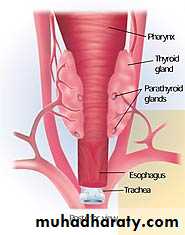
Thyroid gland
Prof.Dr. Alaa JamelFACS. MRCSI C.A.B.S. MBCHBObjective
1-to understand the embryology, anatomy , blood supply and lymphatic drainage.2-to understand the physiology of thyroid gland.
3- to list the tests for thyroid gland estimation.
4-to know congenital anomaly of thyroid .
5- to describe the sign and symptoms of hypothyroidism.
6-to list the causes of hypothyroidism and who we treat.
7-to describe the signs and symptoms of hyperthyroidism and who we diagnose and treated.
8-to define the grav's disease. diagnose and treat it.
9- to know types of thyroid carcinoma .
10 –to know who we can reach the diagnosis of thyroid malignancy and know the main line of treatments.
Embryology
The thyroid gland arise as a diverticulum originating in the foramen caecum which lie at the midline at the junction of ant.2/3 and post.1/3 of the tongue).then descend through thyroglossal duct.
Failure to descend of the thyroid lead to;
ectopic thyroid ,
Lingual thyroid ;
thyroglossal cyst which may cause fistula.
Retrosternium goiter if descend too far.
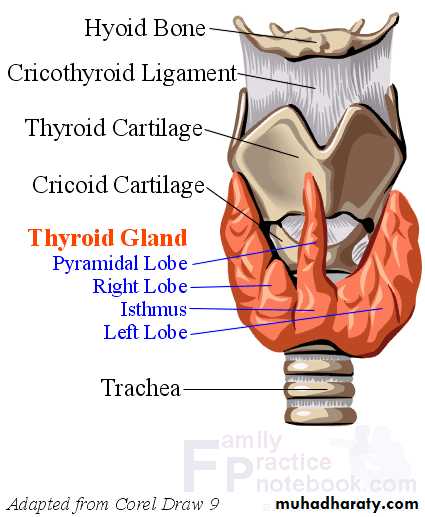
Pyramidal lobe
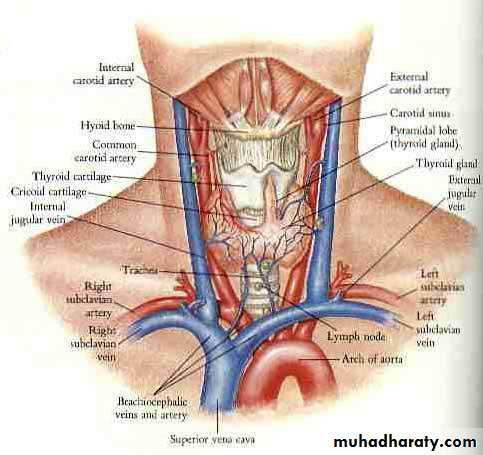
Surgical anatomy
Normal wt of thyroid gland is 20 -25 gm, functional unite is lobule which contain 20 -40 follicles ,
.blood supply from sup and inf thyroid arteries..branches from ??
Venouse return ;
Internal jugular vein
Brachiocephalic vein
Pyramidal Lobe
Normally the thyroglossal duct atrophies, although it may remain as a fibrous band.In about 50% of individuals, (e.g., Graves’ disease, diffuse nodular goiter, or lymphocytic thyroiditis), the pyramidal lobe usually is enlarged and palpable.
Thyroid physiology;
Iodine Metabolism. requirement is 0.1 mg, derived from foods such as fish, milk, and eggs or as additives in bread or salt.In the stomach and jejunum, iodine is rapidly converted to iodide .
The thyroid is the storage site of>90% of the body’s iodine content and accounts for one third of the plasma iodine loss. The remaining plasma iodine is cleared via renal excretion.
The second step in thyroid hormone synthesis involves oxidation of iodide to iodine and iodination of tyrosine residues .
In the euthyroid state, T4 is produced and released entirely by the thyroid gland, whereas only 20% of the total T3 is produced by the thyroid Most of the T3 is produced by peripheral deiodination of T4 in the liver, muscles, kidney, and anterior pituitary,
In conditions such as Graves’ disease, toxic multinodular goiter, or a stimulated thyroid gland, the proportion of T3 released from the thyroid may be dramatically elevated.
Thyroid hormones are transported in serum bound to carrier proteins such as T4-binding globulin, T4-binding
prealbumin, and albumin. Only a small fraction (0.02%) of thyroid hormone (T3 and T4) is free (unbound) and is the physiologically active component.
T3 is the more potent .
, its circulating plasma level is much lower than that of T4.
T3 is less tightly bound to protein in the plasma than T4, and so it enters tissues more readily.
T3 is three to four times more active than T4 per unit weight,
with a half-life of about 1 day, compared to approximately 7 days for T4..
.it also secretes calcitonin from parafolicullar c cells which reduce the level of serum calcium ,so it antagonistic to the parathyroid hormone
Physiological control of secretion
TSH.( secrete from where?)a negative feed back mechanism .
and under influence of TRH which secreted from hypothalamus
Lingual thyroid
Failure of thyroid gland to descend and it remain as a lump in the foramen of caecum of the tongue .may be the only thyroid tissue present.Complication obstructive symptoms such as;
choking,
dysphagia,
airway obstruction,
hemorrhage.
hypothyroidism.
Medical treatment options include administration of exogenous thyroid hormone to suppress thyroid- stimulating hormone (TSH) .
radioactive iodine (RAI) ablation followed by hormone replacement.
Surgical excision is rarely needed.
Ectopic Thyroid
esophagus,
trachea, .
anterior mediastinum.
Thyroid tissue has been observed adjacent to the aortic arch, in the aortopulmonary window,
within the upper pericardium, .
in the interventricular septum.
Thyroglossal duct cysts
are the most commonly encountered congenital cervical anomalies.During the fifth week of gestation, the thyroglossal duct lumen starts to obliterate.
the duct disappears by the eighth week of gestation.
They are usually asymptomatic but occasionally become infected by oral bacteria and cause abscess why?.
May get papillary carcinoma why?,
Treatment involves the “Sistrunk operation,” which consists of en bloc cystectomy and excision of the central hyoid bone to minimize recurrence.
Thyroglossal cyst
.its diagnosed by characteristic clinical signsa- it move up word when the patients protrude the tongue because it attached to the tract of the thyroid descent
b- it move on swallowing because its attached to the larynx by the pretracheal fascia
Location of cyst
a- beneath foramen caecum .b- in the Foor of the mouth.
c- suprahyoid 24%.
d- subhyoid 65% .
e- on the level of thyroid cartilage f- on the level of cricoids cartilage
thyroglossal fistula
this present as an opening on to the skin in the line of the thyroid descend in the midline of the neck. it may discharge thin .fluid .and attack of infection can occur.
Its never congenital ,its acquired due to infected thyroglossal cyst or incomplete resection of the tract
Treatment
complete excision of the fistula with the body of hyoid bone and dissection is continued up to the region of foramen caecum of the tongue. name of operation(sistrunk’s operation)
Pathology of goiter
The term goiter is used to describe any enlargement of the thyroid gland irrespective of the underling pathology.
Tests of thyroid function
1- serum T.F.T
a- serum TSH
b-T4 and T3
2- isotope scanning I 123
3-thyroid antibodies4- thyroid US and or CT scan
5 - FNAC
5- FNAC;
Fine-needle aspiration biopsy of the thyroid gland is safe, inexpensive, minimally invasive, and highly accurate in the diagnosis of nodular thyroid disease.
Four cytological diagnostic categories are used. benign,
suspicious,
malignant,; .
non diagnostic,.
Limitations of fine-needle aspiration are related to the skill of the aspirator, the expertise of the cytologist, and the difficulty in distinguishing some benign follicular adenomas from their malignant .
The recommend fine needle aspiration biopsy of the thyroid in the following situations:
To make a diagnosis of a thyroid nodule;To help select therapy for a thyroid nodule;
To drain a cyst that may be causing pain; or
To inject a medication to shrink a recurrent cyst.
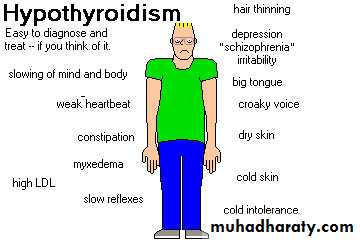
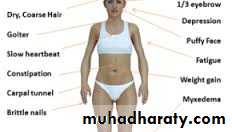
HYPOTHYRODISM
Causes of hypothyroidismPrimary (Increased TSH Levels) Secondary (Decreased TSH Levels)
Post thyroidectomy
Subacute thyroiditis
Medications: antithyroid drugs, lithium
Rare: iodine deficiency, dyshormogenesis
Secondary (Decreased TSH Levels) Pituitary resection or ablation, Pituitary tumor.
Tertiary Hypothalamic insufficiency Resistance to thyroid hormone
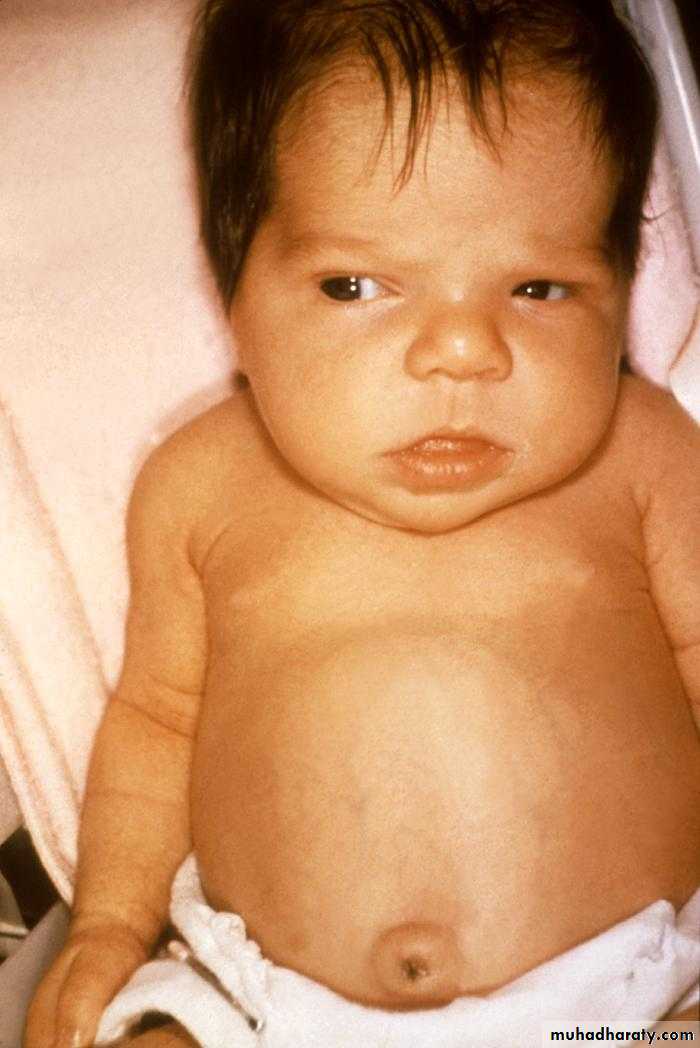
(congenital hypothyroidism(cretinism
( cretinism are characteristic facies similar to those of children with Down syndrome and dwarfism) .
hypothyroidism
1- congenital hypothyroidism(cretinism);its due to complete or near complete failure of thyroid development (partial failure cause juvenile myxedema) .in endemic areas due to maternal and fetal iodine deficiency .
immediate diagnosis and treatment is important why?.
IT occur in 1/4000 live birth .
women under anti thyroid treatment may give birth with hypothyroidism.
clinical featue of The infant is stunted, and mentally defective ,puffy lips large tongue and protruded abdomen ,umbilical hernia.
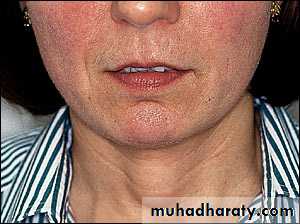
2- adult hypothyroidism (myxoedema)usually affect women and most often occur in the middle aged or elderly.
Signs of thyroid deffeciency ;
brady cardia,
cold extremities,
dry skin and hair ,
preorbital buffness ,
hoarse voice ,
slow movements .
delay relaxation phase of ankle jerks..
Symptoms
tiredness,
mental lethargy,
cold intolerance,
weight gain,
constipation,
menstrual disturbance ,
carpal tunnel syndrome why?
Delayed relaxation of ankle jerk reflex is the most useful clinical sign in making the diagnosis
Cardiovascular changes in hypothyroidism
include ;bradycardia,
cardiomegaly,
pericardial effusion,
reduced cardiac output, .
صور الى signs
Laboratory Findings
Hypothyroidism is characterized by ;low circulating levels of T4 and T3.
Raised TSH levels are found in primary thyroid failure,
whereas secondary hypothyroidism is characterized by low TSH levels that do not increase following TRH stimulation.
Thyroid autoantibodies are highest in patients with autoimmune disease (Hashimoto’s thyroiditis.
and may also be elevated in patients with nodular goiter .
and thyroid neoplasms.
An electrocardiogram demonstrates decreased voltage with flattening or inversion of T wave
Treatment
T4 is the treatment of choicedosages varying from 50 to 200 μg per day, depending on the patient’s size and condition.
Starting doses of 100 μg of T4 daily are well tolerated; however, elderly patients and those with coexisting heart disease and profound hypothyroidism should be started on a considerably lower dose such as 25 to 50 μg daily.
The dose can be slowly increased over weeks to months to attain a euthyroid state.
T4 dosage is titrated against clinical response and TSH levels, which should return to normal
Thyroid enlargement
Normal thyroid gland is impalpable
Classification of thyroid swellingSimple goiter; diffuse hyperplastic (physiological, pubertal, pregnancy)or multinodular goiter
Toxic goiter; diffuse (graves" ds) ,multinodular goitre ,toxic adenoma
Neoplastic ;benign ,malignant
Inflammatory; autoimmune(hashematose ds),granulomotous(De Quervain"s thyroditis), fibrosing (redel"s thyroiditis),infective (acute or chronic)
Others (amyloid)
Simple goiter;
Causes
Due to excessive stimulation of gland cells by TSH
increase its level either due to
excessive secretion of hormone by microadenoma in ant. Pituitary gland (rare) or
due to chronic low level of thyroid hormone .
Low level of TSH due to dietary iodine deficiency (daily requirement of iodine 0.1-0.15 mg) or due to increase demand on thyroid hormone as in puberty or pregnancy
Diffuse hyperplastic goitre
In this condition the gland soft, diffuse, and may become large enough to cause discomfort .colloid goiter isolate stage of diffuse hyperplasia when the follicle become filled with colloid
Simple Nodular goitre
It’s a complication of long standing simple diffuse hyper plastic goitre ,usually only one macroscopic nodule is found but microscopic changes will be present through out the gland.
Complication
1-Treacheal obstruction due to . gross lateral displacement .compression in a lateral or anterior posterior plane .retro sternal extension of the goiter.2-secondary thyrotoxicosis
3- carcinoma
Increase incidence of follicular carcinoma so rapidly growing nodule in long standing goiter should always be subjected to aspiration cytology.
In endemic cases when deficiency of diet iodine goitre can be reduced it by add iodized salt or in physiological increase demand on thyroid hormone can be regress goiter by thyroxin in dose 0.15-o.2mg daily for few mounts.
Multinodular goiter is irreversible
Most of multinodular goiter is asymptomatic and not need operation,
indication for operation are
1-for cosmetic
2- for pressure symptoms
3- patient want
4- retro sternum goiter
Type of surgery ;
1-total thyroidectomy with thyroxin replacement long life2- near total thyroidectomy -- total lobectomy + subtotal lobectomy + isthmstectomy
2-subtotal thyroidectomy 8 mg from each lobe
3- lobectomy lobectomy + isthmstectomy
Selection of types of operation dpend on
1- diagnosis
2- risk of thyroid failure
3- risk of RLN injury
4- risk of recurrence
5_ graves ds
6- multinodular goiter
7- thyroid cancer
8- risk of hypoparathyrodism
Clinically discrete swelling
Discrete swelling in impalpable gland is called isolated or solitary while prominent swelling in generalized abnormal gland is called dominant swelling ..The importance of discrete swelling is risk of neoplasia about 15% are malignant and 30-40% are follicular adenoma
Investigation
1- tft 2- antibody titer (the presence of circulating AB may increase the risk of thyroid failure after lobectomy} ,3- isotope scanning I123 (hot, worm, cold) 4- US 5- FNAC( cannot distinguish between benign follicular adenoma and follicular carcinoma because is depend on histological criteria which include capsule and vascular invasion).
6- radiology chest and thoracic innless to detect tracheal deviation or compression and retrosternal goiter
7- indirect laryngoscopy preoperatively why??
8- trucut biopsy high diagnostic accuracy but poor patient compliance and have more complication so not routinely used.
Thyroid cyst
30% of clinically isolated swelling contain fluid (cyst) or party cystic .sudden painfull cystic swelling indicate bleedind in to the cyst which resolve over period of wks if untreated ,about 50% of cystic swelling are the result of colloid degeneration or uncertain eitiology .
Indication of operation in isolated or dominant cyst are
1- suspected of neoplasm 2- toxic adenoma
3- pressure symptoms 4- cosmetic 5- patients wishes
.
Retrosternal goiter
Most of retrosternal goiter arise from lower lobe of thyroid gland rarely arise from ectopic thyroid tissue ,it may descend to the sup. Mediastinum if short neck and strong neck muscle as in male.C.F
It may be symptom less and discovered on routine CXR , and it may be cause symptoms as ;
Dyspnea ,dysphagia, Obstruction of venous return at the thoracic inlet from a substernal goiter results in a positive Pemberton’s sign—facial flushing and dilatation of cervical veins upon raising the arms above the headRecurrent nerve paralysis ( rare)
Treatment
In obstructive symptoms and associated with thyrotoxicosis usually not treated with anti thyroid drug or radioiodine because it may cause enlarge of goiter.
Surgical operation through neck incision rarely need sternatomy
Thyrotoxicosis
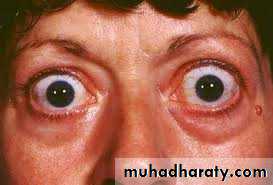
The clinical manifestations DUE TTO increase thyroid H.. It is important to distinguish disorders such as Graves’ disease and toxic nodular goiters that result from increased production of thyroid hormone from those disorders that lead to a release of stored hormone from injury to the thyroid gland (thyroiditis) or from other non thyroid gland–related conditions. The former disorders lead to an increase in RAI uptake (RAIU), whereas the latter group is characterized by low RAIU..Clinical type
1- difuse toxic goiter- Graves ds mostly occur in women called 1* thyrotoxicosis associated with eye signs 50% of cases has family history of autoimmune endocrine ds . its due to abnormal thyroid stimulating antibodies that bind to TSH receptors site and produced prolong effect
It is an autoimmune disease with a strong familial predisposition, female preponderance (5:1), and peak incidence between the ages of 40 and 60 years. Graves’ disease is characterized by thyrotoxicosis, diffuse goiter, and extrathyroidal conditions including ophthalmopathy, dermopathy (pretibial myxedema), thyroid acropachy, gynecomastia, andother manifestations
It is characterized by deposition of glycosaminoglycans, leading to thickened skin in the pretibial region and dorsum of the foot .
Diagnostic Tests.
The diagnosis of hyperthyroidism is made by a suppressed TSH with or without an elevated free T4 or T3 level. If eye signs are present, other tests are generally notneeded.However, in the absence of eye findings, an I123 uptake and scan should be performed. An elevated uptake, with a diffusely enlarged gland, confirms the diagnosis of Graves’ disease and helps to differentiate it from other causes of hyperthyroidism.
Treatment of thyrotoxicosis
1-Antithyroid medications generally are administered in preparation for RAI ablation or surgery.The drugs commonly used are propylthiouracil (PTU, 100 to 300 mg three times daily) and methimazole (10 to 30 mg three times daily, then once daily).
actions of drugs
PTU …inhibit ..conversion of t4 to t3
cross the placenta …PTUeter in breast feeding and pregnancy
Side effects
of treatment include reversible granulocytopenia, skin rashes, fever, peripheral neuritis, polyarteritis, vasculitis, hepatitis, and, rarely, agranulocytosis and aplastic anemia. The dose of antithyroid medication is titrated as needed in accordance with TSH and T4 levels
Most patients have improved symptoms in 2 weeks and become euthyroid in about6 weeks. Treatment with antithyroid medications is associated with a high relapse rate when these drugs are discontinued, with40% to 80% of patients developing recurrent disease after a 1- to 2 year course.
β-Blockade should be considered in all patients with symptomatic thyrotoxicosis and is recommended for elderly patients
, those with coexistent cardiac disease, and patients with resting heart rates >90 bpm. These drugs have the added effect of decreasing the peripheral conversion of T4 to T3.
Propranolol is the most commonly prescribed medication in doses of about 20 to40 mg four times
Daily
Calcium channel blockers IN ASTHMA
2-radioactive iodine 131 …medication till euthyroid then discontinue to peak gland up take I131
3- iodides may reduce the vascularity of the thyroid
4-Surgical treatment
2- toxic nodular goiter—due to prolong standing of simple nodular goiter her called 2* thyrotoxicosis rarely associated with eye signs .
3- toxic nodule solitary overactive nodule which may be part of generalized nodularity or a true toxic adenoma ,the normal thyroid tissue surrounding the nodule is suppressed and in active
4- hyperthyroidism due to rare cases as in neonatal thyrotoxicosis and 2*carcinoma
Symptoms ---
Tiredness, heat intolerance ,wt loss, increase appetite, palpitationSigns----
Tachycardia, hot moist palm, exophthalmos, lid lag/led retraction agitation, goiter &bruit
What are the different between 1* and 2* thyrotoxicosis? In 1*
Goiter diffuse and vascular ,the onset is abrupt, hyperthyroidism is more sever, eye signs is sever but cardiac failure is rare
Cardiac rhythm
Fast heart rate which persist during sleep its characteristic of thyrotoxicosis.
Stages of development of thyrotoxic arrythemia are
1- multiple extra systol 2- paroxysmal tachycardia 3- paroxysmal AF 4- persistence AFEye signs
1- exophthalmos which may be unilateral .defined exophthalmos ? 2- lid lag and lid retraction ( levetor palpebrae superioris partly inervated by sympathetic fibers)
3- ophthalmoplagia and diplopia (double vision ) 4- papilledema
5- ecchymosis
Surgical treatment
Advantage goiter removed, cure is rapid, cure rate is highDisadvantage recurrence of thyrotoxicosis occur in 5%
Intra and post operative complication
Radioiodine
Its destroyed thyroid cells ---advantage no surgery & no prolonged drug therapy
Dis advantage
The rate and timing of late thyroid failure are influenced by the dose selected ,the higher dose is likely to cause thyroid failure within 6 months
Choice of therapy
Diffuse toxic goiter if pt over 45 radioiodine is appropriate
If under 45 years surgery for the large goiter
and anti thyroid drug and iodine in small goiter,
Toxic nodular goiter
Should be treated surgically
Toxic nodule
Surgery or radioiodine which benefit if age more 45 years
Recurrent thyrotoxicosis after surgery
Radioiodine is treatment of choice, but in young women who want children can use anti thyroid drugs
Failure treatment with anti thyroid or radioiodine can treat surgically
Surgery to thyrotoxicosis
Preoperative preparation
1- carbemazol 10mg x3 till euthyroid condition 8-12 wks then maintenance dose 5mg x3
2- B blocker agents which act on target organs and not on the gland itself Inderal 40 mg x3 which also inhibit conversion of t4 to t3. Or use nadalol 160 mg x1 .this drug not affect on hormone secretion so thyroid hormone still high during and after operation so must continue with B blocker 7 post operative days.
Thyroid surgery
Preoperative investigation
Technique
Post operative complication
*haemorrhge ;its due to slip ligature of sup. thyroid artery or from remnant of thyroid tissue or from thyroid vein it may cause tension hematoma and respiratory distress
* respiratory obstruction mostly due to laryngeal edema which due to;
tension haematoma, surgical manibulation, trauma to the larynx by anesthetic intubation
*unilateral or bilateral recurrent nerve paralysis ;this may be unilateral or bilateral .transit or permanent ,transit occur in 3% recover in 3 wks to 3 months
* thyroid insufficiency usually occur within 2 wks
.
parathyroid insufficiency due to either removal of prathgland or infarction due to damage to parathyroid end artery
(what means end artery give me example?)
*thyrotoxic crisis ;its acute exacerbation of hyperthyroidism
*wound infection
* hypertrophic or keloid scar
*stitch granuloma
About 25 % of patients develop transient hypocalcaemia and if associated symptoms are sever we give i.v ca gluconate or oral ca. may be necessary .the serum ca should be measured at first attendance 4-6 wk after operation.
thyroid Storm
It’s a condition of hyperthyroidism accompanied by fever, central nervous system agitation or depression, and cardiovascular and GI dysfunction, including hepatic failure
. The condition may be precipitated by abrupt cessation of antithyroid medications, infection, thyroid or nonthyroid surgery, and trauma in patients with untreated thyrotoxicosis..
β-Blockers are given to reduce peripheral T4 to T3 conversion and decrease the hyperthyroid symptoms.
Oxygen supplementation
hemodynamic support should be instituted.
Nonaspirin compounds can be used to treat pyrexia, Lugol’s iodine
. PTU therapy blocks the formation of new thyroid hormone and reduces peripheral conversion of T4 to T3. Corticosteroids often are helpful to prevent adrenal exhaustion and block hepatic thyroid hormone conversion
Neoplasm
Benignfollicular adenoma which present as clinically solitary nodule which distinguish from follicular carcinoma only by histological examination
Malignant Neoplasm
1-,papillary carcinoma accounts for 80% of all thyroid malignancies in iodine-sufficient areas and is the.Distant metastases are uncommon at initial presentation, but may ultimately develop in up to 20% of patients. The most common sites are lungs, followed by bone, liver, and brain.
Psammoma bodies, which are microscopic, calcified deposits representing clumps of sloughed cells, also may be present. Multifocality is common in papillary carcinoma and may be present in up to 85% of cases on microscopic examination. Multifocality is associated with an increased risk of cervical nodal metastases
Lateral aberrant thyroid” almost always denotes a cervical lymph node that has been invaded by metastatic cancer
occult/microcarcinoma refers to tumors of 1 cm or less in size with no evidence of local invasiveness through the thyroid capsule or angioinvasion, and that are not associated with lymph node metastases.
Treated by total thyrodectomy + post operative radioiodine.e
Neoplasm
2- Follicular carcinomas account for 10% of thyroid cancers and occur more commonly in iodine-deficient areas. and a mean age at presentation of 50 years old. Follicular cancers usually present as solitary thyroid nodules, occasionally with a history of rapid size increase, and long-standing goiter.. Unlike papillary cancers, cervical lymphadenopathy is uncommon at initial presentation
Hürthle Cell Carcinoma
It’s account for approximately 3% of all thyroid malignancies andconsidered to be subtype of follicular thyroid cancer
It’s characterized by vascular or capsular invasion and, therefore,
cannot be diagnosed by FNAB., it derivedfrom the oxyphilic cells of the thyroid gland
. Hurthle cell
tumors differ from follicular carcinomas in that
They are more often multifocal and bilateral (about 30%),
usually do not take
up RAI (about 5%), are more likely to metastasize to local nodes
(25%) and distant sites, and are associated with a higher mortality
rate (about 20% at 10 years). Hence, they are considered to
be a separate class of tumors by some groups.
3-, anaplastic carcinoma 10% occur in elderly ,highly malignant tumour ,rapid local spread, with local invasion with early metastasis to l.n and blood stream. treatment by surgery if possible ,pailative compined chemotherapy and external beam radiation . avoid tracheostomy because tumor invade the tracheostomy site.
4-, medullary carcinoma 5% MTC accounts for about 5% of thyroid malignancies and arises from the parafollicular or C cells of the thyroC cells secrete calcitonin, a 32-amino-acid polypeptide that functions to lower serum calcium levels, Most MTCs occur sporadically. However, approximately25% occur within the spectrum of several inherited syndromes such as familial MTC, MEN2A, and MEN2B
5-lymphoma account for <1% of thyroid malignancies, and most are of the non-Hodgkin’s B-cell type.
2*either metastasis or direct invasion
Etiology of malignant tumor
Most important is irradiation of thyroid under age of 5 years mainly cause papillary carcinomaIn endemic goiter area more common follicular type
Malignant lymphoma some time develop in auto immune thyroiditis
Staging of thyroid tumor
According to T.N.M
T= TUMOUR T0 –no evidence of 1* tumor T1-1CM OR LESS T2-1-4 CM LIMITED TO THYROID T3--> 4CM LIMITED TO THYROID T4-any size extend beyond capsule
N=NODES N0-- no regional nod metastasis N1—reginoal node metastasis
M=METASTASIS M0—no metastasis M1—metastasis present
Thyroditis
Its common condition usually associated with increase thyroid ab ,there may be family history of other autoimmune disease ,commonly present with goiter which may be nodular ,onset may be insidious or sudden and painful ,
Diagnosis depend mainly on rise one or more of thyroid A.B which present in 85% of cases ,fnac very useful
Treatment
Full replacement of thyroxin in case of hypothyroidism and in large goiter thyroidectomy may need .
Parathyroid gland;
Anatomy; normal glands are khaki colored –soft usually oval shape , about 6 mm in length,30- 50 mg ,. most individual have 4 glands but about 10% have more and few population have fewer than 4 glands.
Positions ; variable , sup. Glands located at the junction of inf thyroid art and r.l.n usually post to the nerve and sup. To the art. While inf. Glands usually located ant to the r.l.n.
صوره للغده
Blood supply; inf. Thyroid art.
Ectopic gland may received blood from arteries supply pharnex and oesophagus.Embryology ; sup. Glands develops from endodermal cellular proliferation , while inf. Develops from the thymus from 3rd pharangeal pouch.
Function of the gland;
It secrete parathyroid hormones it’s a peptide 84 amino acid which control the level of calcium in the blood and extracellular fluid.It increase level of calcium by ; a- in kidney ; stimulate calcium re absorption and inhibit phosphate re absorption and stimulate the synthesis of vitamin D.
In bone ; it stimulate resorption by increase osteoclast activity and stimulate osteoplast activity.
A rise in serum calcium cause a reduction in circulating pth level.
Parathyroid Physiology and Calcium Homeostasis
Extracellular calcium levels are10,000-fold higher than intracellular levels,
Extracellular calcium is important for excitation contraction coupling in muscle tissues, synaptic transmission in the nervous system, coagulation, and secretion of other hormones.
Primary hyperparathyroidism;
Its sporadic or familial disorder associated with hypercalciemia . due to elevated or inappropriately raised P.T.H level with enlargement of parthyroid gland. So in this type of hyperparath. Both increase calcium and parath. H.If it familial it associated with 1- men type 1.(multiple endocrine neoplasia, vermer's syndrome)it autosomal dominant disorder ,clinical feature include hyperparathyroidism at least 90%, benign pituitary adenoma 40%which may be functioning or not., multiple pancreaticoduodenal neuroendocrine tumour 50% as gasterinoma or insulinoma.
• .
2- multiple endocrine neoplasm type 2 (men-2) in which hyper parathy. Occur in 25%3- familial isolated hyperparathyroidism. It a rare autosomal dominant ds associated with increase risk of parathyroid carcinoma in 20%.
Pathology;
In pt with sporadic primary hyperparathyroidism finding include ; adenoma 85%. Hyperplasia 14% and carcinoma 1%;Hyper functioning gland usually brown in color and enlarge.
Parathyroid carcinoma usually a large tumors , grey white in appearance and adherent to adjacent tissues.
Microscopically appears of ca. a thickened capsule, fibrous band and nodule and capsular and vascular invasion.
;
d.d of primary hyperparathyroidism;
1- hypercalcimia of malignancy mediated by parathyroid hormone –related peptid. Or associated with bone metastasis.2- familial hypocalciuric hypercalcimia ----- autosomal dominant
3- neonatal hyperparathyroidism;
Treatments;
Surgical indication;
1-pt less than 50 years old
2- history of urinary tract calculi
3- bone disease with markedly reduced bone density
4- serum calcium level greater than 2.85
mmol/l-1
5- sever symptoms
COMPLICATION OF PARATHYROID SURGERY;
1-failure to achieve biochemical cure 5%2- R.L.N. injury 1%
3- postoperative haemorrage 1%
4-perminint hypoparathyrodism
5- recurrent hyperparathyroidism
in the immediate preoperative phase surgeon can give the pt methelen blue 5 mg kg body wt in 500 ml of dextrose- saline to visualize parathyroid tissue.
secondary hyperparathyroidism;
this is occur in chronic renal failure why ? hypocalcaemia and phosphate retention cause continuous stimulation of parath. gland and cause parathyr. hyperplasia .tertiary hyperparathy.
occur after renal transplant;
hypoparathyrdism
congental;
*digeorge's syndrome ( absent parthy. gland
*auto immune poly glandular syndrome type 1
acquired;
post operative
haemochromatosis (Wilsons disease)
symtoms and signS
it cause hypocalcaemia what are the symptoms of hypocalcaemia ? peripheral numbness, tingling, parasthesia of the fingers and toes, in sever case ventricular arrhythmia , laryngeal spasm and grand mal fitcan see 3 signs
- Chvosteck's sign2- carbopedal spasm
3- ecg finding prolong QT interval and qrs complex changes.