Amebiasis
By
Dr. Ameer kadhim Hussein.
M.B.Ch.B. FICMS (Community
Medicine).
IDENTIFICATION
The term "amoebiasis" has been defined by WHO as the
condition of harbouring the protozoan parasite Entamoeba
histolytica with or without clinical manifestations.
The symptomatic disease occurs in less than 10 percent of
infected individuals. The symptomatic group has been further
subdivided into intestinal and extraintestinal amoebiasis.
Only a small percentage of those having intestinal infection
will develop invasive amoebiasis.
IDENTIFICATION
The intestinal disease varies from mild abdominal discomfort
and diarrhoea to acute fulminating dysentery.
Extraintestinal amoebiasis includes involvement of liver
(liver abscess), lungs, brain, spleen, skin, etc.
Amoebiasis is a potentially lethal disease. It carries
substantial morbidity and mortality.
IDENTIFICATION
Infection with Entamoeba histolytica is a leading
parasitic cause of death in developing nations and is
an important health risk to travelers.
Amebiasis is transmitted by parasite cysts via fecal-
oral contamination from infected individuals or from
contaminated food or water.
E. histolytica infections may be noninvasive and
asymptomatic or may cause varying degrees of
symptoms through tissue invasion.
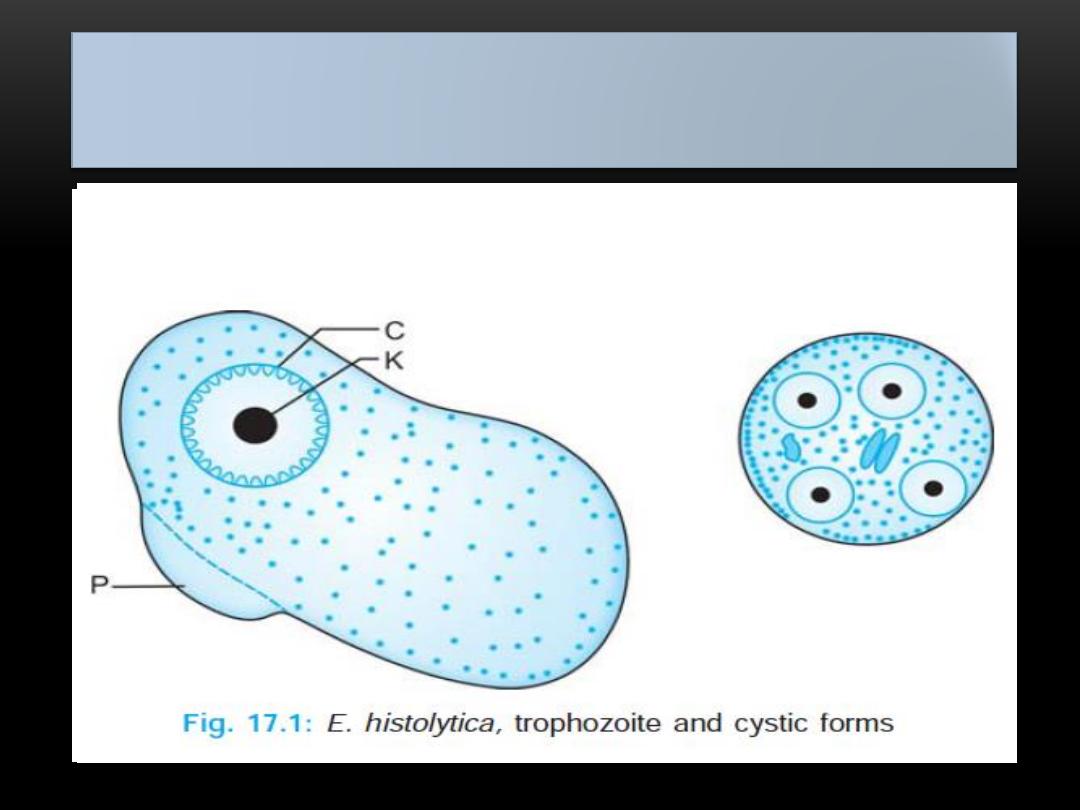
INFECTIOUS AGENT
Amoebiasis is caused by potentially pathogenic strains of E.
histolytica.
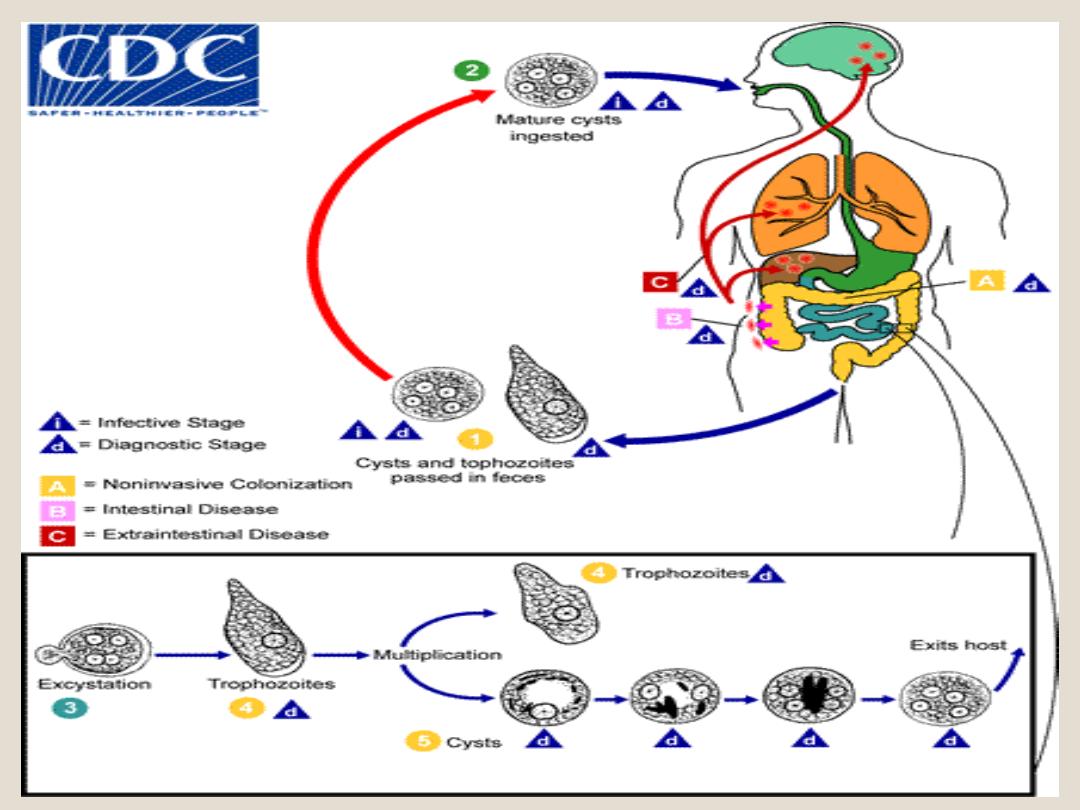
E. histolytica exists in two forms vegetative (trophozoite) and
cystic forms. Trophozoites dwell in the colon where they
multiply and encyst. The cysts are excreted in stool. Ingested
cysts release trophozoites which colonize the large intestine.
Some trophozoites invade the bowel and cause ulceration,
mainly in the caecum and ascending colon; then in the rectum
and sigmoid. Some may enter a vein and reach the liver and
other organs.
INFECTIOUS AGENT
The trophozoites are short-lived outside the human
body; they are not important in the transmission of the
disease.
In contrast the cysts are infective to man and remain
viable and infective for several days in faeces, water,
sewage and soil in the presence of moisture and low
temperature. The cysts are not affected by chlorine in
the amounts normally used in water purification, but
they are readily killed if dried, heated (to about 55 deg
C) or frozen.
INFECTIOUS AGENT
RESERVOIR
Man is the only reservoir of infection.
The immediate source of infection is the
faces containing the cysts.
Most individuals infected with E.
histolytica remain symptom free and are
healthy carriers of the parasite.
The greatest risk is associated with
carriers engaged in the preparation and
handling of food.
PERIOD OF COMMUNICABILITY
As long as cysts are excreted; the period
may be several years, if cases are
unrecognized and untreated.
INCUBATION PERIOD
Variable from few days to several months or
years, commonly 2 to 4 weeks or longer
MODES OF TRANSMISSION
Water polluted with sewage may cause an
epidemic, the feco oral route being the
predominant mode of entry. Food handlers,
if they are convalescent or healthy carriers,
play an important role.
Flies and cockroaches can harbour cysts
and contaminate food. Farm vegetables
contaminated by sewage may infect man.
MODES OF TRANSMISSION
Sexual transmission as a result of oro
anal contact, especially among male
homosexuals, has been increasingly
reported during recent years.
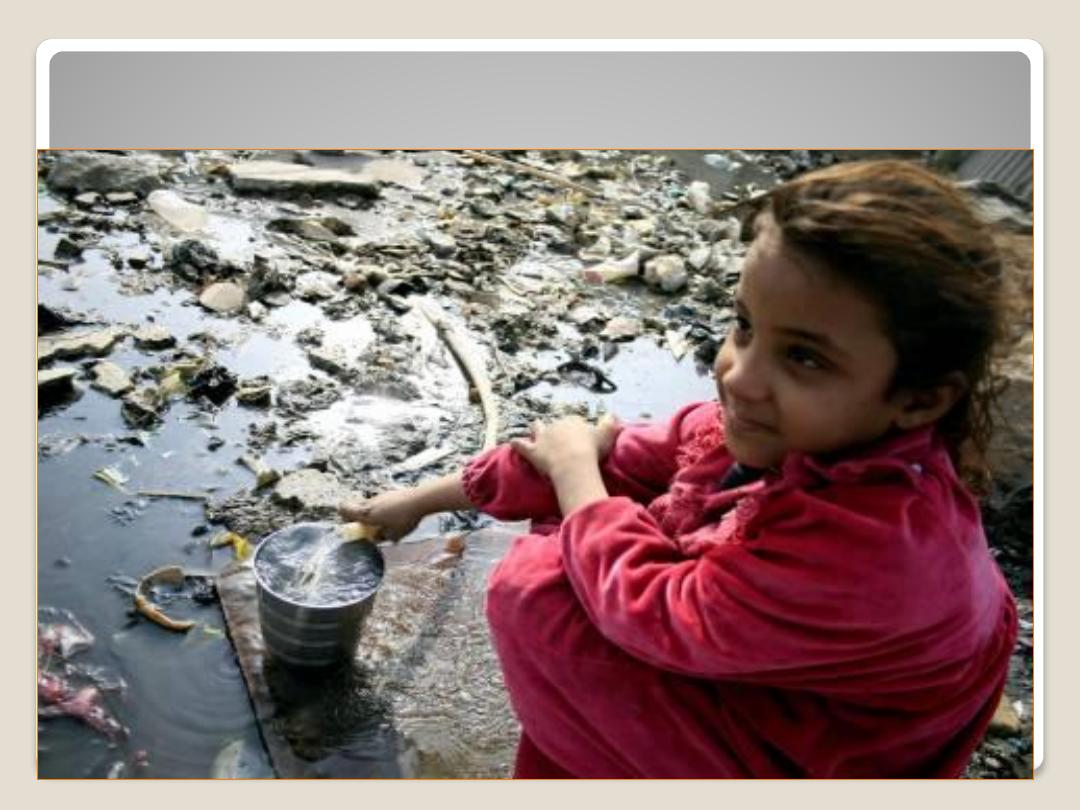
Poverty, ignorance and poor sanitation
are favorable to the spread of disease in
developing countries. Hot, dry climate
is inimical to the cysts.

HOST FACTORS
Amoebiasis may occur at any age. There is no sex or
racial difference in the occurrence of the disease.
Amoebiasis is frequently a household infection.
When an individual in a family is infected, others in
the family may also be affected. Specific anti-
amoebic antibodies are produced when tissue
invasion takes place. There is strong evidence that
cell mediated immunity plays an important part in
controlling the recurrence of invasive amoebiasis.
ENVIRONMENTAL FACTORS
Amoebiasis is more closely related to poor sanitation
and socio-economic status than to climate.
In countries with marked wet-dry seasons, infection
rates are higher during rains, presumably since cysts
may survive longer and the potential for transmission
is there by increased. Epidemic outbreaks are usually
associated with sewage seepage into the water supply.
EPIDEMIOLOGY
Amoebiasis is a common infection of the human
gastro-intestinal tract. It has a worldwide distribution.
It is a major health problem in the whole of China,
South East and West Asia and Latin America,
especially Mexico.
Globally it is estimated that 500 million people carry E.
histolytica in their intestinal tract and approximately
one-tenth of infected people suffer from invasive
amoebiasis. It is probable that invasive amoebiasis,
accounted for about 100,000 deaths in the world.
EPIDEMIOLOGY
Prevalence rates vary from as low as 2 percent to 60
percent or more in areas devoid of sanitation. In areas
of high prevalence, amoebiasis occurs in endemic
forms as a result of high levels of transmission and
constant reinfection.
Epidemic water-borne infections can occur if there is
heavy contamination of drinking water supply.
EPIDEMIOLOGY
Amebiasis has a worldwide distribution but is most common in
the developing world.
In underdeveloped areas where drinking water is obtained from
fecally contaminated water sources and contaminated water or
sewage is used to grow or freshen vegetables, amebiasis has
high incidence.
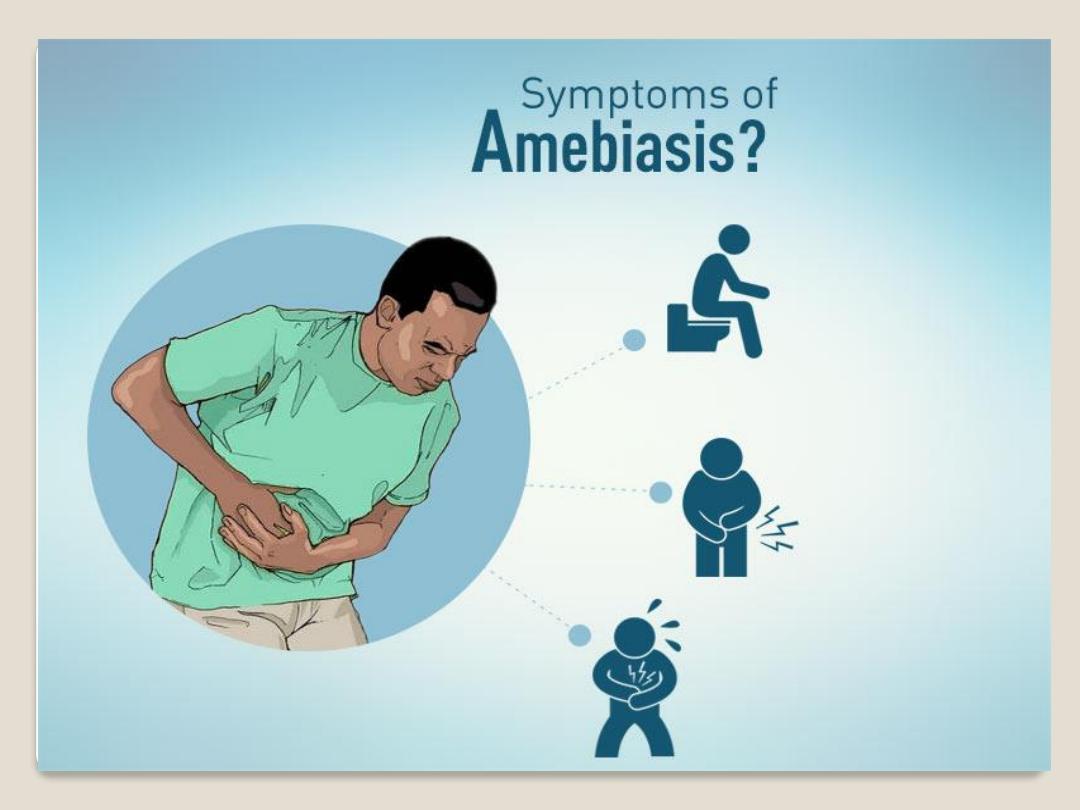
Clinical features
There is a variable clinical response to E. histolytica infection.
Invasive amebiasis leading to dysentery, liver abscess, pleuro-
pulmonary involvement, or, less commonly, involvement of other
organs occurs in the minority of infections. The majority of cases
have either non-dysenteric intestinal amebiasis with mild to
moderate symptoms or are asymptomatic cyst passers.
Amebic dysentery, or acute amebic colitis, usually has an
incubation of about 8 to 10 days, and onset is often sudden.
Typical acute symptoms include severe abdominal cramps, chills,
fever, nausea, headache, and tenesmus. The stools are liquid and
contain bloody mucus with leukocytosis. In very severe cases,
The complications can be fatal.
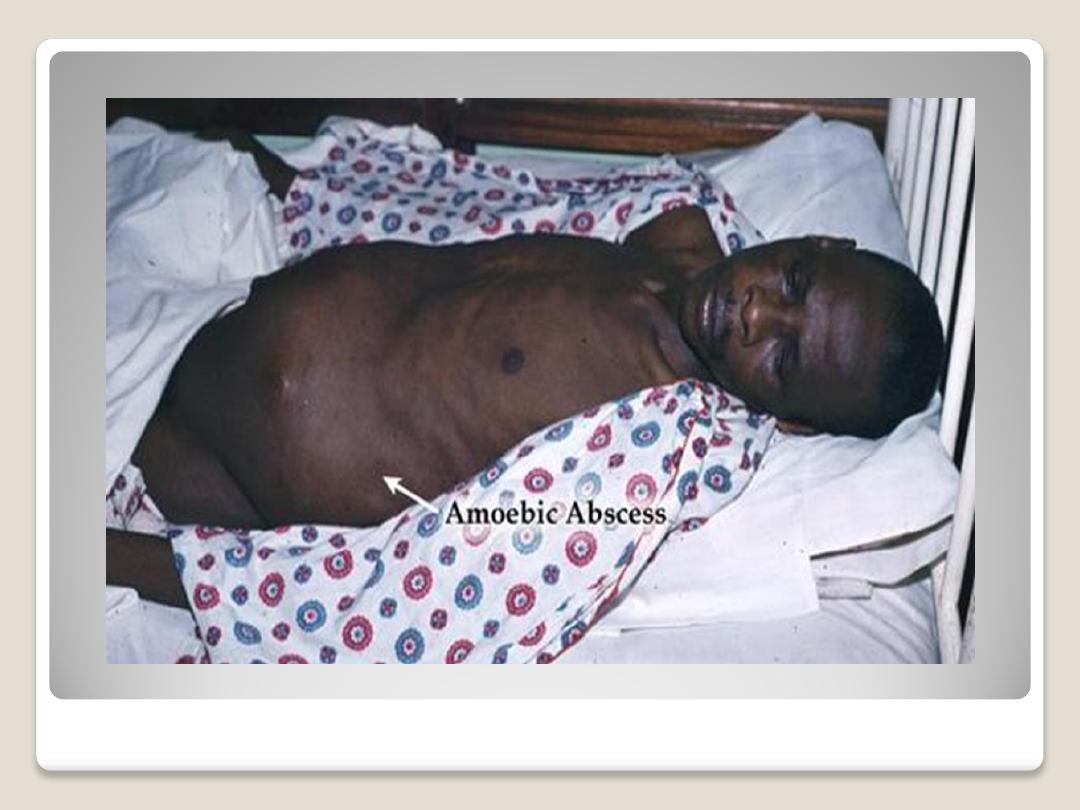
Extra-Intestinal Amebiasis

Primary prevention
a. Sanitation : Safe disposal of human excreta coupled
with the elementary sanitary practice of washing hands
after defecation and before eating is a crucial factor in
the prevention and control of amoebiasis.
But there are too many hurdles (both social and
economic) in enforcing it in many developing
countries. With the cooperation of the local
community, the sanitary systems should be constructed
taking into consideration the customs and practices of
the population and the available resources.
Primary prevention
b. Water supply : The protection of water supplies
against faecal contamination is very important
because amoebic cysts may survive for several days
and weeks in water. The cysts are not killed by
chlorine in amounts used for water disinfection.
Sand filters are quite effective in removing amoebic
cysts. Therefore water filtration and boiling are
more effective than chemical treatment of water
against amoebiasis.
Primary prevention
c. Food hygiene:
Environmental measures should also include the protection of
food and drink against faecal contamination. Uncooked
vegetables and fruits should be disinfected.
In most instances, thorough washing with detergents in running
water will remove amoebic cysts from fruits and vegetables.
Since food handlers are major transmitters of amoebiasis, they
should be periodically examined, treated and educated in food
hygiene practices such as hand washing.
d. Health education of the community about the risk of
disease and mode of transmission and preventive measures.
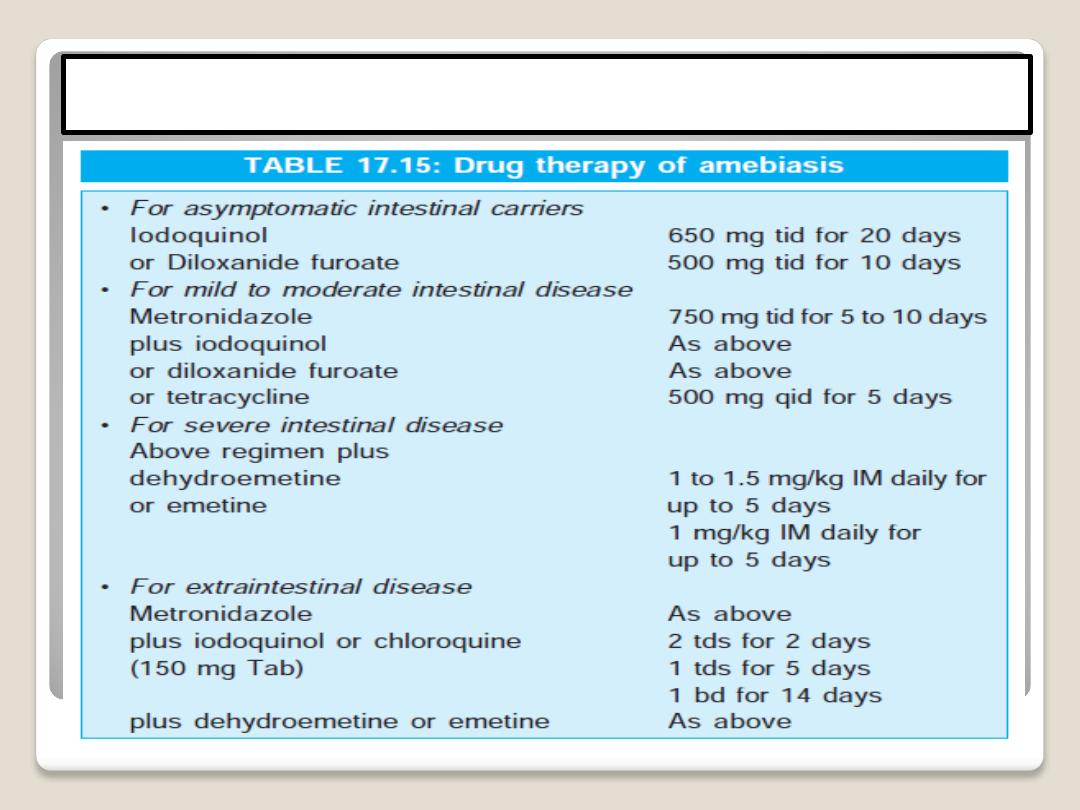
Secondary prevention
Diagnosis and treatment:
Diagnosis By microscopic demonstration of trophozoites or cysts in fresh
stool specimens, smear of aspirates obtain by proctoscopy or aspirates of
abscess or sections of tissue.
Demonstration of trophozoites containing red cells is diagnostic. They are
most readily seen in fresh mucus passed per rectum.
Serological tests are often negative in intestinal amoebiasis, but if positive,
they provide a clue to extraintestinal amoebiasis.
Indirect haemagglutination test (IHA) is regarded as the most sensitive
serological test. Newer techniques include counter immuno-electrophoresis
(CIE) and ELISA techniques.
Secondary prevention
Avoid un safe source of water supply

Thank you for wash your hand
