
BRANCHES OF ORTHODONTICS
Orthodontics can be divided into three categories based on the nature and
time of intervention.
• Preventive orthodontics
• lnterceptive orthodontics
• Corrective orthodontics.
PREVENTIVE ORTHODONTICS
It is defined as the action taken to preserve the integrity of what appears to
be a normal occlusion at a specific time. supervision of the growth and
development of the dentition and the cranio-facial structures, the diagnostic
procedures undertaken to predict the appearance of malocclusion and the
treatment procedures instituted to prevent the onset of malocclusion .
1. Caries control
2. Parent counseling
3. Space maintenance
4. Exfoliation of deciduous teeth
5. Abnormal frenal attachments
6. Treatment of locked permanent first molars
INTERCEPTIVE ORTHODONTICS
Is that phase of orthodontics that recognize and eliminate potential
irregularities and malpositions in the developing dentofacial complex. It
implies that corrective measures may be necessary to prevent a potential
irregularity from progressing into a more severe malocclusion, The basic
interceptive procedures that are undertaken by the interceptive pedodontist
are:
1. Space regaining
2. Correction of anterior and posterior cross bites
3. Elimination of oral habits
4. Muscle exercises
5. Removal of soft or hard tissue present in the pathway of emption
Orthodontic Diagnosis
Relationships of the teeth and jaws :
• Arch alignment and symmetry
• Anteroposterior characteristics
• Transverse characteristics
• Vertical characteristics
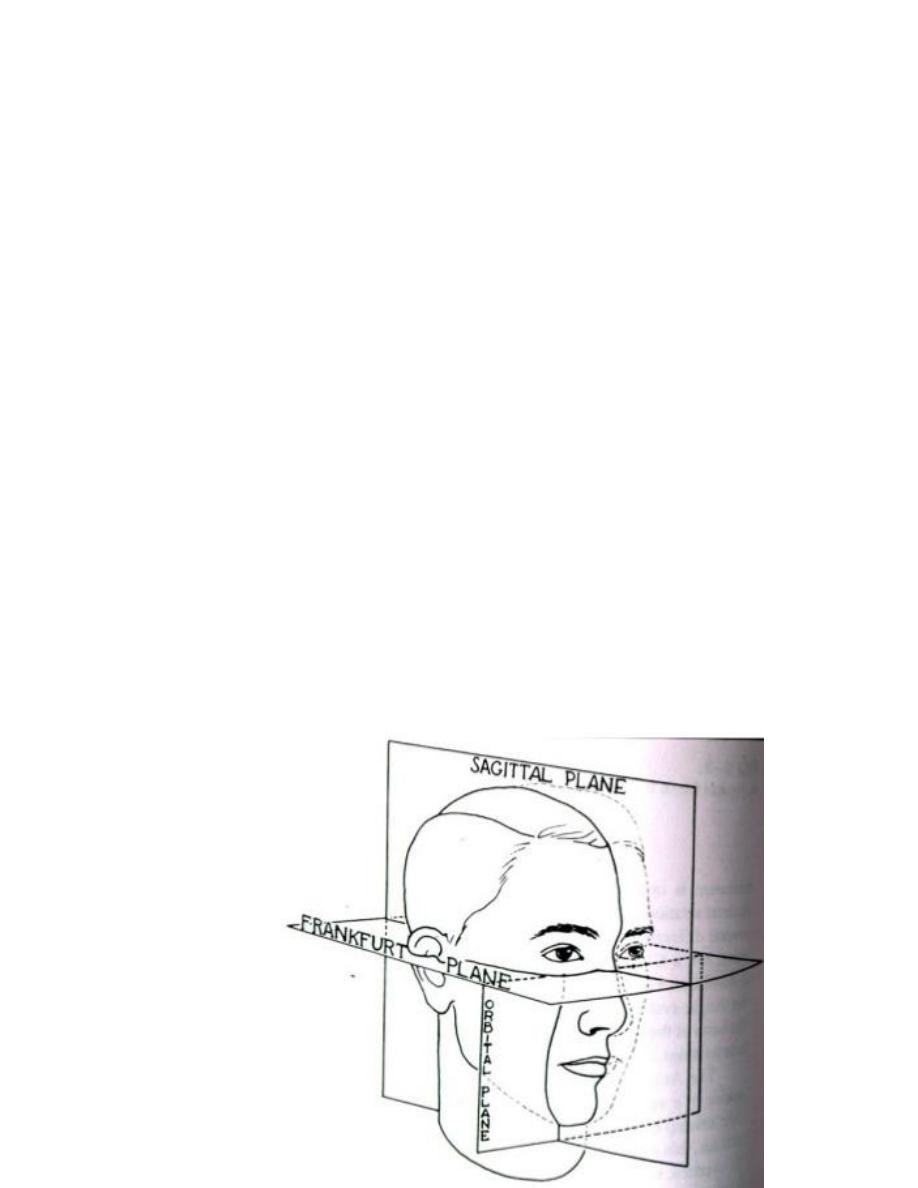
• Orientation of the occlusal plane in NHP(natural head position) i.e.,
standing or sitting up), not with the patient prone in a dental chair.
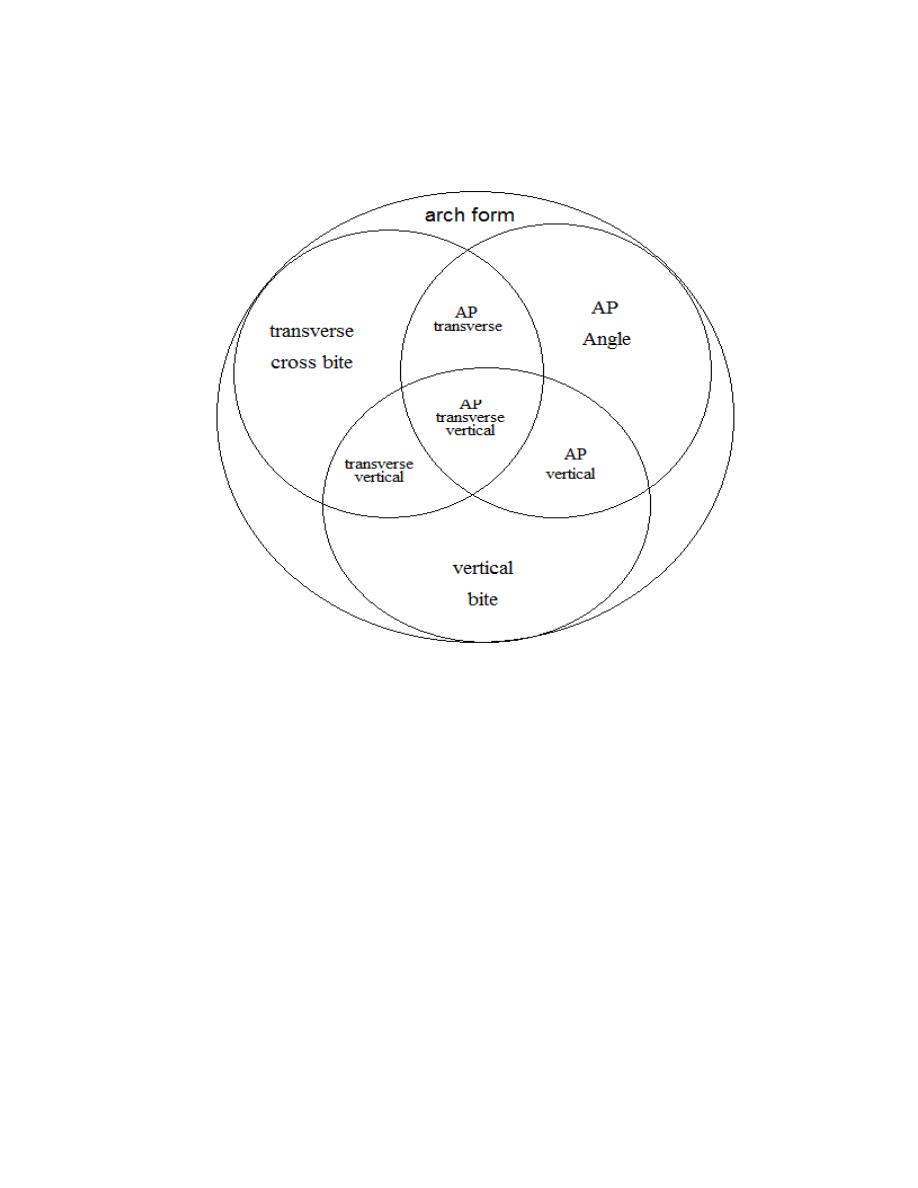
Ackerman-Proffit orthogonal analysis. representing arch form in three planes
of space
Essential diagnostic aids
Those are considered essential for the diagnosis of an orthodontic
case. Ideally before starting a case, a treating clinicianmust possess these
aids. These include the following.
1. Case history
2. Clinical examination
3. Study models
4. Certain radiographs:
Periapical radiographs
Lateral radiographs(cephalometric radiograph)

Orthopantomograms
Bite wing radiographs.
5. Facial photographs.
Non-essential or supplemental diagnostic aids
These diagnostic aids may be required only in certain cases and may
require specialized equipment, which might not be available in every dental
clinic. The supplemental diagnostic aids include:
1. Specialized radiographs; like
Occlusal views of maxilla and/or mandible.
Selected lateral jaw views, etc.
2. Electromyographic examination of muscle activity
3. Hand-wrist radiographs
4. Computed axial tomography (CT scan)
5. Magnetic Resonance Imaging (MRI)
6. Endocrine tests and/or other blood tests
7. Estimation of the basal metabolic rate
8. Sensitivity (vitality) tests
9. Biopsy.

CASE HISTORY
Case history is the information gathered from the patient and/or parent
to aid in the overall diagnosis of the case. It includes certain personal details,
the chief complaint, past and present dental and medical history and any
associated family history. The aim is to establish a rapport with the patient
and to obtain an accurate account of the individual's complaints, which,
following examination will enable, a diagnosis to be made.
Name
The patients name should be recorded not only for the purpose of
communication and identification but because it gives a personal touch to
the following conversation. It makes the patients more comfortable when he
is addressed by his first name and arouses a feeling of familiarity, which has
a positive psychological effect on the patient.
Age and Date of Birth
The chronologic age of the patient helps in diagnosis, treatment
planning and growth prediction. Certain transient conditions, which might be
perceived as malocclusion by the patient and parents, can be identified and
the concerned are counseled accordingly. The age of the patient also dictates
the use of certain treatment protocols-for example, surgical correction might
be advocated following cessation of growth whereas the same malocclusion
might be treated using functional appliances if the patient has a potential to
grow.

Sex:
Sex of the patient also helps in treatment planning. Girls mature
earlier than boys, i.e. the timing of growth related events including growth
spurts, eruption of teeth and onset of puberty are different in males and
females.
Address and Occupation
These are important for communication, assessing the socioeconomic
status as well as for records. The socioeconomic status might dictate the kind
of appliance required. Also, patients coming from far may require a different
appliance therapy as they might not be able to visit the clinician more
frequently.
CHIEF COMPLAINT
The patient's chief complaint should be recorded in his or her own
words. It should mention the conditions the patient feels he / she is suffering
from. This helps in identifying the priorities and desires of the patients. The
parents' perception of the malocclusion should also be noted. This will help
in setting the treatment objectives and satisfying the family in general.
At the first meeting, the orthodontist should not assume that
appearance is the patient’s major concern just because the teeth appear
unattractive. Nor should the dentist focus on the functional implications of,
for instance, a crossbite with a lateral shift without appreciating the patient’s
concern about what seems to be a trivial space between the maxillary central
incisors. As we have noted, for an individual with what appears to be
reasonably normal function and appearance and appropriate psychosocial
adaptation, the major reason for treatment may well be a desire to improve

appearance “beyond normal.” The greater orientation of modern family
practice toward cosmetic dentistry increases the chance that a patient may be
referred to an orthodontist for comprehensive treatment to improve dental
and facial appearance
.
MEDICAL HISTORY
Knowledge of a patient's general health is essential and should be
obtained prior to examination. It is best obtained by a questionnaire. In most
cases orthodontic treatment can be undertaken but precautions may be
required prior to extractions. Antibiotic coverage may be required in patients
with rheumatic fever or cardiac anomalies even for molar band
placement/removal, if the adjacent gums are inflamed or bleeding is
anticipated. Mentally or physically challenged patients may require special
management.
The first, of course, is when the patient last saw his or her physician.
If it was within the last year and was for a regular checkup, this usually is a
good sign. Another important question is whether the patient has ever been
hospitalized and, if so, for what reason. For prospective orthodontic patients,
one usually includes a specific question as to whether the patient has had a
tonsillectomy and/or an adenoidectomy. This may be a clue that the patient
had an earlier airway problem, which might have affected the jaw and
tongue posture. Sometimes the admission to the hospital was the result of
trauma, and it is important to know whether the jaws, face, or teeth were
involved in the accident. If they were, the orthodontist should be particularly
vigilant regarding facial asymmetry that may have resulted from a healed
subcondylar fracture. A closer look at the panoramic radiograph would be
indicated if this is a suspicion. If the injury involved one or more teeth, a
closer evaluation of the vitality of the teeth involved is clearly indicated, and
the patient or parent should be made aware that orthodontic tooth movement
can possibly exacerbate periapical symptoms.
DENTAL HISTORY
The patient's dental history should include information on the age of
eruption and exfoliation of deciduous and permanent teeth. Reason for
exfoliation will also hint at the oral hygiene maintenance capabilities of the
patient. The past dental history will also help in assessing the patients and
parents attitude towards dental health.
Patient treated for arthritis or osteoporosis, high doses of
prostaglandin inhibitors or resorption-inhibiting agents may impede
orthodontic tooth movement. These examples should serve as a reminder
that an orthodontist must know the contraindications of orthodontic
treatment and be able to rule out that any of these factors are involved with
any given patient.
Clinical Examination
General Examination
General examination should begin as soon as the patient first comes to
the clinic. A general appraisal of the patient is done. The clinician should
observe the gait, posture and physique of the patient. Height and weight are
recorded to assess for the physical growth and development of the patient.
Abnormal gait may be present due to an underlying neuromuscular disorder.
Abnormal posture also may lead to mal-occlusions.
The orthodontist should make some diagnostic determinations “from
the doorway” regarding the patient’s face, posture, and expression. One can
often tell from the first moment whether the orthodontic problem will be
largely a dental one or a difficult skeletal or facial problem.
It is best for the mutual confidence of the parent, patient, dentist, and
orthodontist to make these dental health determinations before treatment
begins. If told earlier, the parent or patient views it as an explanation. If
explained after the fact, they see it as an excuse! Because parents often do
not realize the relationship between overall health, dental health, and
dentofacial development, persistence in pursuing these questions is
important.
Cephalic and Facial Examination
This includes assessing anterior tooth display, as well as the relative
convexity and concavity and divergence of the face in profile view and
vertical proportions of the face. As discussed previously, faces can be
categorized in profile view by their relative convexity and divergence.
The shape of the head can be evaluated based on the cephalic index of
the head which was formulated as:
Maximum skull width
I
= ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ
Maximum skull length
Index values
• Mesocephalic (average)
• Brachycephalic (short, broad skull)
• Dolicocephalic (long, narrow skull)
Brachycephalic(round) Mesocephalic(oval) Dolicocephalic(long
oval)
Assessment of Facial Symmetry
The shape of the face is assessed by the morphologic facial index as:
Morphologic facial height (distance between nasionand gnathion)
I
=
ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ
ــــــــــــــ
Bizygomatic width (distance between the zygomapoints)
The face should be examined in the transverse and vertical planes to
determine greater degree of asymmetry than is considered normal. Gross
facial asymmetries may be seen in patients with:
1. Hemifacial hypertrophy / atrophy
ii. Congenital defects.

iii. Unilateral condylar hyperplasia
iv. Unilateral Ankylosis, etc.
Facial Profile
the Angle classification is used and is merely supplemented by stating
whether a deviation is skeletal, dentoalveolar, or both. The skeletal
possibilities are normal, maxillary prognathism, mandibular retrognathism,
maxillary hypoplasia, mandibular prognathism, or any combination of these.
The sagittal cant of the occlusal plane (pitch) is also evaluated. Patients with
severe Class II orthodontic conditions often have steeper occlusal planes
accompanied by longer faces.
The profile is examined from the side by making the patient view at a
distant object, with the FH(Frankfurt plane) plane parallel to the floor.
Clinically or in extraoral photographs, the profile can be obtained by joining
two reference lines:
a. Line joining forehead and soft tissue point A
b. Line joining point A and soft tissue pogonion.
Three types of profiles are seen:
a. Straight or Orthognathic profile : The two lines form an almost
straight line
b. Convex profile :The two lines form an acute anglewith the concavity
facing the tissues. This type of profile is seen in Class II div 1 patients
due to either a protruded maxilla or a retruded mandible.

c. Concave profile: The two lines form an obtuse angle with the
convexity facing the tissues. This type of profile is seen in Class III
patients due to either a protruded mandible or a retruded maxilla.
Convex Straight Concave
Assessment of antero-posterior jaw relationship
A fair picture of the sagittal skeletal relationship can be obtained
clinically by placing the index and middle fingers at the approximate A and
B points after lip retraction. Ideally, the maxilla is 2 to 3 mm anterior to the
mandible in centric occlusion. In skeletal Class II cases, the index finger is
much ahead of the middle finger whereas in Class III the middle fingeris
ahead of the index finger.
Assessment of vertical skeletal relationship
A normal vertical relationship is one where the distance between the
glabella and subnasale is equal to the distance from the subnasale to the
lower border of the chin.By looking at frontal and profile views of the face
and examining how aesthetic mathematical principles of proportions can be
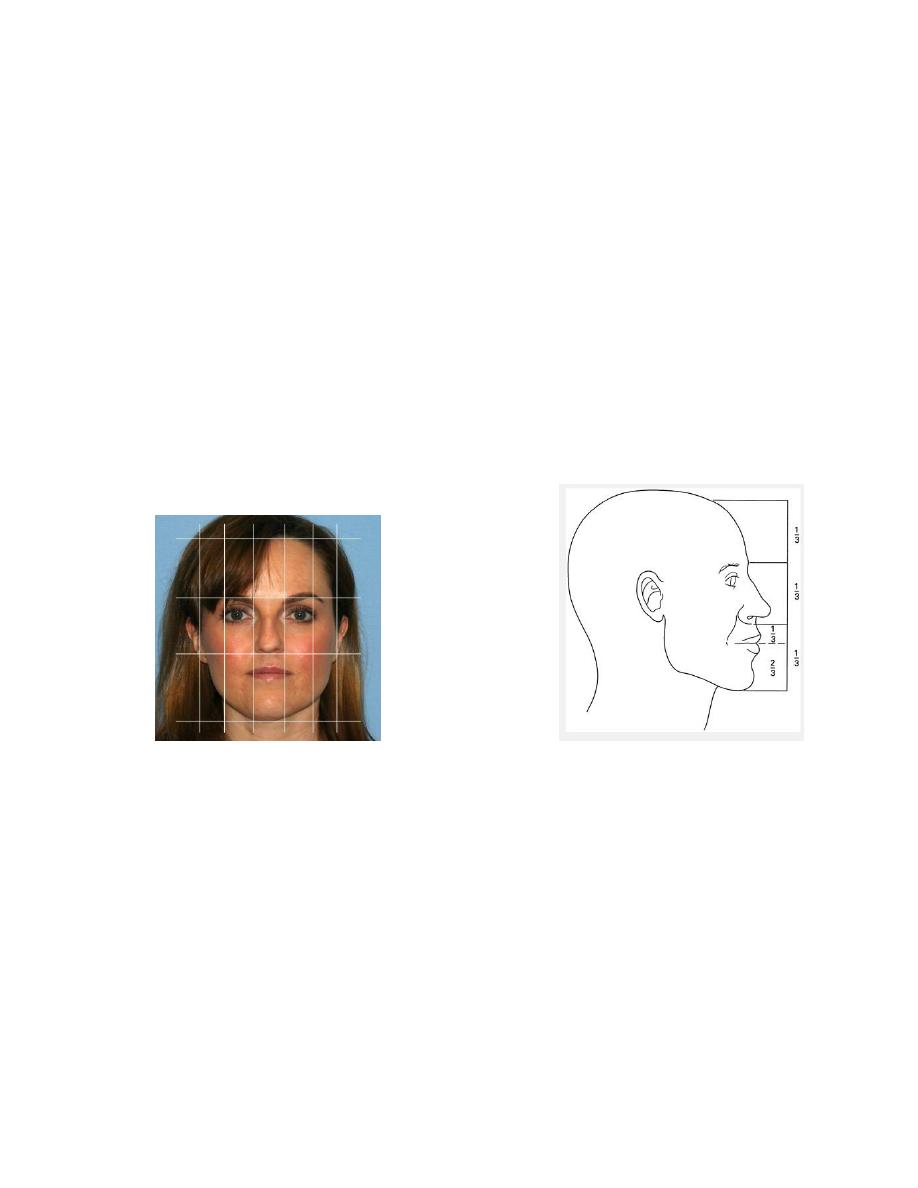
applied. We can observe symmetry by dividing the face vertically into three
thirds, where the nose represents the middle third of the face.
Lower facial third divided into 1/3 upper lip, and 2/3 lower lip
Reduced lower facial height is associated with deep bites while
increased lower facial height is seen in anterior open bites.
The role of fifth
If we divide the face vertically into fifths, we can observe that the
nasal width should be approximately equivalent to the width of each eye.
Examination of the Soft Tissues
Extraoral
1. Forehead The esthetic prognosis of an orthodontic case is determined by
its profile, which in turn is influenced by the shape of the forehead and the
nose. For a face to be harmonious, the height of the forehead (distance from
hairline to glabella) should be as long as the mid-third (glabella-to-
subnasale) and the lower third (subnasale-to-menton), i.e. each of these is

one-third the total face height. Dental bases are more prognathic in cases
with a steep forehead, than with a flat forehead.
2. Nose Size, shape and position of the nose determines the esthetic
appearance of the face and is therefore important in the prognosis of a case.
3. Lips Lip length, width and curvature should be assessed. In a balanced
face, the length of the upper lip measures one-third, the lower lip and chin
two thirds of the lower face height. The upper incisaledge exposure with the
upper lip at rest should be normally 2 mm.
Lips can be classified into:
a. Competent lips: Slight contact of lips when musculature is relaxed.
b. Incompetent lips: Anatomically short lips, which do not contact when
musculature is relaxed. Lip seal is achieved only by active contraction of the
orbicularis oris and mentalis muscles.
c. Potentially competent lips: Lip seal is prevented due to the protruding
maxillary incisors despite normally developed lips
d. Everted lips: These are hypertrophied lips with redundant tissue but weak
muscular tonicity
NASOLABIAL ANGLE
This is the angle formed between a tangent to the lower border of the nose
and a line joining the subnasale with the tip of the upper lip. Normal value is
110 degrees.
Chin
The configuration of the chin is determined not only by the bone structure,
but also by the thickness and tone of the mentalis muscle.

• Mentalis activity : mentalis muscle becomes hyperactive in certain
malocclusions like Class II div 1
Mento-labial sulcus It is the concavity present below the lower lip. Deep
sulcus is seen in Class II cases whereas a shallow sulcus is seen usually in
bimaxillary protrusion
INTRAORAL EXAMINATION
Tongue
Tongue is examined for shape, color and configuration. It may be small,
long on broad. Tongue size can be roughly estimated with the help of a
lateral cephalogram. An excessively large tongue (macroglossia) The lingual
frenum should be examined for tongue tie.Tongue tie can lead to impaired
tongue movements. Abnormalities of the tongue can upset muscle balance
and equilibrium leading to maloclusion.
Lip and Cheek Frena
Among the different frena, the maxillary labial frenum is most commonly
the cause of a malocclusion. A thick, fibrous, low labial frenum , prevents
upper central incisors from approximating each other leading to a midline
diastema. A frenectomyis indicated when the frenum is inserted deeply with
fiber extensions into the interdental papilla.
Gingiva
The gingiva should be examined for the type (thick fibrous or thin fragile),
inflammation and muco-gingival lesions. Gingivitis is a contraindication for

orthodontic treatment. Treatment should be started only when the gingival
condition improves.
Clinical Examination of the Dentition
The dentition is examined for:
1. The dental status, i.e. number of teeth present, un-erupted or missing.
2. Dental and occlusal anomalies should be recorded in detail. Carious teeth
should be treated before beginning orthodontic treatment. Dentition should
be examined for other malformation, hypoplasia, restorations, wear and
discoloration.
3. Assessment of the apical bases.
• Sagittal plane Check whether molar relation is Class I,normal or malO.
• Vertical plane Overjet and overbite are recorded and variations like deep
bite, open bite should be recorded.
• Transverse plane Should be examined for lateral shift and cross-bite.
4. Midline of the face and its coincidence with the dental midline should be
examined.
5. Individual tooth irregularities, e.g. rotations, displacements, fractured
tooth
6. Shape and symmetry of upper and lower arches.
Technological Advances
New methods that have affected current orthodontic practice and have
even greater potential for changing the way orthodontists will practice in the
future include digital photography, videography, 3D photography, computer
imaging, virtual dental models, cone beam computed tomography,
stereolithographic models, and custom milling of attachments and robotic

wire bending. Nonetheless, technological innovations should not be
confused with fundamental changes in orthodontic thinking. It is similar to
when recorded music became digital. The tone of the music improved, but
the tune remained the same. This can be the litmus test for a clinician
considering the adoption of any new technology
Digital Photography, Videography, and Three-dimensional
Photography
The conversion of photography from an analog to a digital process has
revolutionized imaging in all fields, with orthodontics very much the
beneficiary of this stunning technological advance. The ability of digital
video to capture the dynamics of anterior tooth display during speech and
smiling has not yet been fully embraced despite the information that can be
gleaned from this type of record.
Computer Imaging.
The ability to morph images with special computer software and the
creation of algorithms that can simulate the facial outcomes of tooth and jaw
movement provide an excellent treatment planning and communication tool
in orthodontics.
Three-dimensional images created by computed tomography (CT)
have been used in medicine for many years now but were not used in
evaluating orthodontic patients until recently for two reasons: the radiation
dose and the cost.

Virtual Dental Models.
Models of the teeth, the traditional diagnostic record from the beginning of
orthodontics, have been used to view the relationships of the teeth from any
orientation. The advent of digitized laser-scanned dental impressions that
produce a three dimensional image of the teeth has overcome the problem of
having to pour and trim plaster casts and has obviated the need to store and
retrieve the models each time a patient is seen. Now it is possible to view a
virtual dentition on a computer screen by rotating the virtual models to allow
the same type of three-dimensional view as hand-held models. In practices
where 75 to 100 or more patients are seen each day, the task of “pulling
models” becomes an onerous task for the orthodontic staff. Thus, the push
by orthodontists toward the paperless office has represented a real advance
in practice efficiency. As well, in a multi-office practice where patients are
occasionally seen at more than one location, the innovation of using all
digital records has been a real boon. These visual representations can be
measured with at least as great accuracy as plaster models that are measured
with calipers, and it is likely that this technology has not yet matured to its
full potentiality.
Cone Beam Computed Tomography.
Cone beam computed tomography (CBCT) produces three dimensional
volumetric images that can be reliably measured. A major advantage of
CBCT imaging is that all extraneous structures that would otherwise obscure
the desired view can be excluded. This allows visualization of dimensions
for the wanted structures. As a definition : It is an equipment specialized

for maxillofacial imaging to offers a relatively low-dose and convenient
way to follow changes in facial morphology in three dimensions.



