
ا د مهند الشاله
Intestinal obstruction
Lecture 2

■ Initially treat conservatively provided there are no signs of strangulation;
should rarely continue conservative treatment for longer than 72 hours
■ At operation, divide only the causative adhesion(s) and limit dissection
■ Repair serosal tears; invaginate (or resect) areas of doubtful viability
■ Laparoscopic adhesiolysis may be considered in highly selected cases of
small bowel obstruction and should only undertaken by surgeon with advanced
laparoscopic skills
Treatment of adhesive obstruction

Large bowel obstruction is usually caused by an underlying carcinoma or
occasionally diverticular disease, and presents in an acute or chronic form.
The condition of pseudo-obstruction should always be considered and excluded
by a limited contrast study or CT scan to confirm organic obstruction.
After full resuscitation, the abdomen should be opened through a midline
incision.
TREATMENT OF ACUTE LARGE BOWEL OBSTRUCTION

Identification of a collapsed distal segment of the large bowel and its sequential
proximal assessment will readily lead to identification of the cause.
Distension of the caecum will confirm large bowel involvement.
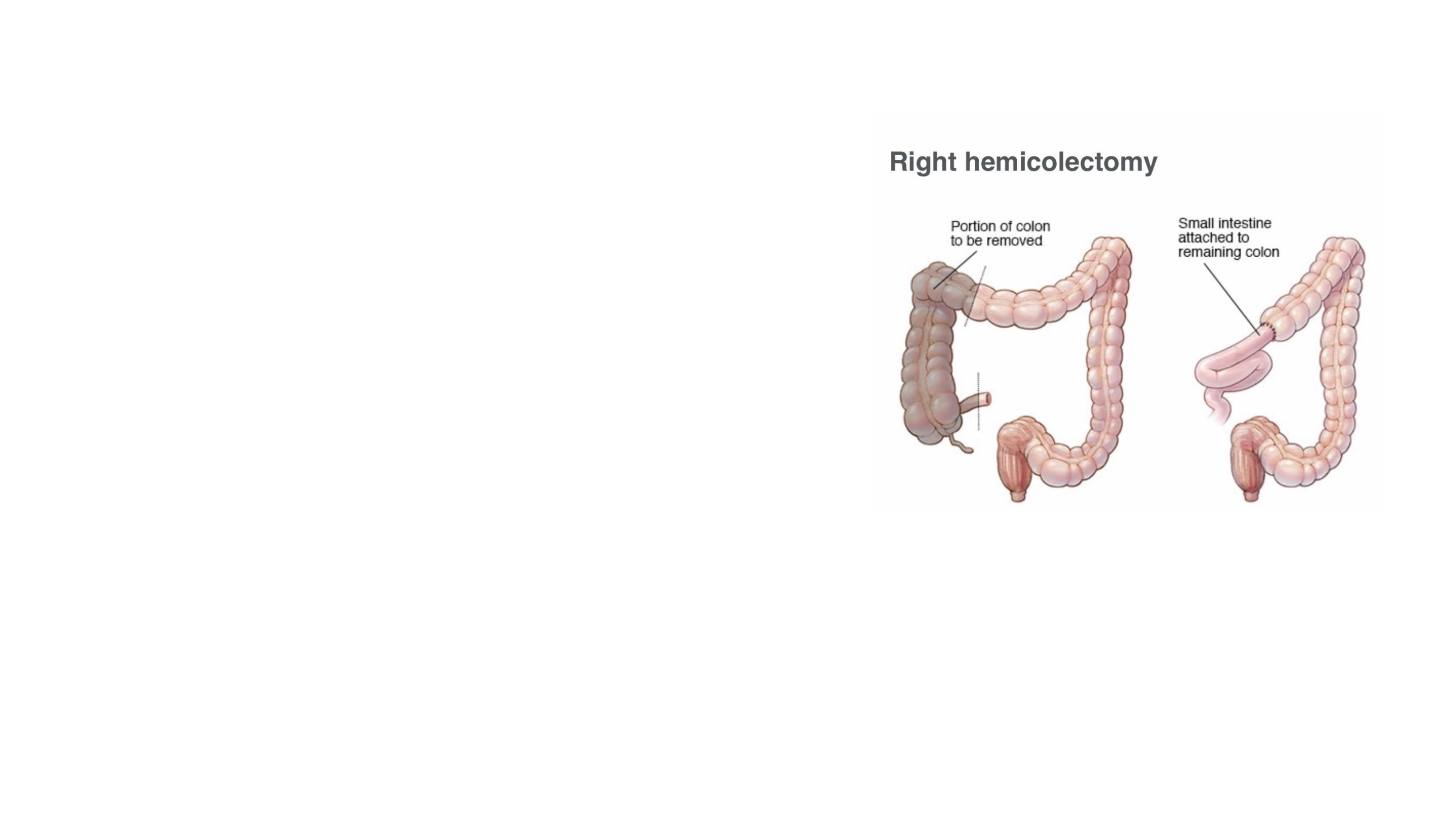
When a removable lesion is found in the caecum,
ascending colon, hepatic flexure or proximal
transverse colon, an emergency right
hemicolectomy should be performed.
A primary anastomosis is safe if the patient’s
general condition is reasonable.
If the lesion is irremovable (this is rarely the case), a
proximal stoma (colostomy or ileosotomy if the
ileocaecal valve is incompetent) or ileotransverse
bypass should be considered.
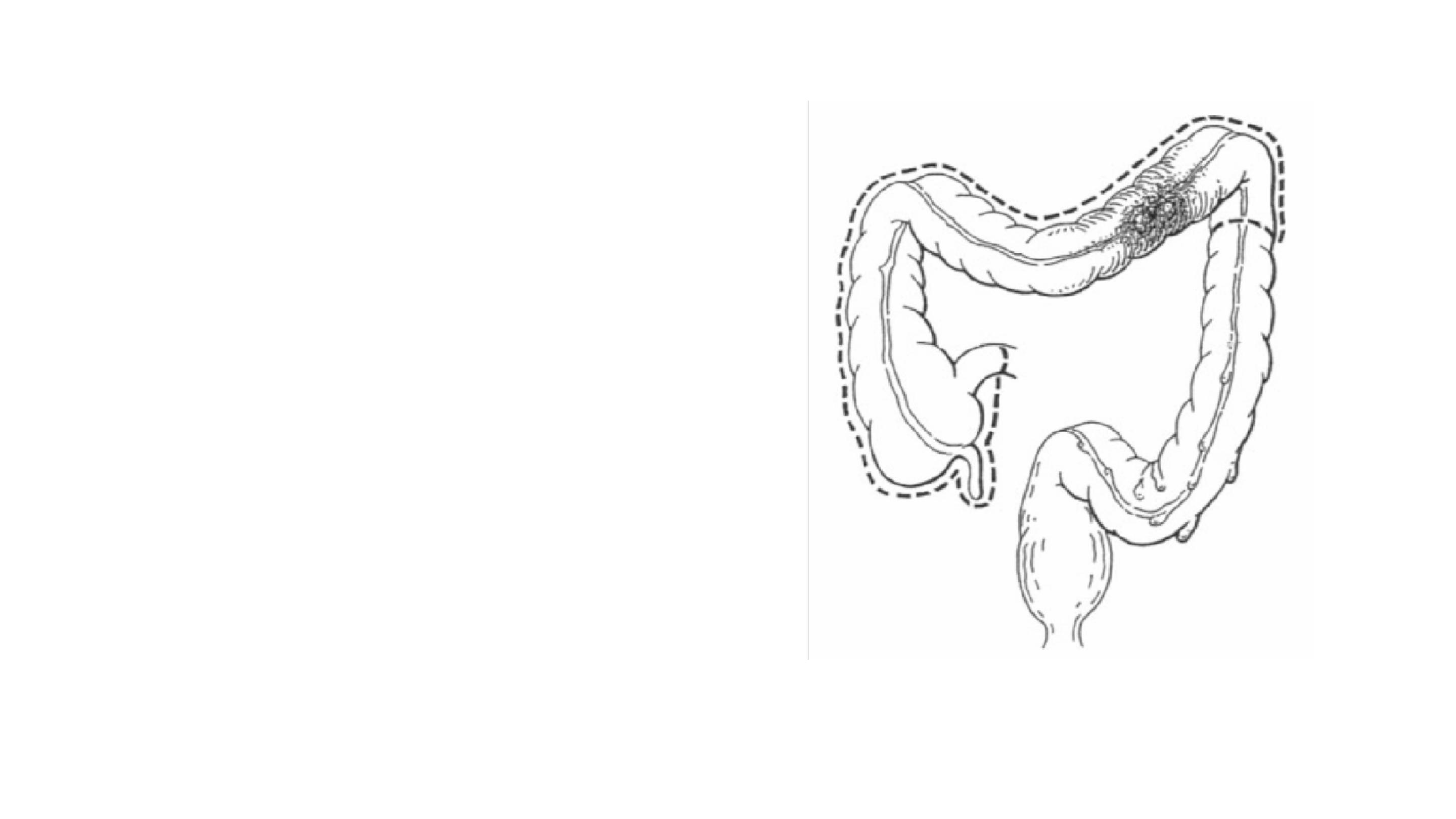
Obstructing lesions at the splenic flexure
should be treated by an extended right
hemicolectomy with ileo- descending
colonic anastomosis.
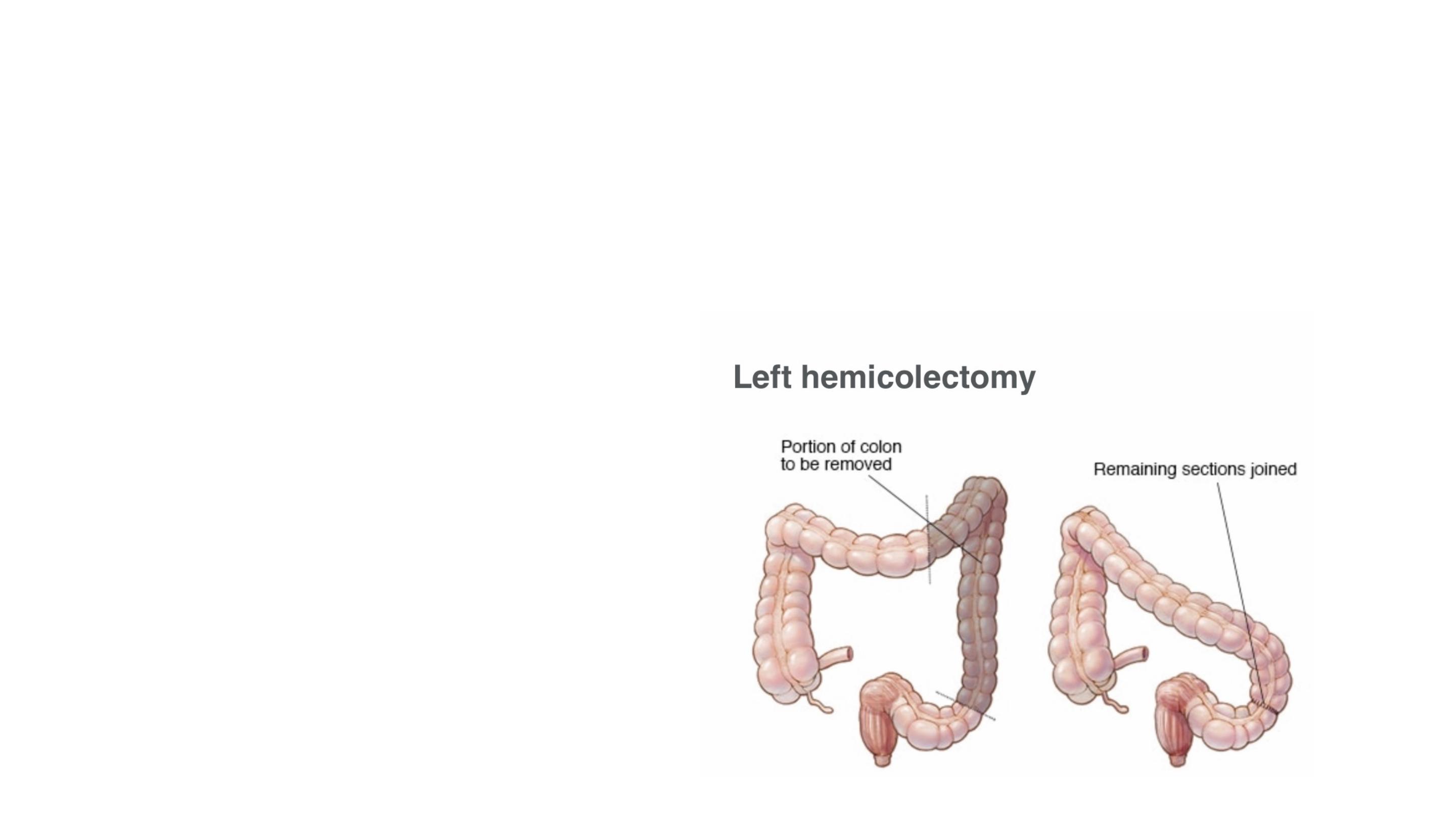
For obstructing lesions of the left colon or rectosigmoid junction,
immediate resection should be considered unless there are clear
contraindications
■ Inexperienced surgeon
■ Moribund patient
■ Advanced disease
Contraindications to immediate resection include:

In the absence of senior clinical staff, it is safest to bring the proximal
colon to the surface as a colostomy.
When possible, the distal bowel should be brought out at the same time
(Paul–Mikulicz procedure) to facilitate subsequent closure.

In the majority of cases, the distal
bowel will not reach and is closed and
returned to the abdomen (Hartmann’s
procedure).
A second-stage colorectal
anastomosis can be planned when the
patient is fit.
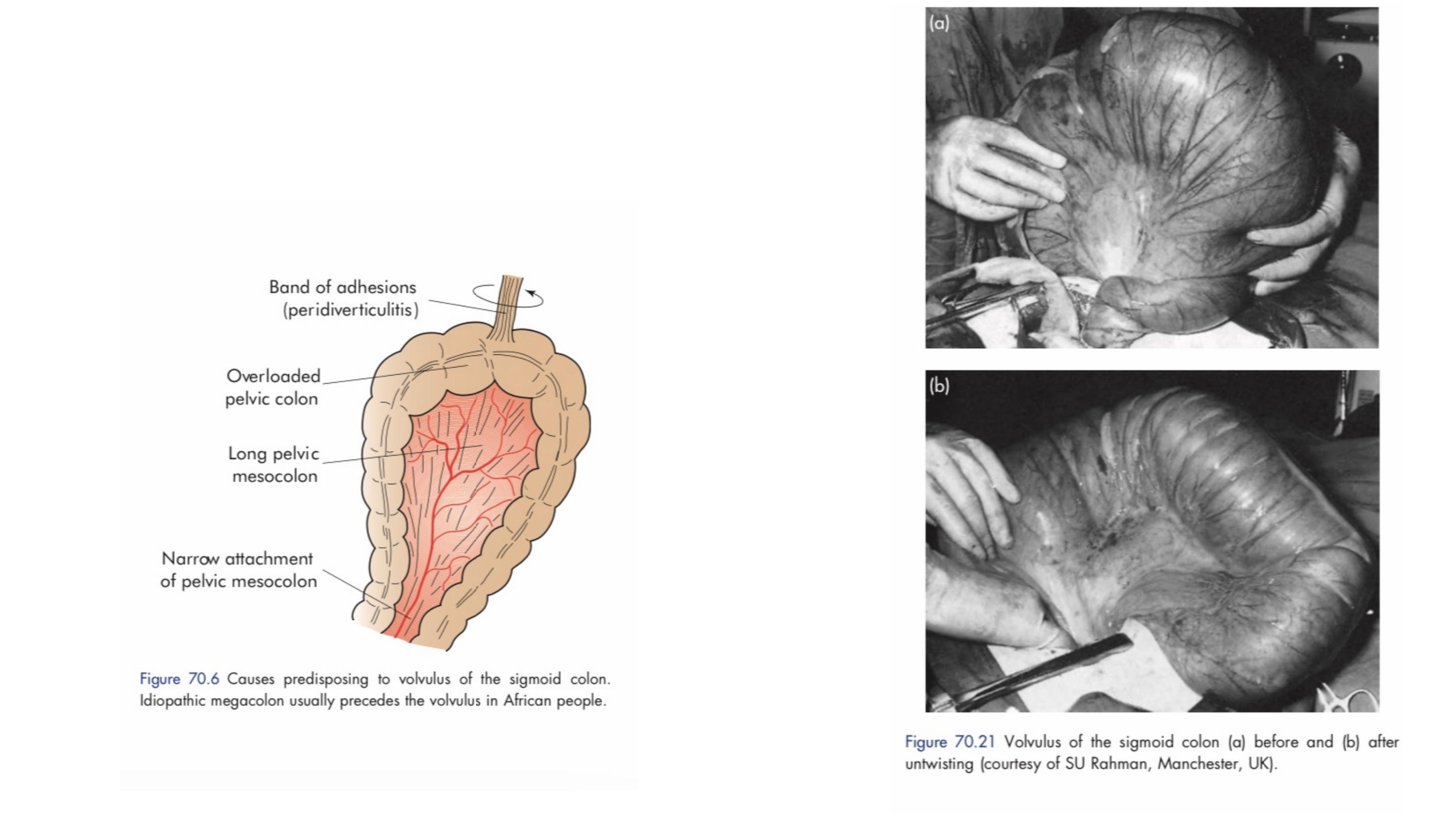
Sigmoid volvulus
The symptoms are of large bowel obstruction.

Flexible sigmoidoscopy or rigid sigmoidoscopy and insertion of a flatus tube
should be carried out to allow deflation of the gut.
The tube should be secured in place with tape for 24 hours and a repeat x-ray
taken to ensure that decompression has occurred.
Successful deflation, as long as ischaemic bowel is excluded, will resolve the
acute problem.
Treatment of sigmoid volvulus

In young patients, an elective sigmoid colectomy is required.
In the elderly patients , it is reasonable not to offer any further treatment following
successful endoscopic decompression as there is a high death rate (~80 per cent at
two years) from causes other than recurrent volvulus.
Failure results in an early laparotomy, with untwisting of the loop .
When the bowel is viable, fixation of the sigmoid colon to the posterior abdominal wall
may be a safer manoeuvre in inexperienced hands.
Resection is preferable if it can be achieved safely.
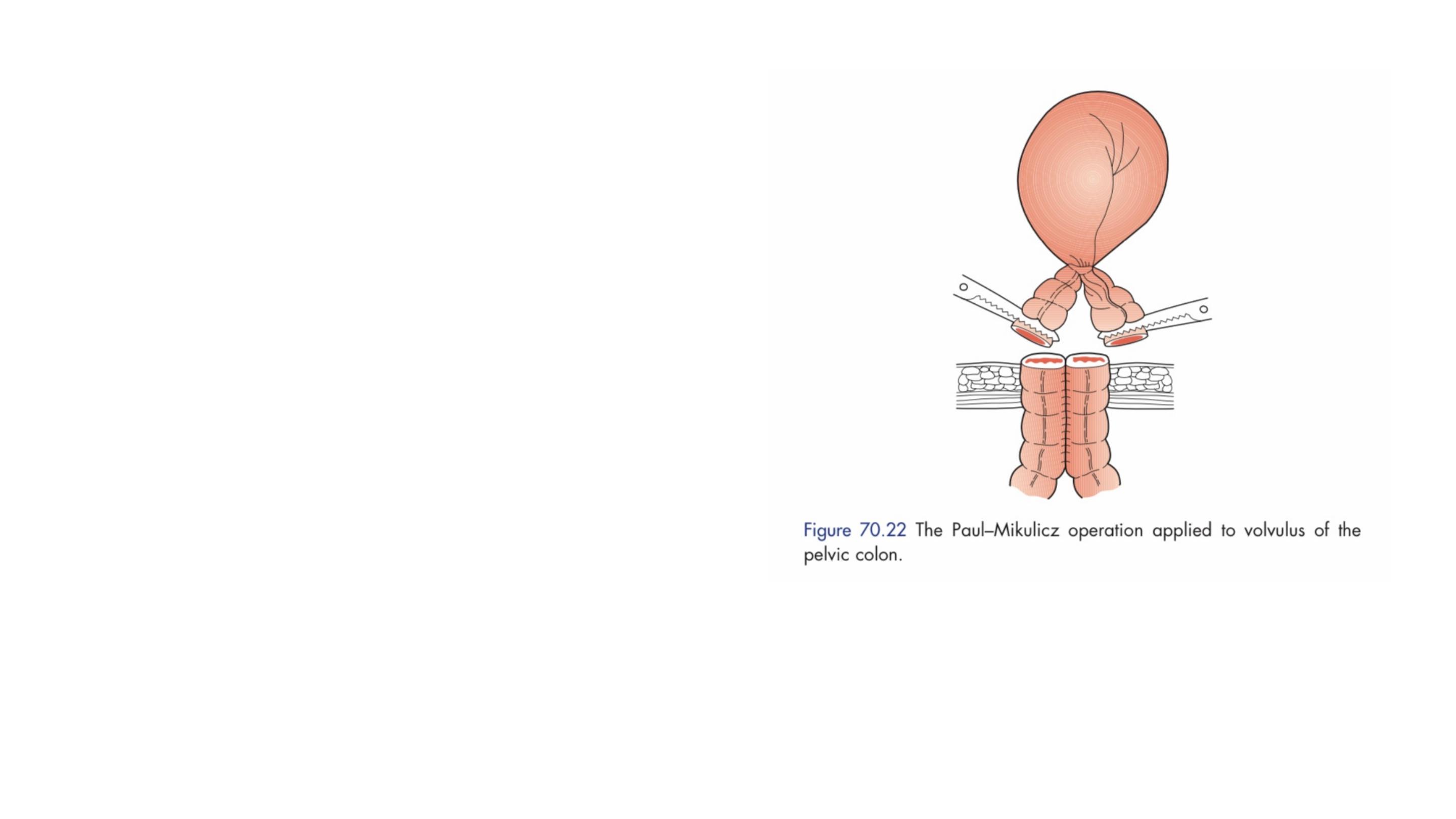
A Paul–Mikulicz procedure is
useful, particularly if there is
suspicion of impending gangrene.
an alternative procedure is a
sigmoid colectomy and, when
anastomosis is considered unwise,
a Hartmann’s procedure with
subsequent reanastomosis can be
carried out.

organic:
• intraluminal (rare) – faecal impaction;
• intrinsic intramural – strictures (Crohn’s disease,
ischaemia, diverticular), anastomotic stenosis;
• extrinsic intramural (rare) – metastatic deposits
(ovarian), endometriosis, stomal stenosis;
or functional:
• Hirschsprung’s disease, idiopathic megacolon, pseudo-
obstruction.
The causes of obstruction may be
CHRONIC LARGE BOWEL OBSTRUCTION

The symptoms of chronic obstruction differ in their predominance,
timing and degree from acute obstruction.
In functional cases, the symptoms may have been present for
months or years.

Plain abdominal radiography confirms the presence of large bowel
distension.
All such cases should be investigated by a subsequent single-contrast
water-soluble enema study, CT scan or endoscopic assessment to rule
out functional disease

Organic disease requires decompression with either
a laparotomy or stent.
Stomal stenosis can usually be managed at the
abdominal wall level.
Surgical management after resuscitation depends
on the underlying cause.

Functional disease requires colonoscopic
decompression in the first instance and
conservative management.
Intestinal perforation can occur in patients
with functional obstruction.

Paralytic ileus
This may be defined as a state in which there is failure of transmission of
peristaltic waves secondary to neuromuscular failure (i.e. in the myenteric
(Auerbach’s) and submucous (Meissner’s) plexuses).
The resultant stasis leads to accumulation of fluid and gas within the bowel,
with associated distension, vomiting, absence of bowel sounds and
absolute constipation.
ADYNAMIC OBSTRUCTION

The following varieties are recognised:
• Postoperative. A degree of ileus usually occurs after any abdominal
procedure and is self-limiting, with a variable duration of 24–72 hours.
Postoperative ileus may be prolonged in the presence of hypoproteinaemia
or metabolic abnormality.
• Infection. Intra-abdominal sepsis may give rise to localised or generalised
ileus.
• Reflex ileus. This may occur following fractures of the spine or ribs,
retroperitoneal haemorrhage or even the application of a plaster jacket.
• Metabolic. Uraemia and hypokalaemia are the most common contributory
factors.

Paralytic ileus takes on a clinical significance if, 72 hours after
laparotomy:
• there has been no return of bowel sounds on auscultation;
• there has been no passage of flatus.
Abdominal distension becomes more marked and tympanitic.
Colicky pain is not a feature.
Distension increases pain from the abdominal wound.
Effortless vomiting may occur.
Radiologically, the abdomen shows gas- filled loops of intestine with multiple
fluid levels (if an erect film is felt necessary).
Clinical features

Paralytic ileus is managed with the use of nasogastric suction and restriction of oral
intake until bowel sounds and the passage of flatus return.
Electrolyte balance must be maintained.
The use of an enhanced recovery programme with early introduction of fluids and
solids is, however, becoming increasingly popular.
In resistant cases, medical therapy with a gastroprokinetic agent, such as
domperidone or erythromycin may be used, provided that an intraperitoneal cause
has been excluded.
Management

If paralytic ileus is prolonged, CT scanning is the most effective
investigation; it will demonstrate any intra-abdominal sepsis or
mechanical obstruction and therefore guide any requirement for
laparotomy.
The need for a laparotomy becomes increasingly likely the longer the
bowel inactivity persists, particularly if it lasts for more than 7 days or if
bowel activity recommences following surgery and then stops again.
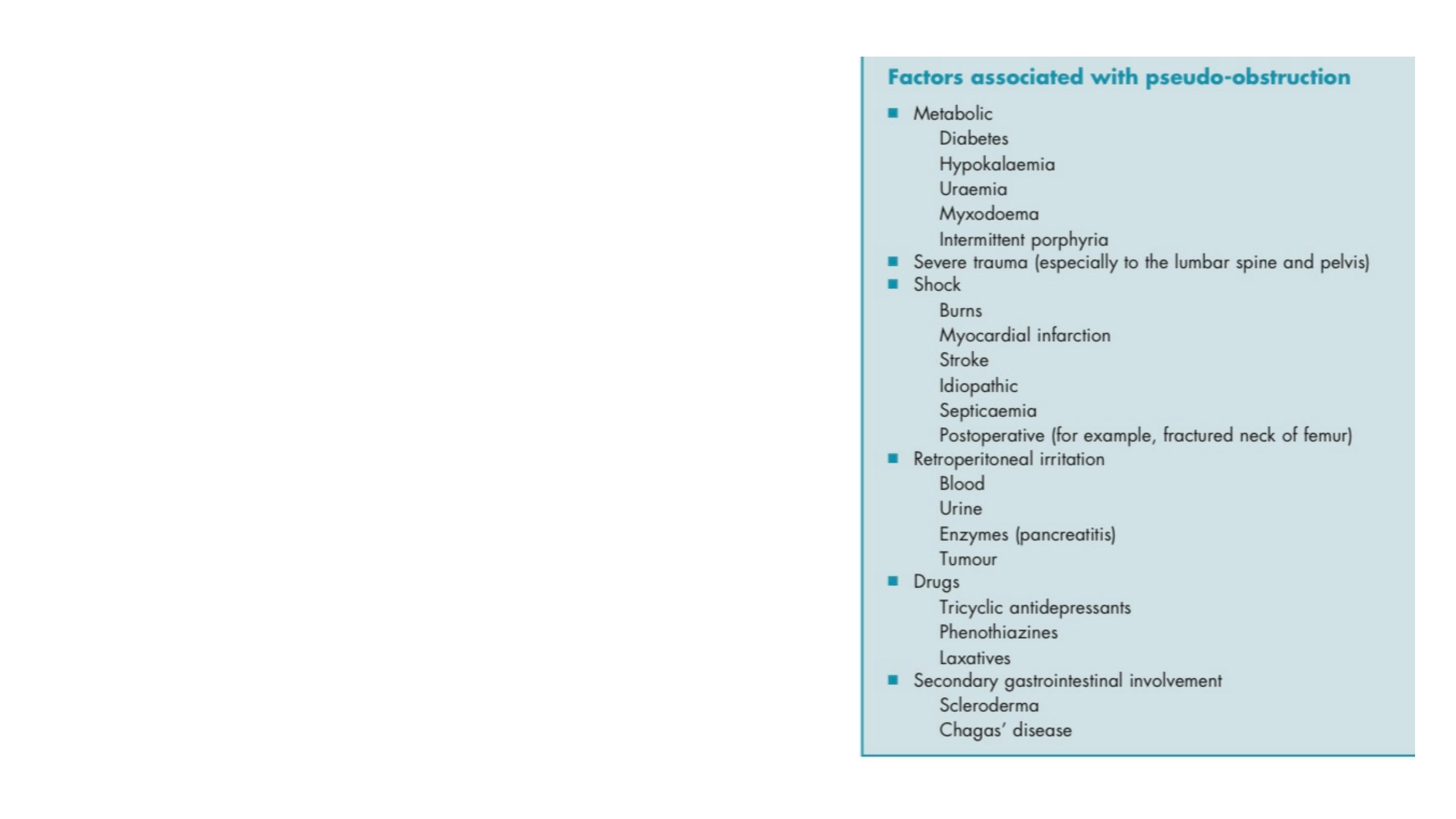
This condition describes an obstruction,
usually of the colon, that occurs in the
absence of a mechanical cause or acute intra-
abdominal disease.
It is associated with a variety of syndromes in
which there is an underlying neuropathy and/
or myopathy and a range of other factors
Pseudo-obstruction

Presents as acute large bowel obstruction.
The absence of a mechanical cause requires urgent confirmation by colonoscopy or
a single-contrast water-soluble barium enema or CT.
Once confirmed, pseudo-obstruction requires treatment of any identifiable cause.
If this is ineffective, intravenous neostigmine should be given.
If neostigmine is not effective, colonoscopic decompression should be performed.
Abdominal examination should pay attention to tenderness and peritonism over the
caecum and as with mechanical obstruction, caecal perforation is more likely if the
caecal diameter is 14 cm or greater.
Surgery is associated with high morbidity and mortality and should be reserved for
those with impending perforation when other treatments have failed or perforation
has occurred.
Ogilvie’s syndrome
