Gall Bladder
Assist. Prof . Dr Salah aljanaby
General surgeon and laparoscopic surgeon
Babylon medical college
Lecture 1
Anatomy
■
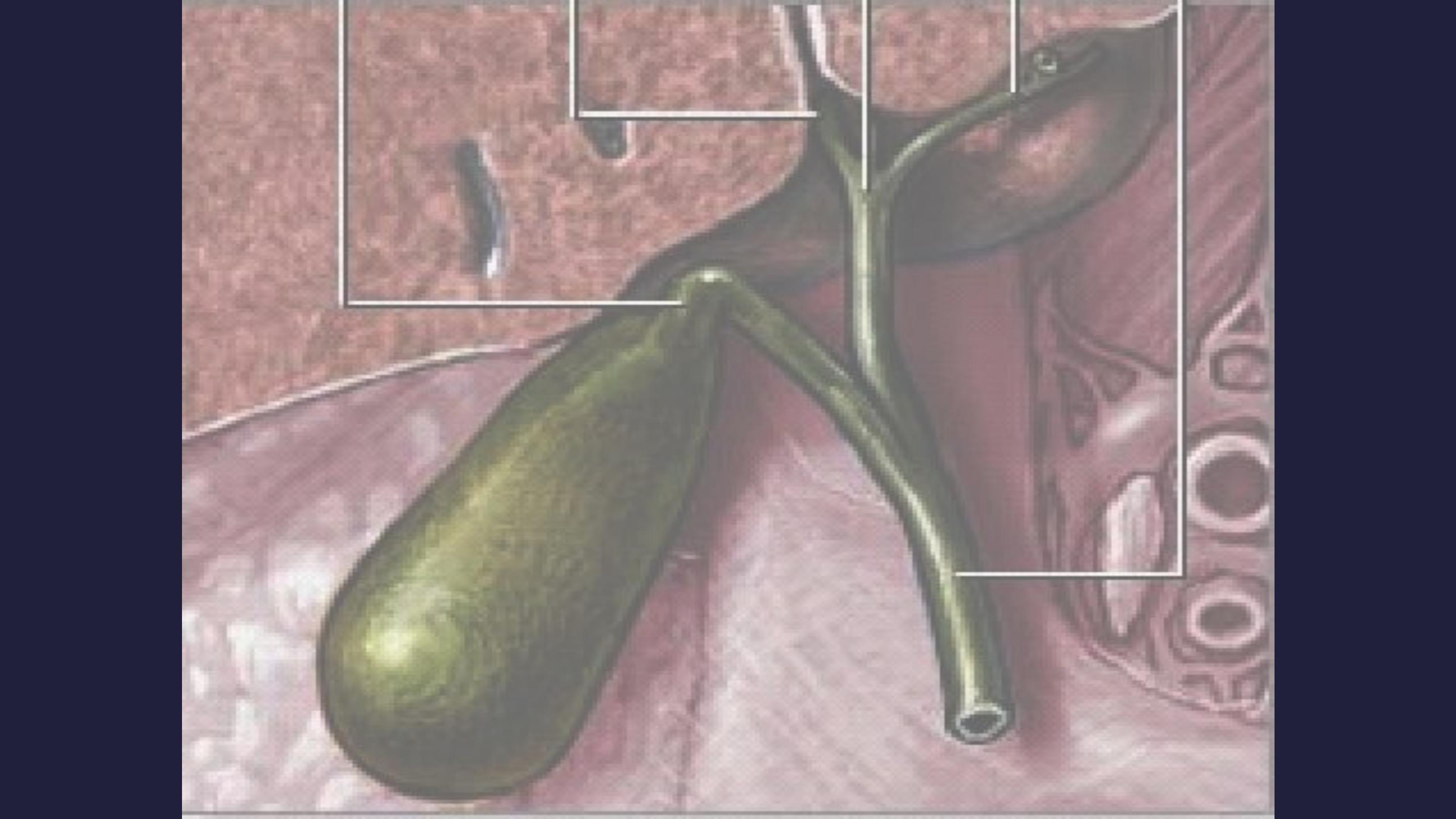
The gallbladder (or
cholecyst,
sometimes gall
bladder) is a pear-
shaped organ that
stores about 50 mL
of bile (or "gall") until
the body needs it for
digestion.
Anatomy
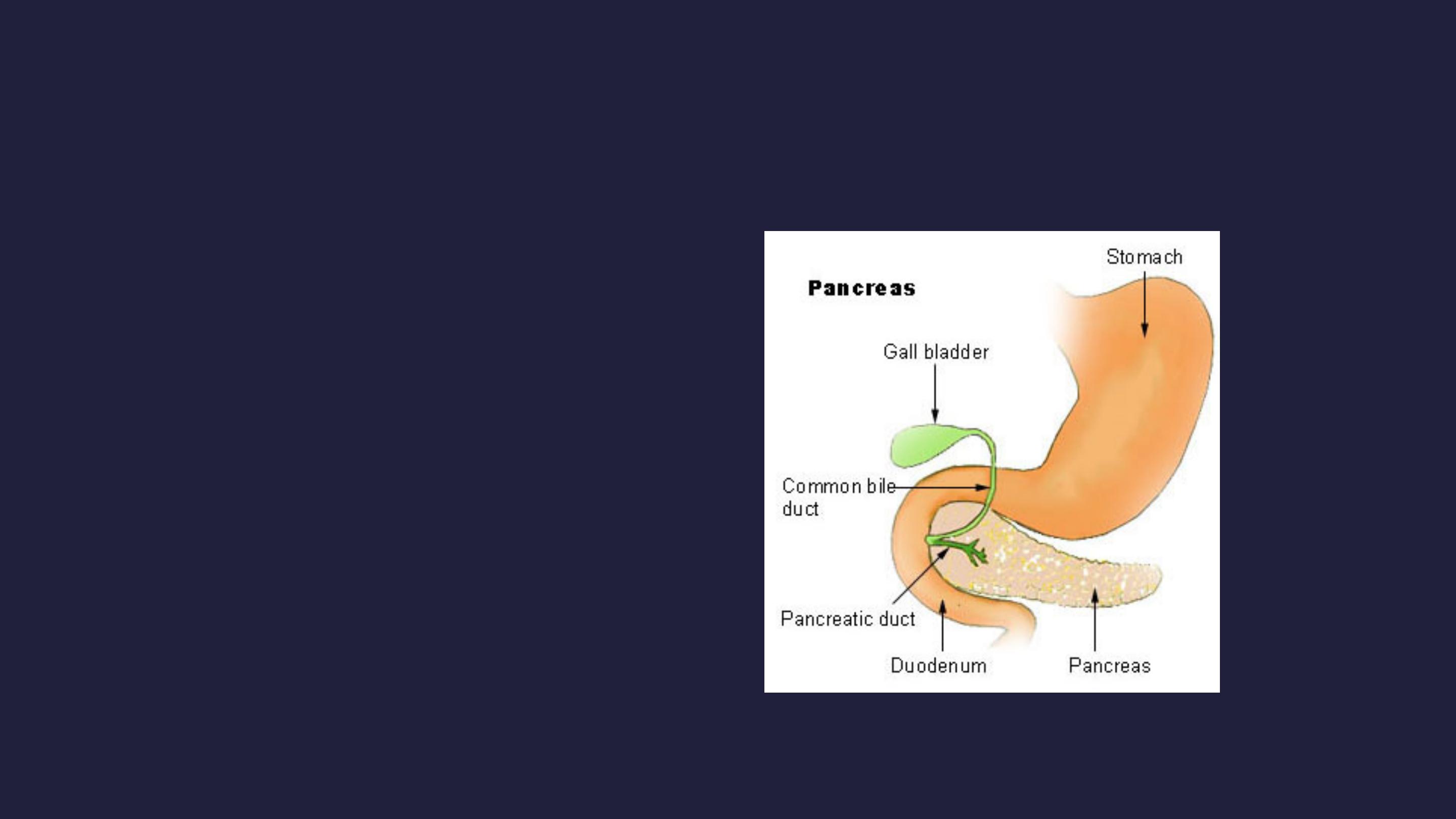
The gallbladder is about 7-10 cm
long in humans and appears
dark green because of its
contents (bile), rather than its
tissue. It is connected to the liver
and the duodenum by the biliary
tract.
■
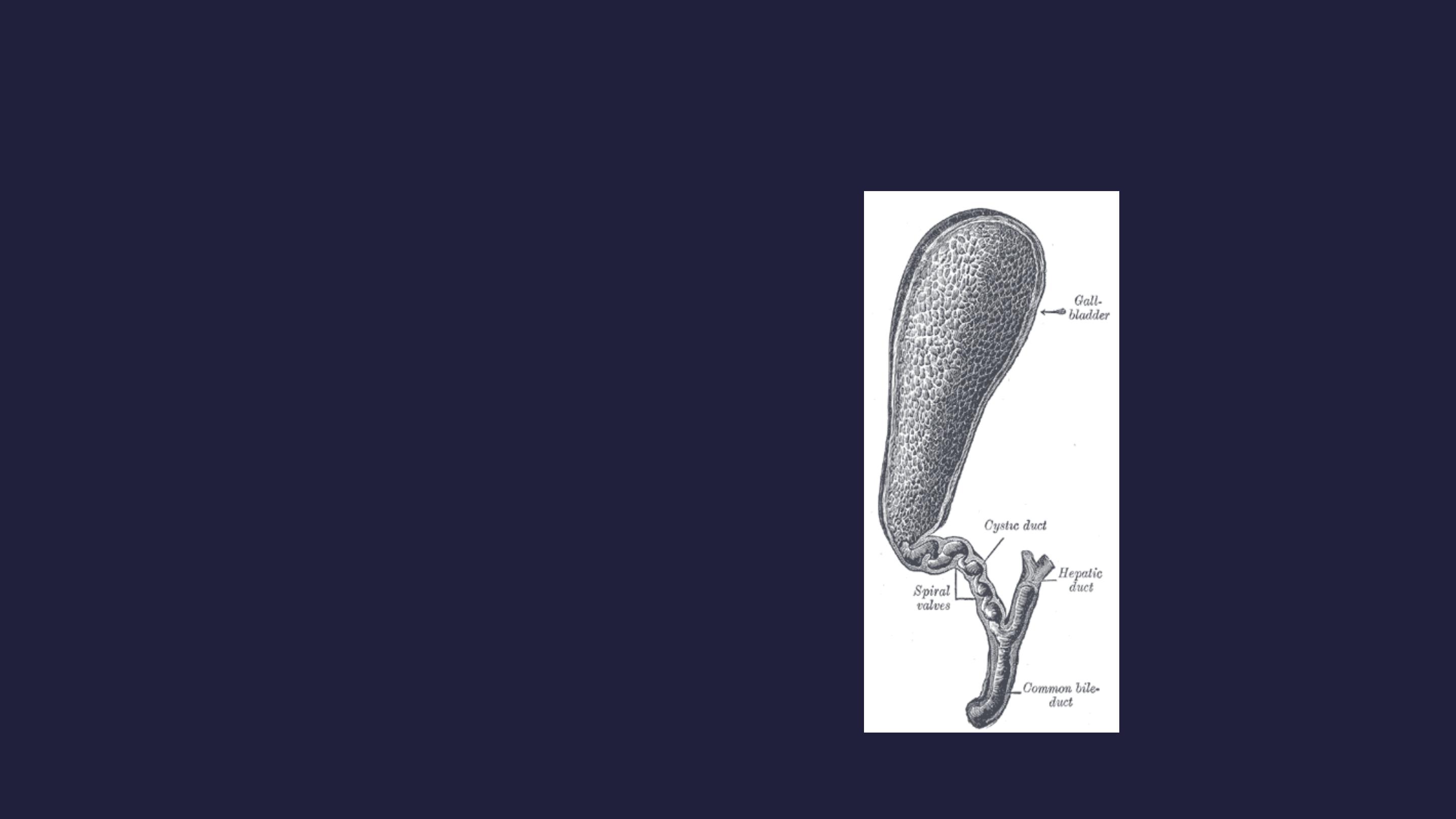
The cystic duct leads from the
gallbladder and joins with the
common hepatic duct to form the
common bile duct.
■
The common bile duct then joins
with the pancreatic duct, and
enters the duodenum through
the hepatopancreatic ampulla at
the major duodenal papilla.
Anatomy
Artery
Cystic artery
Vein
Cystic vein
Nerve
Celiac ganglia, vagus
Precursor
Foregut

Histology
The layers of the gallbladder are as follows:
■
The gallbladder has a simple columnar epithelial lining
characterized by recesses called Aschoff's recesses
(lacunae of Luschka) , which are pouches inside the
lining.
■
Under the epithelium there is a layer of connective
tissue.
■
Beneath the connective tissue is a wall of smooth
muscle that contracts in response to cholecystokinin,
a peptide hormone secreted by the duodenum.
■
There is essentially no submucosa.

Function
■
The gallbladder stores about 50 mL of bile , which is
released when food containing fat enters the digestive
tract, stimulating the secretion of cholecystokinin
(CCK). The bile, produced in the liver, emulsifies fats
and neutralizes acids in partly digested food.
■
After being stored in the gallbladder, the bile becomes
more concentrated than when it left the liver,
increasing its potency and intensifying its effect on
fats. Most digestion occurs in the duodenum.

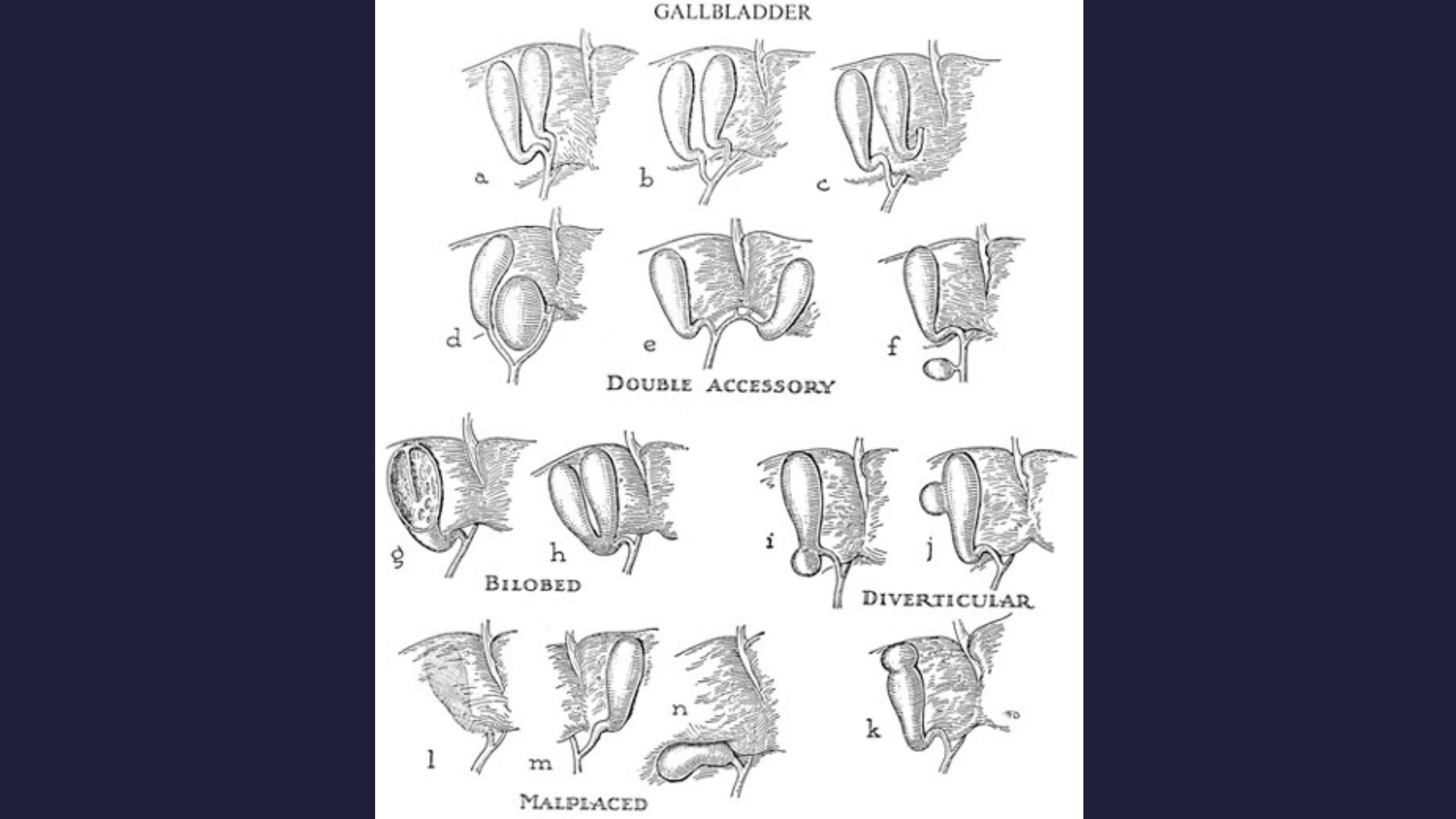
Anomalies
■
The gallbladder may be absent = 0.075%
■
The gallbladder and cystic duct may be absence.
■
the gallbladder is irregular in form or constricted
across its middle; more rarely, it is partially divided in
a longitudinal direction.
■
two distinct gallbladders, each having a cystic duct
that joined the hepatic duct. (0.026%), The cystic duct
may itself be doubled
■
The gallbladder has been found on the left side (to the
left of the ligamentum teres) in subjects in whom there
was no general tranposition of the thoracic and
abdominal viscera.

■
The gallbladder may be intrahepatic or
beneath the left lobe. Ectopic sites include
retrohepatic positions, or in the anterior
abdominal wall or falciform ligament, they may
be suprahepatic or transversely position,
floating, or retroperitoneal. They may be in the
midline anterior epigastric above the left lobe
or suprahepatic above the right hepatic lobe.

Choledochal cyst
■
Choledochal cysts are congenital anomalies of the
bile ducts. They consist of cystic dilatations of the
extrahepatic biliary tree, intrahepatic biliary radicles,
or both.
■
Douglas is credited with the first clinical report in a 17-
year-old girl who presented with intermittent
abdominal pain, jaundice, fever, and a palpable
abdominal mass.
■
Pathophysiology: The pathogenesis of choledochal
cysts is most likely multifactorial.
■
A congenital etiology,
■
A congenital predisposition to acquiring the disease under
the right conditions.

■
The vast majority of patients with choledochal
cysts have an anomalous junction of the
common bile duct with the pancreatic duct
(anomalous pancreatobiliary junction [
APBJ
]).
An APBJ is characterized when the pancreatic
duct enters the common bile duct 1 cm or
more proximal to where the common bile duct
reaches the ampulla of Vater.
■
APBJs in more than 90% of patients with
choledochal cysts.

■
The APBJ allows pancreatic secretions and
enzymes to reflux into the common bile duct.
In the relatively alkaline conditions found in
the common bile duct, pancreatic pro-
enzymes can become activated. This results
in inflammation and weakening of the bile duct
wall. Severe damage may result in complete
denuding of the common bile duct mucosa.

■
From a congenital standpoint, defects in
epithelialization and recanalization of the
developing bile ducts during organogenesis
and congenital weakness of the duct wall have
also been implicated. The result is formation
of a choledochal cyst.

Anatomy of Choledochal cyst
based on the Todani classification published in 1977.
■
Type I choledochal cysts
■
most common ; 80-90% of the lesions.
■
Type I cysts are dilatations of the entire common hepatic
and common bile ducts or segments of each.
■
They can be saccular or fusiform in configuration.
■
Type II choledochal cysts
■
isolated protrusions or diverticula that project from the
common bile duct wall. They may be sessile or may be
connected to the common bile duct by a narrow stalk.
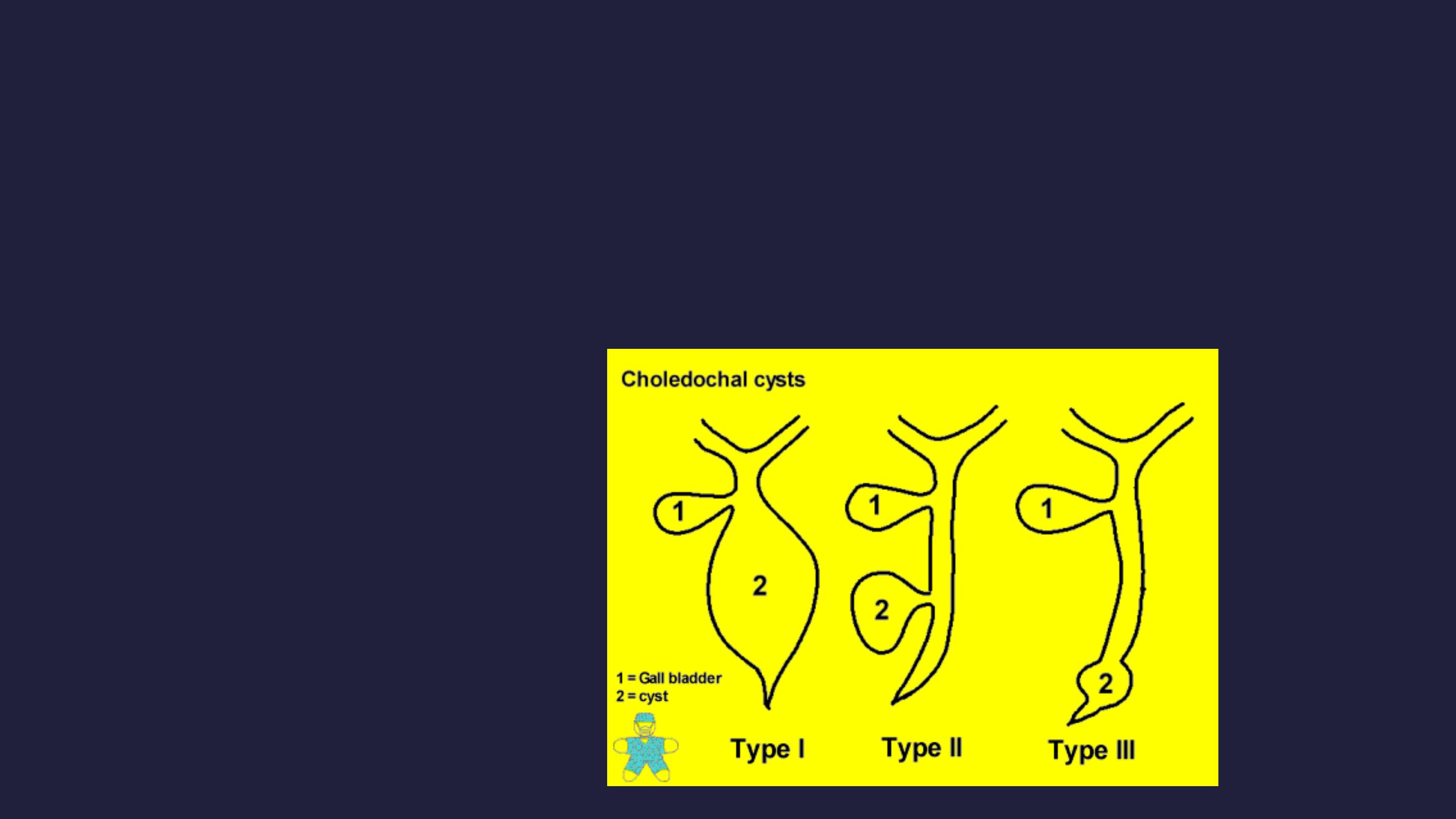
■
Type III choledochal cysts are found in the
intraduodenal portion of the common bile duct.
Another term used for these cysts is choledochocele.

■
Type IVA cysts are characterized by multiple dilatations of the
intrahepatic and extrahepatic biliary tree. Most frequently, a large
solitary cyst of the extrahepatic duct is accompanied by multiple
cysts of the intrahepatic ducts. Type IVB choledochal cysts
consist of multiple dilatations that involve only the extrahepatic
bile duct.
■
Type V choledochal cysts are defined by dilatation of the
intrahepatic biliary radicles. Often, numerous cysts are present
with interposed strictures that predispose the patient to
intrahepatic stone formation, obstruction, and cholangitis. The
cysts are typically found in both hepatic lobes. Occasionally,
unilobar disease is found and most frequently involves the left
lobe.

■
The patient may present at any age with
1.
Obstructive jaundice
2.
Cholangitis and
3.
Abd signs, with RUQ swelling in some cases
■
It is a premalignant condition
■
Diagnosis by US and MRI
■
Radical excision of the cyst is the treatment
of choice with Roux – en –Y reconstruction

Gall stones
■
Gall stones are the most common abdominal reason
for admission to hospital in developed countries and
account for an important part of healthcare
expenditure. Around 5.5 million people have gall
stones in the United Kingdom, and over 50 000
cholecystectomies are performed each year.
■
Normal bile consists of 70% bile salts (mainly cholic
and chenodeoxycholic acids), 22% phospholipids
(lecithin), 4% cholesterol, 3% proteins, and 0.3%
bilirubin.
■
There are two major types of gallstones, which seem
to form due to distinctly different pathogenetic
mechanisms.

Cholesterol Stones
■
About 90% of gallstones are of this type.
These stones can be either;
■
almost pure cholesterol {Cholesterol stones}
■
or mixtures of cholesterol and other
substances{ cholesterol predominant (mixed)
stones}.

■
The key event leading to formation and
progression of cholesterol stones is
precipitation of cholesterol in bile.
■
Unesterified cholesterol is virtually insoluble
in aqueous solutions and is kept in solution
in bile largely by virtue of the detergent-like
effect of bile salts.

Imbalance lead to stone formation
■
Hyper-secretion of cholesterol into bile due to
■
obesity,
■
acute high calorie intake,
■
chronic polyunsaturated fat diet, contraceptive
steroids or pregnancy,
■
diabetes mellitus and
■
certain forms of familial hypercholesterolemia.

■
Hypo-secretion of bile salts due to
■
impaired bile salt synthesis and
■
abnormal intestinal loss of bile salts (e.g. recirculation
failure due to ileal disease).
■
Impaired gallbladder function with incomplete
emptying or stasis.
■
seen in late pregnancy
■
with oral contraceptive use,
■
in patients on total parenteral nutrition and
■
due to unknown causes, perhaps associated with neuro-
endocrine dysfunction.
