
Genital tract trauma
Episiotomy
Definition
An episiotomy is an incision through the perineum made to enlarge the
diameter of the vulval outlet and assist childbirth.
Indications:
• Fetal distress.
• Rigid perineum.
• Shoulder dystocia.
• Fetal malposition e.g. occiput posterior.
• Breech delivery.
• Instrumental delivery.
• Previous pelvic surgery.
Technique
The question of informed consent needs to be addressed during
antenatal care; when the fetal head is crowning, it is not possible to
obtain true informed consent
•
An episiotomy is performed in the second stage, usually when the
perineum is being stretched and it is deemed necessary.
•
If there is not a good epidural, the perineum should be infiltrated
with local anaesthetic.
•
The incision can be midline or at an angle from the posterior end
of the vulva (a mediolateral episiotomy).
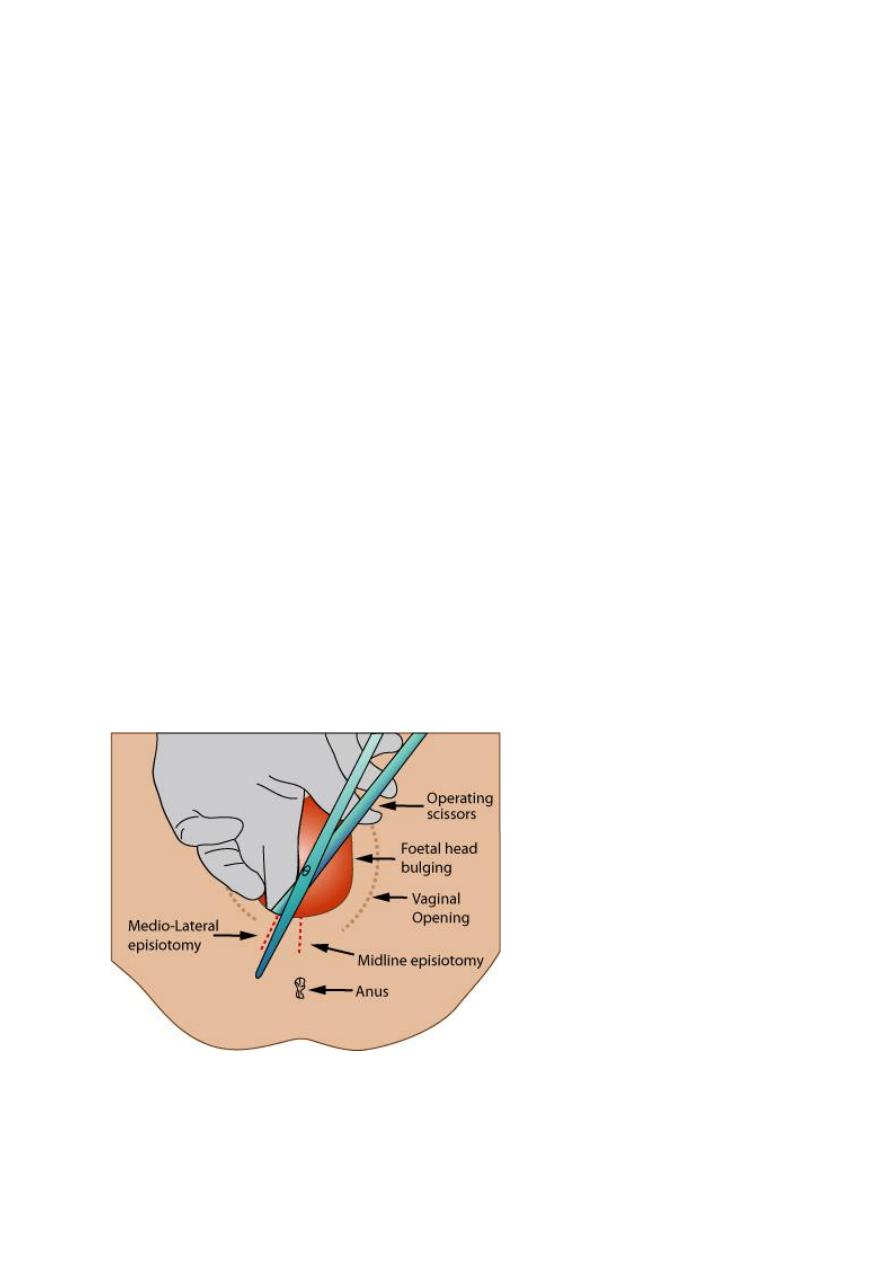
•
A mediolateral episiotomy is usually recommended; a midline
episiotomy is an incision in a comparatively avascular area and results
in less bleeding, quicker healing and less pain, however, there is an
increased risk of extension to involve the anal sphincter (third/ fourth-
degree tear).
•
A mediolateral episiotomy should start at the posterior part of the
fourchette, move backwards and then turn medially well before the
border of the anal sphincter, so that any extension will miss the
sphincter
Complications
Complications include haemorrhage, infection (prophylactic
antibiotics may be indicated if contamination is suspected), extension
to the anal sphincter (third/fourth-degree tears) and dyspareunia.
Perineal trauma
Definitions
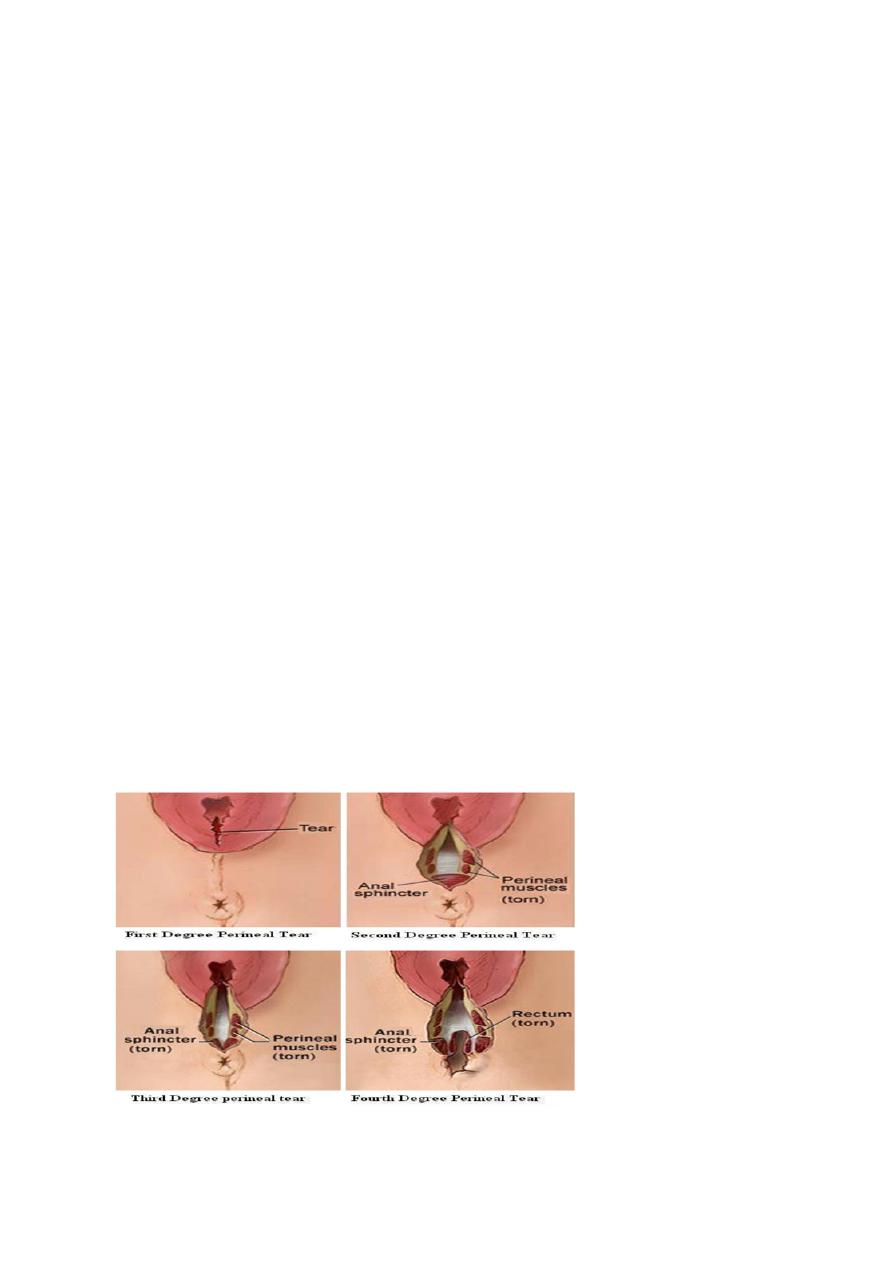
1. First-degree trauma corresponds to lacerations of the skin/vaginal
epithelium alone.
2. Second-degree tears involve perineal muscles and therefore
include episotomies.
3. Third-degree extensions involve any part of the anal sphincter
complex (external and internal sphincters):
i
Less than 50 per cent of the external anal sphincter is torn.
ii More than 50 per cent of the external anal sphincter is torn.
iii Tear involves the internal anal sphincter (usually there is
complete disruption of the external sphincter).
4. Fourth-degree tears involve injury to the anal sphincter complex
extending into the rectal mucosa.

An increased risk of perineal trauma is associated with:
•
larger infants
•
prolonged labour
•
instrumental delivery.
Internal anal sphincter incompetence results in insensible faecal
incontinence, whereas external anal sphincter incompetence causes
faecal urgency.
Perineal repair (
ﻟ
ﻸ
ط
ﻼ
ع
)
• Ensure adequate analgesia. This may be achieved by topping up
an epidural or by infiltration with local anaesthetic.
•
Check the extent of cuts and lacerations.
•
First repair the vaginal mucosa using rapidly absorbed suture
material on a large, round body needle. Start above the apex of the cut
or tear (as severed vessels retract slightly) and use a continuous stitch
to close the vaginal mucosa.
•
Interrupted sutures are then placed to close the muscle layer.
•
Closure of the skin follows. Interrupted sutures can be used;
however, a continuous subcuticular stitch produces more comfortable
results.
•
Perform a gentle vaginal examination to check for any missed
tears or inappropriate apposition of anatomy. Remove the pad that was

placed at the top of the vagina and check that no swabs have been left
in the vagina.
• Finally, put a finger in the rectum to check that no sutures have passed
through into the rectal mucosa and that the sphincter is intact. If sutures
are felt in the rectum they must be removed and replaced.
Repair of third- and fourth-degree trauma should be performed or
direcdy supervised by a trained practitioner. There must be adequate
analgesia. In practice, this means either a regional or general
anaesthetic, as local infiltration does not allow relaxation of the
sphincter enough to allow a satisfactory repair. The lighting must be
adequate and an assistant is usually needed.
Repair of the rectal mucosa should be performed first. The torn
external sphincter is then repaired. It is important to ensure that the
muscle is correctly approximated with long-acting sutures so that the
muscle is given adequate time to heal. Some surgeons opt for an end-
to-end repair, while others use an overlap technique; The remainder of
the perineal repair is as for second-degree trauma.
Lactulose and a bulk agent are recommended for 5—10 days. It is
common sense to give a broad-spectrum antibiotic that will cover
possible anaerobic contamination, such as metronidazole . Adequate
oral analgesia should also be prescribed.
At 6-12 months, a full evaluation of the degree of symptoms should
take place. Symptomatic women should be offered investigation
including endoanal ultrasound and manometry
Further deliveries should be by C\S.
Uterine Rupture
Uterine rupture implies complete separation of the uterine
musculature through all of its layers, ultimately with all or a part of the
fetus being extruded from the uterine cavity. The overall incidence is
0.5%.
Uterine rupture may be spontaneous, traumatic, or associated with a
prior uterine scar, and it may occur during or before labor or at the time
of delivery. A prior uterine scar is associated with 40% of cases. With
a prior lower-segment transverse incision, the risk for rupture is less
than 1%, whereas the risk with a high vertical (classical) scar is 4% to
7%.
DIAGNOSIS AND MANAGEMENT
The signs and symptoms of uterine rupture are highly variable.
Typically, rupture is characterized by the sudden onset of intense
abdominal pain and some vaginal bleeding. Impending rupture may be
heralded by hyperventilation, restlessness, agitation, and tachycardia.
After the rupture has occurred, the patient may be free of pain
momentarily and then complain of diffuse pain thereafter. The most
consistent clinical finding is an abnormal fetal heart rate pattern. The
patient may or may not have vaginal bleeding, and if it occurs, it can
range
from spotting to severe hemorrhage. The presenting part may be found
to have retracted on pelvic examination, and fetal parts may be more
easily palpated abdominally. Abnormal contouring of the abdomen

may be seen. Fetal distress develops commonly, and fetal death or long-
term neurologic sequelae may occur in 10% of cases.
A high index of suspicion is required, and immediate laparotomy
is essential. In most cases, total abdominal hysterectomy is the
treatment of choice, although debridement of the rupture site and
primary closure may be considered in women of low parity who desire
more children.
MATERNAL-FETAL RISK
Delay in management places both mother and child at significant risk.
The major risk to the mother is hemorrhage and shock. Although the
associated maternal mortality rate is now less than 1%, if the mother is
left untreated, she will almost certainly die. For the fetus, rapid
intervention will minimize morbidity and mortality. The associated
fetal mortality rate is still about 30%.
