1
Operative delivery
1- Instrumental delivery
Incidence: 6-12%
Indication:
1- Delay in 2
nd
stage of labor
2- Poor maternal effort
3- Fetal distress, cord prolapse in 2
nd
stage of labor.
4- Maternal indication: sever cardiac, respiratory, hypertension disease
or intracranial pathology that bearing down effort my lead to death.
Causes of prolonged second stage of labor:-
1- Inadequate uterine contraction
2- Poor expulsive effort by the mother.
3- Minor disproportion or malposition.
4- Uses of epidural analgesia à inadequate uterine contraction
secondary to abolition of Ferguson's reflex (stretching of lower
vagina by presenting part à lead to release of oxytocin).
How to approach patient necessitate instrumental delivery?
1- Medical person should introduce himself to the patient.
2- Explain the indication, complication & contraindication of the
procedure.
3- Verbal or written consent should be taken from the mother &
partner.
4- Prerequisite criteria need to be full filled.
5- General examination of the mother, pain relief & hydration.
6- Analgesia in form of pudendal block & local perineal infiltration with
20 ml of 1% lignocaine & sometime spinal anesthesia is used in (
midcavity forceps)
7- Fetal condition should be assessed either clinically or by CTG
2
8- Abdominal examination is important for assessment of the size of
the fetus & if > 4.5 kg, caution is required. , engagement of the head
& uterine contraction which should be efficient ( 3 contractions > 40
sec / min )
9- Empty bladder is necessary
10- Vaginal examination is done to know
a- Membrane rupture or not
b- Head engagement ( below ischial spine )
c- Fully dilated cervix
d- Assessment for caput ( soft tissue swelling of the scalp ) or
molding ( overlapping of skull bone )
e- Position of the head & descend of presenting part with each
contraction
11- Position of the mother à the leg is flexed & abducted or in left
lateral position but much easier in lithotomy position
12- Aseptic technique as vulva & perineum is washed with antiseptic
solution.
Choice of the instruments, forceps or ventouse
The choice of the forceps or vacuum depend on
1- Operators Experience
2- Station & position of the head
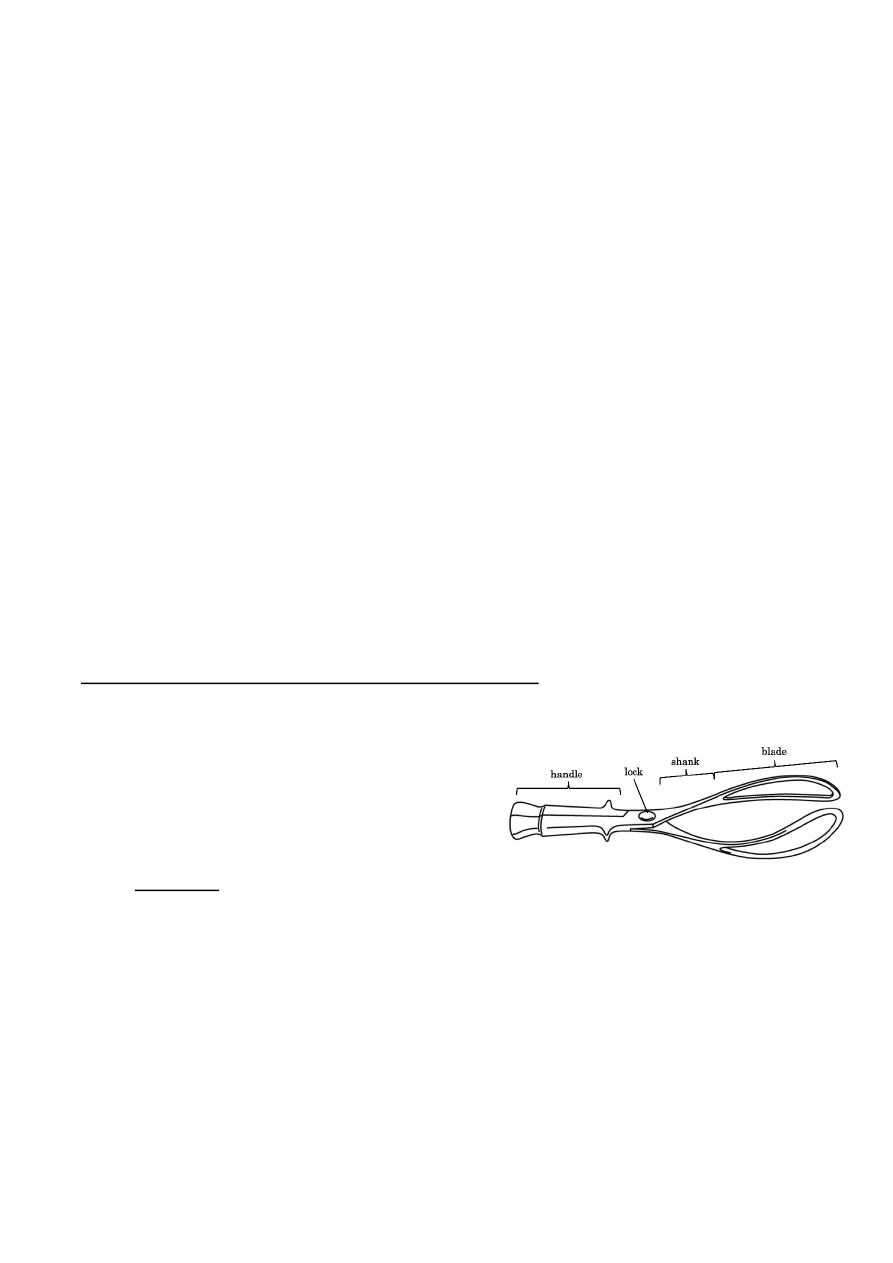
1) Forceps: could be fenestrated or not & consist of two blades, shank,
handle & lock.
Types of forceps:
i. Long forceps: midcavity forceps or Simpson's forceps
ii. Short forceps : outlet forceps ( Wrigley's forceps )
iii. Rotational forceps : for occipitolateral or occipitoposterior
position ( Keiland forceps )
3
The blade has cephalic curve, which apply on the fetal maxilla or
molar eminence while pelvic curve fit the maternal pelvis.
Keiland forceps has no pelvic curve, as it is rotational forceps used
for malposition.
Prior to application of forceps, the blades should be assessed to
check whether they fit together as pair.
Left blade put on the left side of the vagina by the left hand while
right blade is held by right hand & applied between the left hand that
protect vaginal wall & then locked horizontally & when apply
forceps:
a- The sagittal suture is in the midline
b- Occiput is 3-4 cm above the shank
c- Traction applied with the contraction & maternal bearing
d- Traction is applied upward as the head is delivered by extension
e- Episiotomy done when the head is crowning
Keiland forceps:
Is a rotational forceps used for occipitoposterior & occipitotransverse
position.
1- Determine the direction of fetal back
2- Apply the anterior blade over the face of the fetus, posterior blade
apply directly & then rotational movement by sliding the shank to
rotate the occiput toward the fetal back to occiput anterior. It
need experience one.
Complication of Forceps:
1- 3
rd
& 4
th
perineal tear
2- Transient facial & scalp abrasion.
4
3- Rare complication: facial nerve injury or palsy, cephalo-
haematoma, skull bone fracture of the fetus.
2) Ventouse delivery:
It is an alternative for forceps delivery for similar indication in second
stage of labor.
It is vary in size of the cup 4, 5, 6, cm.
The cup is applied at flexion point which 3-4 cm in front of the
occiput on the midline indicated by sagittal suture
This to increase flexion of the head to permit minimal diameter to
descend.
Once the cup is applied correctly , vacuum is created start by 0.2
kg/cm
2
negative pressure , then increase the pressure up to 0.7 -0.8
kg/cm
2
& then traction is applied , descend of the head with flexion
promote autorotation of the head to occipito-anterior.
It is less causing perineal trauma.
Types of ventouse:
1- Metallic type
2- Silk type
3- selastic type
Anterior cup à for O.A position & its tube arise from the anterior
surface of the cup.
Posterior cup à for O.P., O.T. & its tube arise from the lateral side of
the cup & usually it is metallic type.
Complication of vacuum:
1. Chignon: soft tissue of the scalp sucked into cup & usually
resolve within 2-3 days.
2. Scalp abrasion
3. Retinal haemorrhage.
4. Skull haematoma
5. Neonatal jaundice.
5
6. Subgaleal haemorrhage which is associated with high PNM &
mortality.
Contraindication of vacuum:
1- Gestational age < 34 weeks (gestational age)
2- Fetal scalp haemorrhage
3- Face presentation.
2- Caesarean Section C/S:
It means delivery of the baby by an abdominal & uterine incision.
Incidence: 10-25%
Types:
1) Emergency: immediate threaten to the life & should be done within
30 min.
2) Urgent C/S: no immediate threaten to the life & should be done
within 60-75 min.
3) Elective C/S: when the patient is prepared & done at 39 weeks
gestational age.
Indication of C/S:
1. antepartum haemorrhage ( APH ) à abruption placenta & placenta
previa
2. Cord prolapse.
3. rupture scar
4. Fetal hypoxia, FHR bradycardia < 80 BPM.
5. Failure of progress of labor
6. IUGR with absent diastolic flow
7. Sever PET with unfavorable cervix
8. Malpresentation ( breech , brow )
9. History of hysterotomy or vertical incision.
6
10. History of HIV infection
11. History of vesicovaginal fistula.
Placenta accrete is more common complication & may result in
massive haemorrhage that lead to hysterectomy so consent &
preparation of the patient is necessary. (Placenta accrete occur when
the placenta is anterior, lower laying in women with history of scar)
Types of C/S:
1) lower uterine segment incision involve horizontal incision of the
lower segment after reflecting the vesical peritoneum , this is the
commonest type & the abdomen opened by lower midline ,
paramedian & commonly by pfannensteil incision ( suprapubic
horizontal incision ) & the peritoneal cavity opened , the bladder
is reflected from the lower uterine segment & transverse incision
is made at lower uterine segment & the presenting part is
delivered through the lower segment ,
The merits of single versus two layers closure of the muscle &
closure versus non-closure of the vesical peritoneum is currently
being investigated by many randomized controlled studies.
Advantages of lower segment incision:
1- easier to incise & suture as it is thin
2- Less blood loss & infection rate compared with upper uterine
segment.
Then the uterine cavity should be cleaned, not to leave any
retained piece & should be sure that cervical os is open to allow
drainage of the blood.
Closure of the uterus is followed by peritoneal toilet through
removing of any blood or liquor in the abdominal cavity either by
suction or gauze swab.
Inspection of the ovary & tubes is done.
Prophylactic antibiotic is given routinely.
7
If the mother is Rh –ve & the baby is Rh +ve, anti-D should be
given.
2) Classical C/S:
Could be done at upper or lower uterine segment, commonly it
start in the lower segment at as a small incision & extend upward
Disadvantage of it:
1- Difficulty to incise it
2- More blood loss
3- Inadequate apposition at closure
4- Increase risk of scar rupture that increase maternal mortality &
morbidity.
But it has certain indication:
1- When the lower segment approach is difficult because of fibroid
or anterior placenta previa.
2- Preterm breech with poorly formed lower segment
3- Impacted transverse lie with rupture membrane.
4- Impacted transverse lie with congenital anomaly.
5- Perimortem C/S
3) Other types: are inverted T & J – shape incision.
Complication of C/S:
Early complication :
Late complication:
1- primary haemorrhage
1- secondary hemorrhage
2- anesthetic related complication
like lung atelectasis, Mendelson's
syndrome
2- wound infection
3- Injury to the bowel, bladder,
ureter & to the fetus sometime.
3- vesico-vaginal , uretrovaginal
fistula are rare
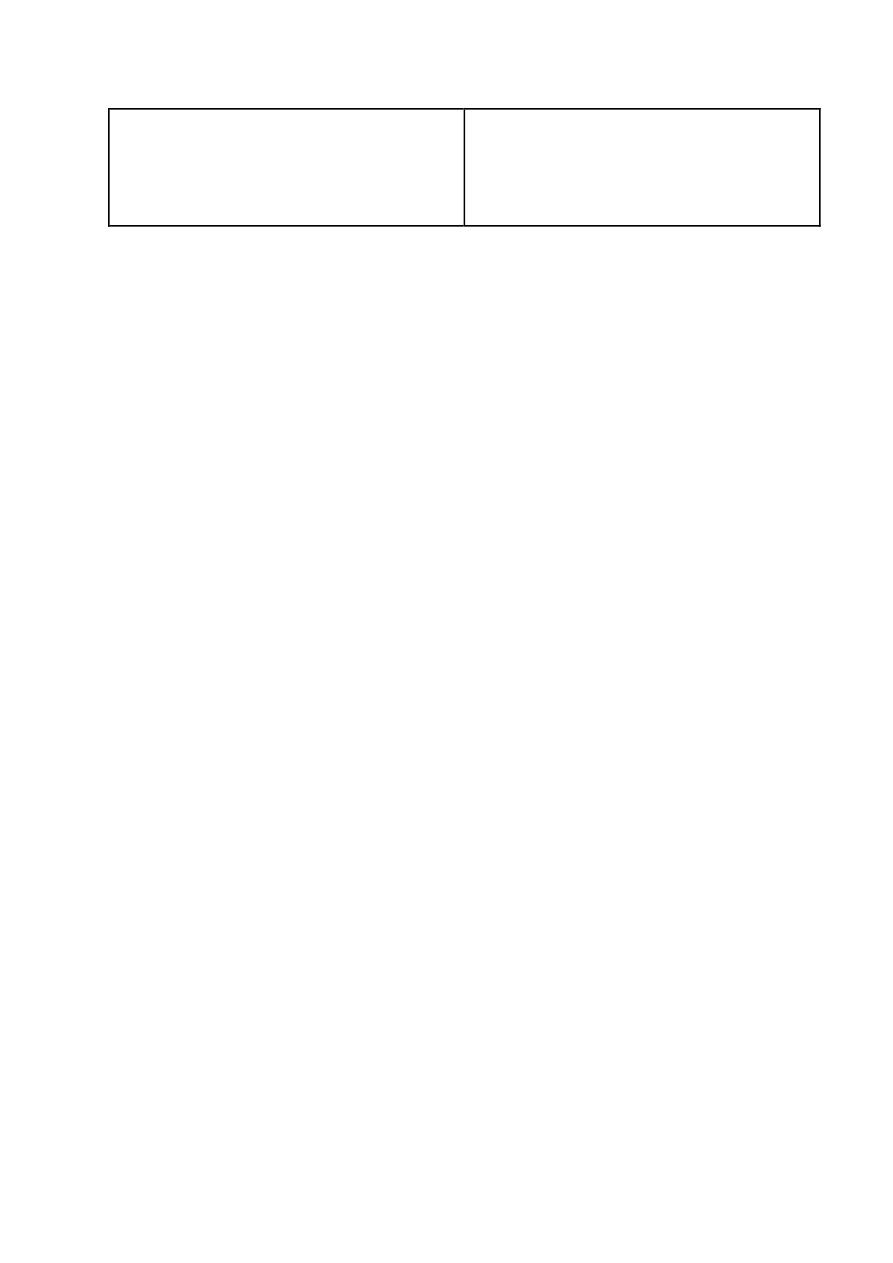
8
4- pulmonary embolism
4- DVT, so prophylactic dose of
heparin is used & post operatively,
early mobilization & chest
physiotherapy is advocated.
C/S may complicated by caesarean hysterectomy in :
1- Placenta previa, placenta accreta.
2- Uncontrollable postpartum haemorrhage.
3- Rupture uterus
4- CA- cervix
Maternal mortality is rare less than 0.3/1000 & is related to reason for
which C/S is done or to anesthesia or to haemorrhage complication.
