Male genital tract pathology
Lecture 2
Prostatic pathology
Dr.Ahmed Raji
F.I.C.M.Path
College of Medicine - University of Babylon
29.6.2020

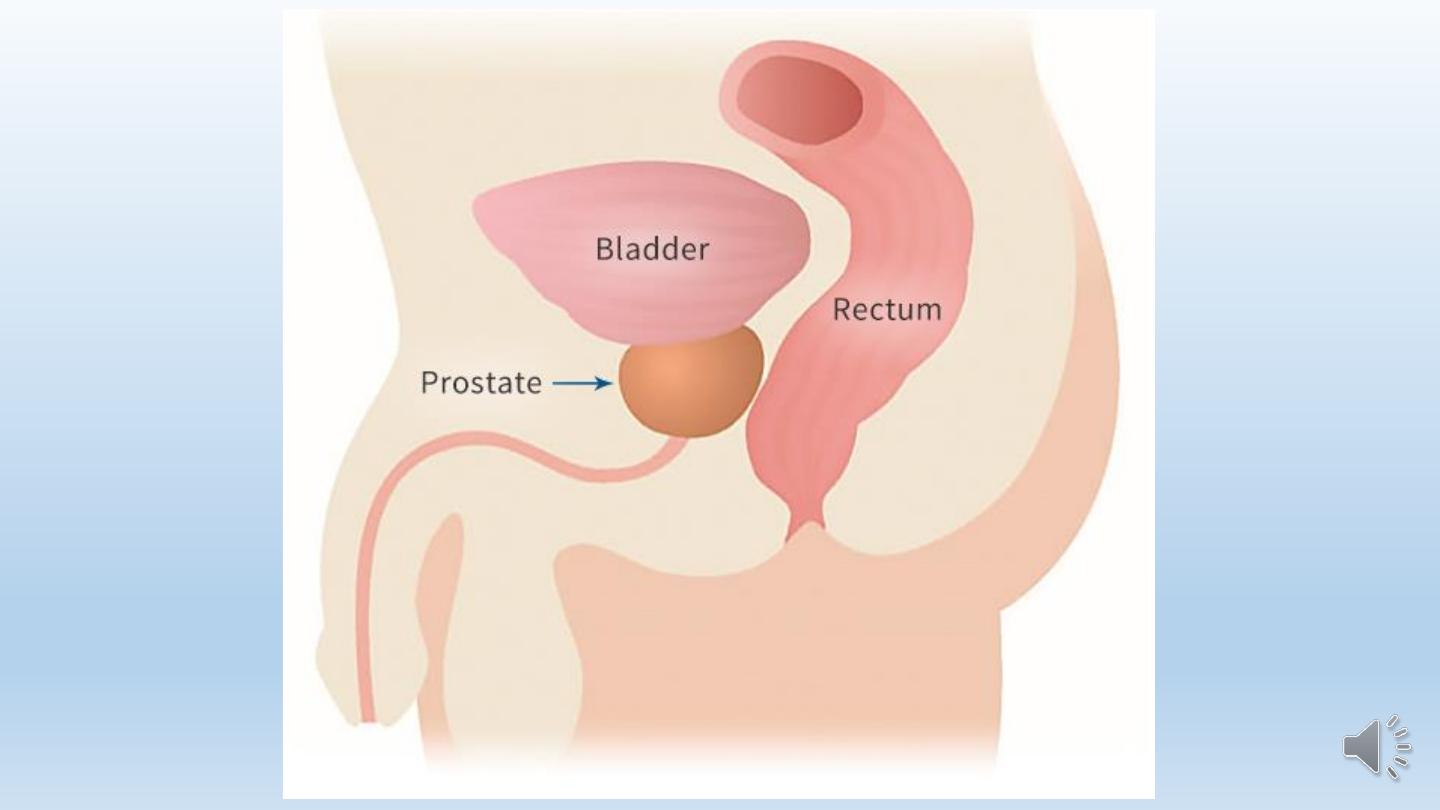
The prostate is a fibromuscular glandular organ that surrounds the
prostatic urethra.
It is about 3 cm long and lies between the neck of the bladder above and
the urogenital diaphragm below.
A fibrous capsule surrounds the prostate.
The somewhat conical prostate has a base, which lies against the bladder
neck above, and an apex, which lies against the urogenital diaphragm
below.
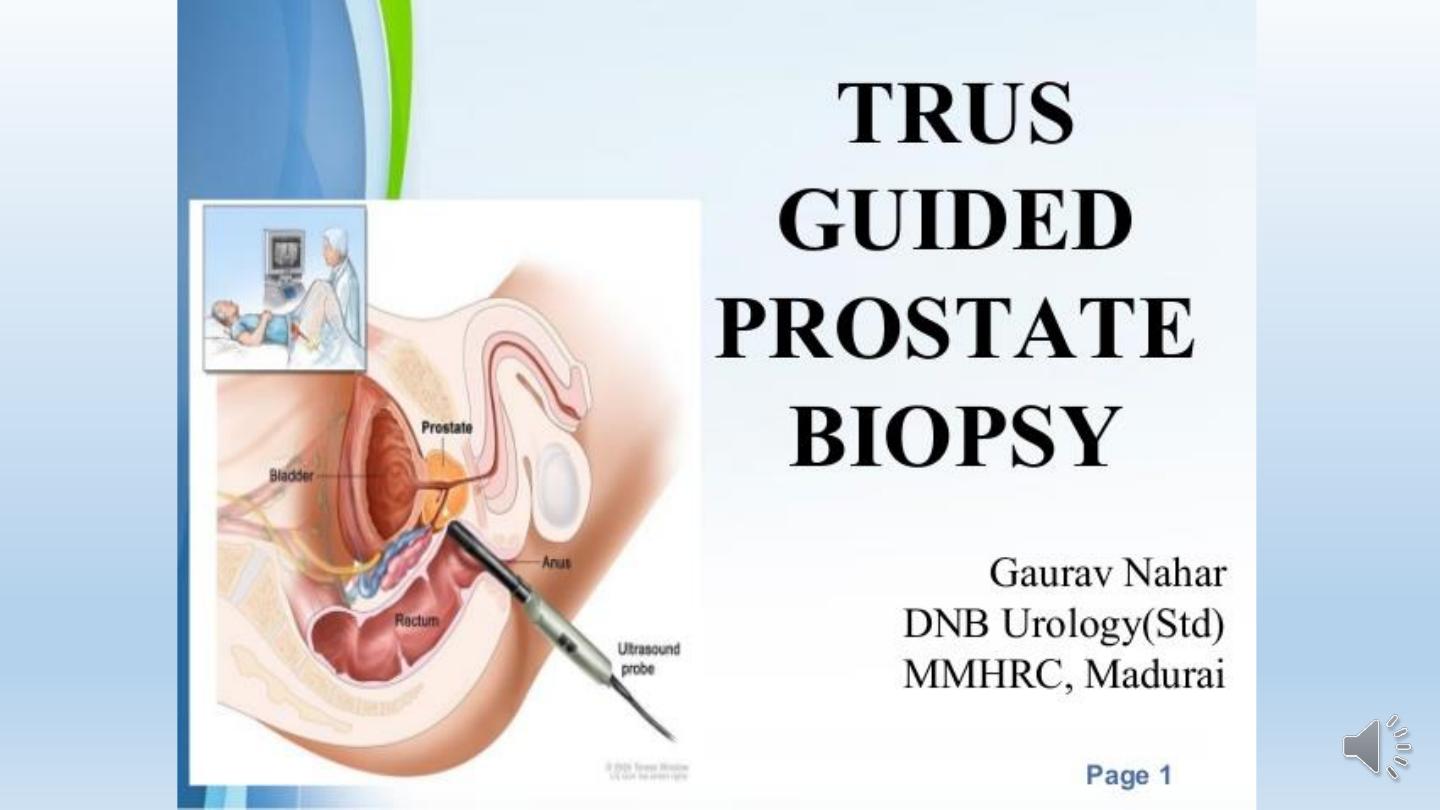
Posteriorly: the prostate is closely related to the anterior surface of the
rectal ampulla and is separated from it by the rectovesical septum.
Benign Prostatic Hyperplasia (BPH) or Nodular Hyperplasia
BPH is an extremely common disorder in men over age 50.
It is characterized by hyperplasia of prostatic stromal and epithelial
cells.
BPH can be seen in approximately 20% of men 40 years of age, a
figure that increases to 70% by age 60 and to 90% by age 80.
Only 25% of those who have microscopic evidence of BPH develop
clinical symptoms.

Etiology.
It is believed that the main cause of BPH is impaired cell death.
The overall reduction of the rate of cell death, resulting in the
accumulation of aged cells in the prostate.
The main androgen in the prostate, is
dihydrotestosterone
(DHT). It is
formed in the prostate from the conversion of testosterone by the
enzyme type 2
5α-reductase
. It is believed that DHT-induced growth
factors like fibroblast growth factor (FGF) family, particularly FGF-7,
FGFs 1 and 2, and TGFβ increase the proliferation of stromal cells and
decreasing the death of epithelial cells.
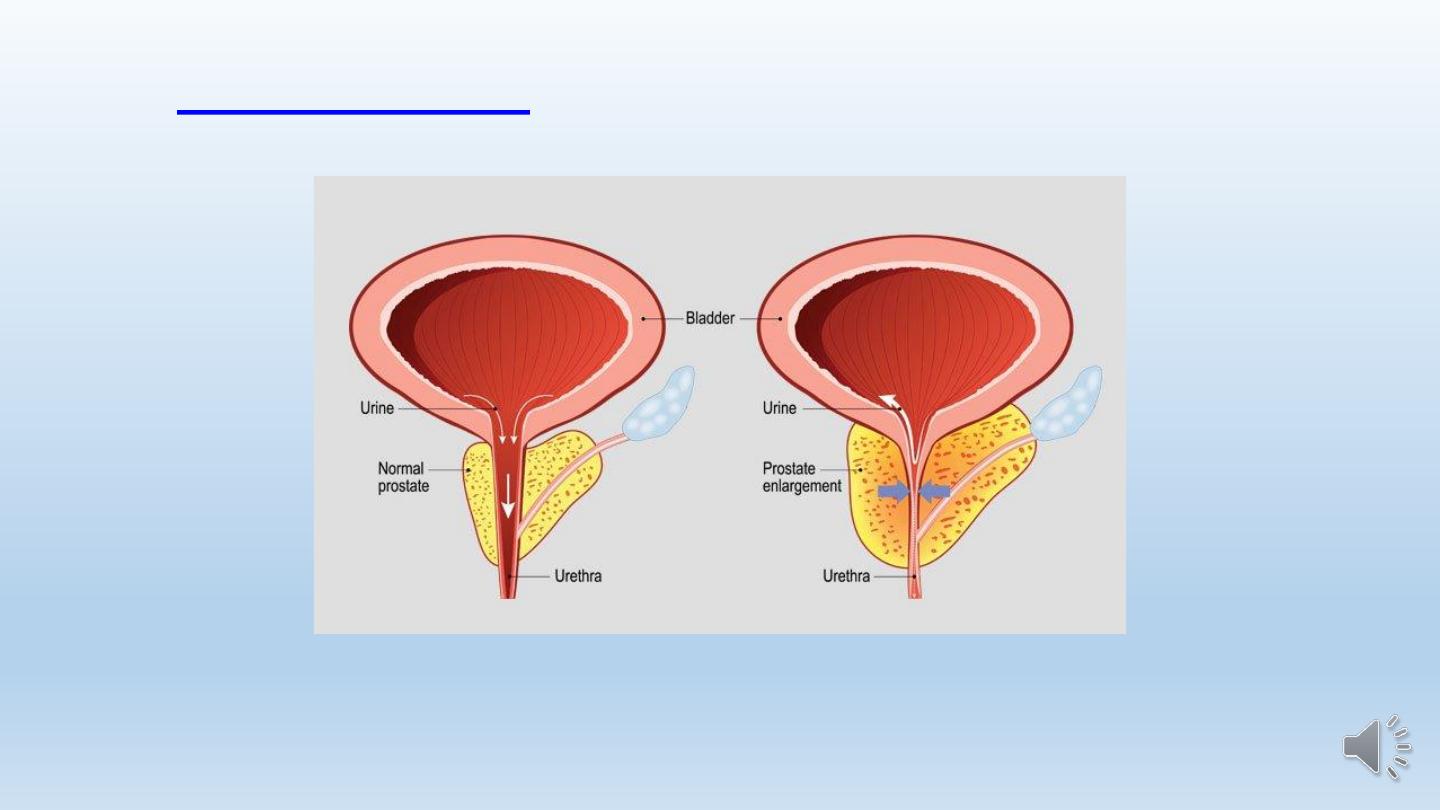
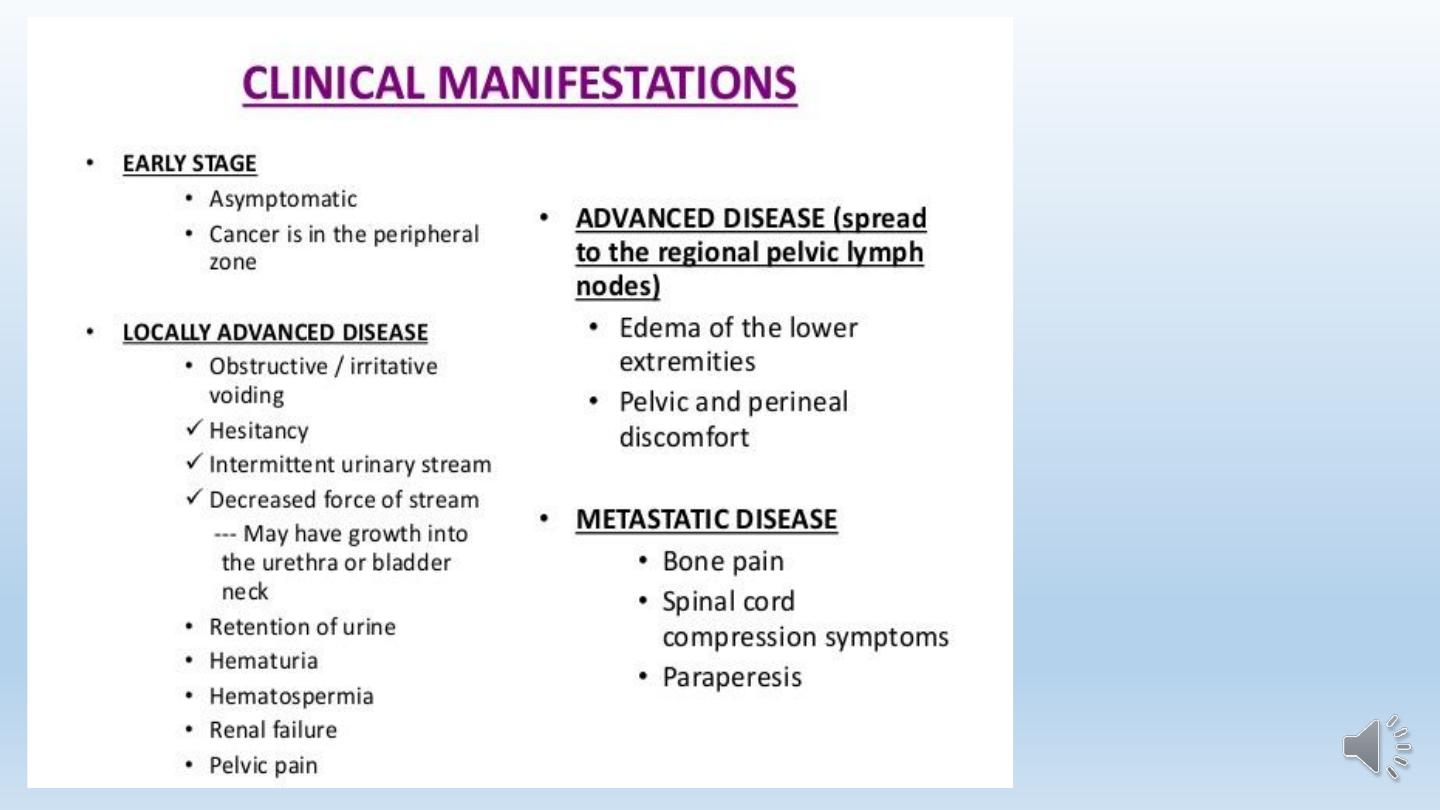
Clinical features:

Clinical features:
1- Nocturia, which is the need to urinate two or more times per night.
2- Dribbling at the end of urinary stream.
3- Incontinence.
4- The need to strain when urinating.
5- A weak urinary stream.
6- Urgency.
7- A slowed or delayed urinary stream.
8- Dysuria.
9- Hematuria .
Morphology.
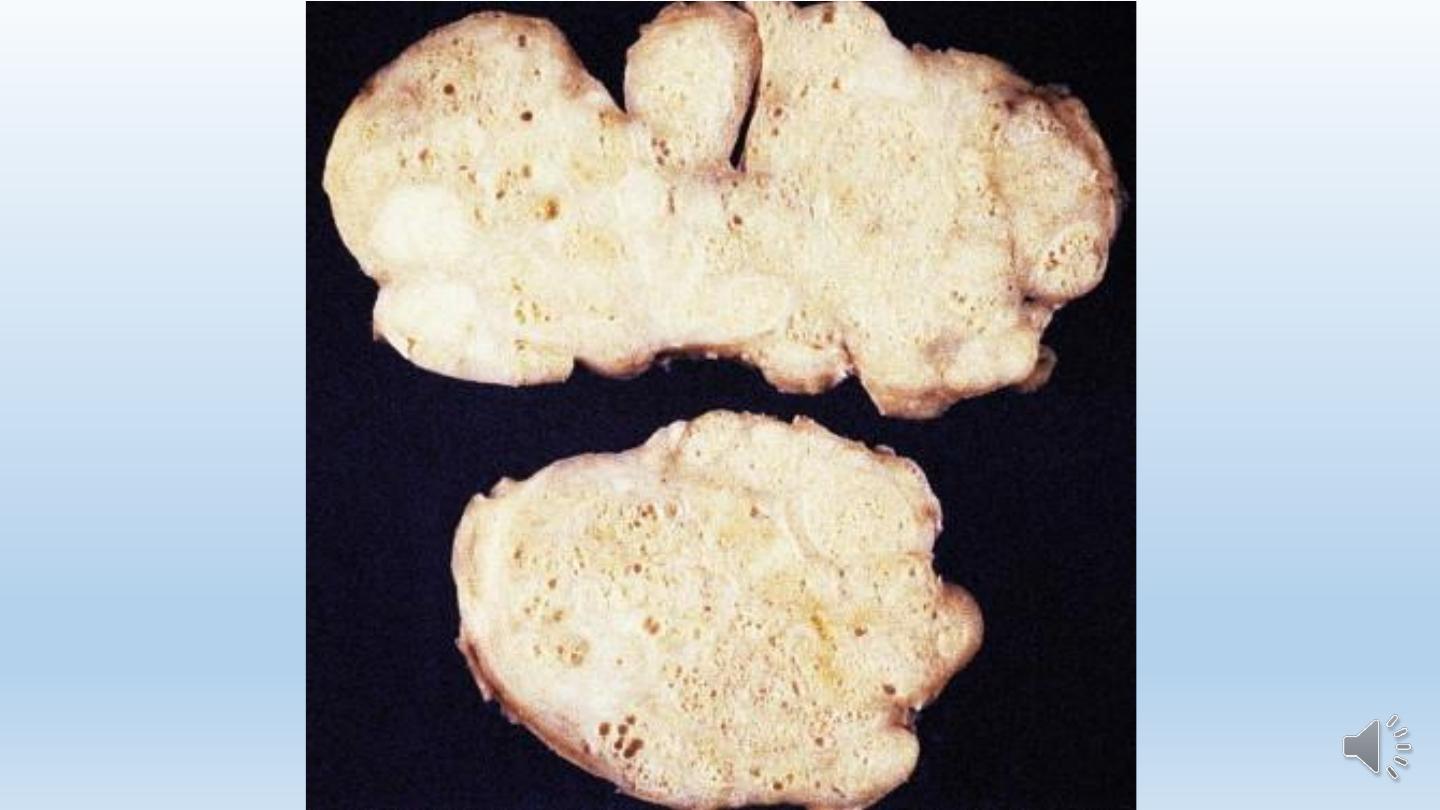
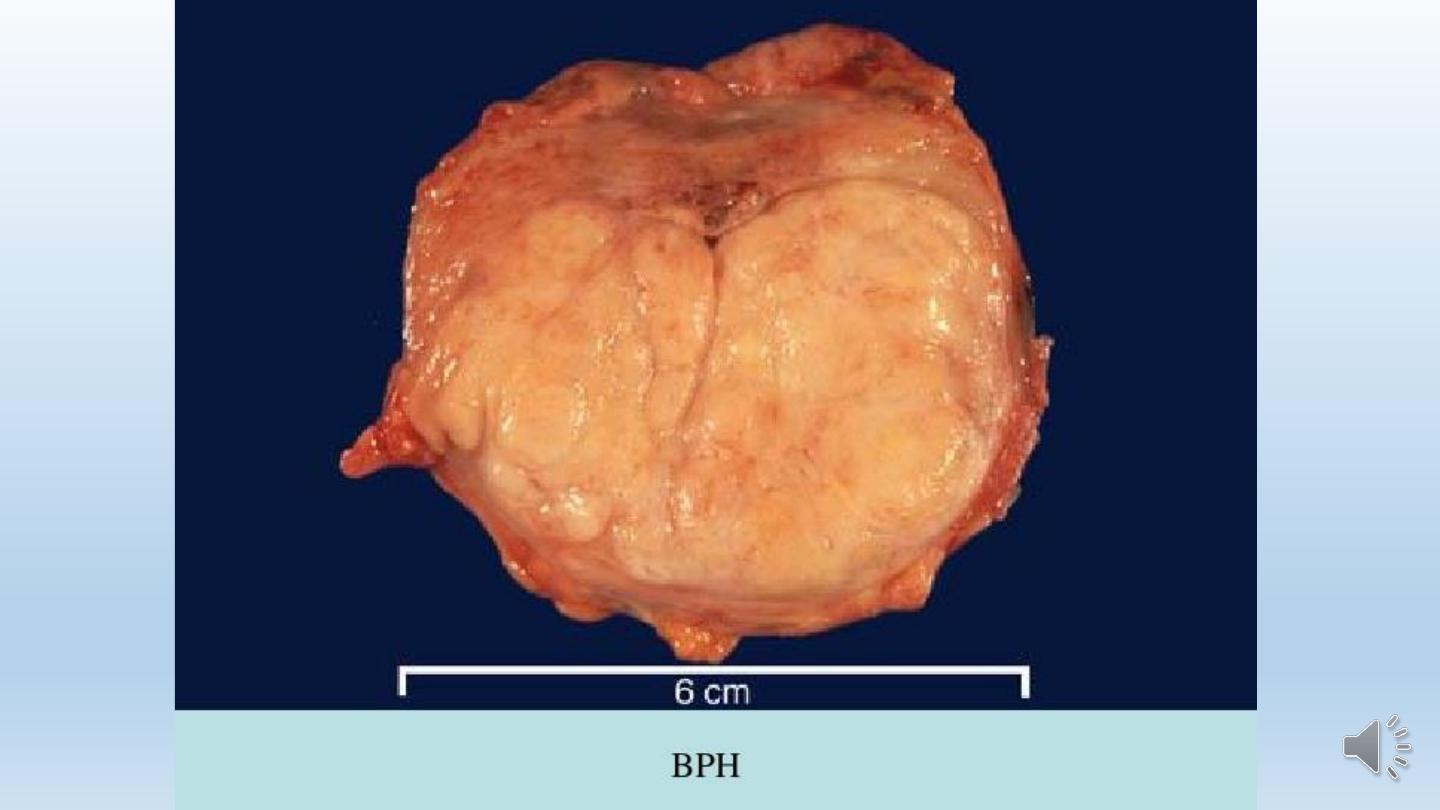
Grossly
1- The prostate weighs between 60 and 100 gm.
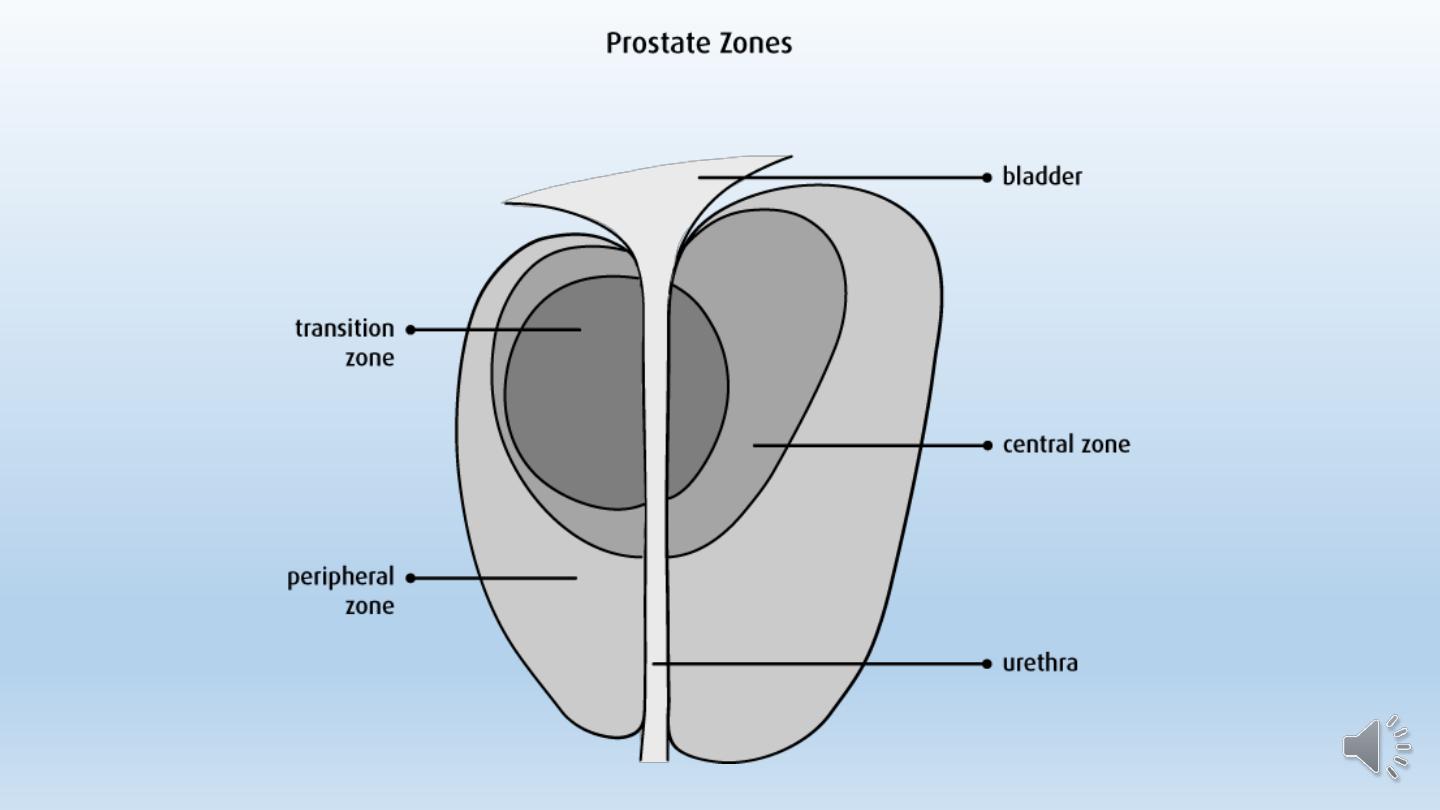
2- Nodular hyperplasia of the prostate originates almost
exclusively in the inner aspect of the prostate gland.
3- On cross-section, the nodules vary in color and
consistency.
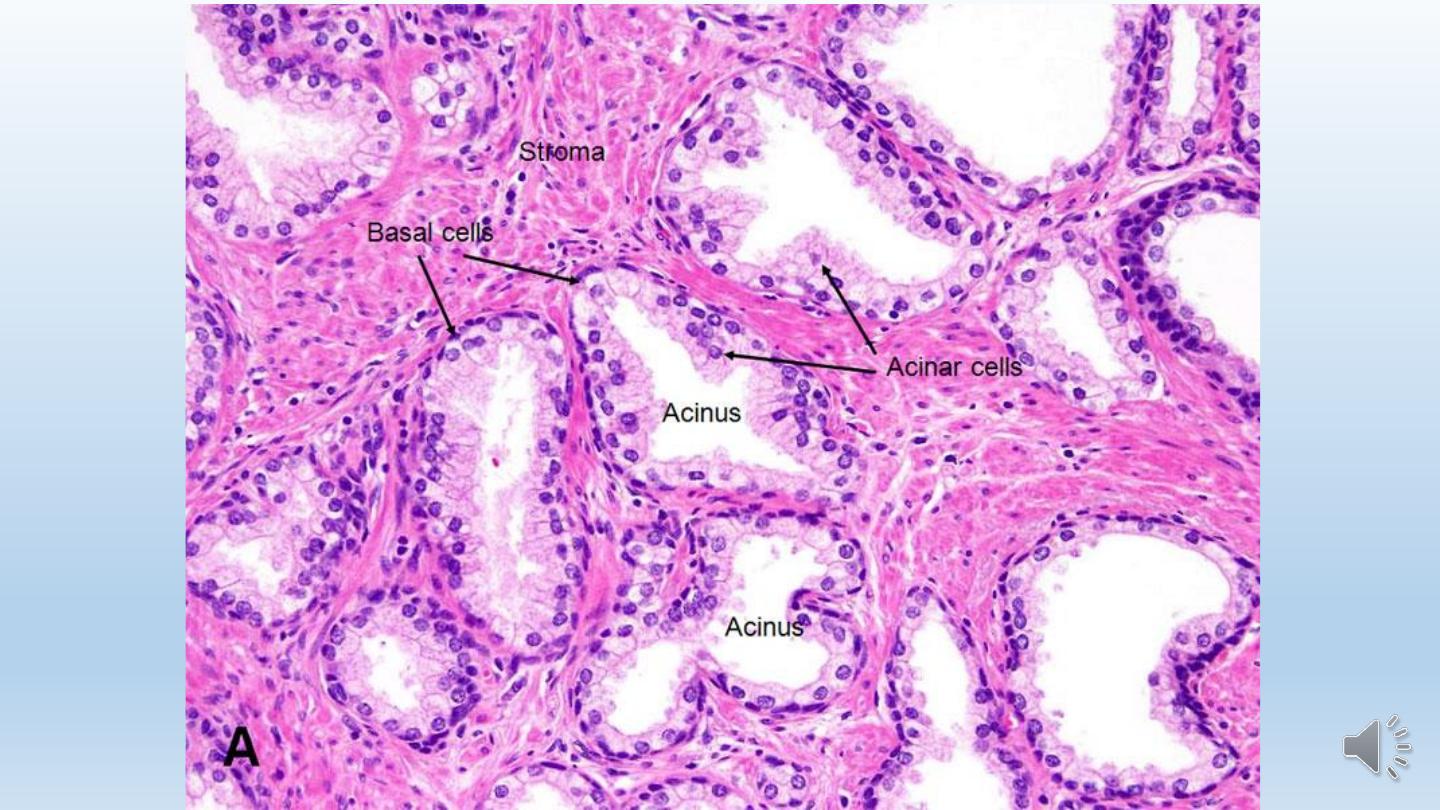
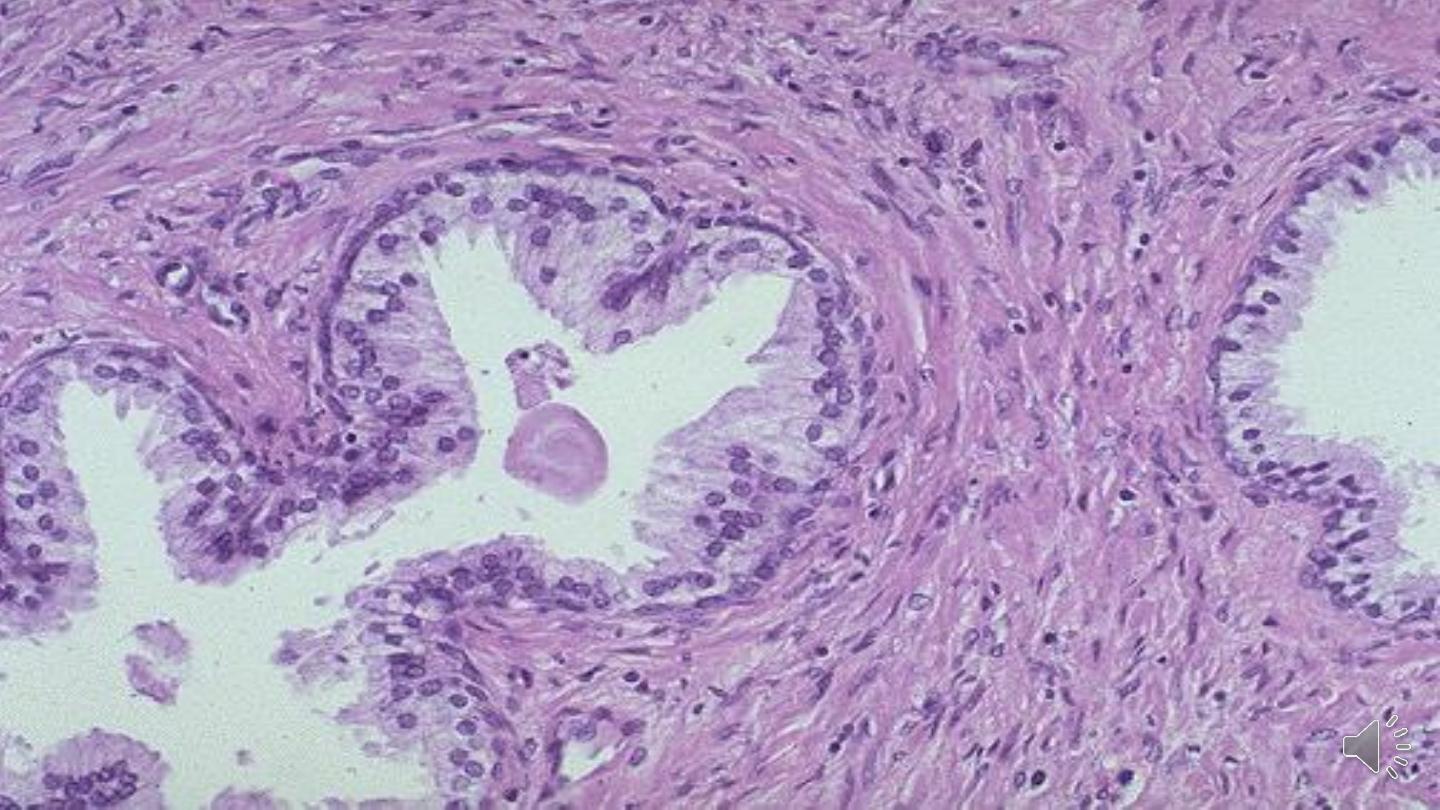
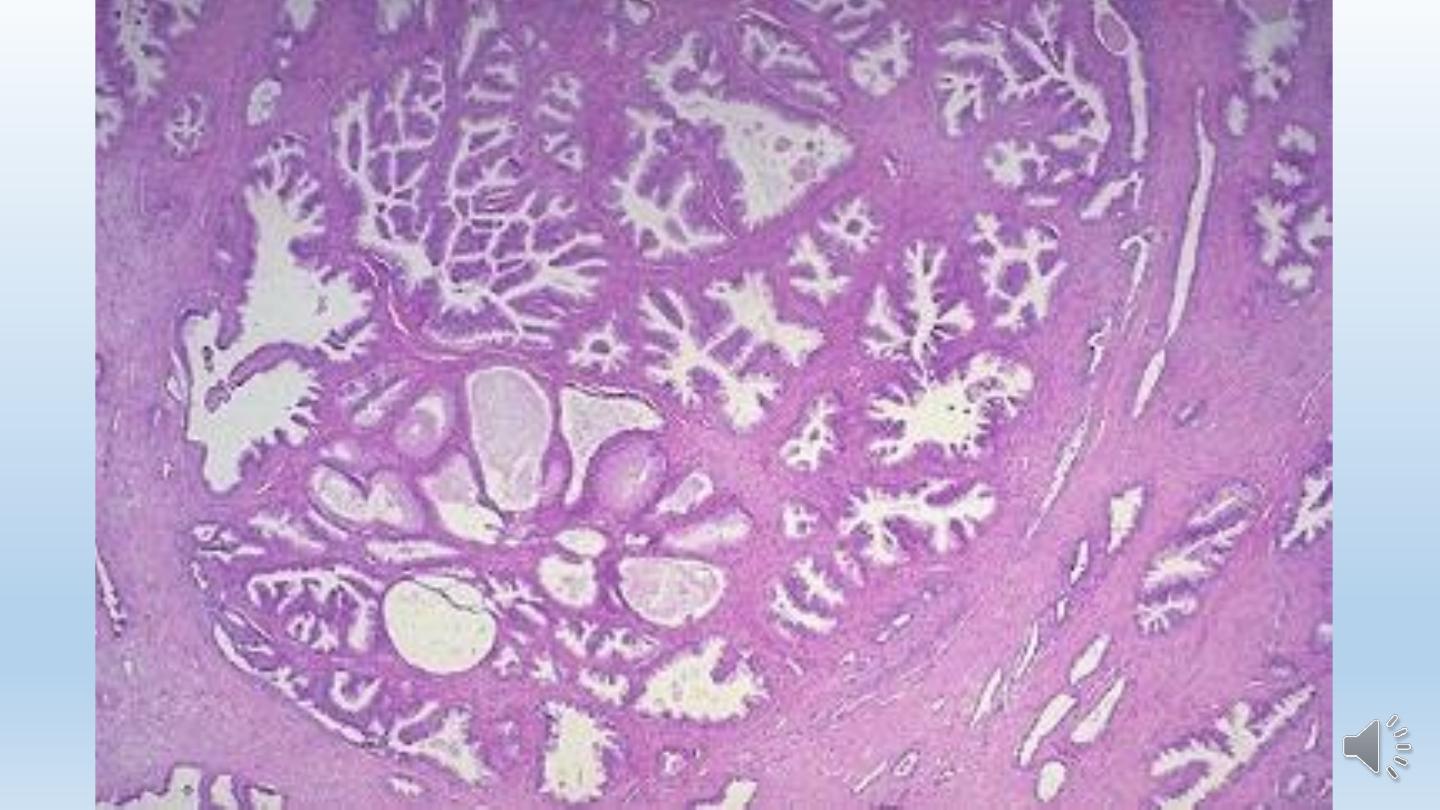
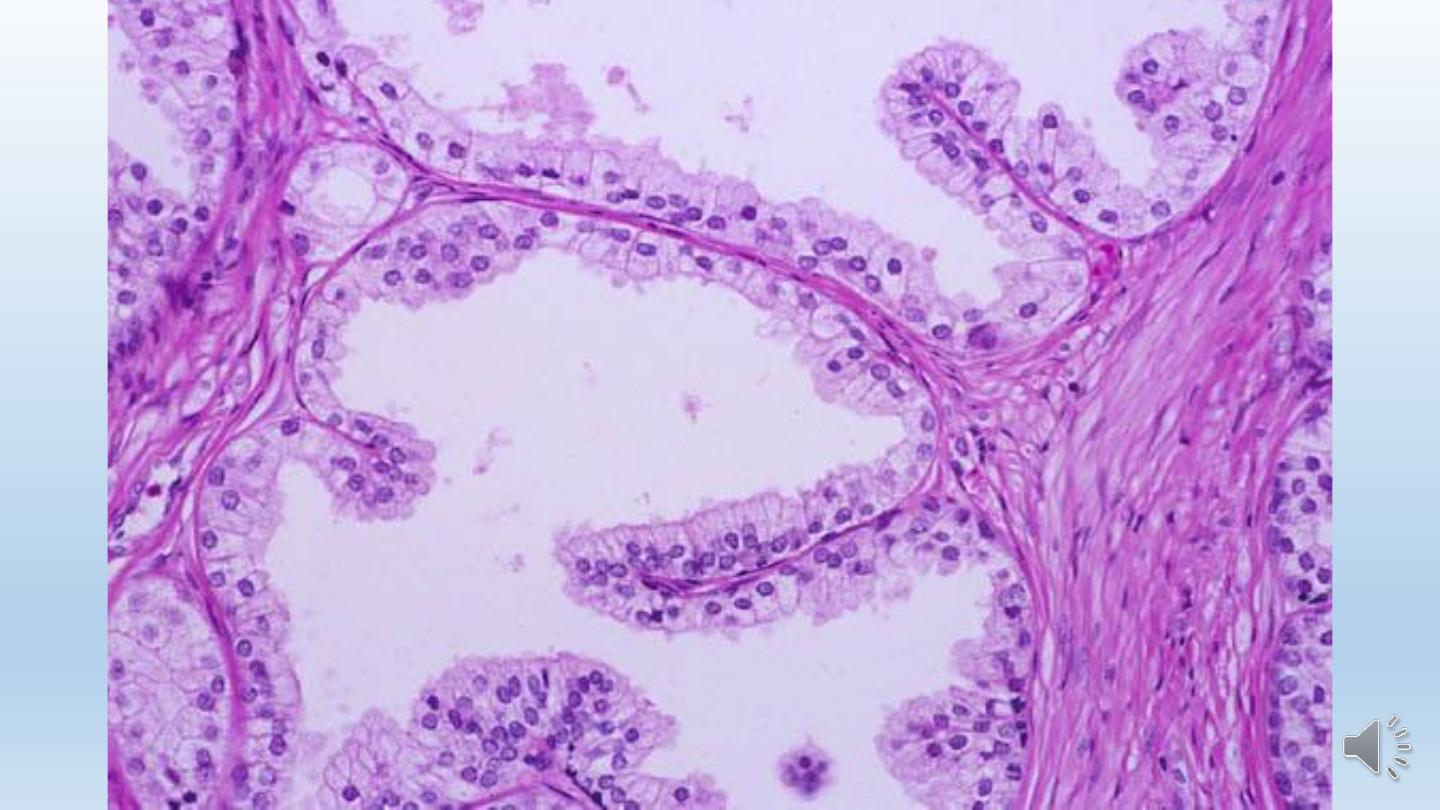
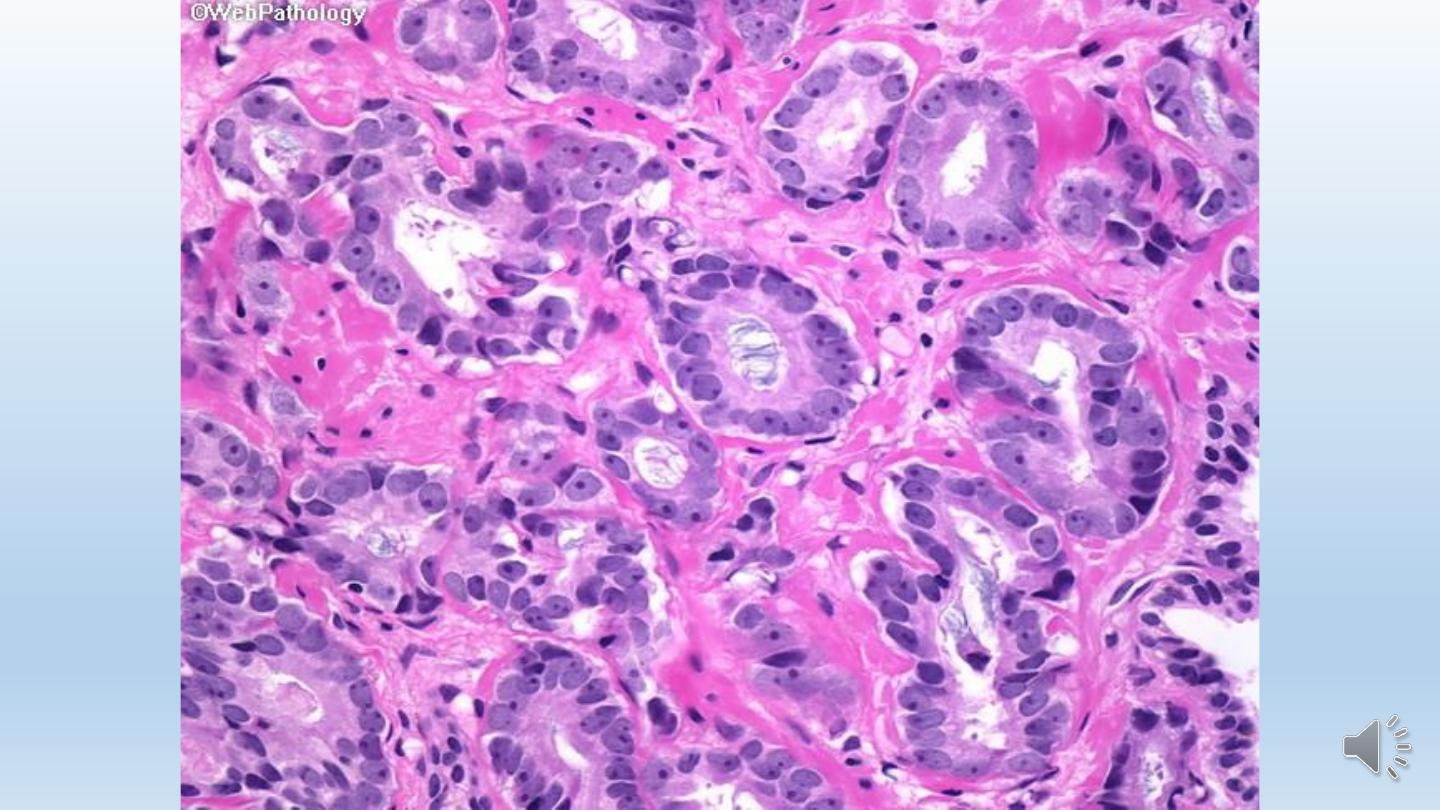
Microscopically
1- Nodular appearance.
2- The composition of the nodules ranges from purely stromal
fibromuscular nodules to fibroepithelial nodules.
3- Glands range from small to large to cystically dilated glands,
lined by two layers, an inner columnar and an outer cuboidal or
flattened epithelium.
Tumors
Adenocarcinoma
Adenocarcinoma of the prostate is one of the most common
form of cancer in men. There is a one in six lifetime probability
of being diagnosed with prostate cancer. Cancer of the prostate
is typically a disease of men over age 50.Prostatic cancer is
uncommon in Asians and occurs most frequently among blacks.

Etiology.
1-Environmental factors, for example, increased consumption of fats has
been implicated. Other dietary products suspected of preventing or
delaying prostate cancer development include lycopenes (found in
tomatoes), selenium, soy products, and vitamin D.
2-Androgens play an important role in prostate cancer. The growth and
survival of prostate cancer cells depends on androgens.
3-Family history, men with one first-degree relative with prostate cancer
have twice the risk and those with two first-degree relatives have five
times the risk of developing prostate cancer.
Prostatic specific antigen
(PSA)

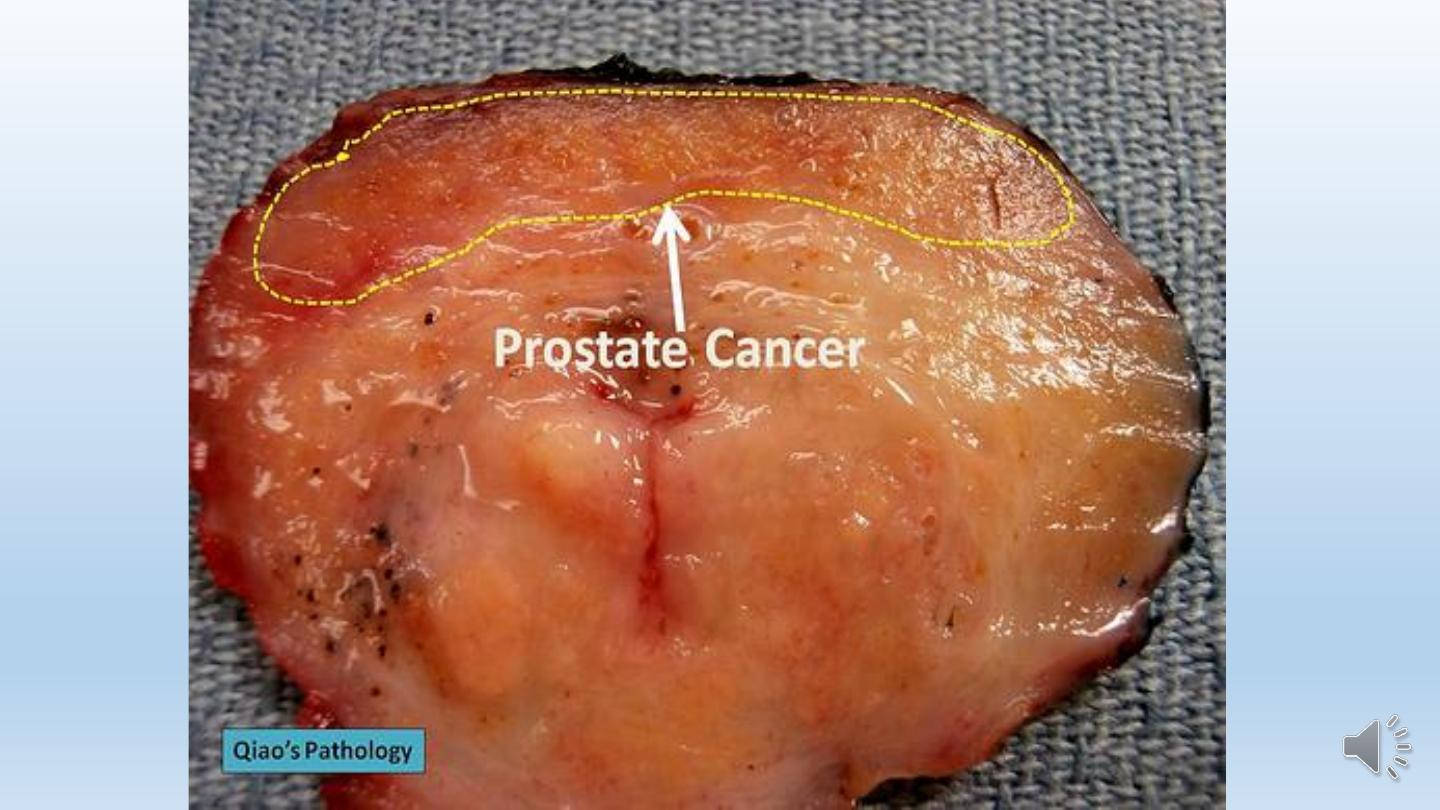
Morphology.
Grossly
On cross-section of the prostate the neoplastic tissue is gritty
and firm, but when embedded within the prostatic substance
it may be extremely difficult to visualize and be more readily
apparent on palpation.


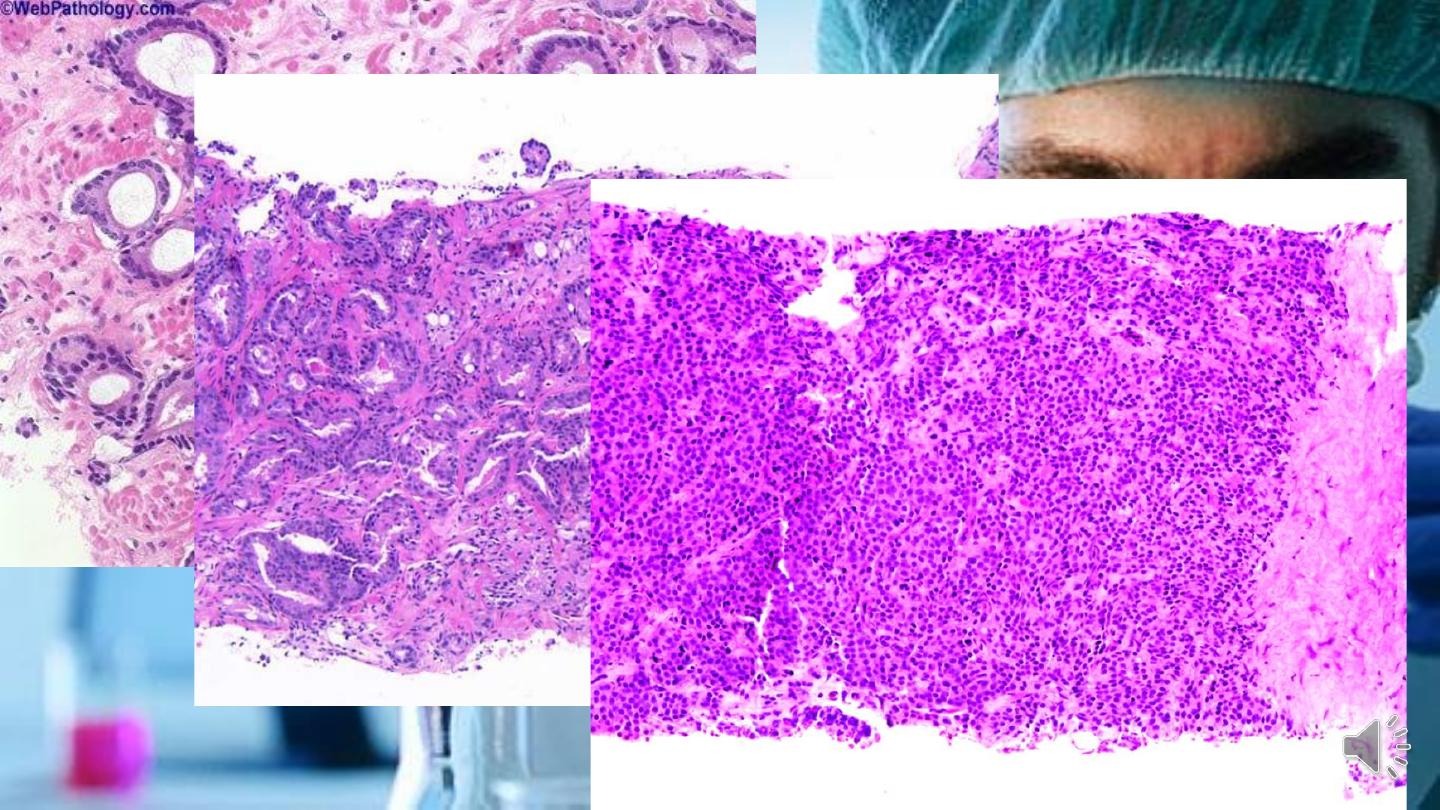
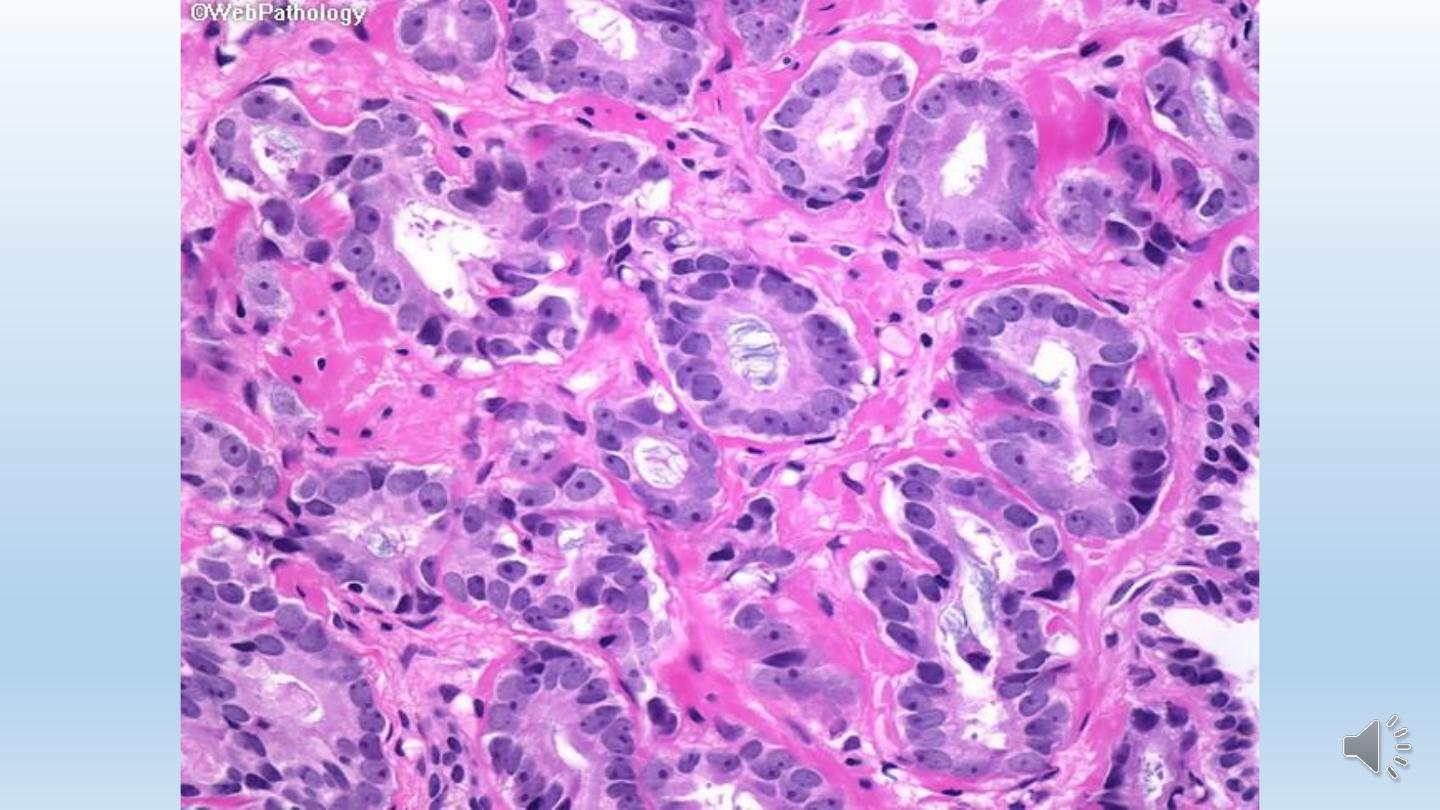
Histologically
1- Most lesions are adenocarcinomas that produce well-defined, glandular patterns.
2- The glands are typically smaller than benign glands and are lined by a single uniform
layer of cuboidal or low columnar epithelium. In contrast to benign glands, prostate
cancer glands are more crowded, and characteristically lack branching and papillary
infolding.
3-Nuclei are large and often contain one or more large nucleoli. There is some variation
in nuclear size and shape, but in general pleomorphism is not marked.
4-The outer basal cell layer typical of benign glands is absent.
5- Mitotic figures are uncommon.

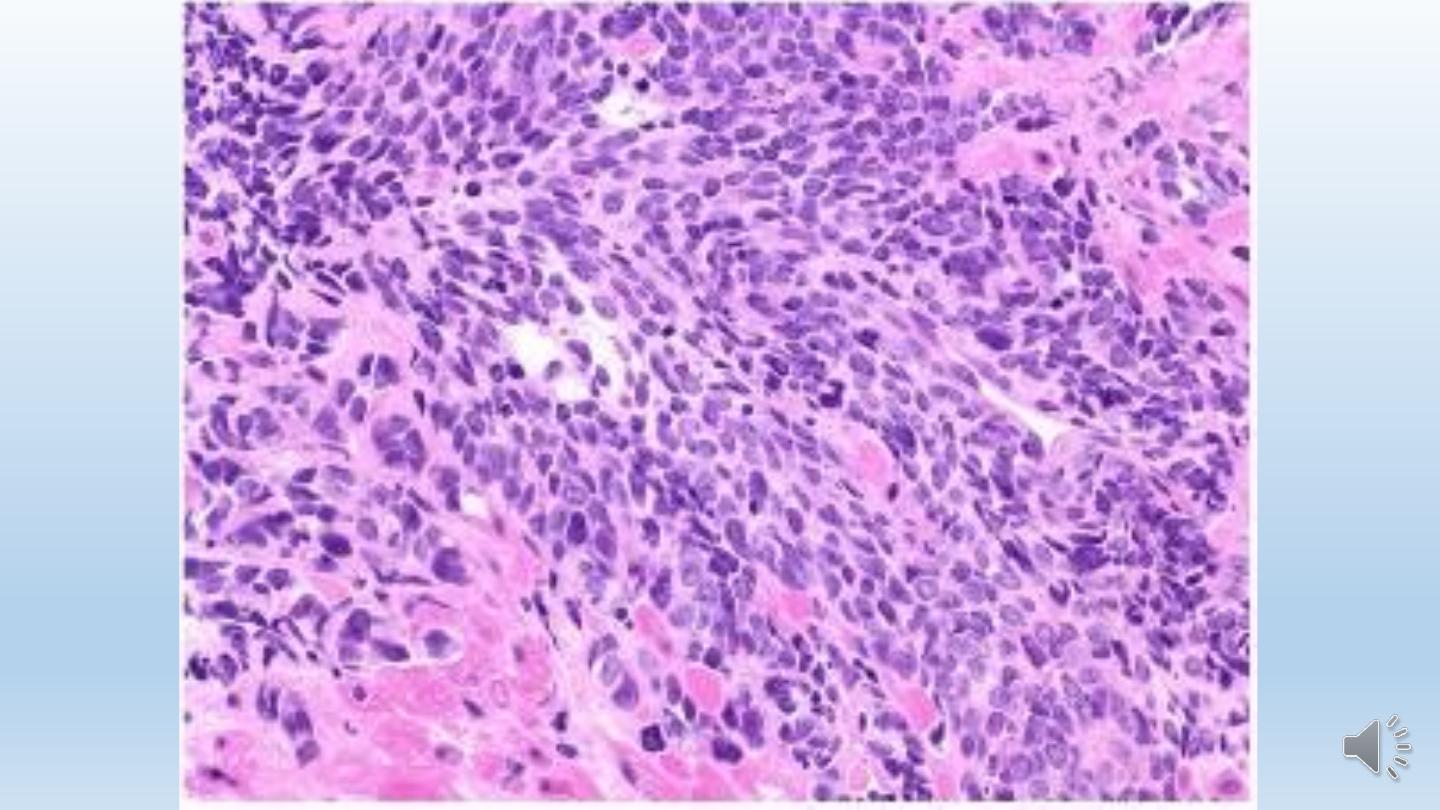
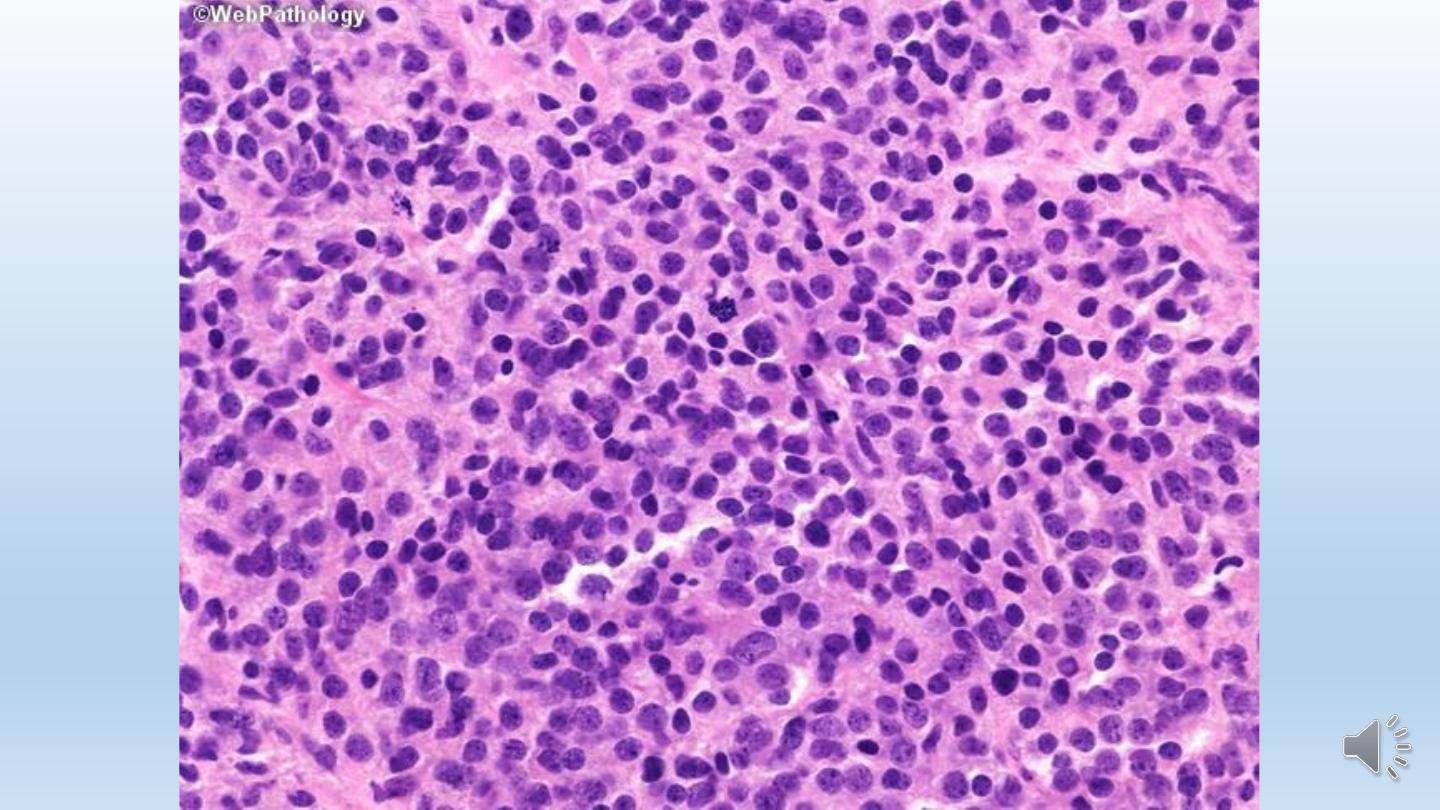
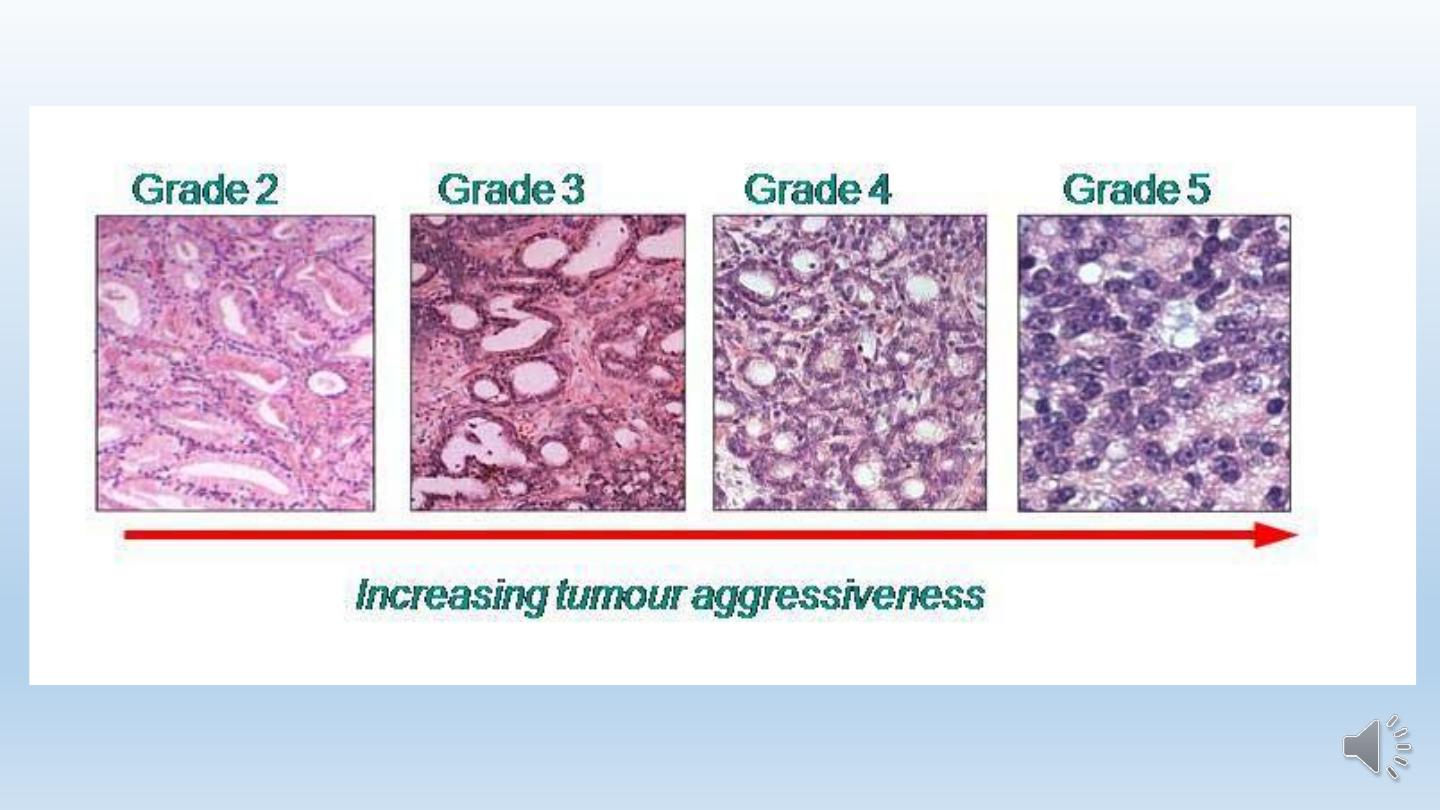
Grading
Grading is of particular importance in prostatic cancer, because
grade and stage are the best prognostic predictors.
Prostate cancer is graded using the Gleason system, which stratifies
prostate cancer into five grades on the basis of glandular patterns of
differentiation. Grade 1 represents the most well differentiated
tumors, in which the neoplastic glands are uniform and round in
appearance and are packed into well-circumscribed nodules.
In contrast, grade 5 tumors show no glandular differentiation, with
tumor cells infiltrating the stroma in the form of cords, sheets, and
nests .
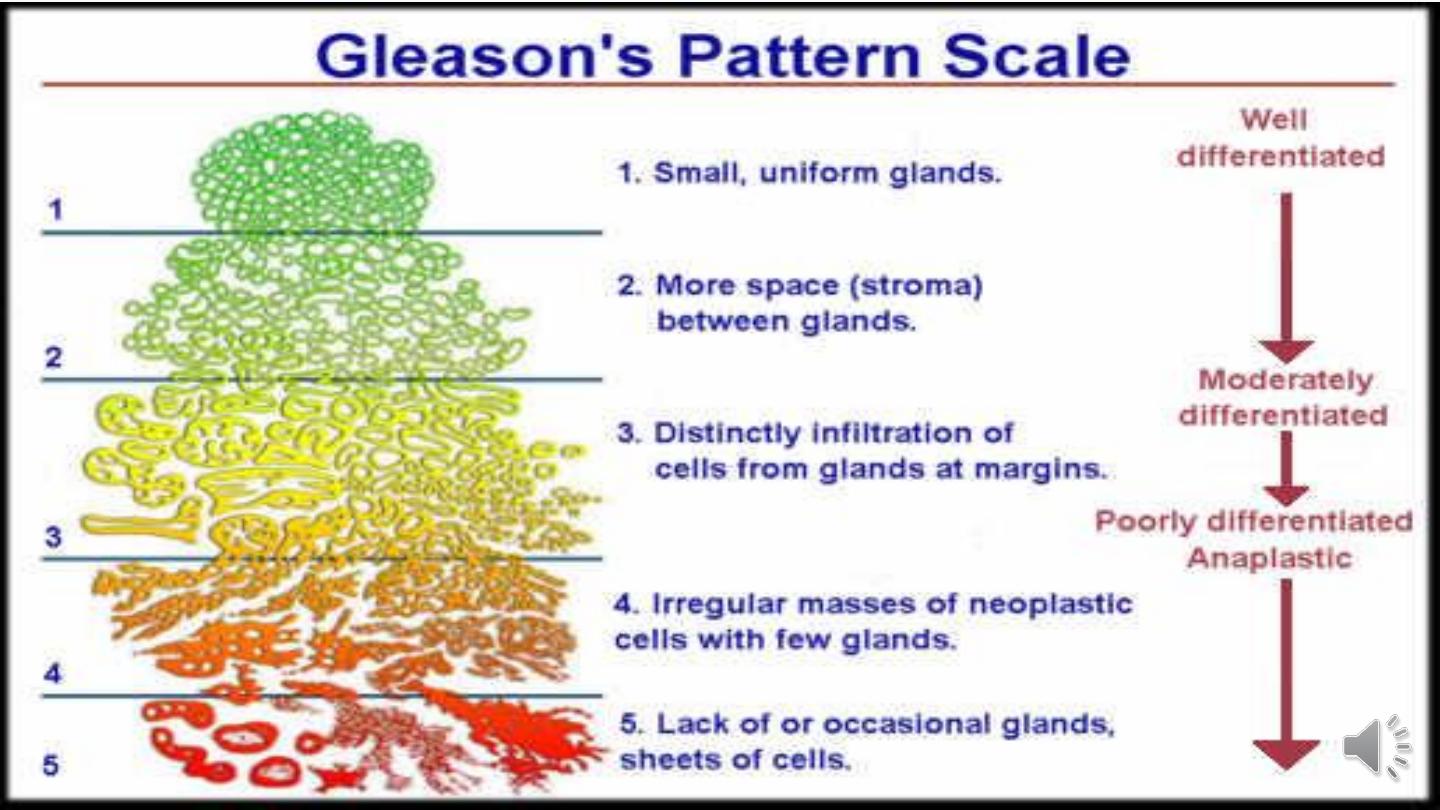

The other grades fall in between these extremes.
Most tumors contain more than one pattern; in such
instances, a primary grade is assigned to the dominant
pattern and a secondary grade to the second most
frequent pattern.
The two numeric grades are then added to obtain a
combined Gleason grade or score.

Thank You
