Dr.Majeed M.Al-Hamammi
lectures 4th yearMedical college
Thi- Qar 2020-2021
Respiratory disease
Pulmonary medicinePulmonology
Respiralogy
Objectives
At the end of this lecture we should be Know and familiar withRespiratory physiology
Respiratory anatomy
-Respiratory symptoms.
-Respiratory signs.
-Investigation of respiratory diseases.
Respiratory disease
Is responsible for a major burden of morbidity and mortality, and conditions such as
tuberculosis,
pandemic influenza ,SARSCoV2.
pneumonia
are the most important conditions in world health terms.
Respiratory Cases In Primary care and Hospital admission
Respiratory medicine is an exciting and varied specialty caring for patients with a range of acute and chronic conditionsThe increasing prevalence of allergy, asthma and chronic obstructive pulmonary disease (COPD) .
By 2025, smokers world-wide is anticipated to increase to 1.5 billion.
FUNCTIONAL ANATOMY AND PHYSIOLOGY
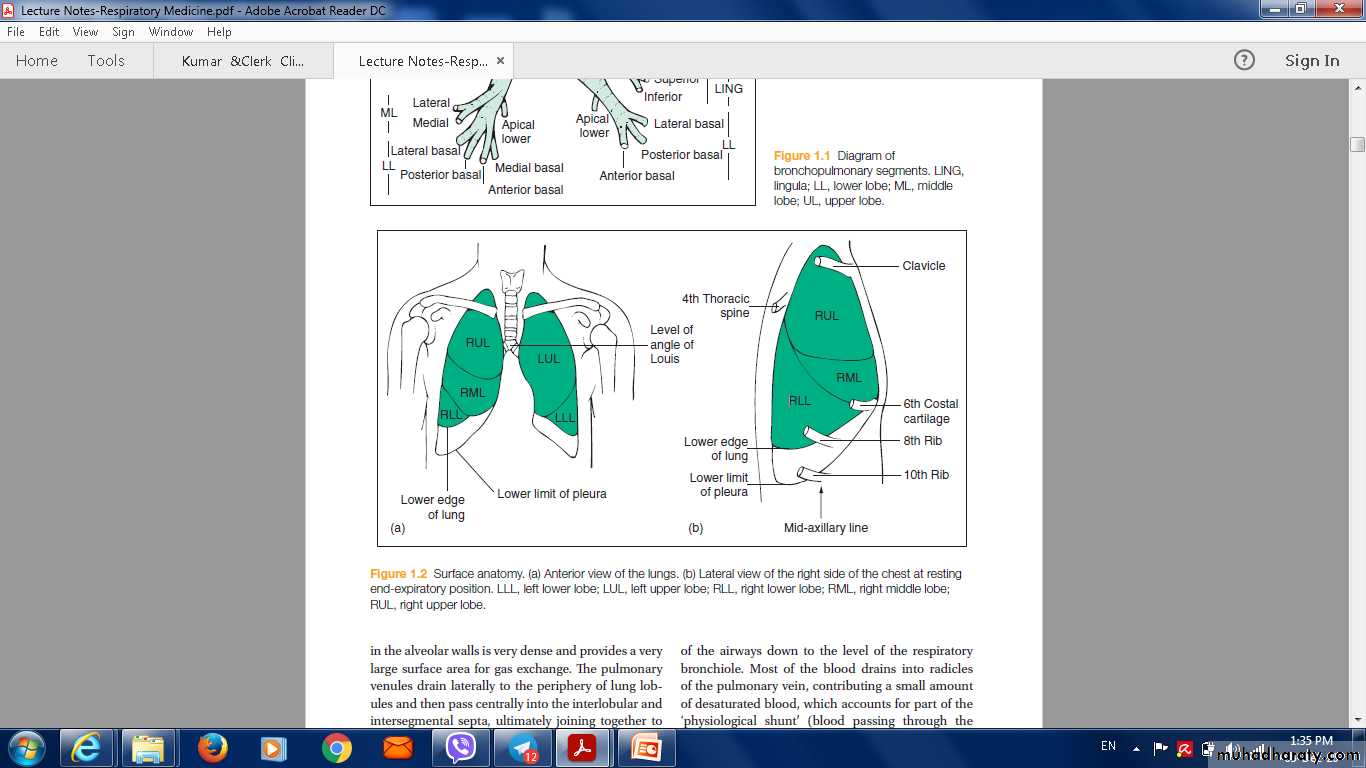
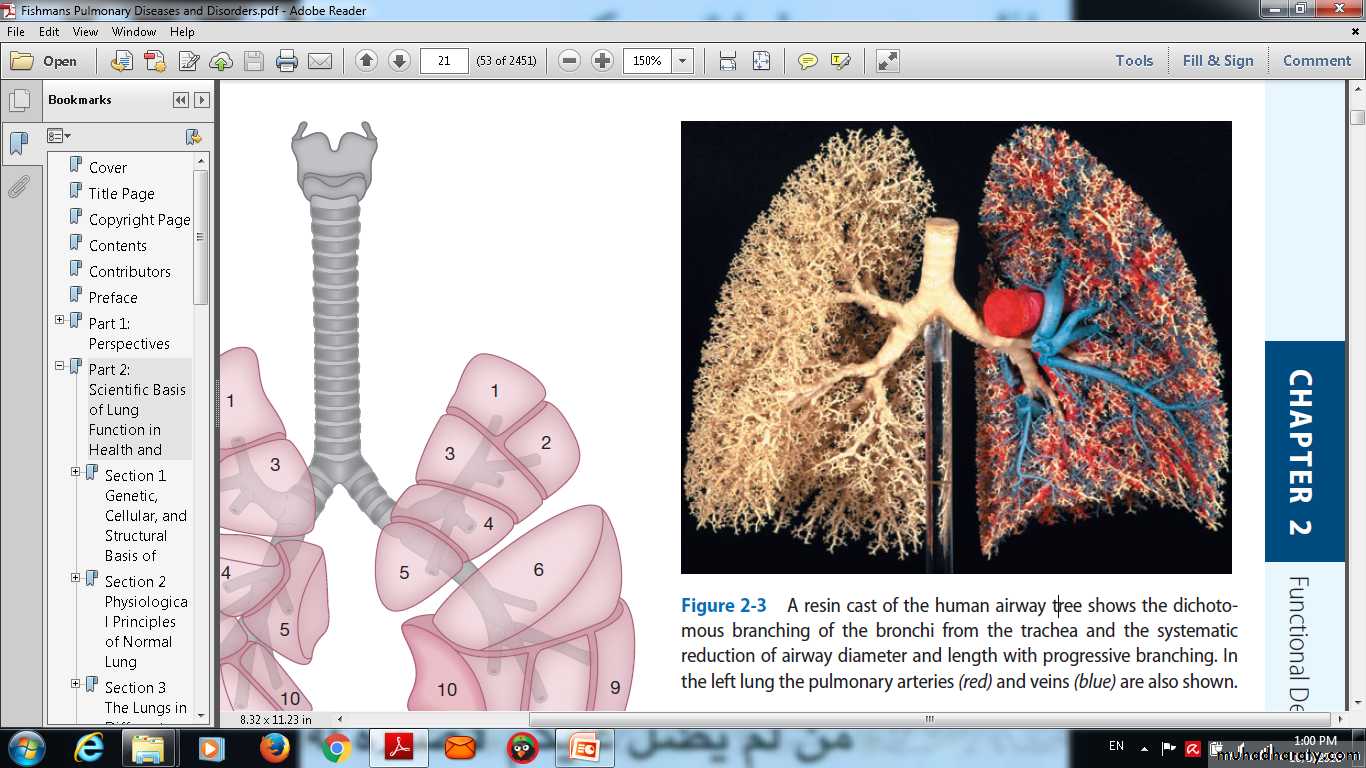
The lungs occupy the upper two-thirds of the bony thorax, bounded medially by the spine, the heart and the mediastinum and inferiorly by the diaphragm.& Segment Lungs Surface Anatomy
Aspect of lungs Lateral
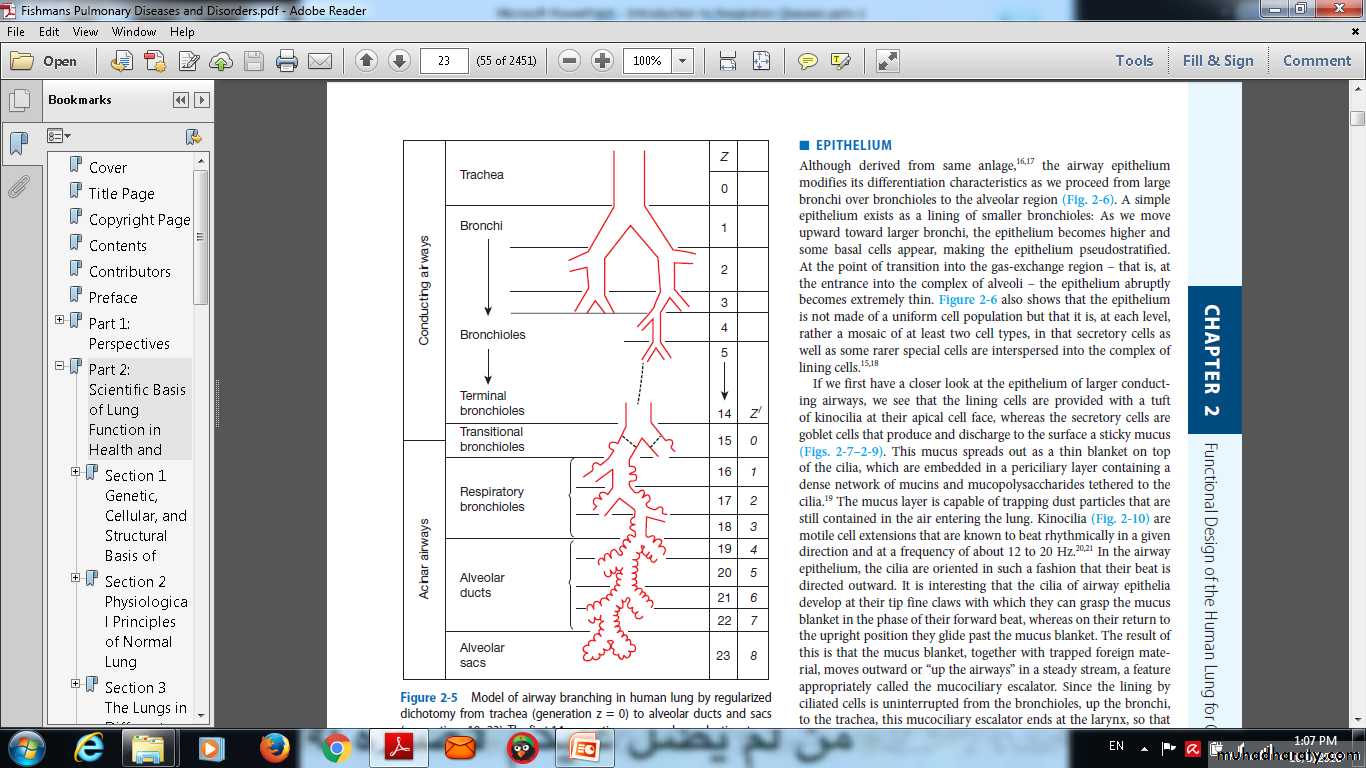
The conducting airways
from the nose to the alveoli connect the external environment with the extensive, thin and vulnerable alveolar surface.In the glottis and trachea, obstruction by foreign bodies and tumours.
in the third-generation respiratory, very slow flow rates.
Model of airway branching in human lung by regularizeddichotomy from trachea (generation z = 0) to alveolar ducts and sacs(generations 19–23). The first 14 generations are purely conducting; transitionalairways (generation 15) lead into the acinar airways with alveolithat branch over 8 generations (z′).
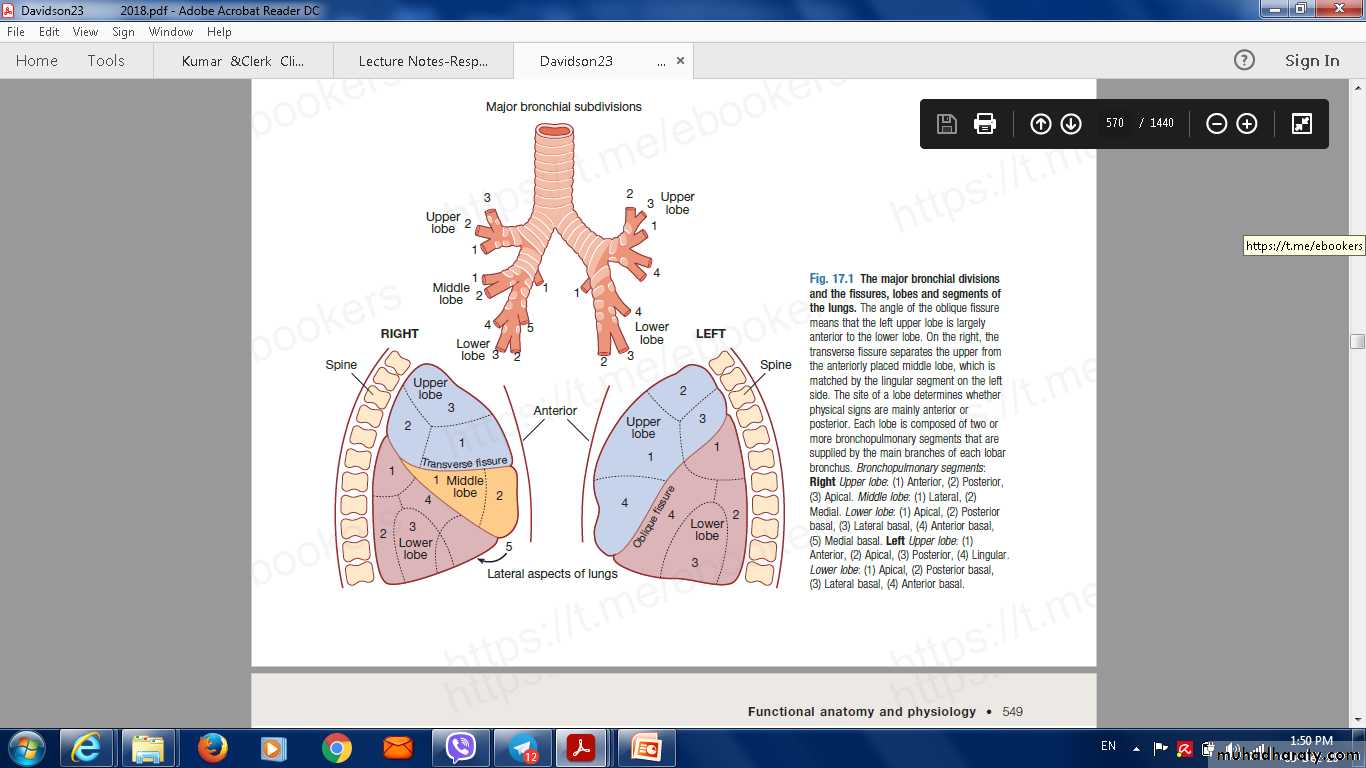
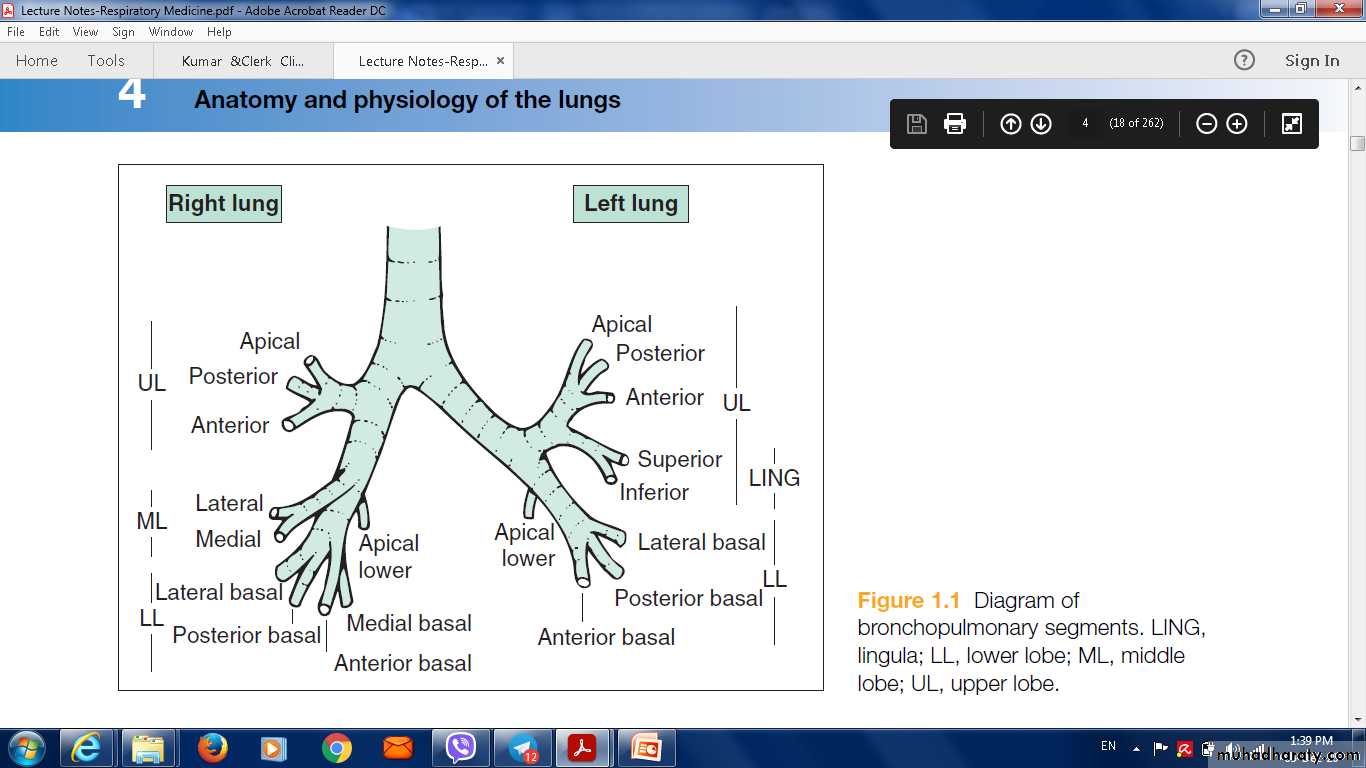
Brnchopulmonary segments
The Major Bronchial divison
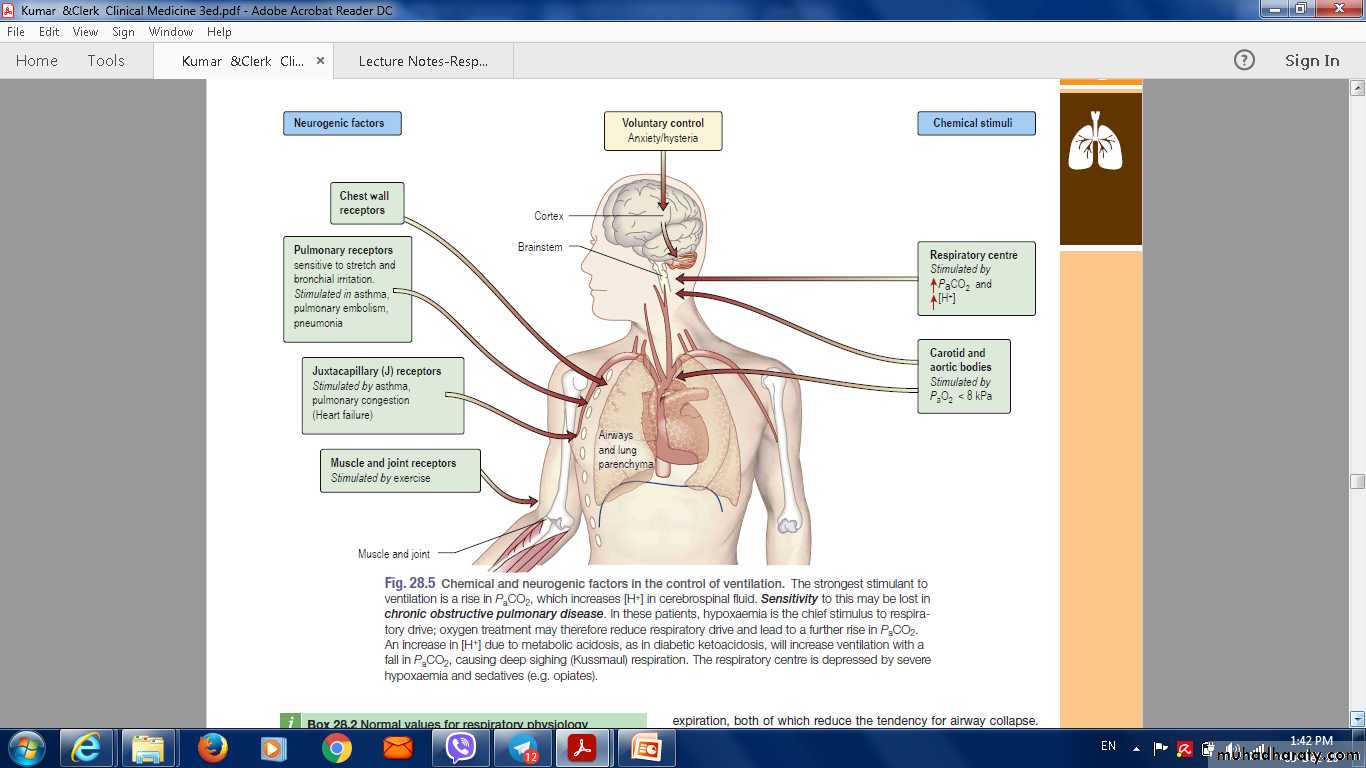
Control of breathing
The respiratory motor neurons in the medulla oblongata sense the pH of the cerebrospinal fluid (CSF) and are indirectly stimulated by a rise in arterialPCO2.
• The carotid bodies sense hypoxaemia but are mainly activated by arterial PO2 values below 8 Kpa (60 mmHg). They are also sensitised to hypoxia by raised arterial PCO2..
Muscle spindles in the respiratory muscles sense changes in mechanical load.
Cortical influences can override the automatic control of breathing.
Chemical and Neurogenic Factors in The Control of Ventilation
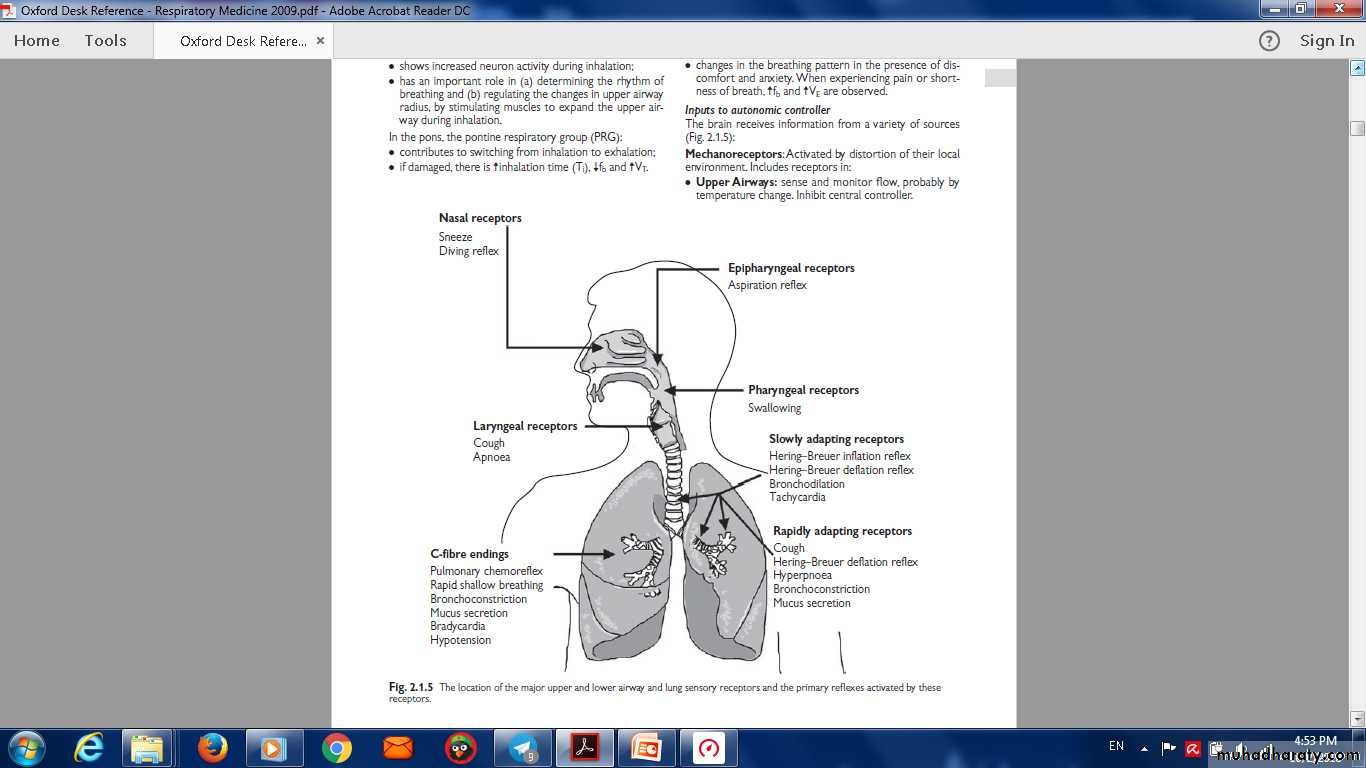
Location of major upper and lower airway receptors
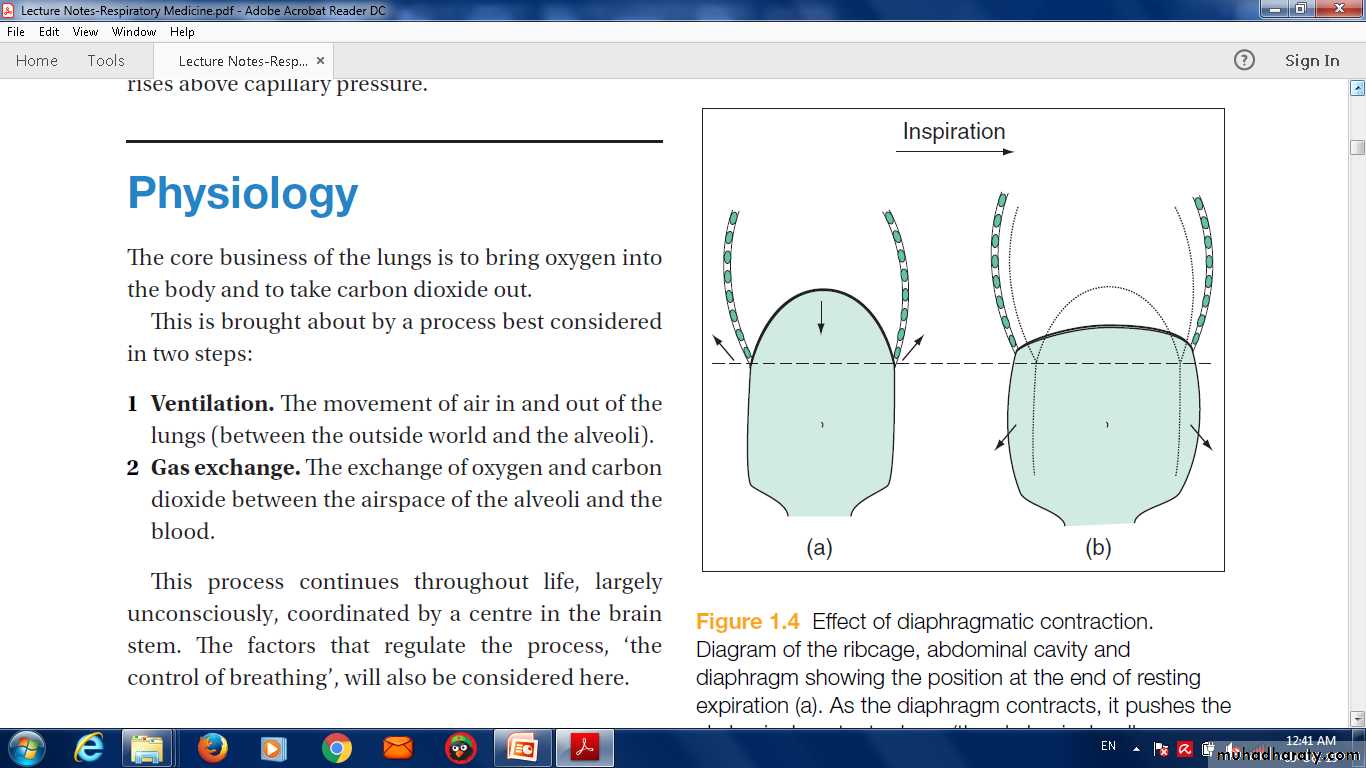
Inspiration
downward contraction of the dome-shaped diaphragm .contraction of the external intercostal muscles.
Expirationlargely passive, driven by elastic recoil of the lungs.
The increased demand in inspiration and expiration operate accessory muscles.
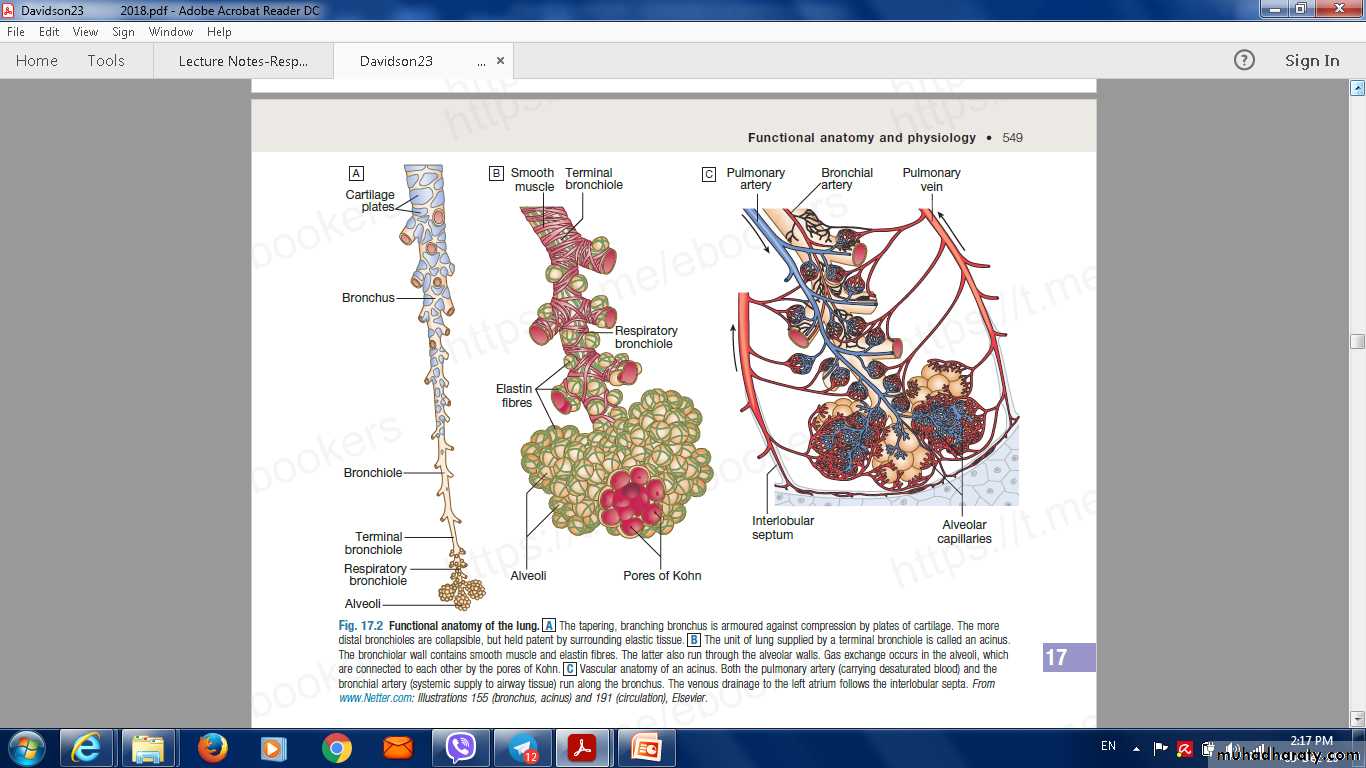
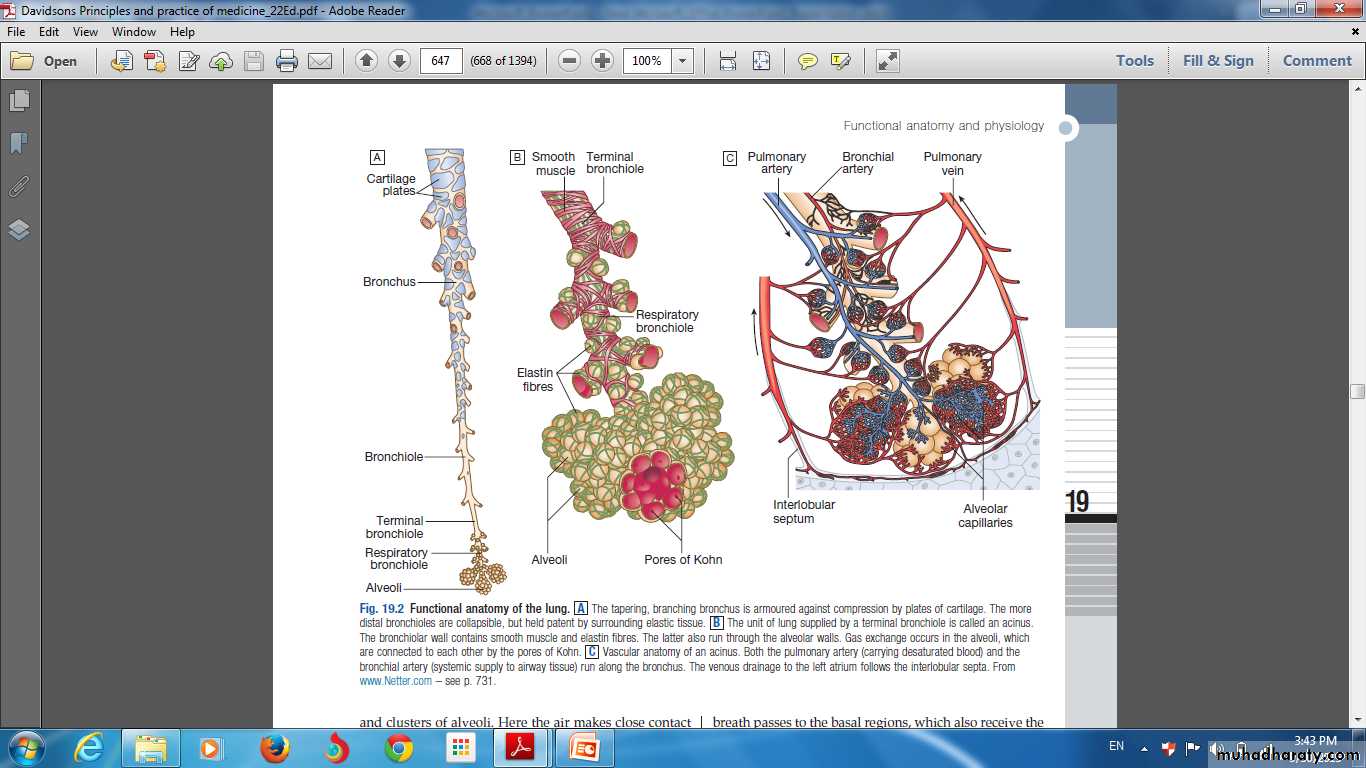
Functional Anatomy of Lungs
Functional anatomy of the lungs
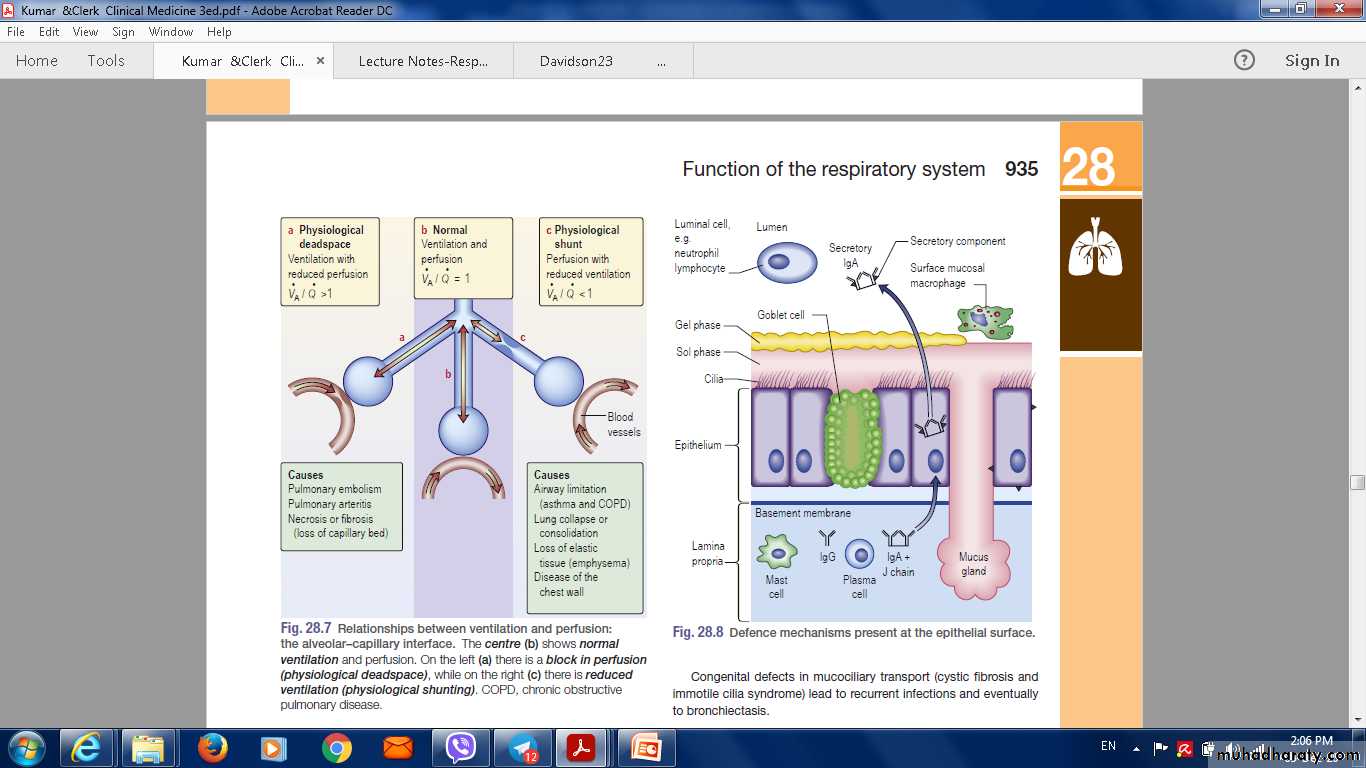
Ventilation/perfusion matching and the pulmonary circulation
Gravity determines the distribution of ventilation and blood flow in the lungs.Hypoxia constricts pulmonary arterioles
Hypercapenia dilates bronchi.
Lung disease which disturb the physiological matching of regional ventilation and perfusion, causing respiratory failure .
Diseases that destroy or thicken the alveolar capillary membrane (e.g. emphysema or fibrosis) can impair gas diffusion directly.
Ventilation perifusion relation
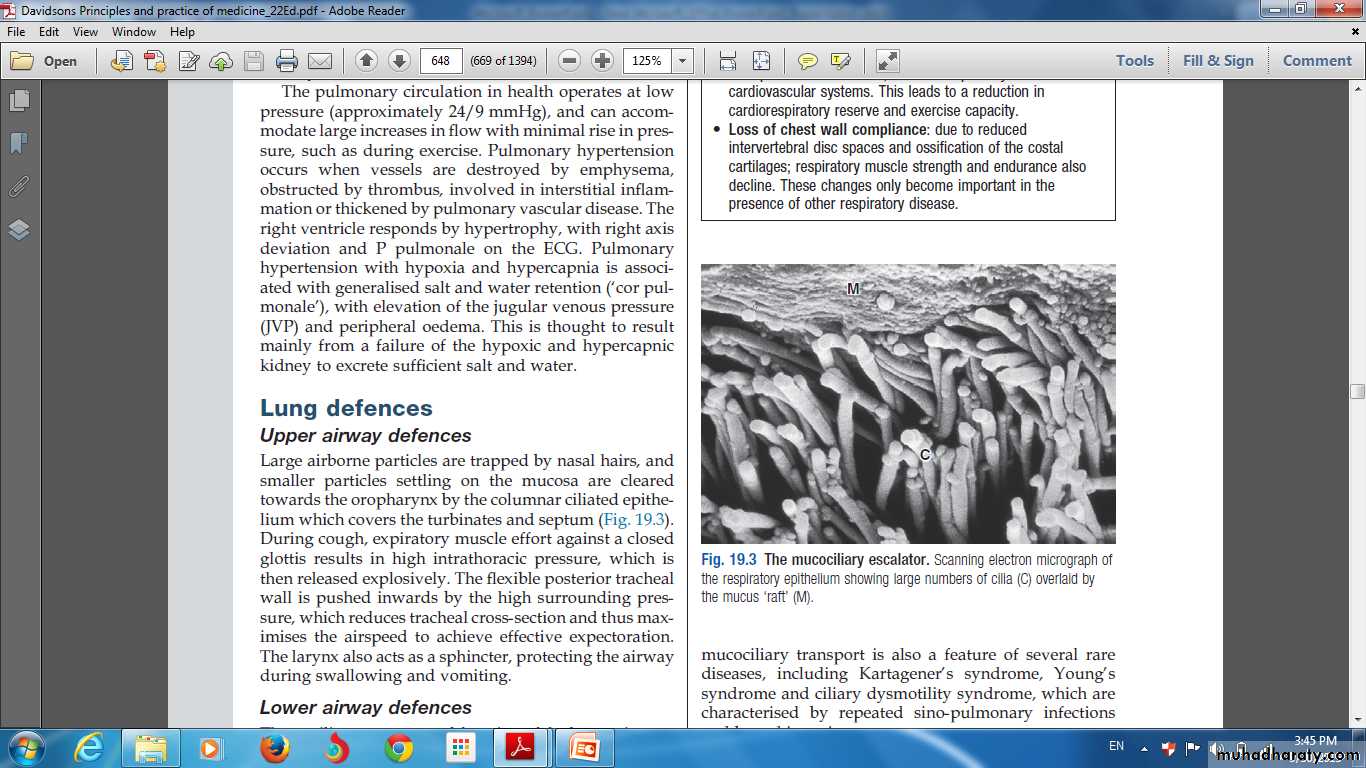
Lung defences
Upper airway defencesnasal hairs.
the columnar ciliated epithelium.
cough.
The larynx.
Lower airway defences
Non specific defencesmucociliary escalator.
Airway secretions contain an array of antimicrobial peptides.
Macrophages.
Adaptive immune defence
Lung dendritic cells.
CD4 T-helper
Defence Mechanism at the epithelial surface
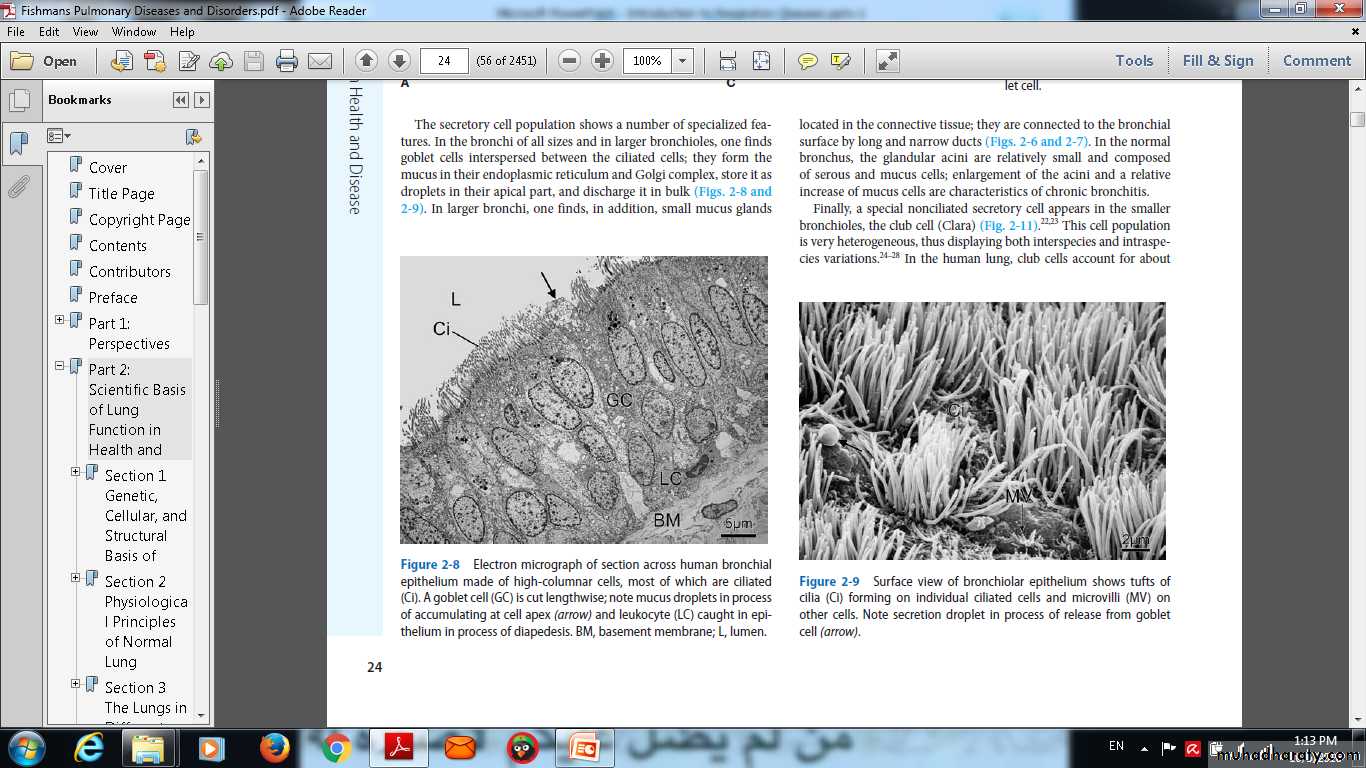
Surface view of bronchiolar epithelium shows tufts ofcilia (Ci) forming on individual ciliated cells and microvilli (MV) onother cells. Note secretion droplet in process of release from gobletcell (arrow).
Mucociliary escelator
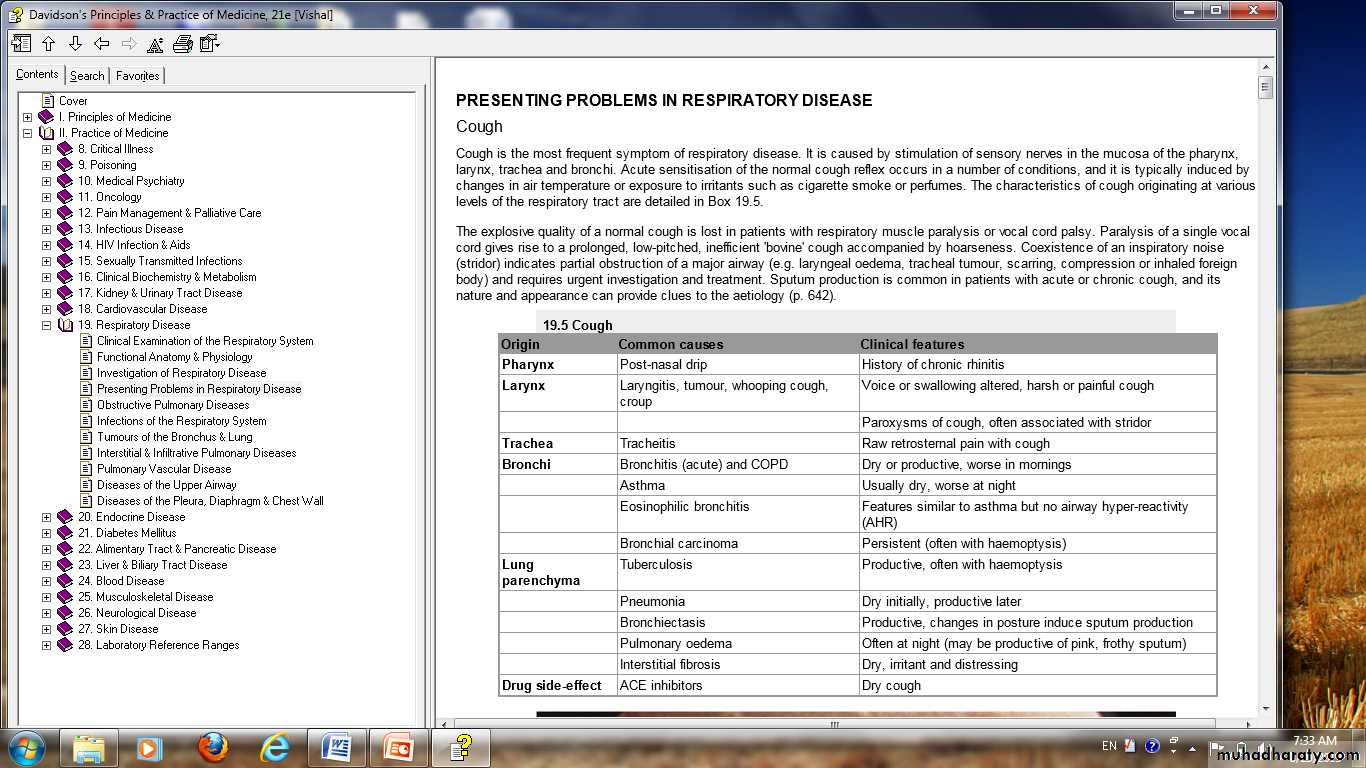
PRESENTING PROBLEMS IN RESPIRATORY DISEASE
CoughThe most frequent symptom of respiratory disease.
Sputum production is common
Acute less than 3 weeks.
Subacute 3 -8 weeks.
Chronic more than 8 weeks.
Acute transient cough
Viral lower respiratory tract infection.
post-nasal drip resulting from rhinitis or sinusitis,
aspiration of a foreign body,
laryngitis
pharyngitis.
Cough occurs in the context of more serious diseases, pneumonia.
Aspiration.
Congestive heart failure.
pulmonary embolism.
chronic cough
• cough-variant asthma.• post-nasal drip secondary to nasal or sinus disease.
• gastro-oesophageal reflux with aspiration.
• angiotensin-converting enzyme (ACE) inhibitors .
• Bordetella pertussis infection in adults .
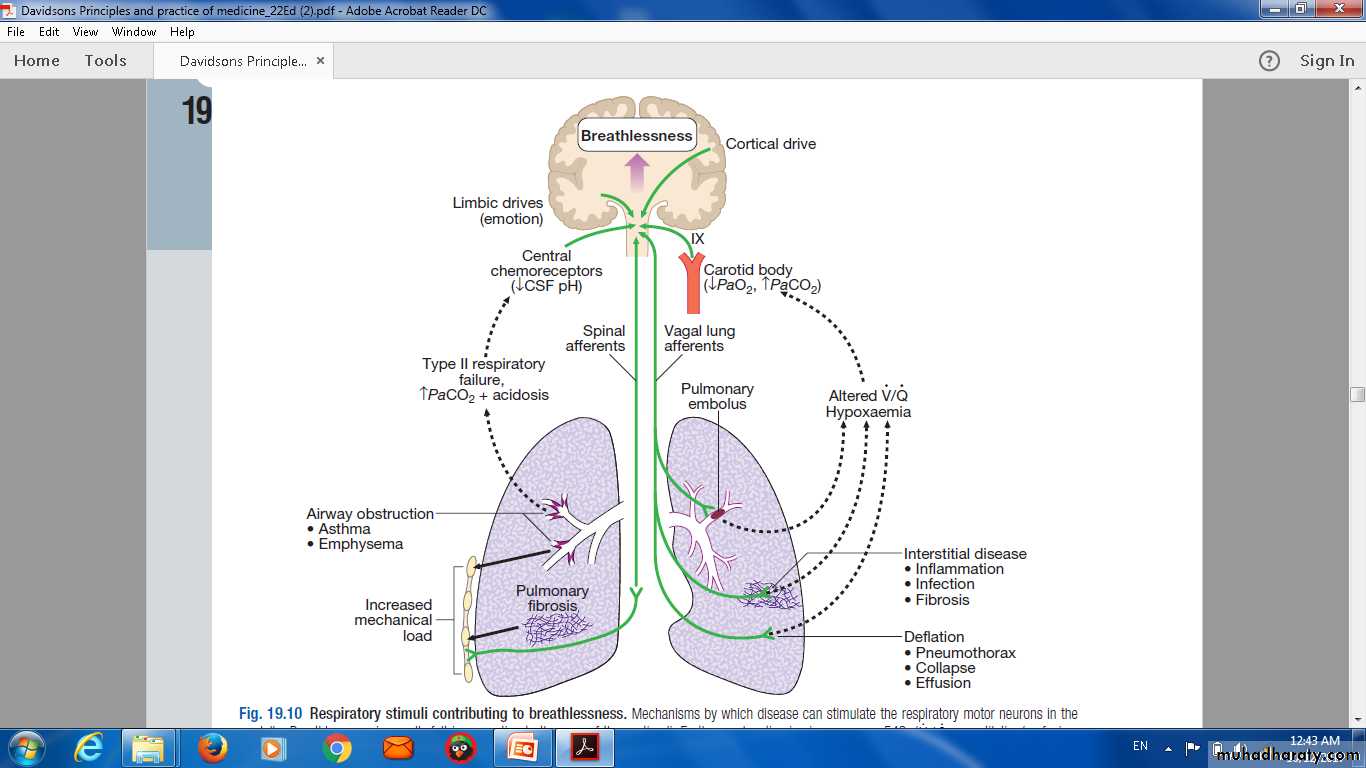
Respiratory stimuli contributing to breathlessness. Mechanisms by which disease can stimulate the respiratory motor neurons in themedulla. Breathlessness is usually felt in proportion to the sum of these stimuli. Further explanation is given on page 543. (V / Q = ventilation/perfusionmatch)
Breathlessness
Pathophysiology :
Respiratory diseases can stimulate breathing and dyspnoea by:
stimulating intrapulmonary sensory nerves .
increasing the mechanical load on the respiratory muscle.
causing hypoxia, hypercapnia or acidosis, stimulating chemoreceptors.
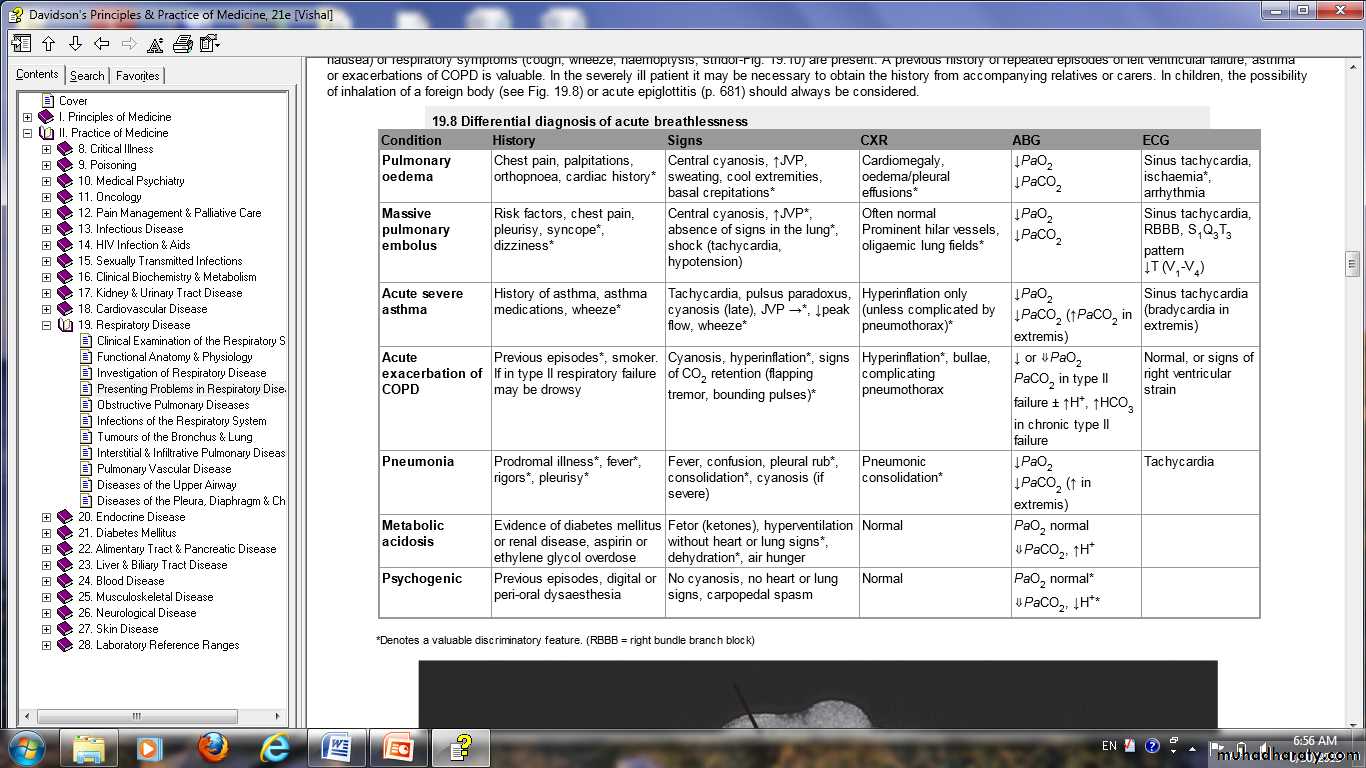
Differential diagnosis of acute breathlessnss
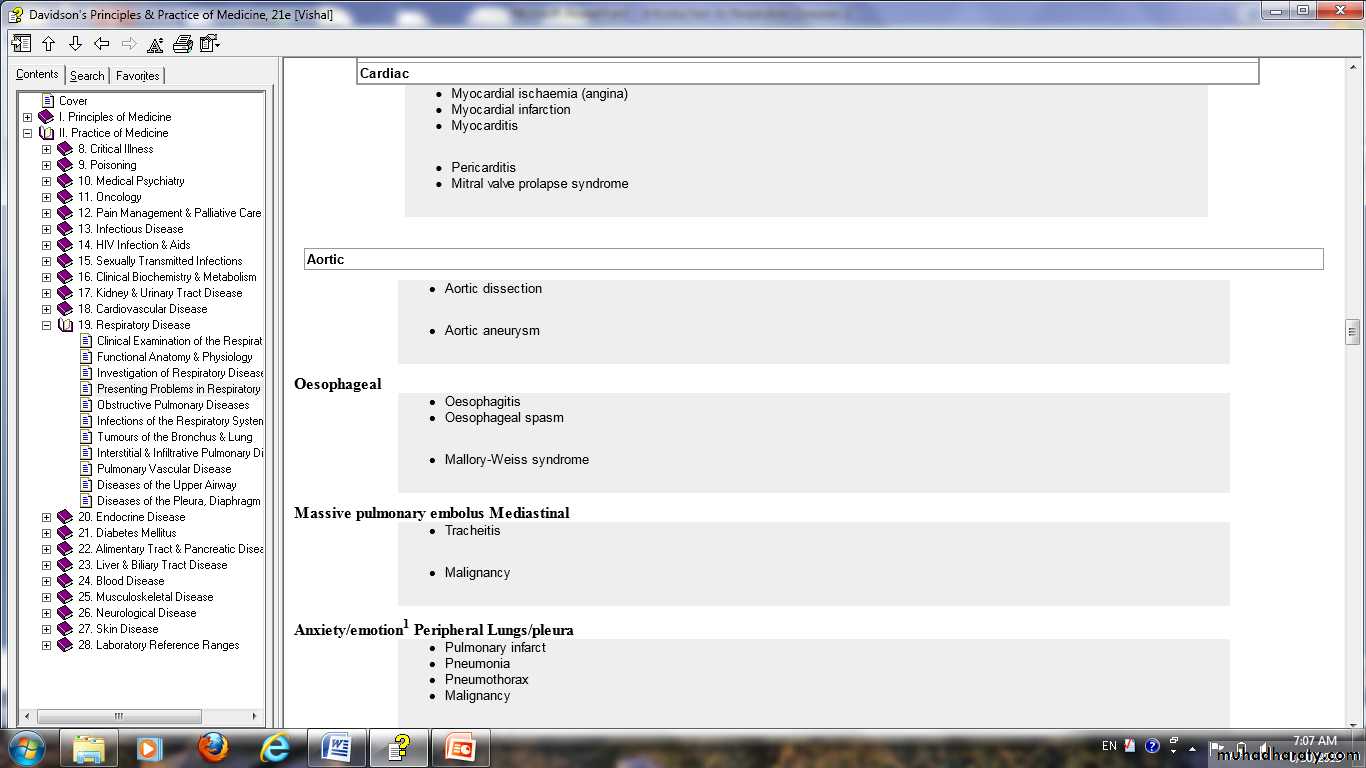
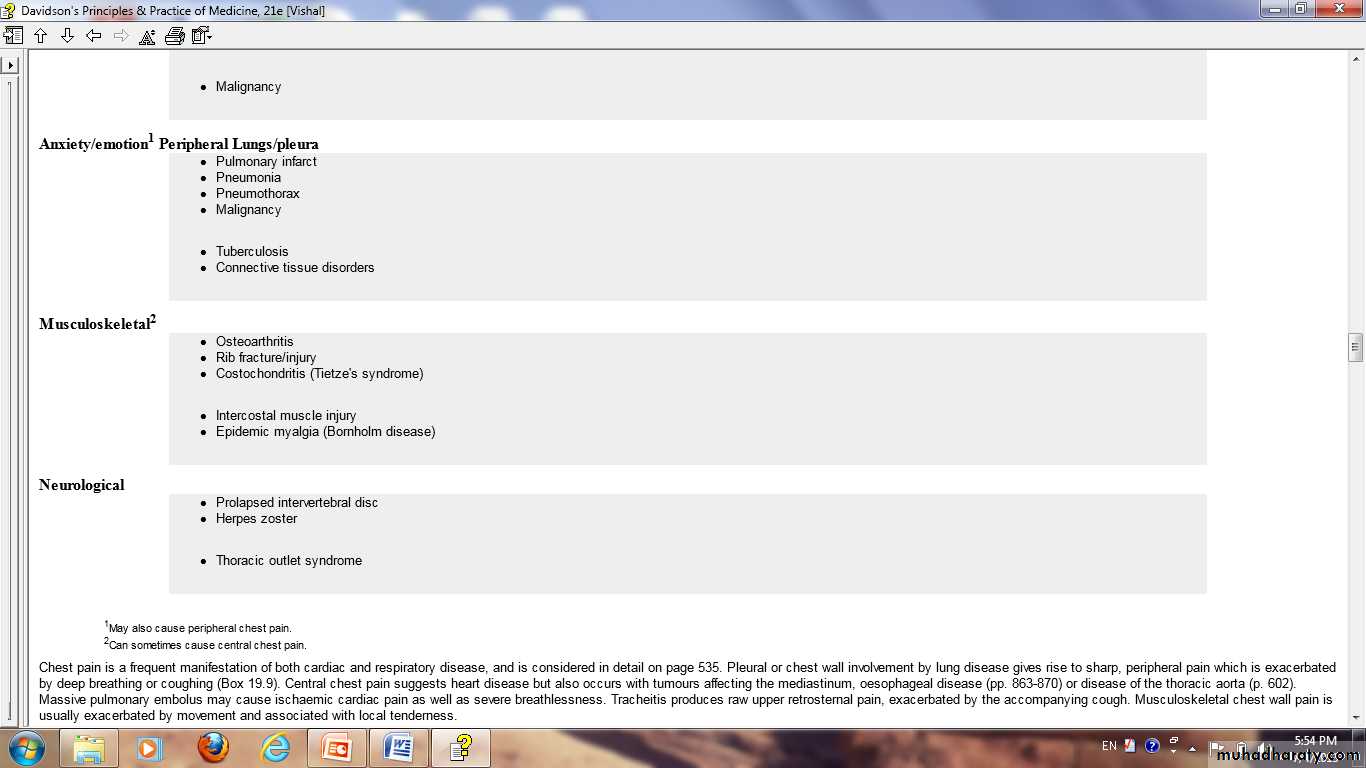
Chest pain :differential diagnosis
Haemoptysis
Coughing up blood. Many episodes of haemoptysis remain unexplained even after full investigationCauses of haemoptysis
Bronchial diseaseCarcinoma
BronchiectasisAcute bronchitis
Others.
Parenchymal disease
TuberculosisOthers.
Lung vascular disease
Pulmonary infarctionGoodpasture's syndrome
Others.
Cardiovascular disease
Acute left ventricular failure.
Mitral stenosis .
Others.
Blood disorders
LeukaemiaOthers
Sputum
pleural effusion
Causes of pleural effusion Common causes Pneumonia ('para-pneumonic effusion')Tuberculosis
Pulmonary infarction*
Malignant disease
Cardiac failure*
Subdiaphragmatic disorders (subphrenic abscess, pancreatitis etc.)
Uncommon causes
Hypoproteinaemia* (nephrotic syndrome, liver failure, malnutrition)
Connective tissue diseases* (particularly systemic lupus erythematosus (SLE) and rheumatoid arthritis)
Acute rheumatic fever
Post-myocardial infarction syndrome
Meigs' syndrome (ovarian tumour plus pleural effusion)
Myxoedema*
Uraemia*
Asbestos-related benign pleural effusion
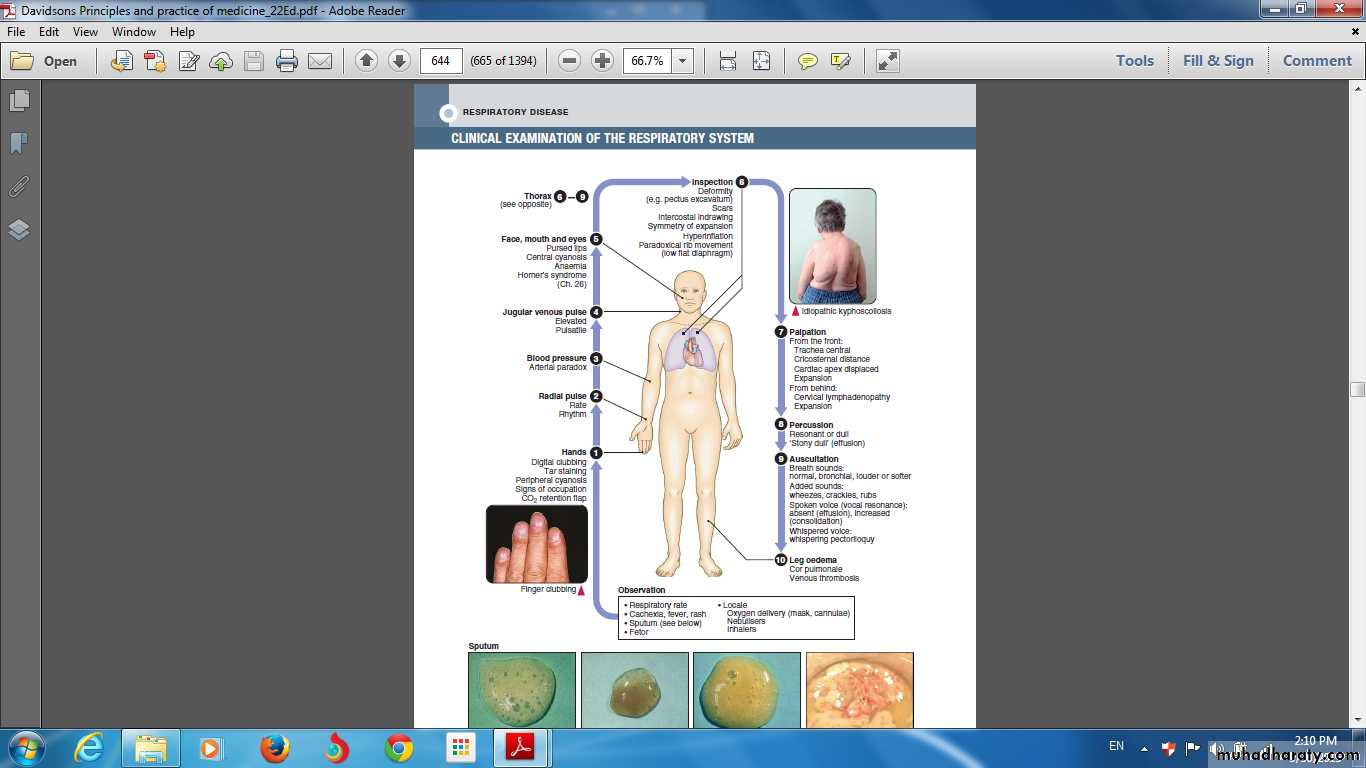
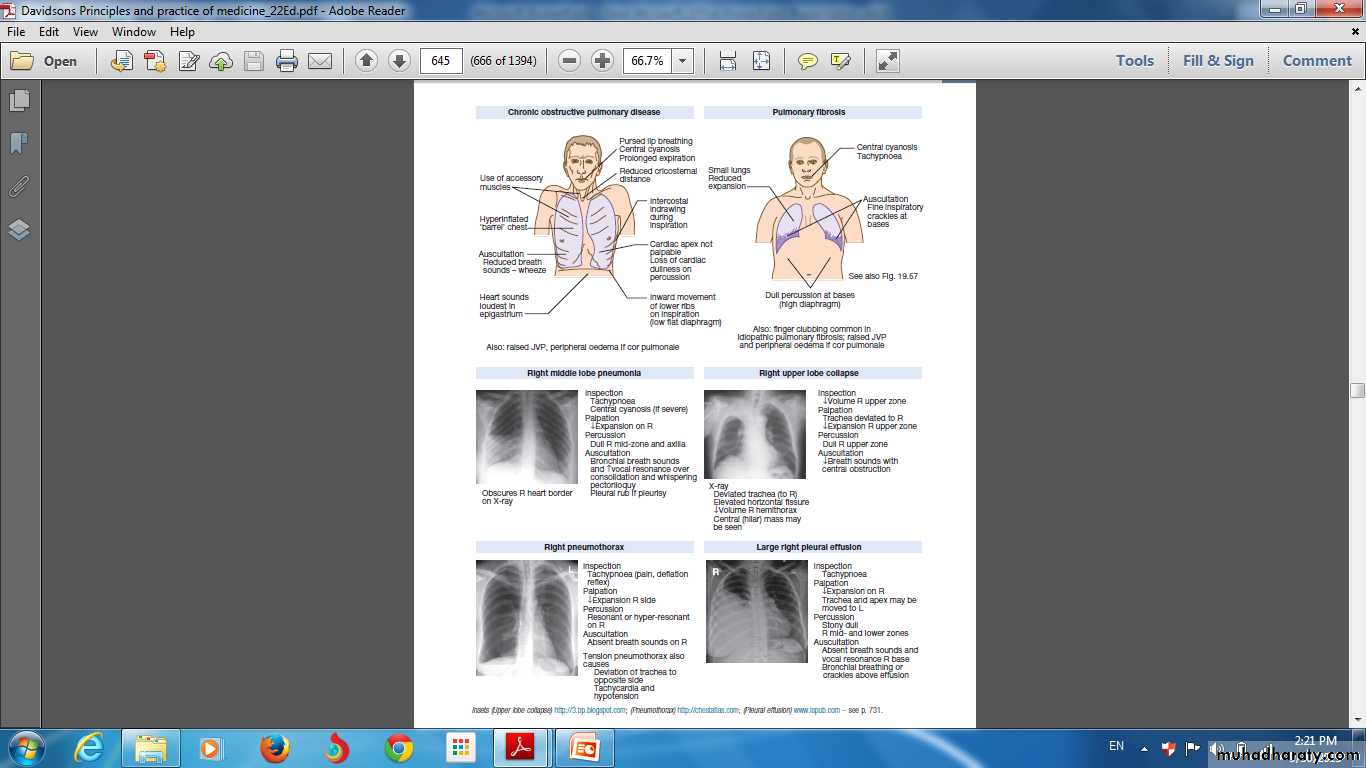
Signs in respiratory disease
INVESTIGATION OF RESPIRATORY DISEASE
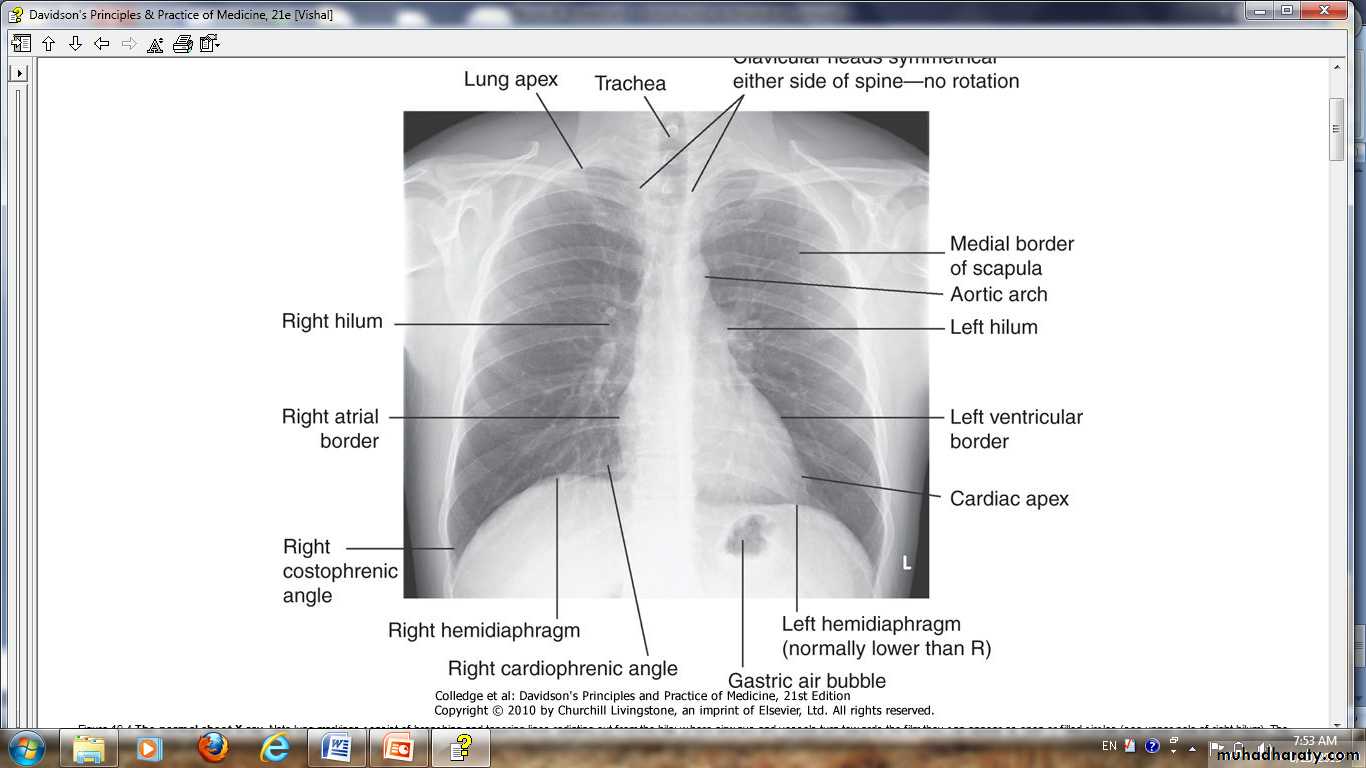
ImagingThe 'plain' chest X-ray
A postero-anterior (PA) film
lateral film.
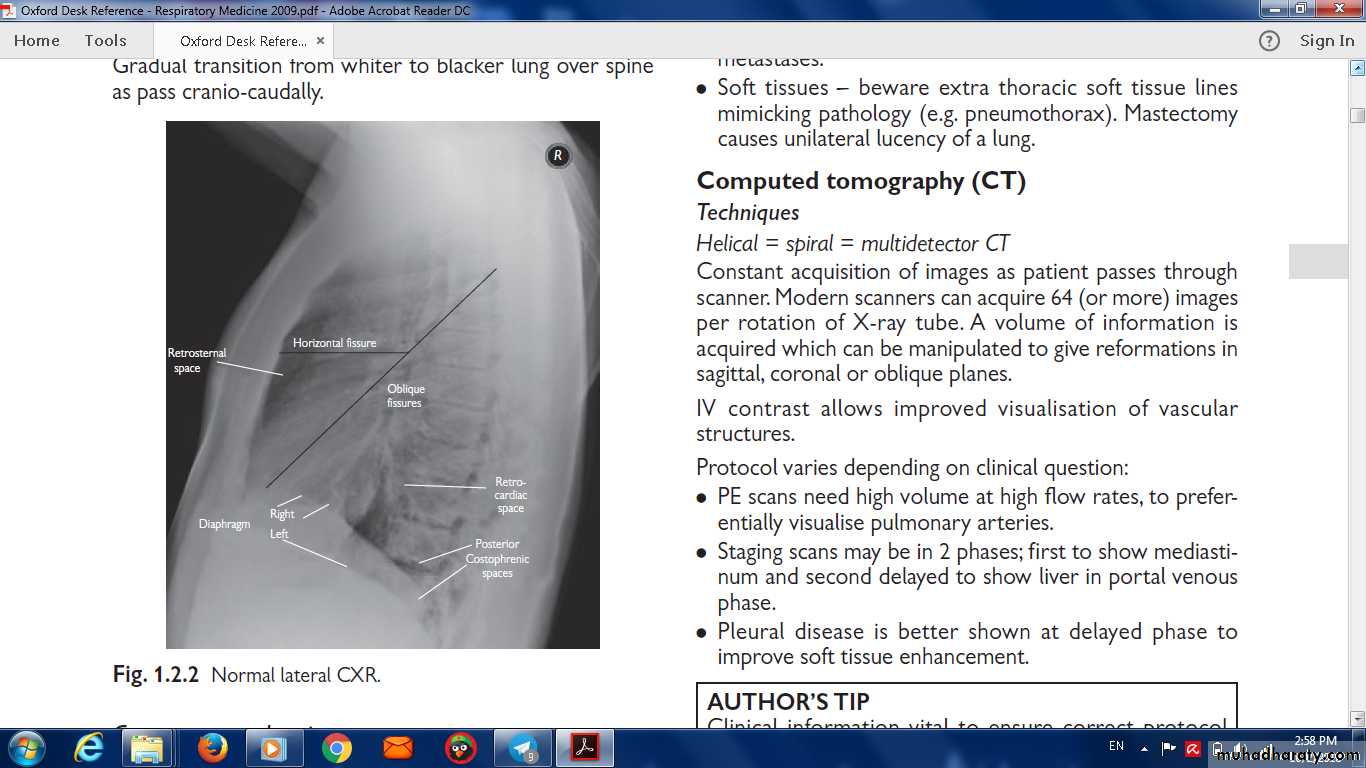
Normal lateral CXR
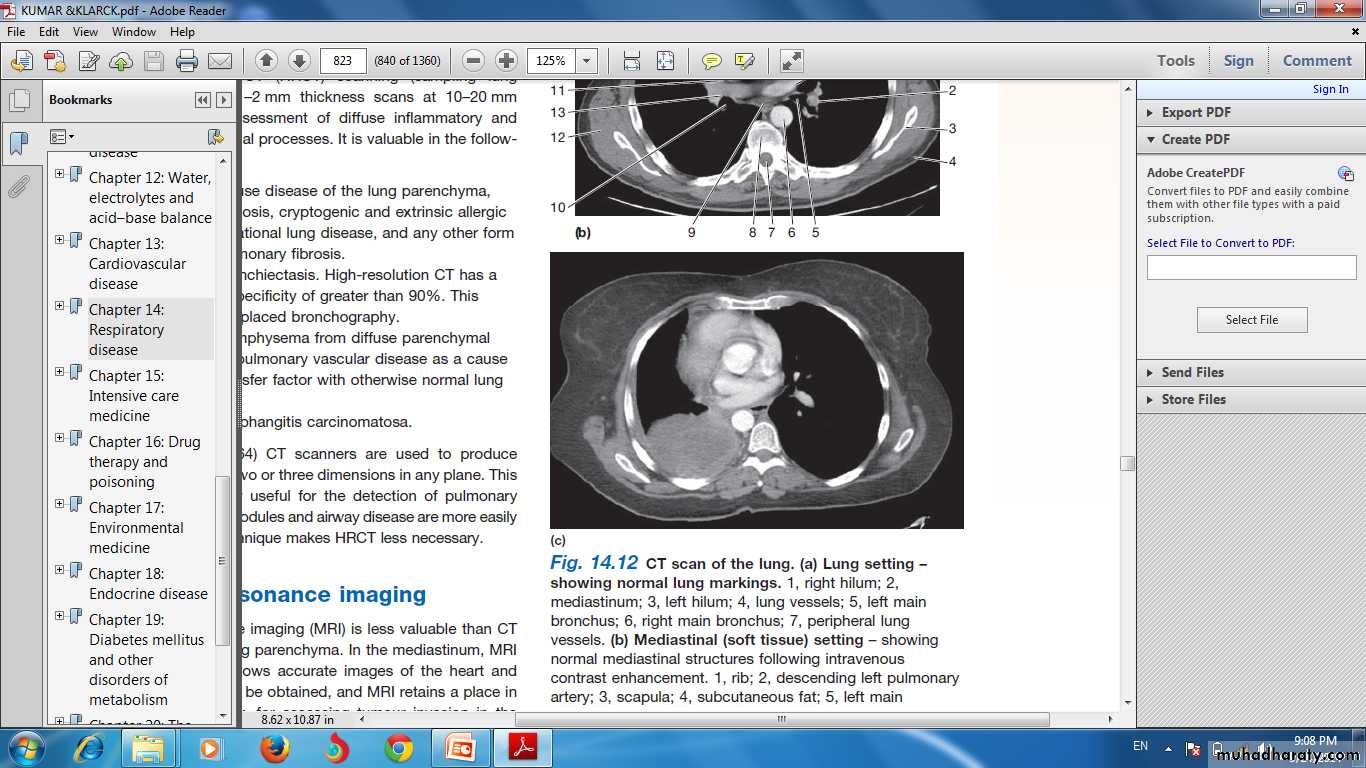
Computed tomography (CT)
CT provides detailed images of the pulmonary parenchyma, mediastinum, pleura and bony structures .High-resolution CT (HRCT)
CT pulmonary angiography (CTPA)
Positron emission tomography (PET)
The radiotracer taken up by malignant tissue.
Computed tomography (CT)
Ultrasound Ultrasound is sensitive at detecting pleural fluid .
pleural biopsy.guide needle biopsy.
Endobronchial ultrasound .
A resin cast of the human airway tree shows the dichotomousbranching of the bronchi from the trachea and the systematicreduction of airway diameter and length with progressive branching. Inthe left lung the pulmonary arteries (red) and veins (blue) .
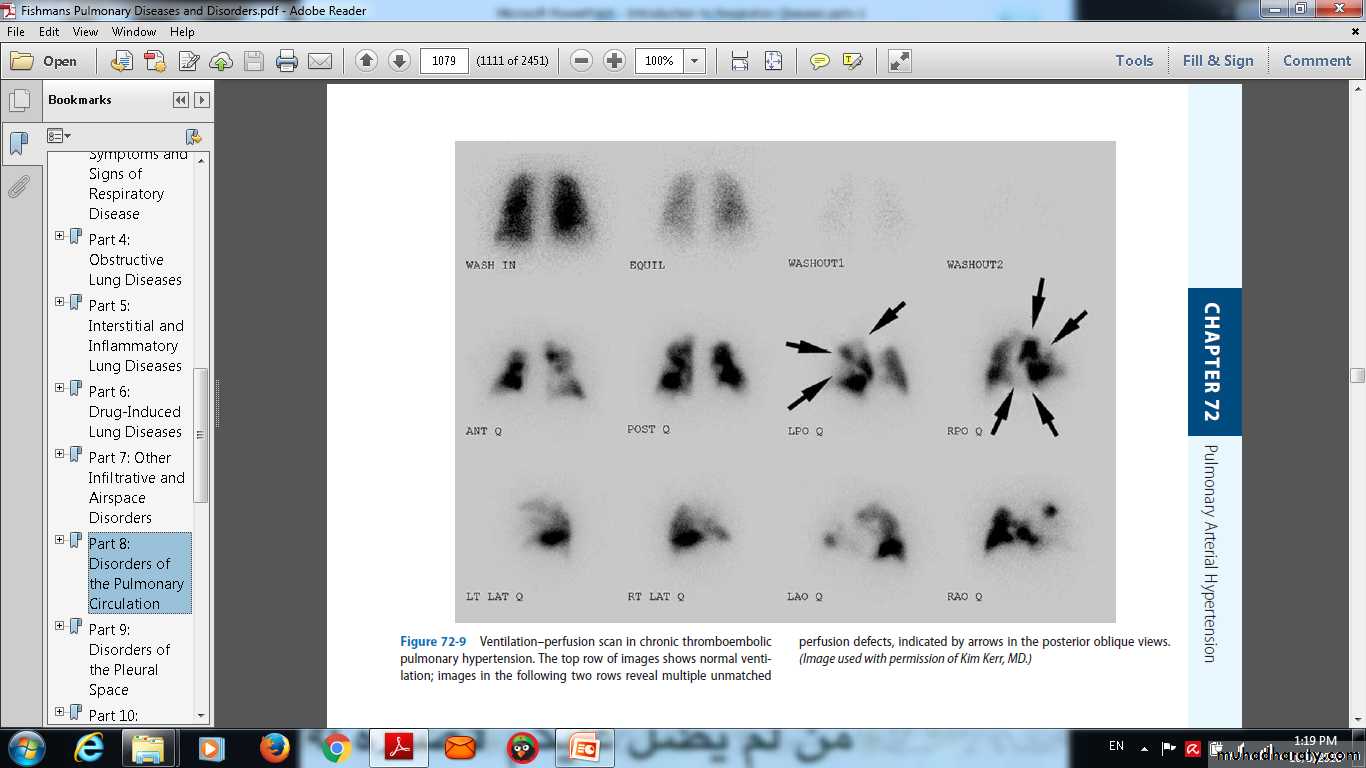
Ventilation-perfusion imaging
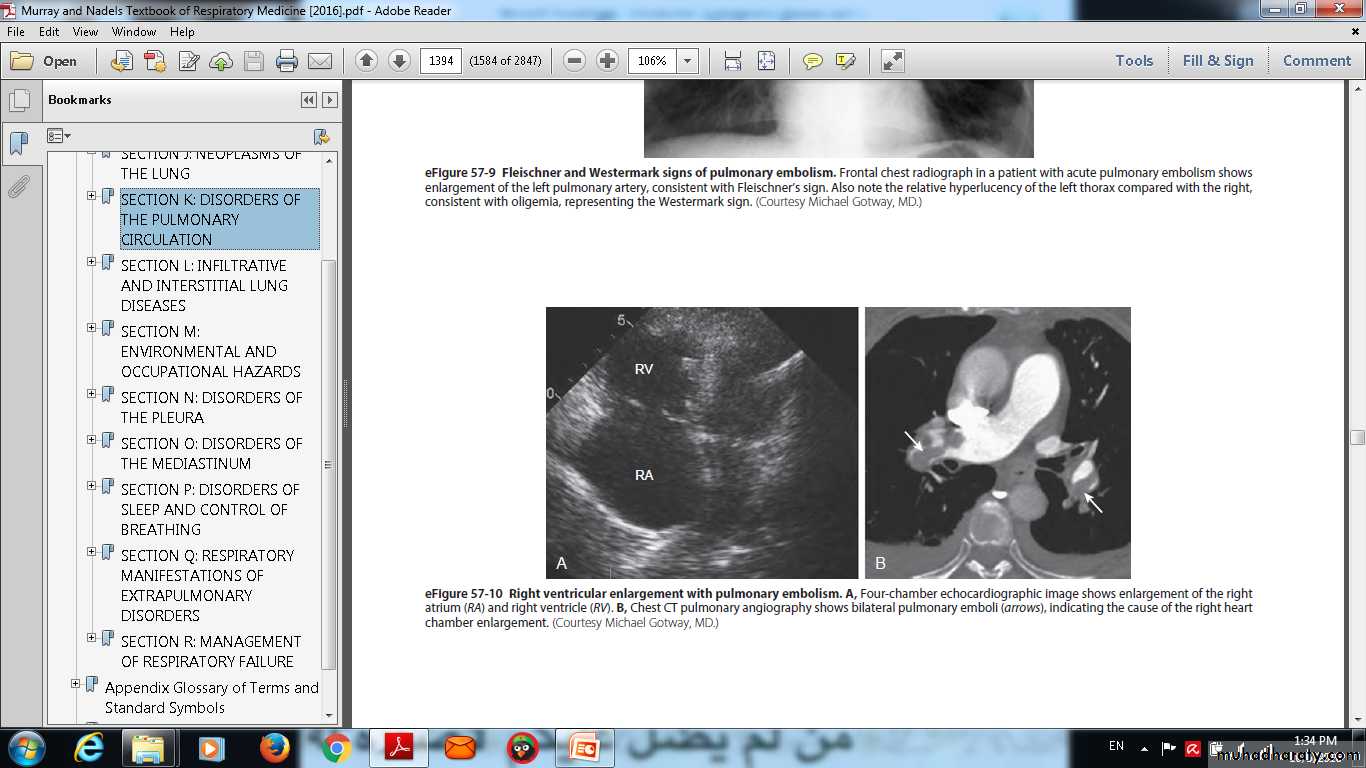
Pulmonary angiography
Echocardiography
Endoscopic examination
LaryngoscopyBronchoscopy
Assessment of the mediastinummediastinoscope
Endobronchial ultrasound (EBUS)
endoscopic ultrasound (EUS).
Investigation of pleural disease
The pleural biopsy using an(1)Abram's needle (2)core biopsy guided by either ultrasound or CT.
Thoracoscopy.
Skin tests
The tuberculin test.
Skin hypersensitivity tests.
Immunological and serological tests
Microbiological investigations
Histopathological and cytological examination .
Cytological examination
Immunological and serological tests
The pneumococcal antigen.Influenza viruses can be detected in throat swab samples.
Legionella, Mycoplasma, Chlamydia or viruses) antibody titres may eventually.
hypersensitivity pneumonitis Precipitating antibodies .
Total levels of immunoglobulin E (IgE), and levels of IgE
Respiratory function testing
Respiratory function tests are used to aid diagnosis.assess functional impairment.
monitor treatment or progression of disease.
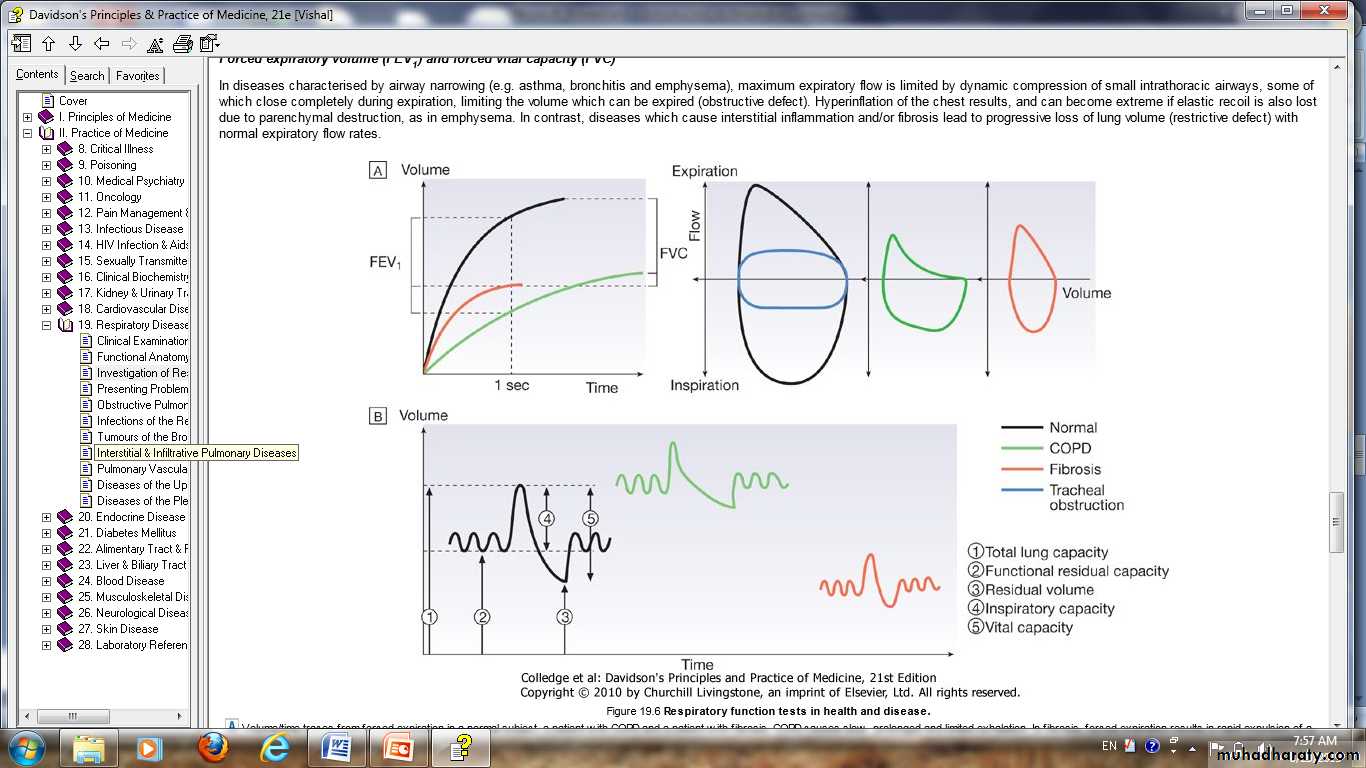
Forced expiratory volume (FEV1) and forced vital capacity (FVC)
Flow/volume loops
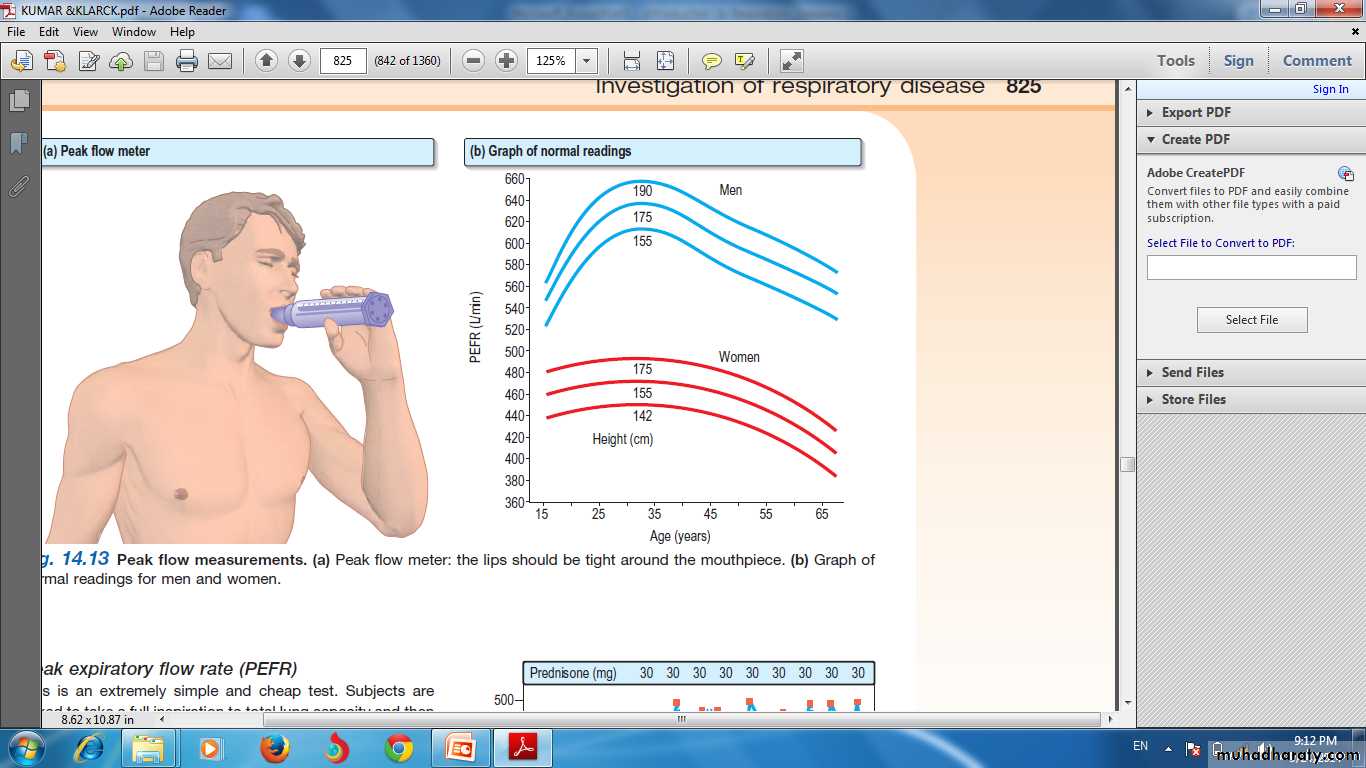
Peak flowmeter
Lung volumes
spirometry.Body plethysmography
Transfer factor
Q
QUIZE