyroid
and surrounding structures with fibrous tissue. There may be associated mediastinal and
retroperitoneal fibrosis. Presentation is with a slow-growing goitre that is irregular and
Lec .4 Dr. Nihad Abdallah Al-jeboori /Subspecialty Endocrinology &Diabetes
stony-hard. There is usually tracheal and oesophageal compression necessitating partial
thyroidectomy. Other recognised complications include recurrent laryngeal nerve palsy,
hypoparathyroidism and eventually hypothyroidism.
