ORAL MEDICINE
Definition:Is that part of dentistry which is involved in the diagnosis and treatment of the oral diseases of a non-surgical in nature which may be localized to the mouth or which may be an oral manifestation of systemic diseases .
OR
It is an art and science of recognition and treatment of various oral lesions .
ORAL DIAGNOSIS :
It is a systematic method of identification of oral lesions.
Diagnostic process or sequence or procedure .
can be divided into the following parts
1-Taking and recording the patient`s history
2-Examination of the patient(physical examination and laboratory studies )
3-Evaluation of the history and results of physical examination and laboratories studies leading to formulating of a diagnosis .
4-Treatment planning recommendation .
Taking and recording the patient`s history:
components of patient history
A- Routine data or identification data
which include the patient`s name .telephone number , sex , address , age and race
B- Chief complaints
recorded by the patient`s own words . it is usually the reason for the patient visits . The CC is subjective in nature and is related to an uncomfortable abnormal sensation . The most successful treatment is achieved if the CC is managed and corrected properly.
C- History of present illness
Is a chronologic account of the CC and associated symptom from the time of onset to the time of history's taken (onset , course ,duration , severity , promoting factors and relieving factors ).
D-Past and present medical history
it is very important for the following reasons
*1. Identification of systemic diseases that could require modification of dental treatment.
*2. Identification of systemic diseases that pose a threat to the dental personnel or others patients.
*3. Identification of drugs that could result in adverse interaction with drugs or treatment administrated by the dentist .
*4. Establishment of good patient –dentist rapport .
*5. Facilitation of effective communication with patient physician.
*6. Provision of medico legal protection for the dental staff.
Past and present medical history is composed of the following subdivision :
1-Previous illness(heart attack ,stroke ,hypertension ,congestive heart failure ,bleeding disorder and diabetic )
2- Childhood diseases
which include any childhood diseases that produce fever may causes enamel defect if it occur during enamel formation. Rheumatic fever may causes damage of the heart valve ,making the prevention of infective endocarditis an important consideration when planning treatment .
3-Hospitalization ;
may indicate past disease and how it was treated .A patient who has had radiation therapy to the head and neck may develop osteo- radionecrosis if not managed properly even many years after treatment .
4-Allergies.
5-Medication ;
The patient should be questioned concerning any medication he or she has been taken in the last six months .It is important to note if the medication is still being taken along with the reason for its prescription .
6-Review of system ;
is that part of the patients medical history covering each major system of the body, concentrate on the signs and symptoms of disorders .* C.V.A : some sign and symptom of C.V.A disease include( prolonged elevated high blood pressure ,chest pain ,ankle edema ,heart murmur and shortness of breath). These finding could be due to( angina pectoris ,MI, coronary artery insufficiency or congestive heart failure ).
*Respiratory system; Symptoms associated with respiratory disorders (shortness of breath[ dyspnea] , cough , hoarseness) may be an indication of ( CV problem , asthma ,emphysema or lung tumor ) .
* C.N.S ; Patient with a history of (convulsion ,pain , parasthesia, paralysis or syncope ) may have a nervous system disorders .
* G.I.T ; Include (nausea ,vomiting, diarrhea ,constipation ,loss of appetite or abdominal pain ).
* Genito-urinary system ; Symptoms associated with these system are (mensturation ,pain during urination , frequency of urination , blood or pus in urine ) . Some oral conditions associated with symptoms of this system like (steven –Johnson syndrome , behcet`s syndrome and Reiter's syndrome ) .
* Muscular –skeletal system ; Symptom associated with this system include (muscle or joint pain , loss of joint function , muscle weakness or multiple bone fracture ).These symptoms may be associated with normal muscular fatigue from exertion or indicative of more serious problem .
* Endocrine system .
* Disorder of the skin ,hair and nail .
* Vital signs .which include (blood pressure , pulse rate ,respiratory rate ,temperature height and weight )
E- Past dental history ;
It is important to know what had been done in the outcome of previous treatment. Restoration , prosthodontics ,orthodontics , endodontic periodontics and complication of anesthesia . Also any difficulties with dental care and recent dental radiography .
F- Family history ;
should include
* The health of the patient`s parents and siblings .
*The cause of the death of relative may be an important clue to the presence of an inherited disorder .
*The record of an illness with hereditary familial tendency such as (hypertension , hemophilia ,diabetes , allergies , some form of cancer , magrain and psychiatric neurogenic disorder ) . *Should be used to discover communicable diseases that may infect members of that household (TB, hepatitis ) .
G-Social history ;
Which include
* Marital state ,number of children , habits .
* Education and job- information [ occupation ] .
* Drinking of alcohol , smoking and drug taken as caffeine and heroin .
EXANINATION OF THE PATIENT
Outlines for clinical examination1-Principles
2-General
3-Oral
Principle:
A number of examination techniques are helpful in evaluating a patient , an organ and a tissue . The basic examination techniques are
1-Visual inspection :
Is a systematic observation of the patient . It begins at the first visit with the patient . Adequate lighting is necessary to perform an examination well and by using the dental mirror to reflect light into dark area of the mouth . The structures to be inspected it must not be covered by clothing , cosmetic ,saliva , plaque and other debris .Additionally eye glass , removable partial denture , complete denture , obturator and other appliance must be removed . Some structures may require displacement in order to adequately inspect them , displace the tongue to examine the floor of mouth and retract the eyelid to examine the conjunctiva . By visual inspection we can see any change in the morphology such as size , shape , symmetry , deformity , swelling and abnormal muscle development .
2-Palpation :
Is a procedure wherein the examiner feels or presses upon the structures being examined .Palpation give information about ; texture ,dimension , consistency , temperature and function events.
*Texture ; is best determined through light palpation with finger tips . The texture of surface or mass may be (smooth ,rough or pebbly {lobulated } ).
* Dimension ; cannot always be assessed by the eye alone , some nodules may have very little dimension in terms of depth .
*Consistency ; it is described usually in term of compressibility , so the mass may described as (soft , rubbery or indurated {hard} ).
Both consistency and dimension can be evaluated by pressing the object against unyield structures that deeper or lateral to the object being palpated .
Types of palpation :
1-Bidigital palpation ;
Consistency may be evaluated by pressing the structure with examiner thumb and index figure , e.g. in the evaluation of the nodules in the lips or buccal mucosa and helix of the ear .
2-Bimanual palpation ;
Manipulation of structure with the fingers of one hand and thump of other hand .e.g. palpation of the submandibular salivary gland with the index of one hand in the floor of mouth and the finger of the other hand pressing against the skin of the submandibular area .
* Temperature ; Are best evaluated by using the dorsal or extensor surface of the finger since the skin here is thin and well innervated . e.g. inflamed area or soft tissue overlying vascular lesion may be warmer owing to increased blood flow to the area .
*Functional event ; any movement that can be detected with palpating hand . e.g. the pulsatility or thrill of a vascular lesion and movement of the tooth in its socket .
3- Probing :
Is palpation with an instrument and is one of the most important diagnostic technique used in dentistry .The teeth are probed for caries with explorer . Periodontal probe is used to measure the depth of the periodontal sulcus . Lacrimal duct probe are used in the examination of Wharton`s duct of the submandibular duct and stensen`s duct of the parotid gland . Fistula can be probed by gutta-percha to determine the origin of the fistula .4-Percussion :
Is the technique of striking the tissue with the fingers or an instrument . The examiner listen to the resulting sound and observes the response of the patient . Percussion is often used to detect tenderness in the frontal and maxillary sinuses by taping the fingertip against a finger placed over the sinus . Intraoral percussion is used as a method to evaluate the teeth , usually its accomplished by taping the teeth with a mirror handle .This technique may induce pain in area of inflammation from periodontal diseases or pulpitis .5-Auscultation :
Is the act of listening for sounds within the body . The stethoscope is a useful aid to auscultation . The examiner may listen for sound such as wheezing, popping of the T.M.J or clicking . The flat diaphragm is used to detect high frequency sound , whereas the bell collect low-pitched sounds .
6-Aspiration :
Is withdrawal of fluids from a body cavity . The area being aspirated may be limited to soft tissue or may be central in bone .The aspiration is the material that is withdrawn , when nothing can be withdrawn the needle tip should remove to adjacent area . In solid lesion such as neoplasm with minimal vascular content , nothing may be aspirated . Traumatic bony cyst have no aspirate or only small blood –tinted fluid . Aspiration of pus indicate an inflammatory process . If several milliters of blood are aspirated easily indicate a vascular lesion such as hemangioma . Straw colored or blood tinted fluid may indicate a cyst . The aspiration may be used for culture and sensitivity test to identify the pathogen and its best treatment .
7-Diascopy :
Is a specific examination technique whereby the tissue being examined is compressed by a glass slid . The primary objective of the test is to determine whether a reddish or bluish- purple lesion is vascular in nature or due other cause .Vascular lesion such as varies, telangictasia and hemangioma are blanched upon diascopy . If the area dose not blanched it may be due to other causes such as (amalgam tattoo, ink tattoo , nevi ,localized pigmentation and extravasated blood {petechial ,ecchymosis and hematoma} )
8-Evaluation of function :
There are several function that need to be assessed in examination of the head and neck .
*Tear production and tear drainage , by shirmer tear test.
*The function of the salivary glands , can be assessed by palpating or milking the glands.
*Taste; the tongue is the organ of the taste and its function can be assessed with the use of saturated salt solution , quinine and fructose or other sugars.
*Mastication ; can be evaluated by masticatory symptoms like (limited jaw opening ,inability to move the jaw ,pain , difficulty with swallowing and pain with chewing ).
*Neurologic function ; A number of conditions involve the head and neck such as bell`s palsy ,adenoid cystic carcinoma of the parotid gland and tumor of the jaw, these conditions may produce neurologic symptoms such as parasthesia or paralysis .
THE EXTRA-ORAL EXAMINATION
1-General appraised of the patient:
The objective of general appraised is to obtain a general idea of the patient`s physical status . The examiner should note
*The patient gait
*The patient stature
*Nutritional status
*Posture
* Facial form
*Vital signs
Gait –
Refers to the way of the one walks ,a number of disorders can altered gait and may influence the diagnosis and treatment plane .
Stature –
Refers to height and build .
Nutritional status—
Is an evaluation of the degree of obesity or emaciation .
Posture –
Refers to the position of the body.
Vital signs –
Include (blood pressure ,pulse ,respiratory rate and temperature ).
*The blood pressure:
Is taken by using a sphygmomanometer and a stethoscope . Measurement of the blood pressure is used to detect undiagnosed hypertension and if the patients may have a disease that cause hypertension or result from hypertension . The cuff is placed around the arm and secure in position approximately one inch above the antecubital fossa . It is generally accepted that a patient is considered hypertensive when the systolic /diastolic blood pressure exceed a measurement of 150/90 .
*The pulse rate:
Can be taken as the dentist palpates the radial artery . The examiner should use the fingertip rather than the thumb . The pulse rate can be recorded in beats per minute and the normal value is 72/minute . The examiner can evaluate rythme (regular or irregular ). The average rate of the pulse is 60-90 beats/minute . The pulse rate greater than 100beats/minute is termed tachycardia , whereas abnormal slow pulse rate less than 60beats/minute is termed bradycardia .
*The rate of respiration :
Is the number of inspiration recorded during one minute. The normal rate for an adult is approximately 14-18/minute.
*temperature:
Is accomplished by using an oral thermometer . Normal oral temperature is 98.6of (37oc) +0.5of . Rectal temperature is about 1of higher than oral and axillary temperature is about 1of lower than oral .Infection is a common cause for an elevated temperature , hyperthyroidism also elevate the temperature . A decrease in temperature or hypothermia can be associated with a hypo metabolic state such as myxedema .
2-Examination of the head :
This examination includes an evaluation of all structures associated with the head . The following areas are included in the examination (face , hair ,skin , eye , ear , pre & post auricular lymph node ,nasal & para nasal sinus ,TMJ and parotid gland ).
*The face form ;The examiner should note the position of the eye ,nose , mouth and ear as well as their size and symmetry .
*The skin is examined by observation and palpation in order to know the color ,texture ,elasticity , presence or absence of edema .
*The examination of the eye is important since many condition with oral involvement also exhibit ophthalmic changes .The sclera is examined to note the color changes such as
Redness ----------allergy
Yellow -------------- jaundice
Blueness -----------osteogenesis imperfecta
Ear should be inspected visually for abnormal nodules or distortion .*
*Pre &post auricular LN ; The area surrounding the ear should be palpated to detect LN . Any lymph adenopathy in the area may be due to infection of the scalp , temporal area ,frontal area or the eye .It's also caused by systemic viral infection such as German measles(rubella), chicken pox or infectious mononucleosis.
*TMJ ; clicking , swelling and tenderness
*Jaws ; symmetry , anterio-posterior relationship , lateral and protrusive movement .
3-Examination of the neck
The structures in the neck to be evaluated are*The muscles (sternocleidomastoid ,trapezius muscle ) .
*Submandibular and sublingual salivary gland .
*Lymph node .
*Thyroid gland .
*Trachea and carotid artery .
THE ORAL CLINICAL EXAMINATION
The complete examination of the mouth include evaluation of
1- The soft tissues such as lip, buccal mucosa , palate , oropharynx floor of the mouth and tongue.
2-Periodontium .
3-Teeth .
4-Occlusion .
5-Edentulus and partially edentulous mouth .
LABROTORIES STUDY (investigation)
A wide variety of investigations are available . The most frequently utilized in oral medicine are.1-Radiographic examination .
2-Supplemantary diagnostic aids .
Radiographic examination:
The interpretative of radiograph requires knowledge of radiographic appearance of normal anatomy and of pathologic conditions as well as ability to correlate these appearance with clinical findings . Prior to making radiography , the dentist should ask the patient some questions . If the patient is female , the dentist should ask if she might be pregnant or not .
There are two type of radiographic examination
1-Intraoral (periapical ,occlusal )
2-Extaoral
*Trans- cranial& Trans pharyngeal to see the head and neck of the condyle .
*Lateral oblique view to see the ramus and body of mandible
*Cephalometric projection
*Anterio-posterior projection for mandible
*Water view or sinus view
Supplementary diagnostic aids :
After termination of all clinical and radiographical examination of the patient , sometime further investigation are needed . this may be either to
*Confirm a suspected disorder.
*Obtain more information before diagnosis is made .
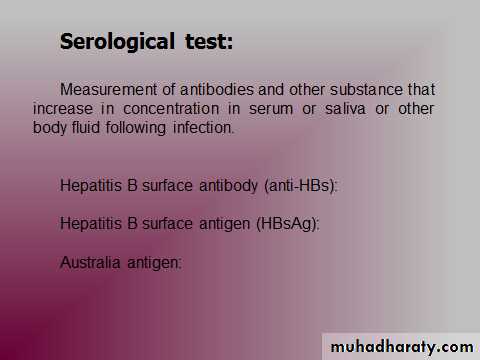
There are many other histopathological ,bacteriological , hematological , biochemical , serological and immunological tests which might occasionally be needed in the diagnosis of oral condition .
1-Bacteriological studies:
a-Preparation of stained smear ;
. Smear of the oral mucosal cells and exudate are usually studied in detail for the following reason .
*To determine the morphology of the micro-organism . The smear is usually air dried , heat , fixed and gram stained.
*To determine premalignant and malignant changes in the oral mucosa . The smear may be immediately fixed with 95% alcohol and stained by the Papanicolaou stain .
* To determine giant cells and other unusual cells that occur in vesicular virus infection (herpes simplex , varicella zoster) and pemphigus . The smear may also be air dried fixed with methanol and Giemsa stained .
b-Bacterial culture and sensitivity testing ;
Are used to isolate and identify causative micro-organism . After isolation , the micro-organism is exposed to a number of antibiotic agents to determine which affect growth . It is helpful in evaluating (throat infection , exudate from sinus infection , root canal infection and bone infection )
Indication of sensitivity test :
*1. When patient dose not respond to therapy.
*2. When patient relapses.
*3. Identification of M.O is uncertain .
*4. When the disease is sever
Sensitivity testing is done in one of several way ;
*Disk diffusion
*Test tube dilution
*Agar diffusion
c-Caries activity test ;
A verity of tests have been designated to measure difference in cariogenic potential of oral cavity . The most frequently used methods for determining caries activity or susceptibility* Lactobacilli count :
A quantitative estimation of lactobacilli present in milliliter of saliva . count of lactobacilli (1000 –10000)/ml suggest low caries activity , count of (50000)/ml of saliva indicate a high caries activity .
* Snyder test ;
Utilize an acid medium containing bromcresol green which when inoculated with saliva . A change in color of the medium within (24h) is generally considered to be indicative of a high caries rate , color changes delayed from (48-72h) indicates less caries activity , whereas no color changes within (4days) is considered to be indicative of no caries activity .
*Fosdick test ;
Measure the rate of dissolution of calcium in powdered enamel .
2-Biopsy test :
It is defined as a tissue removed or the surgical removal of living tissue for the microscopic examination . Biopsy test is indicated;
* To confirm the diagnosis of malignancy in clinically suspicious lesion .
* As a diagnostic aid in evaluation of non-diagnostic lesions as (erosive lichen planus , pemphigus and pemphigoid) .
Types of biopsy :
*Excisional biopsy ;remove all the lesion and send to the lab. It is considered as treatment as in small lesion .
*Incisional biopsy ;
In which a segment of the lesion is removed mostly wedge shape from diseased and normal tissue in certain depth to see the reaction of the tissue .
*Needle biopsy ;
It is the microscopic examination of an aspirate obtained by inserting a fine needle into lesion. It is a painless & a save procedure for rapid diagnosis . Indicated in lesion deep to the surface as lymph node , salivary gland and thyroid gland or bone lesion .
*Intra osseous biopsy;
It is less frequently performed. it may be in the form of exploratory curettage in which the representative tissue is obtained to determine the nature of large radiological alterations.
* Punch biopsy ;
In this technique, a sharpened hollow tube of several millimeters in diameter is rotated until underlying bone or muscle is reached.
* Frozen section biopsy ;
It is performed in order to get an immediate histological report of a lesion.
Indications
To determine whether a lesion is malignant or not.
To evaluate the margins of an excised cancer.
To ascertain that the entire lesion is removed at the time of surgery.
Procedure
The tissue is obtained from lesion & it is kept in deep freeze & then frozen tissue is sectioned & stained to get a prompt diagnosis.
* Oral CDx test ;
It is highly specialized computer assists analysis of an oral brush biopsy performed on oral tissue. It is the most recent development in oral biology technique. This technique is ideal for determining the need for scalpel biopsy in benign appearing oral mucosal leukoplakia
3-Oral exfoliative cytology :
Refers to the microscopic examination of surface cells that have been removed from oral mucosa by scraping . The cells collected are smear on a glass slid and fixed.Indication of exfoliative cytology ;
1. Diffuse lesion covering large area in mucosa , when many incisional biopsy is needed to determine the range of pathologic changes in tissues .
2. Surface lesion in patient receiving radiation in which biopsy may causes persistent ulceration or osteoradionecrosis .
3. Patient who decline biopsy for certain psychological reason .
4. It is helpful in the evaluated of, vesicles and bulla .
The exfolative cytology is contraindicated in;
1. Lesion covered with normal mucosa .
2. Keratotic lesion .
3. Lesion with grossly necrotic surface .
Note ; definitive treatment can`t be based on exfolative cytological smear for serious diseases .
4-Routine hematology screening :
The formed elements of the blood consist of (RBC , WBC and platelets )
* Complete blood picture: Usually includes the following:
a- RBC count.
b- Hematocrit (Hct).
c- Hemoglobin (Hgb).
d- WBC count & differential WBC count. The differential WBC are neutrophil , basophil , eosinophil , lymphocyte and monocyte .
e- Blood smear for cell morphology.
f- Platelet or thrombocyte count .
* Complete hematologic examination; Include:
a-Mean Corpuscular Volume (MCV).
b-Mean Corpuscular Hemoglobin (MCH).
c-Mean Corpuscular Hemoglobin Concentration (MCHC).
d-Erythrocyte Sedimentation Rate (ESR).
Significance
Normal value
Tests
+ polycythemia
- anemia
4-5 million cell/mm3
Total RBC count
+ polycythemia
- anemia
♂ 40-54%
♀ 37-47%
Hematocrit (Packed cell volume) (PCV)
+ polycythemia
- anemia
♂ 13-18 g/dl
♀ 12-16 g/dl
Hemoglobin (Hgb)
+ bacterial infection, polycythemia, tissue-destructive
disease and some leukemias
- aplastic anemia, bone marrow depression, drug induced myelosuppression,
viral infection
4500-11000 cell/mm3
Total WBC count
+ bacterial infection, steroid therapy, following acute hemorrhage
- aplastic anemia, cyclic neutropenia, cancer chemotherapy, viral infection.
50-70 %
Neutrophils
+ certain viral infection (mononucleosis)
30-40 %
Lymphocyte
+ bacterial endocarditis, T.B, typhoid fever
3-7 %
Monocyte
+ allergy, parasitic infection, Hodgkin's disease, sarcoidosis,
metastatic CA, chronic skin disease (autoimmune)
0-5 %
Eosinophils
0-1 %
Basophil
+ macrocytic anemia
- microcytic anemia
82-98 micron3
Mean Corpuscular Volume (MCV)
+ macrocytic anemia
- microcytic anemia
30 µµg
Mean Corpuscular Hemoglobin (MCH)
- microcytic anemia
35 %
Mean Corpuscular Hemoglobin Concentration (MCHC)
+ In tissue destructive disorder e.g trauma, infections, & malignancy.
♂<10 mm/hr
♀<20 mm/hr
ESR
* Hematocrit (PCV) : Is the volume of packed erythrocyte per 100 ml of blood , the erythrocyte are packed by centrifuge .
* Hemoglobin : Is the oxygen carrying component of RBC .
* Mean cell volume( MCV) :is the ratio of the hematocrit to the RBC count .
* Mean cell hemoglobin (MCH) :is the ratio of Hgb to RBC and expressed in picogram .
* Mean cell hemoglobin concentration (MCHC) :This index is a ratio of the hemoglobin to hematocrit . The value is expressed in percentage of volume of RBC , the MCHC measure the concentration of Hgb in gram /100ml of packed erythrocytes .
* WBC or leukocyte are classified as
1-Granulocytes (neutrophile ,eosinophil and basophile )
2-Non granulocyte (lymphocyte and monocyte )
*Erythrocyte sedimentation rate( ESR) : This test measure the rate of sedimentation of red blood cell in tube of fixed volume . It is nonspecific test for evidence of tissue destruction due to ( infection ,infarction , trauma and malignancy)
Values of ESR:
1-male under 50 years ≤15 mm/h
2-male over 50 years ≤ 20 mm/h
3-femal under 50 years ≤30 mm/h
4-femal over 50 years ≤40 mm/h
*Uric acid ; in male (2.1-7.8 mg/100ml)
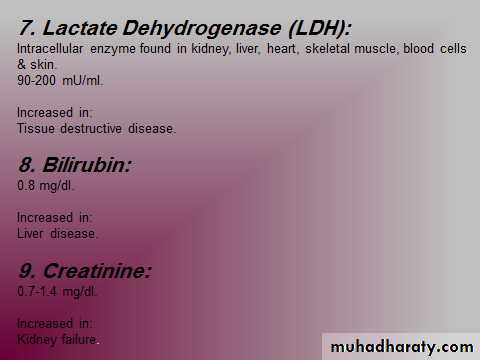
In female (2-6.4 mg/100ml)*Cholesterol ; (150-250 mg/100ml) it has little value in dentistry , increased in CVS disease , bilary obstruction , hypothyroidism and chronic hepatitis
*Total protein ; (6-7.8mg/100ml)
*Albumin /globulin ratio Ab (3.2-5.6 mg/100ml)
Gb (2.3-3.5mg/1ooml)
*Blood urea nitrogen ; (8-18mg/100ml)
*Various electrolyte ; Na ,K , Cl ,Co2
*In hepatitis the hyperbilirubinemia is result of hepato-cellular damage but in other diseases it may result from either over production of bilirubin as in hemolytic anemia or obstruction to the flow of bile e.g in intra hepatic polycystitis as in liver cirrhosis or extra hepatic polycystits due to mechanical blockage of the bile duct from gall bladder stone .
Immunofluorescence :
Fluorescence dye can be conjugated to antibodies and such labeled antibodies can be used to locate and identify antigen in tissue . There are three type of immunofluorescence technique*Direct immunofluorescent technique ;
The antibody is conjugated with fluorescein and applied directly to the tissue on a slide . In testing for pemphigus and pemphigoid , IgG isolated from the patient`s serum is labeled with fluorescein and incubated with tissue from a biopsy specimen of the patient oral mucosa or skin .
In pemphigus, the fluorescence is located to the intercellular spaces between epithelial cells of the mucosa or skin.
In pemphigoid , the fluorescence is located to the basement membrane zone separating epithelium from underlining connective tissue.
*indirect immunofluorescent technique;Secondary (indirect) immunofluorescence uses two antibodies; the unlabeled first (primary) antibody specifically binds the target molecule, and the secondary antibody, which carries the fluorophore, recognizes the primary antibody and binds to it. Multiple secondary antibodies can bind a single primary antibody. This provides signal amplification by increasing the number of fluorophore molecules per antigen. This protocol is more complex and time-consuming than the primary (or direct) protocol, but allows more flexibility because a variety of different secondary antibodies and detection techniques can be used for a given primary antibody.
*sandwich technique
Type of ABIndirect IF
Location
Direct IF
Disease
IgG
+ if disease widely spread
Inter cellular
+
Pemphegus volgaris
IgG
+ if disease widely spread
Basement membrane
+
Bullous pemphigoid
IgG
Usually
Basement membrane
In sever case +
MM pemphegoid
Antinuclear AB
+
Basement membrane
+
Systemic LE
Antinuclear AB
Usually
Salivary duct cell
+
Sjogren`s syndrome
Diagnosis & treatment planning :
Diagnosis : Mean the identification of a disease by an investigation of the signs & symptoms .Differential diagnosis : Is the determination by systematic comparison & contrast of symptoms of several diseases from which a patient suffering .
Treatment planning:
Successful dental treatment is always based on careful planning . The objective of dental treatment planning is to devise the best dental treatment for each patient . The what to do and when to do it constitute the treatment planning .
Outlines for a treatment plan
Treatment planning is depended upon an accurate diagnosis, which in dentistry includes a consideration of all oral structures. Treatment plan is made with these consideration in mind:
The urgency of treatment.
The sequence of treatment.
Result expected from treatment.
General format of the treatment planning :
Most treatment plans follow the same general pattern and several authors have developed format for treatment plans . A format that works effectively in both private practice & institutional dentistry is
*Phase I : priority treatment
*Phase II: disease control
*Phase III: restoration of function & esthetic
*Phase IV: re-evaluation
*Phase V: re-call
Priority treatment:
Designed for procedures that will eliminate1-Acute infection ( cellulitis , NUG , abscess ) .
2-Acute pain .
Disease control :
In this phase , work is completed to control all disease processes but not necessarily eradicate all disease . the following items should be completed in this phase
1-Mangement of the chief complain if not completed in phase I.
2-Oral hygiene instruction .
3-Most oral surgery .
4-Periodontics
5-Endodontic .
6-Orthodontic .
7-Occlussal analysis .
Restoration of function & esthetic :
Includes all remaining procedures which are used to eliminate all disease &restore the full function & esthetic . it is include
1- Operative dentistry ( crown & bridge )
2- Prosthetic therapy
Re- evaluation:
Is usually re-examination to evaluate the treatment plan & to determine additional therapy necessary before the patient is placed on recall state .
Re-call:
Is usually occurs many years after treatment.
Prognosis :
Is a forecast of the probable result of treatment .the objects of prognosis determination are:1-To forecast the success of the treatment plan .
2-To identify interrelation ship of factors .
3-To select the factor that may significantly limit success .
4-Tto develop ultimate treatment plan or establish planning of treatment to correlate with adverse factors .
5- To abort a treatment plan that will fail .