1
stage
th
5
Dr.Khalid Ali
rthopaedics
O
Upper Limb Injuries
The great problem with upper limb injuries is joint stiffness shoulde. Two
points should be considered:
1. Whatever the injury – should encourage exercise from the start
especially the fingers.
2. In elderly patients it is sometimes best to disregard the fractures
and concentrate on regaining movements.
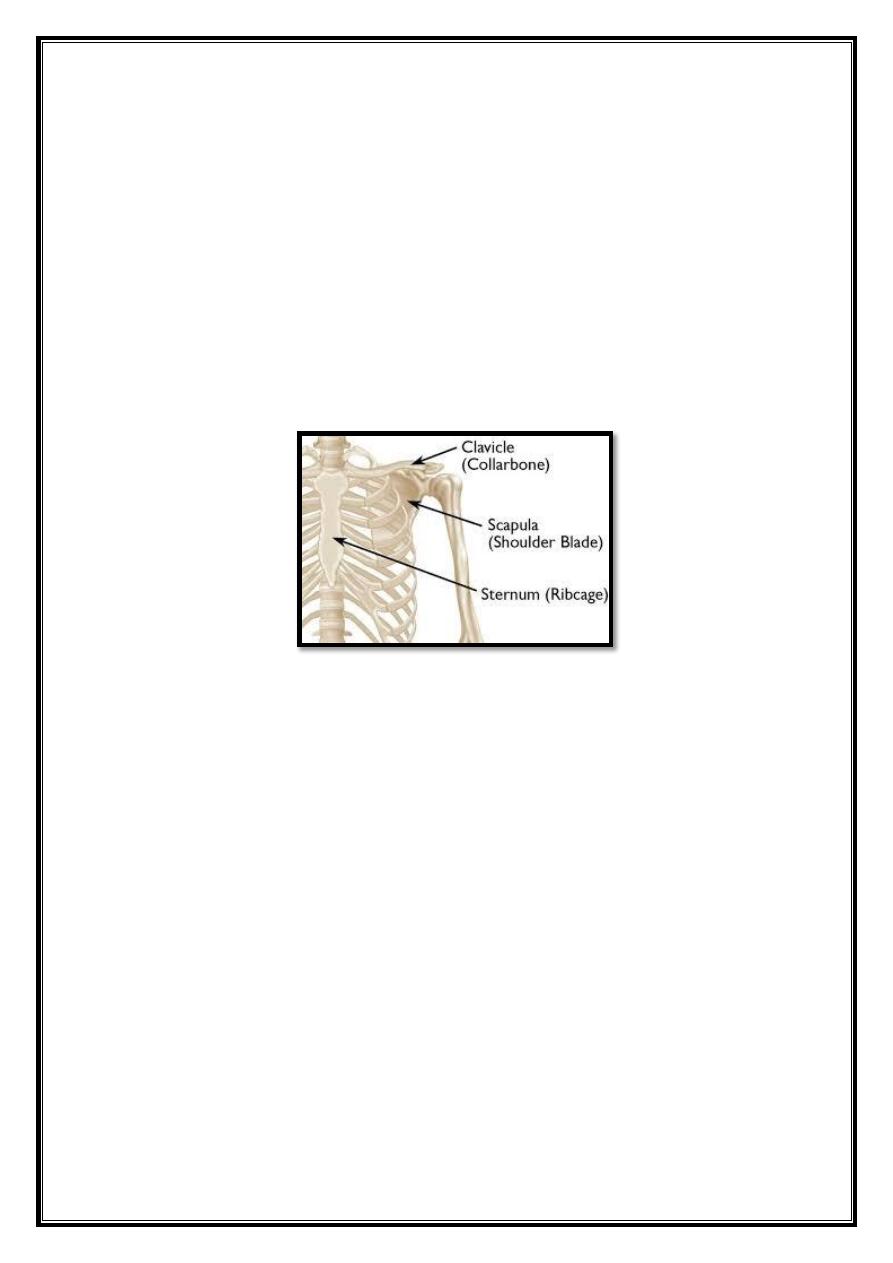
Anatomy of the Shoulder region
Fractures of the Clavicle
It is a common fracture. In children it is almost rapidly unites, often
without complications. In adults it can be a much more troublesome
injury.
Mechanism of injury: A fall on the shoulder or the outstretched hand.
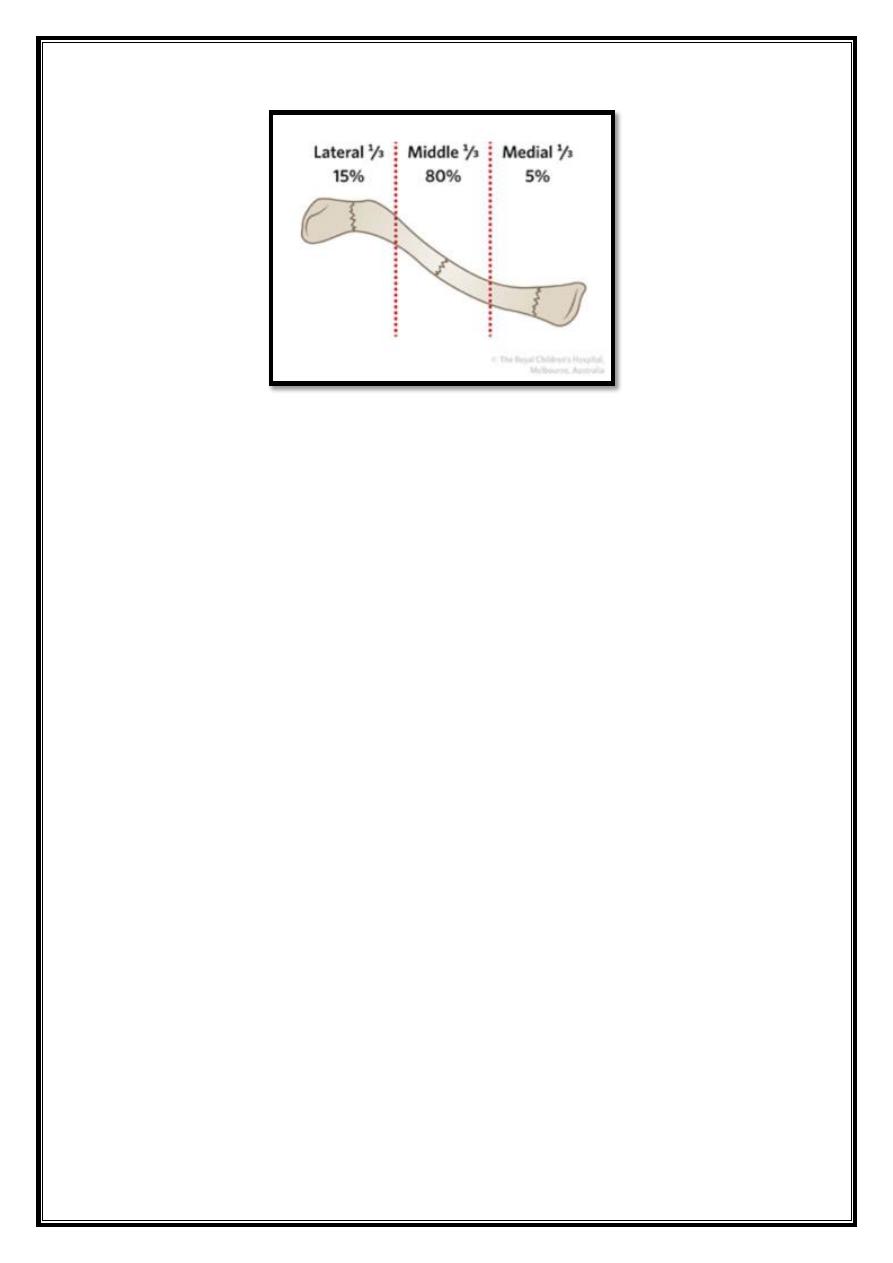
Types:
Type I: Middle 1/3 fractures: it is the commonest type. The outer
fragment is pulled down by the weight of the arm and the inner fragment
is held up by the sternomastoid muscle.
Type II
:
Lateral 1/3 fractures: if the coracoclavicular ligament is intact
there is only little displacement, but if torn, displacement may be severe
and closed reduction is impossible.
Type III: medial 1/3 fracture: it is rare.
2
Clinical Features
the arm is held to the chest to prevent movement, an acutely tender
subcutaneous lump may be obvious and occasionally a sharp fragment
threatens the skin. Lateral third fracture may be missed or mistaken for
acromioclavicular joint injury.
X-ray:
at least an AP view, additional views. The ‘clinical’ union usually
precedes ‘radiological’ union by several weeks.
CT scan
is indicated:
Need to assess accurately the degree of shortening
For diagnosing sternoclavicular joint fracture-dislocation.
Establish whether a fracture has united.
Treatment
Non-operative: arm sling for 1-3 weeks, followed by gradual shoulder
exercise. Non-displaced or mildly displaced.
Indications of surgery:
1. Associated major neurovascular injury.
2. Compound fracture.
3
3. Middle 1/3 fracture if grossly displaced or there is more than 2 cm
shortening.
4. Displaced lateral third fracture: fracture fixation and ligament
reconstruction.
5. Symptomatic non-union.
6. Medial 1/3 fracture displacement threatens the mediastinal
structures.
Complications:
Early: very rare: pneumothorax, subclavian vessels and brachial
plexus injuries.
Late:
- Non-union, risk factors: increasing age, displacement,
comminution, and female sex, and lateral third fracture (11-40
%).
- Malunion: shortening more than 1.5cm lead to periscapular
pain.
- Stiffness of the shoulder joint, and sometimes fingers.
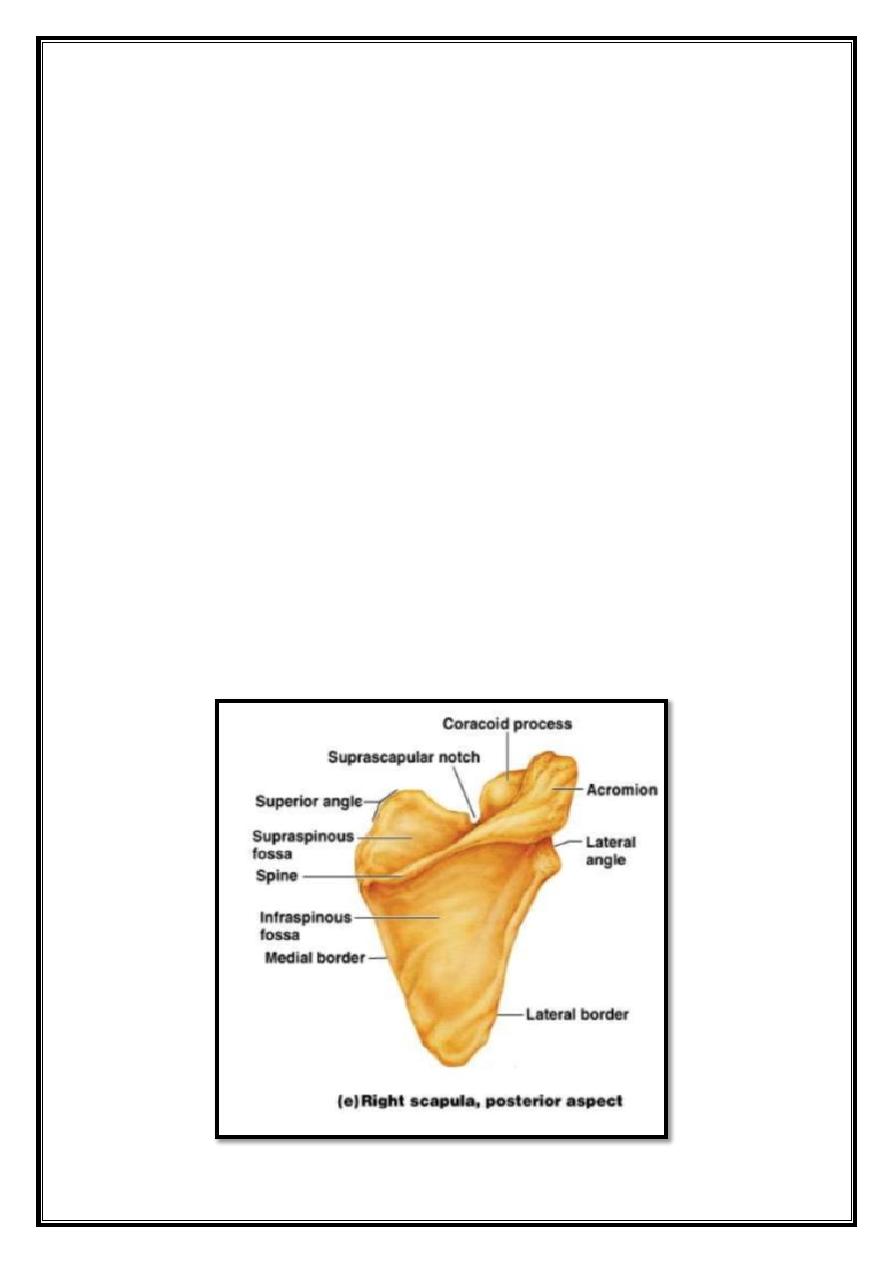
Fractures of The Scapula
4
Types:
1. Scapular body fracture.
2. Glenoid neck (most common).
3. Glenod fossa # (intra-articular).
4. Acromion fracture.
5. Coracoid process.
Clinical features
the arm is held immobile, and there may be severe bruising over
the scapula
or the chest wall.
Always look for associated serious injuries : the chest, spine,
abdomen, head,
vessels, and brachial plexus.
X- ray:
scapular fractures can be difficult to define on plain x-rays
because of the surrounding soft tissues. CT is useful for demonstrating
fractures especially body and glenoid fracture.
Treatment
Sling, analgesia, and exercise.
Grossly displaced # or associated with shoulder instability, needs
open
reduction and internal fixation.
Combine fractures: fracture of glenoid neck and fracture clavicle
‘floating
shoulder’: surgical fixation.
5
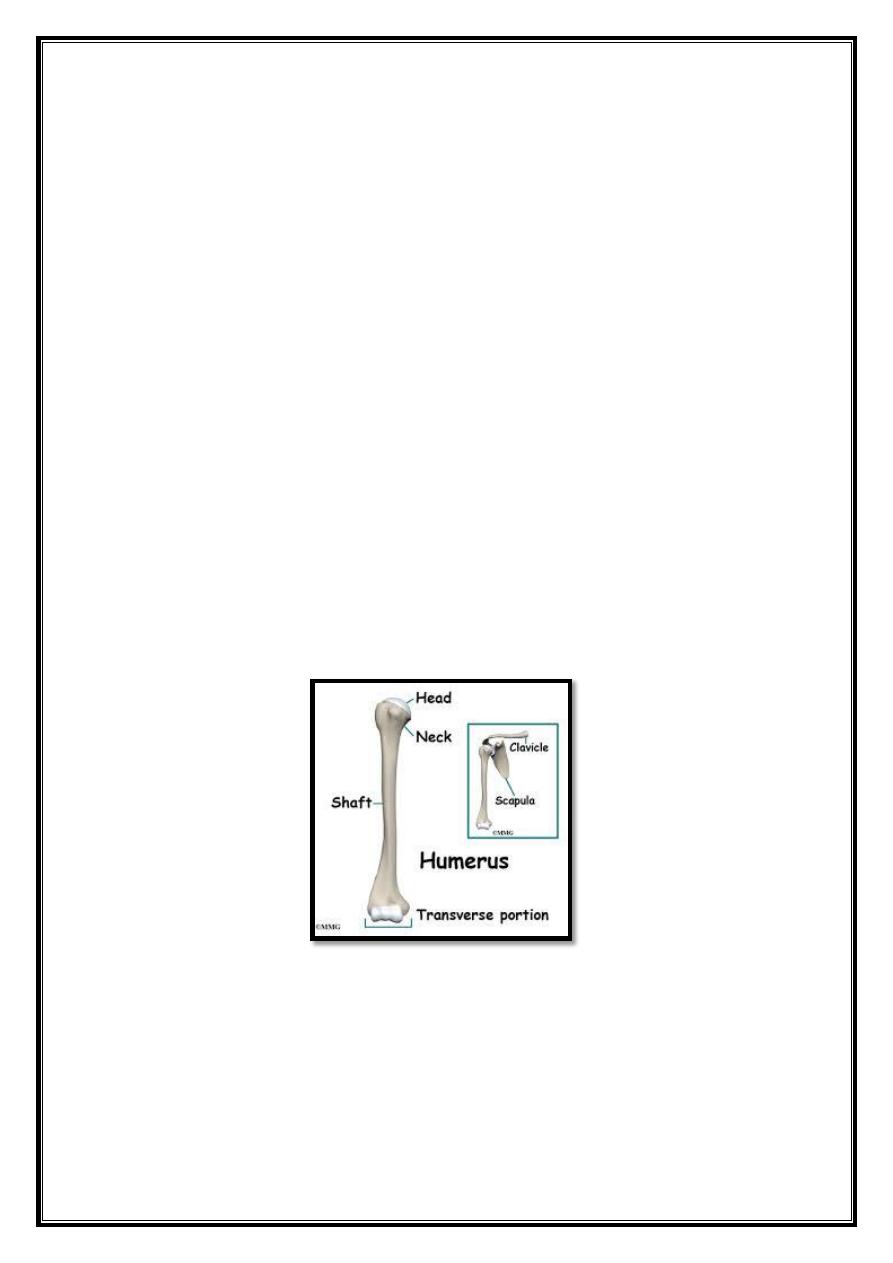
Fractures of Proximal Humerus
Types (Neer’s Classification):
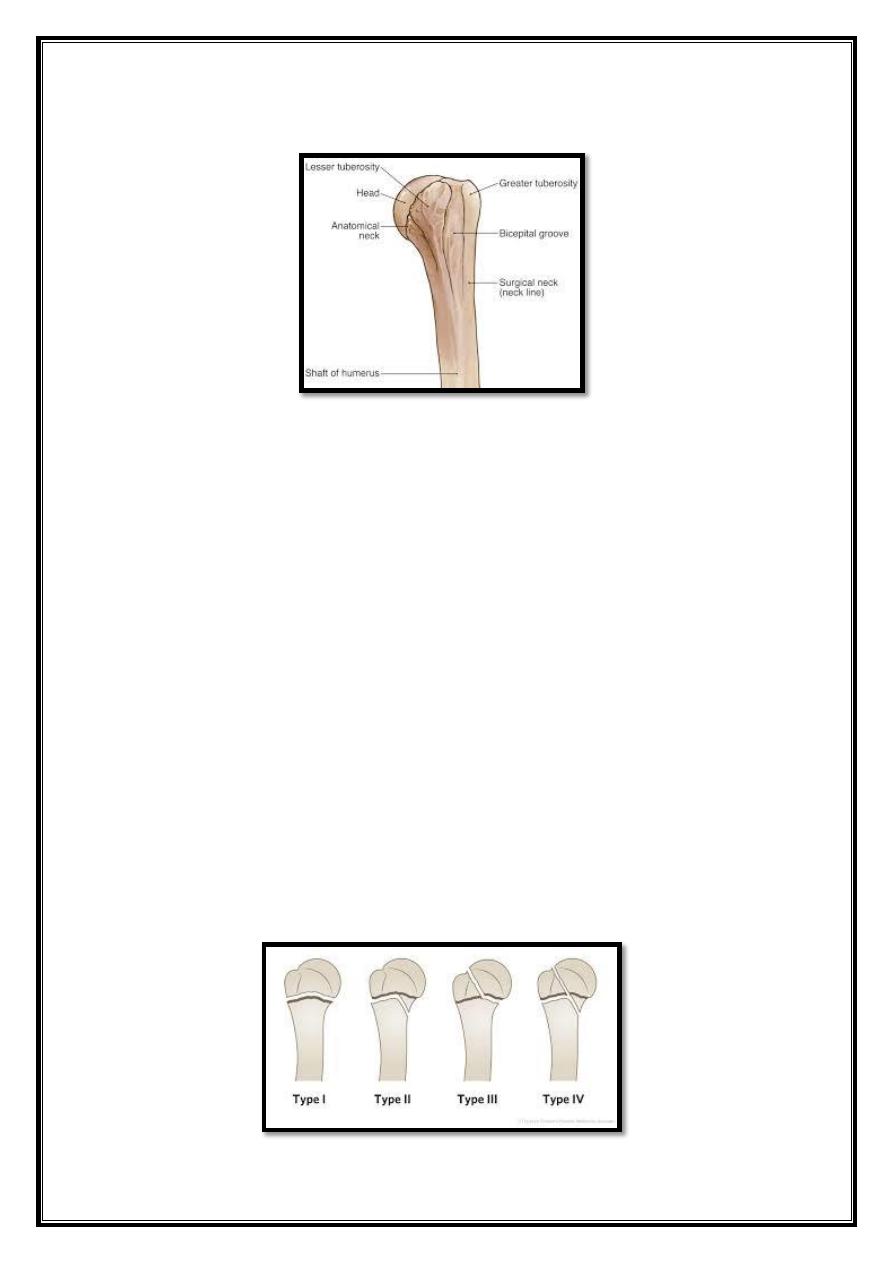
The proximal humerus:
Shaft.
Head.
Greater tuberosity.
Lesser tuberosity.
N.B: The fragment considered to be displaced: if there is more than 1cm
separation or more than 45- degree angulation.
Neer’s Classification:
One-part fracture: even if there are many fracture lines, if the
fragments are undisplaced. It is the most common type.
Two-part fracture: if one major fragment is displaced, as
displaced fracture
of anatomical neck, surgical neck.
Three-part fracture: if two major fragments are displaced.
Four-part fracture: if all the major fragments are displaced.
Fracture-dislocation: if the head of humerus is dislocated plus
two-, three-, or four- part fracture.
6
-
It can occur at any age, but it is most commonly seen after a middle
age.
Most of the patients are osteoporotic, postmenopausal women.
-
It is usually occurring after a fall on outstretched hand. In young
patient
this injury may cause shoulder dislocation.
-
Fracture displacement is usually not marked and only in about 20
% of cases there is considerable displacement of one or more
fragment.
Clinical Features
because the fracture fragments are often firmly impacted, pain may not be
severe. However, the appearance of a large bruise is suspicious.
Radiology:
plain x-ray has high level of inter-observer variation. CT scan
greatly clarifies the fracture fragments.
Treatment
One-part #: only 1-2 weeks arm sling then exercise; passive then
active.
Two- part fracture:
Surgical neck: the fragments are gently manipulated into
alignment and the arm is immobilized in a sling or cast for 4
weeks. If the fracture cannot be reduced closed or very
unstable, then fixation is required.
Greater tuberosity: it is often associated with anterior
dislocation and usually it reduces to a good alignment when
the shoulder is relocated.
Anatomical neck #: young: fixation with a screw. old
patients: prosthetic replacement: high risk of avascular
necrosis of the humeral head.
Three-part #: best treatment is open reduction and internal
fixation.
Four-part #: very difficult, young patient: ORIF. Elderly patient:
prosthetic
implant.
Fracture dislocation: With two-part#: closed reduction. With
three-part#: ORIF. With four-part#: young active: ORIF, old
patient: prosthetic replacement.
7
Complications
Early:
Vascular injury.
Nerve injury: axillary nerve is at particular risk. brachial plexus
may be
also injured.
Chest wall injury.
Late:
Avascular necrosis of humeral head, especially in three and four
part
fractures.
Stiffness of the shoulder. Especially in old age.
Malunion: in children even considerable displacement or
angulation can be
accepted, because of the marked growth and
remodeling of the proximal humerus.
Downward subluxation of humeral head: it is due to muscle atony
and it
usually recovers once exercises begun.
Fracture Shaft of Humerus
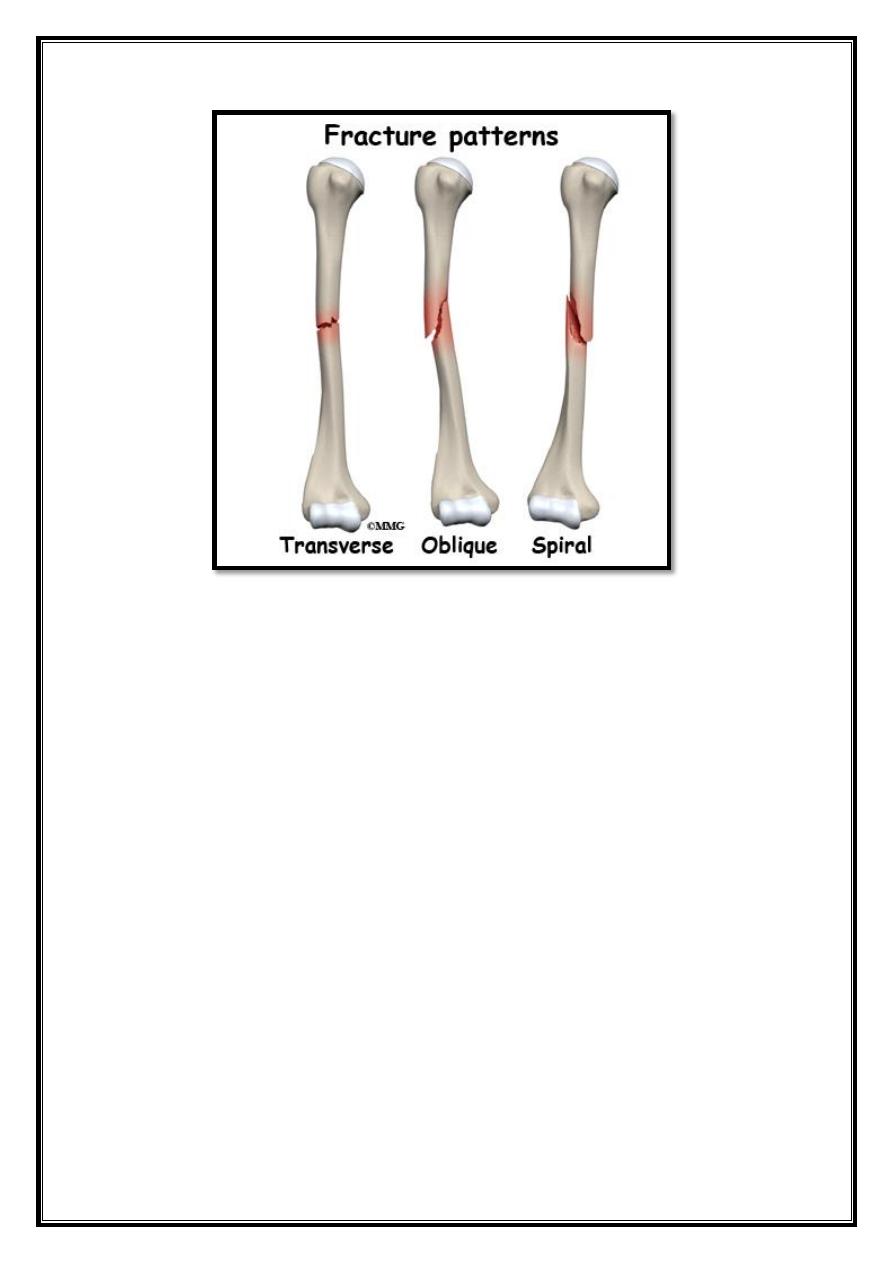
Mechanism of injury:
Fall on the hand (spiral fracture).
Fall on the elbow (oblique or transverse fracture).
Direct blow (transverse or comminuted fracture).
Pathological fracture.
8
Pathological anatomy:
If the fracture is above the deltoid insertion, the proximal fragment is
adducted by pectoralis major. If the fracture is lower down, the proximal
fragment is abducted by the deltoid.
Clinical features:
the arm is painful, bruised, and swollen.
It is important to test for radial nerve function before and after
treatment. Best by assessing the active extension of the MP joint.
X-ray: pathological fracture should be kept in mind.
9
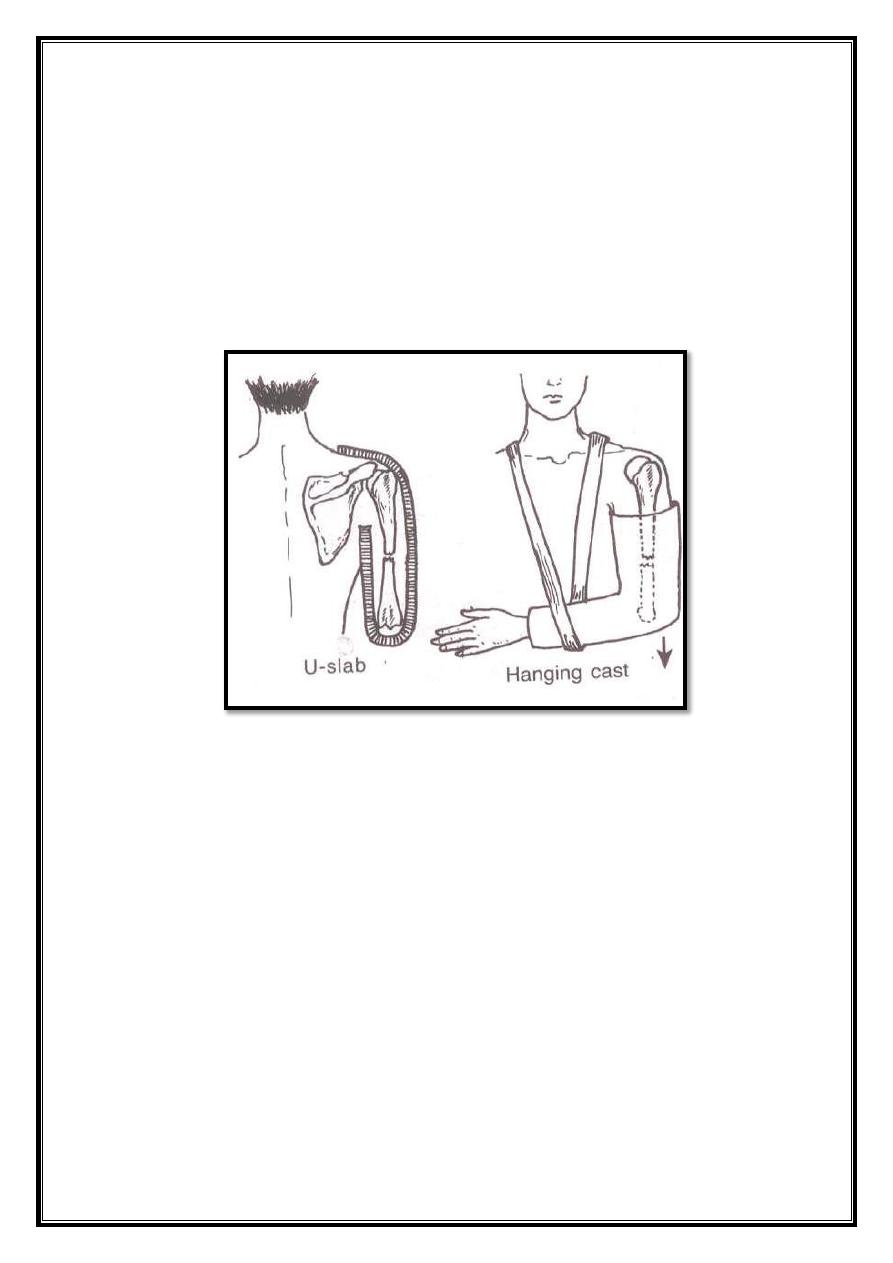
Treatment:
A. Conservative: the fracture shaft humerus, does not require perfect
reduction.
The weight of the arm with an external cast (hanging cast) is usually
enough. This cast is usually replaced after 2-3 weeks by a short cast
(shoulder to elbow- U shape) or a functional brace for a further 6
weeks.
B. Operative: surgery is indicated in the following situations:
1. Severe multiple injuries.
2. Open fracture.
3. Associated major vascular injury.
4. Segmental fracture.
5. Displaced intra-articular extension of the fracture.
6. Pathological fracture.
7. Floating elbow (simultaneous unstable fracture of the humerus and
forearm).
8. Radial nerve palsy after manipulation. NEVER!!!
9. Non-union.
10. Problem with nursing care.
10
Types of fixation:
1. Plate and screws.
2. Intramedullary nail.
3. External skeletal fixation.
Humorous Fracture Recovery: based on several factor:
1. Severity of trauma and soft tissue injury.
2. Number and displacement of bone fragments.
3. Associated Radial Nerve injury.
4. Time delay between injury and treatment.
5. Humorous fracture rehabilitation exercises.
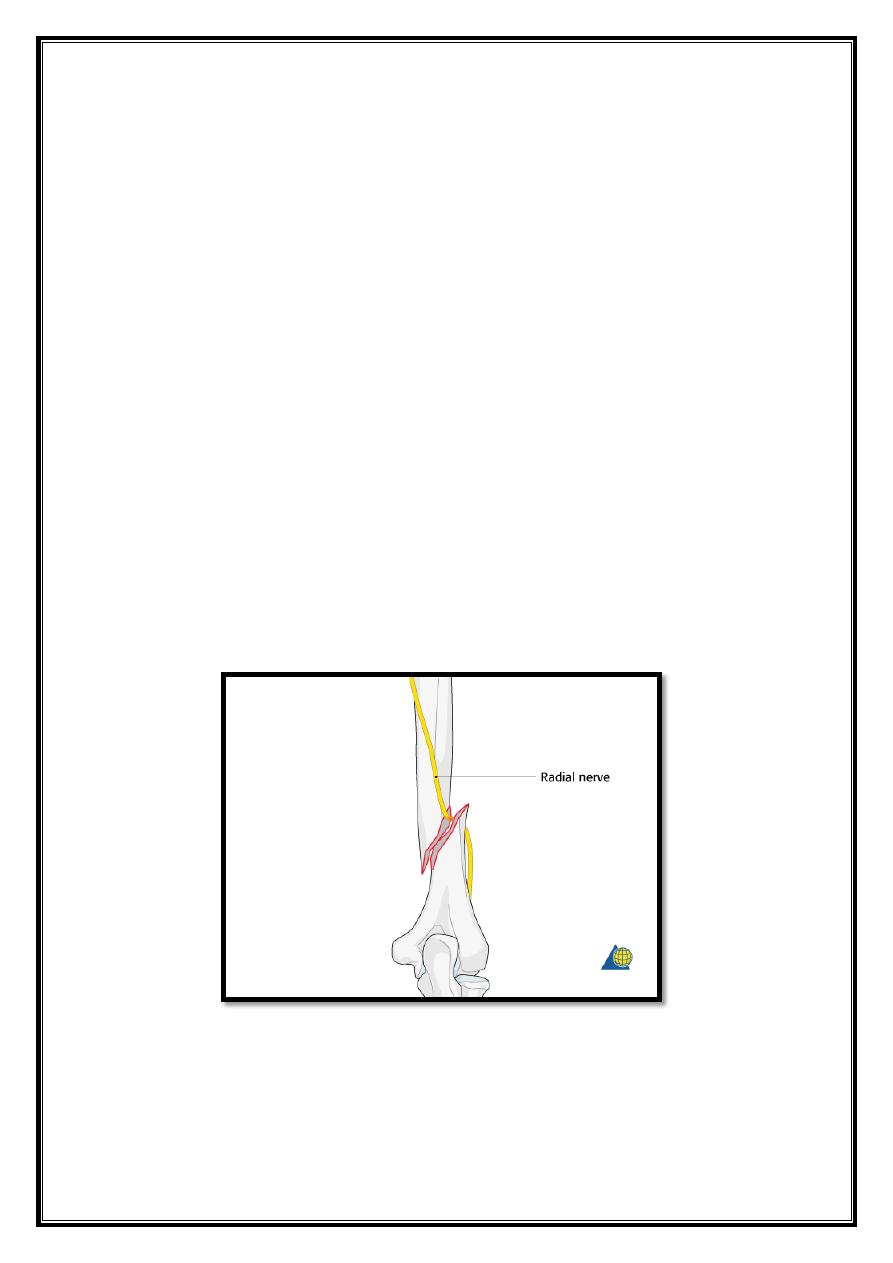
Complications:
Early:
Vascular injury: brachial artery.
Nerve injury: radial nerve injury is common
especially in oblique
fractures at the junction of middle and distal thirds of the bone
(HolsteinLewis fracture).
