1
Biochemistry
stage
nd
2
Dr.Lamees Majid Al-Janabi
Vitamins
Definition:
Vitamins are chemically unrelated organic compounds that cannot be
synthesized in adequate quantities by humans and, therefore, must be
supplied by the diet.
four vitamins (vitamins A, D, K, and E) are termed fat-soluble. In
contrast to the water-soluble vitamins, only one fat soluble vitamin
(vitamin K) has a coenzyme function.
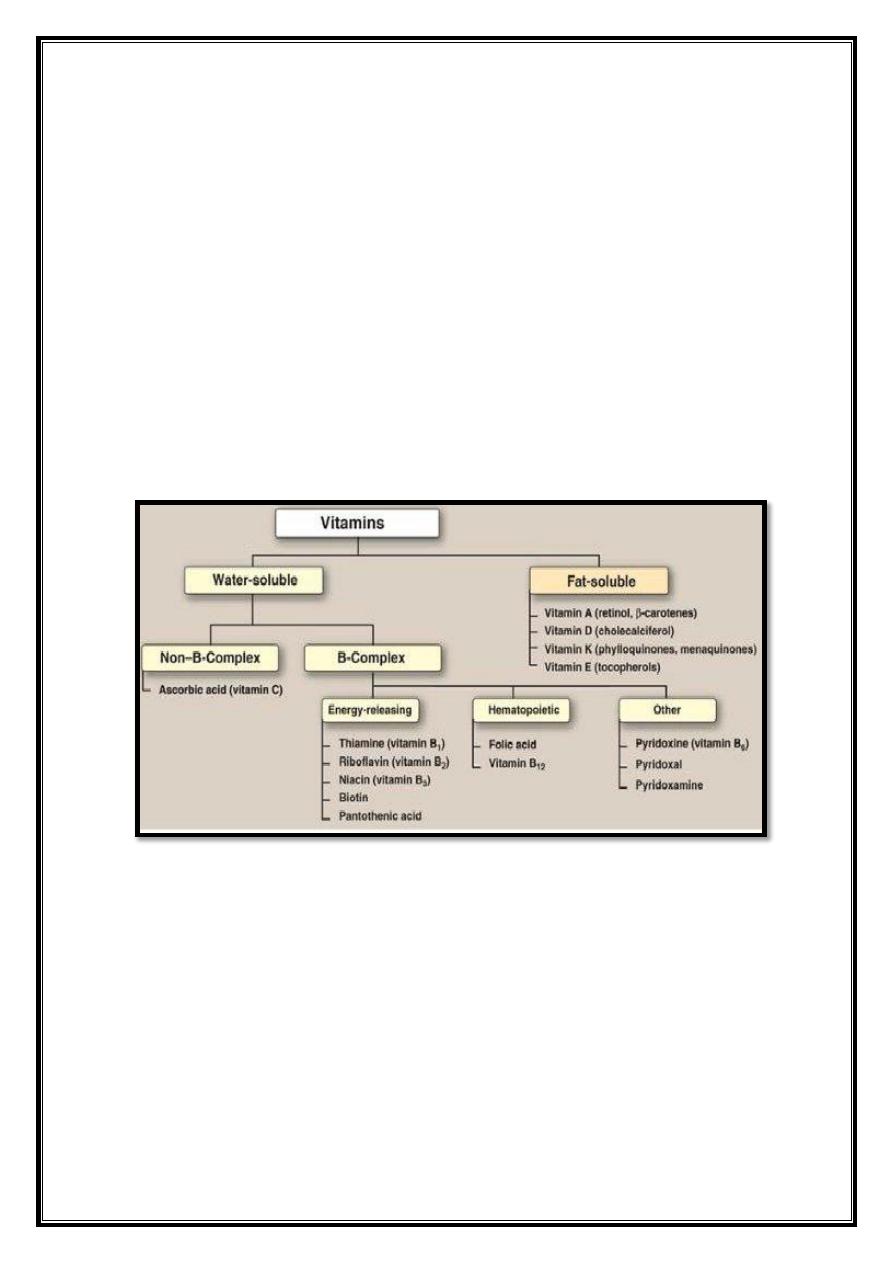
Classification of the vitamins
2
Lipid-soluble Vitamins
Common features:
Nonpolar (hydrophobic) isoprene derivative.
Poorly soluble in water but good in fat and fat solvents.
Existing with the lipids in food products and absorbing with the
lipids .
Specifically binding to lipoprotein and certain binding-protein in
blood and transportation.
Classification:
Vitamin A, Vitamin D, Vitamin E, Vitamin K .
Fat soluble vitamins include (A, K, E, and D) which are released,
absorbed, and transported with the fat of diet. They are not readily
excreted in urine, and significant quantities are stored in the liver and
adipose tissue.
Sometimes excess intake may lead to accumulation of toxic quantities of
these vitamins.
Vitamin A (retinol)
Precursors of vitamin A (the carotenes) are found in the yellow and green
parts of plants and are especially abundant in carrots. The active vitamin
is formed by the hydrolysis of β carotene in the intestinal mucosa; each
molecule can produce two molecules of vitamin A, which are absorbed as
retinol esters and stored in the liver.
Retinol absorbed from the intestine is secreted as a component of
chylomicrons into lymphatic system, to be taken up by, and stored in, the
liver. Retinol is transported to tissues bound to the α-globulin retinol-
binding protein (RBP).
Distribution of vitamin A
Liver, kidney, cream, butter, and egg yolk are good sources of preformed
vitamin A. Yellow and dark green vegetables and fruits are good dietary
sources of the carotenes(especially abundant in carrots), which serve as
precursors of vitamin A.
3
Functions:
Rhodopsin (visual purple), the retinal pigment that is necessary for
vision in poor light (scotopic vision), consists of a protein (opsin)
combined with vitamin A. Rhodopsin decomposes in bright light. It
is partly regenerated in the dark, but, because this is not
quantitatively complete, vitamin A is needed to maintain retinol
levels.
Growth & Reproduction: Especially bone development in children.
Control of cell differentiation and turnover. All-transretinoic acid
and 9-cis-retinoic acid regulate growth, development, and tissue
differentiation
.
Vitamin A is also essential for normal mucopolysaccharide
synthesis and mucus
secretion.
Clinical effects of vitamin A deficiency
a. Owing to rhodopsin deficiency:
‘night blindness’ (nyctalopia): deficiency is associated with poor
vision in dim light, especially when the eyes have recently been
exposed to bright light.
b. Owing to deficient mucus secretion leading to drying and
squamous metaplasia of ectodermal tissue:
1. Skin secretion is diminished and there may be hyperkeratosis of
hair follicles. Dry, horny papules (follicular hyperkeratosis) are
found mainly on the extensor surfaces of the thighs and forearms.
2. The conjunctiva and cornea become dry and wrinkled, with
squamous metaplasia of the epithelium and keratinization of the
tissue (xerosis conjunctivae and xerophthalmia).
3. Poor bone growth in the skull, leading to cranial nerve
compression.
Diagnosis and treatment of vitamin A deficiency
Laboratory tests for the diagnosis of vitamin A deficiency consist of
testing for plasma retinol concentration. Retinol-binding protein is also
low in vitamin A deficiency,
Vitamin A deficiency can be treated with retinyl palmitate.
4
Acne and psoriasis:
Dermatologic problems such as acne and
psoriasis are effectively treated with retinoic acid or its derivatives .
Toxicity of retinoids
Vitamin A:
Excessive intake of vitamin A produces a toxic syndrome
called hypervitaminosis A. Amounts exceeding 7.5 mg/day of retinol
should be avoided. Early signs of chronic hypervitaminosis A are
reflected in the skin, which becomes dry and pruritic, the liver, which
becomes enlarged and can become cirrhotic, and in the nervous system,
where a rise in intracranial pressure may mimic the symptoms of a brain
tumor.
NOTE:
Pregnant women particularly should not ingest excessive
quantities of vitamin A because of its potential for causing congenital
malformations in the developing fetus.
Vitamin D
The D vitamins are a group of sterols that have a hormone-like function.
The active molecule, 1,25-dihydroxycholecalciferol (1,25-diOH-D
3
),
binds to intracellular receptor proteins. The most prominent actions of
1,25-diOH-D
3
are to regulate the plasma levels of calcium and
phosphorus.
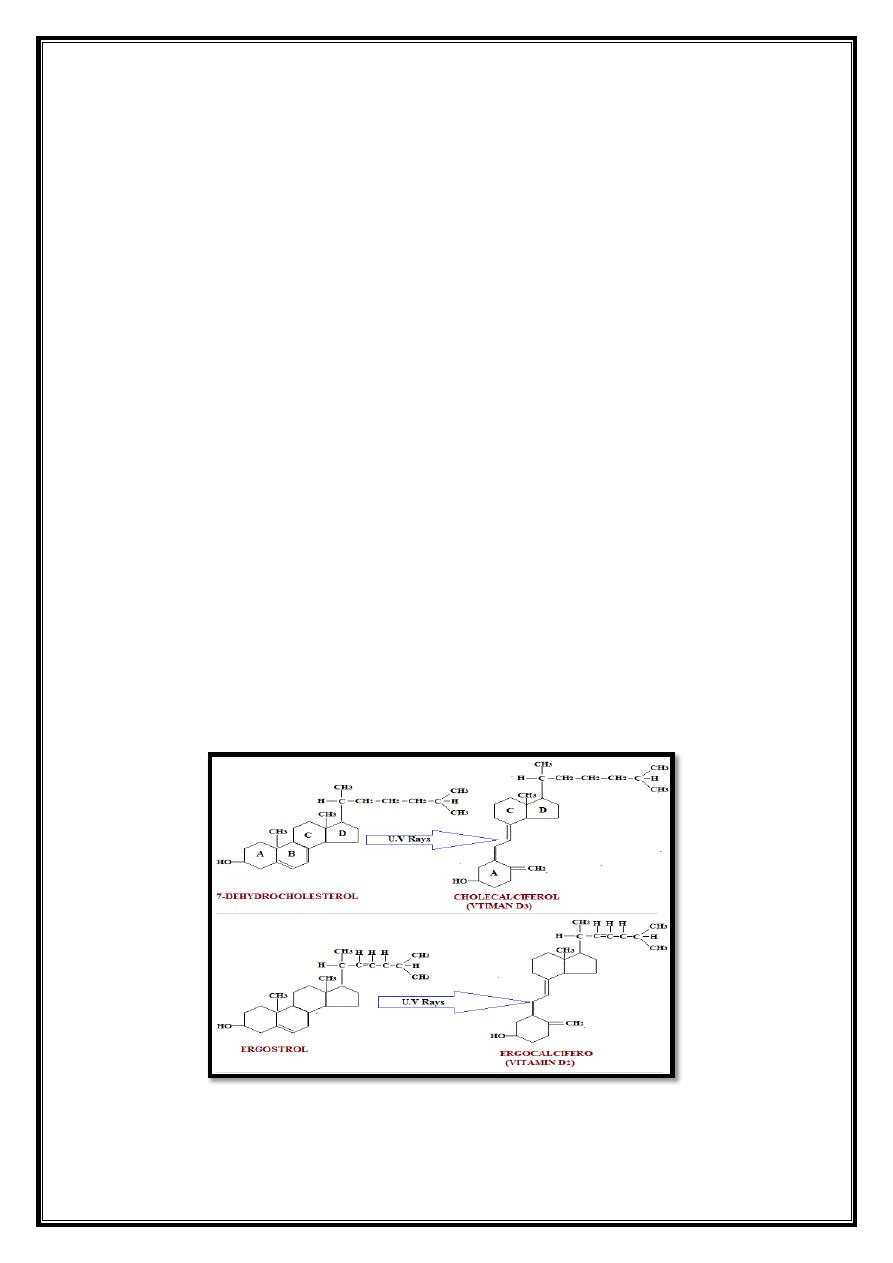
Sources of vitamin D.
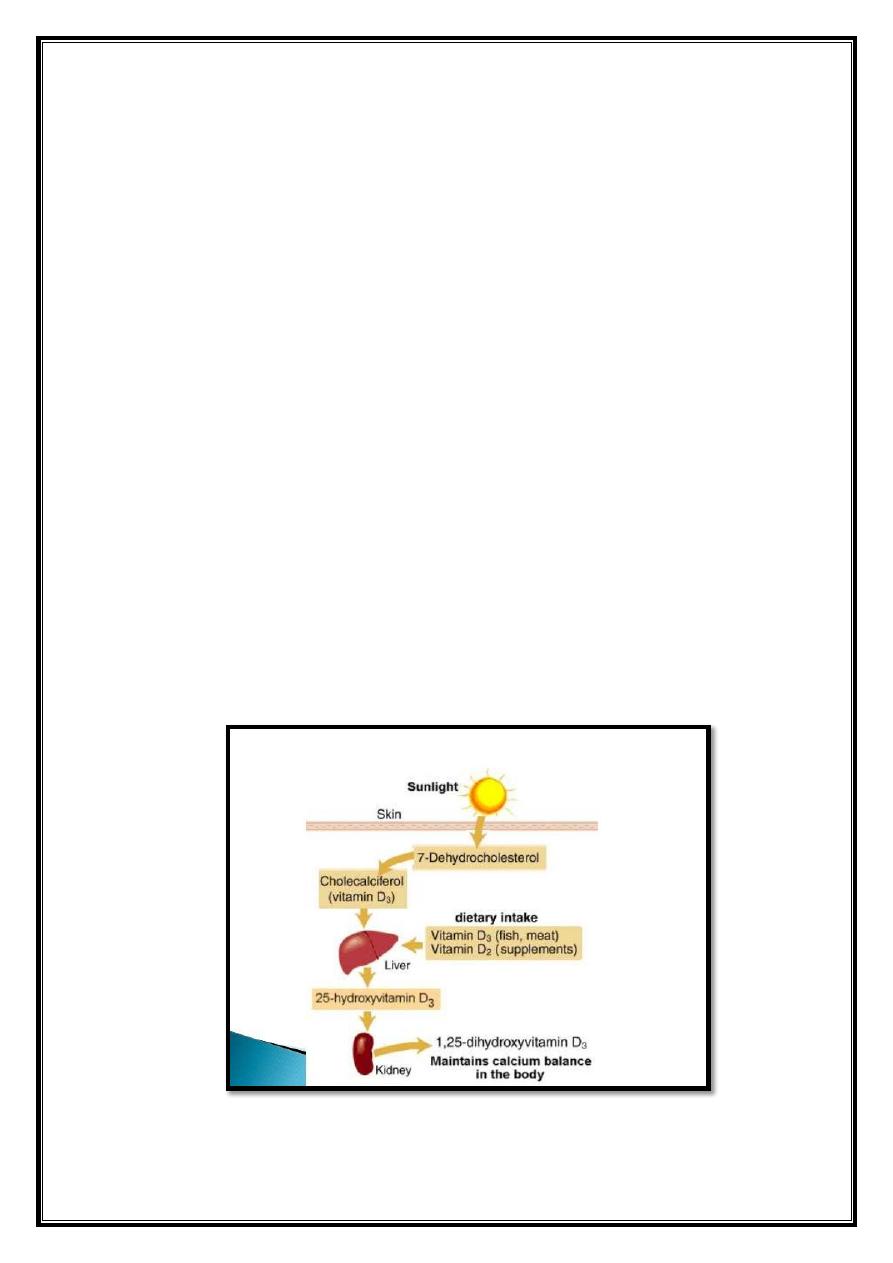
5
Distribution of vitamin D
Diet: Ergocalciferol (vitamin D
2
), found in plants, and
cholecalciferol (vitamin D
3
), found in animal tissues, are sources of
preformed vitamin D activity.
Endogenous vitamin precursor: 7-Dehydrocholesterol, an
intermediate
in
cholesterol
synthesis,
is
converted
to
cholecalciferol in the dermis and epidermis of humans exposed to
sunlight.
Metabolism of vitamin D
Formation of 1,25-diOH-D
3
:
Vitamins D
2
and D
3
are not biologically
active, but are converted in vivo to the active form of the D vitamin by
two sequential hydroxylation reactions
1. The first hydroxylation occurs at the 25-position, and is catalyzed
by a specific hydroxylase in the liver. The product of the reaction,
25-hydroxycholecalciferol (25-OH-D
3
), is the predominant form of
vitamin D in the plasma and the major storage form of the vitamin.
2. 25-OH-D
3
is further hydroxylated at the one position by a specific
25-hydroxycholecalciferol 1-hydroxylase found primarily in the
kidney, resulting in the formation of 1,25-diOH-D
3
.
Metabolism of vitamin D
6
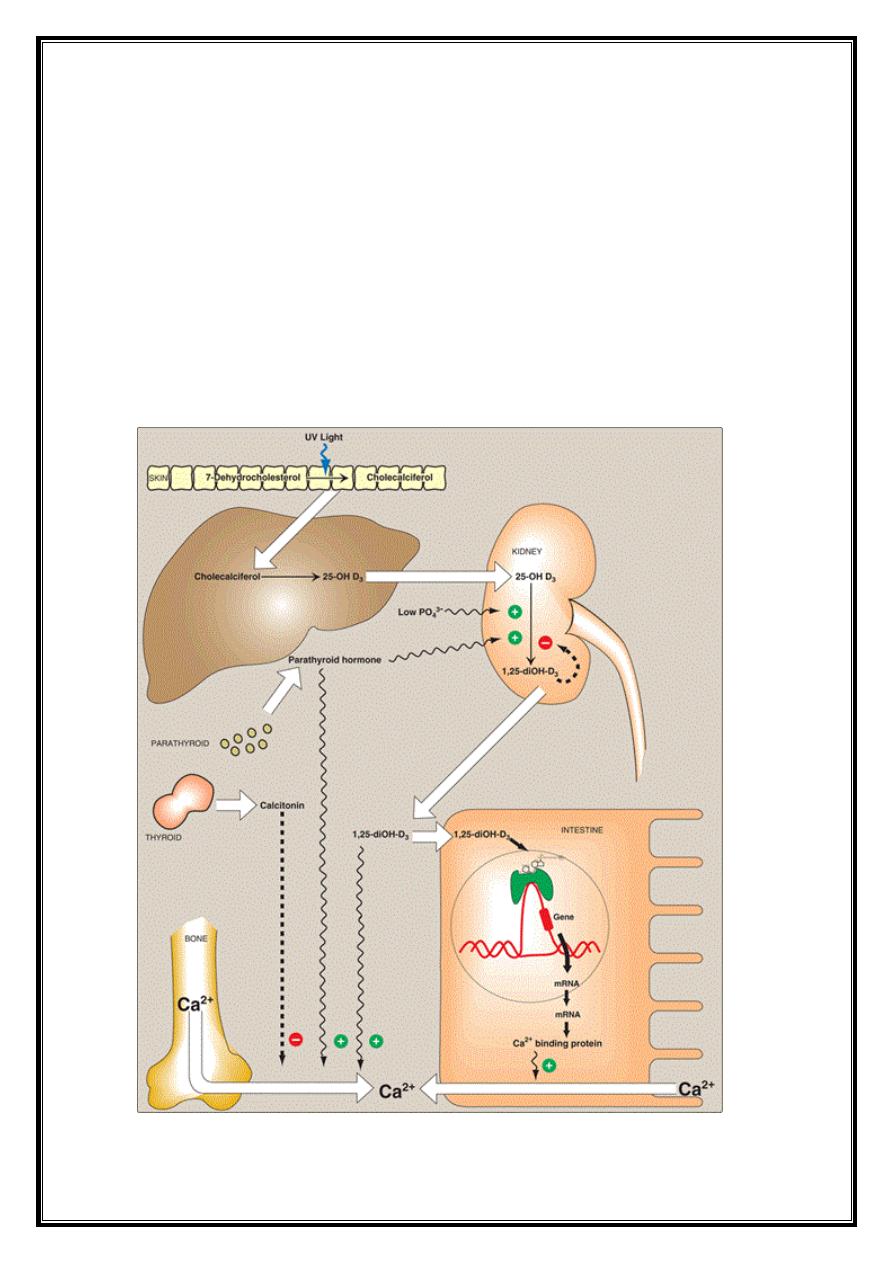
Regulation of 25-hydroxycholecalciferol 1-hydroxylase:
1,25-diOH-D
3
is the most potent vitamin D metabolite. Its formation is tightly regulated
by the level of plasma phosphate and calcium ions.
1. 25-Hydroxycholecalciferol 1-hydroxylase activity is increased
directly by low plasma phosphate or indirectly by low plasma
calcium, which triggers the release of parathyroid hormone (PTH).
2. Hypocalcemia caused by insufficient dietary calcium thus results
in elevated levels of plasma 1,25-diOH-D
3
.
3. 1-Hydroxylase activity is also decreased by excess 1,25-diOH-D
3
,
the product of the reaction.
Regulation of vitamin D metabolism
7
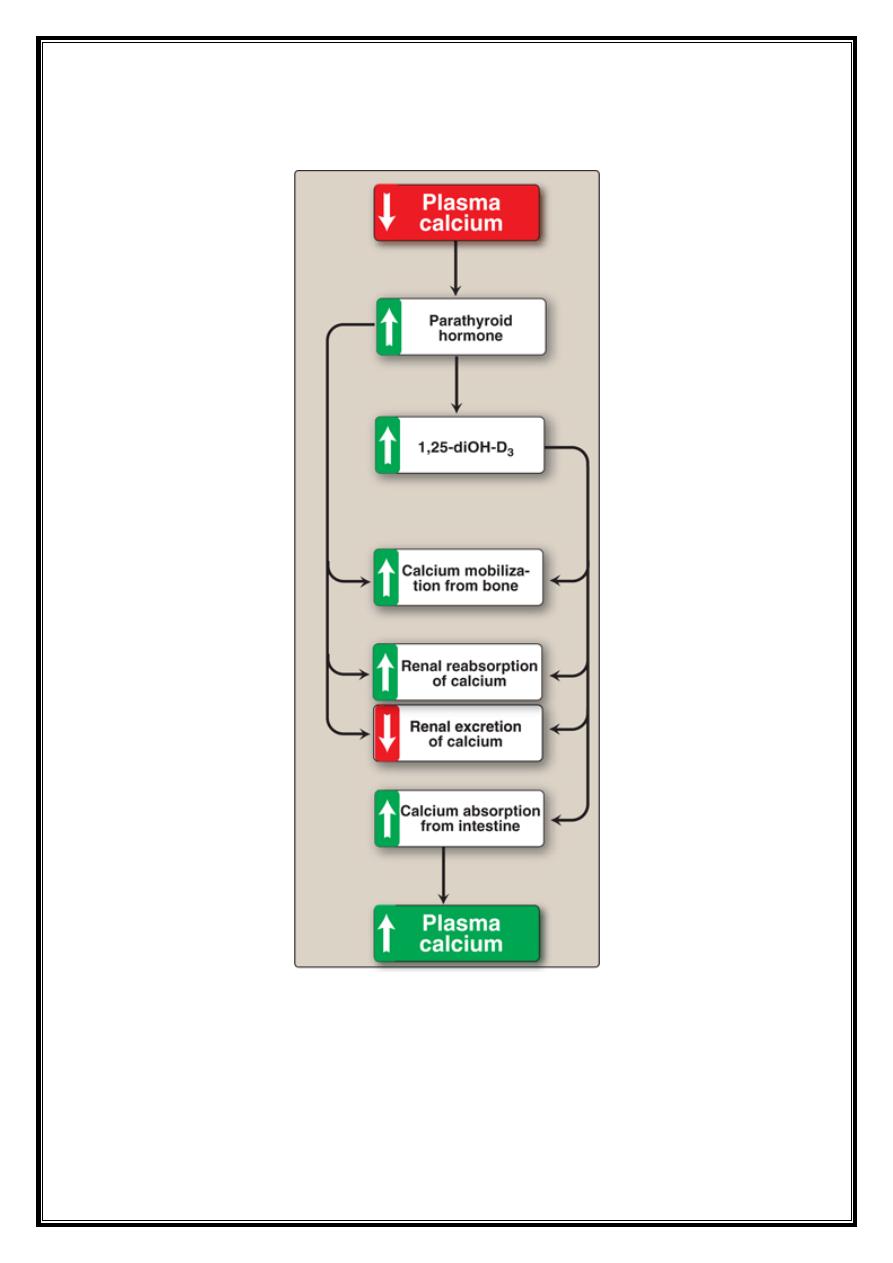
Response to low plasma calcium
8
Function of vitamin D
The overall function of 1,25-diOH-D3 is to maintain adequate plasma
levels of calcium. It performs this function by:
1) increasing uptake of calcium by the intestine,
2) minimizing loss of calcium by the kidney,
3) stimulating resorption of bone when necessary .
Effect of vitamin D on the intestine: 1,25-diOH-D
3
stimulates
intestinal absorption of calcium and phosphate.
Effect of vitamin D on bone: 1,25-diOH-D
3
stimulates the
mobilization of calcium and phosphate from bone by a process that
requires protein synthesis and the presence of PTH. The result is an
increase in plasma calcium and phosphate. Thus, bone is an
important reservoir of calcium that can be mobilized to maintain
plasma levels.
Distribution and requirement of vitamin D
Vitamin D occurs naturally in fatty fish, liver, and egg yolk.
The RDA for adults is 5 mg of cholecalciferol, or 200 international
units (IU) of vitamin D.
Clinical indications
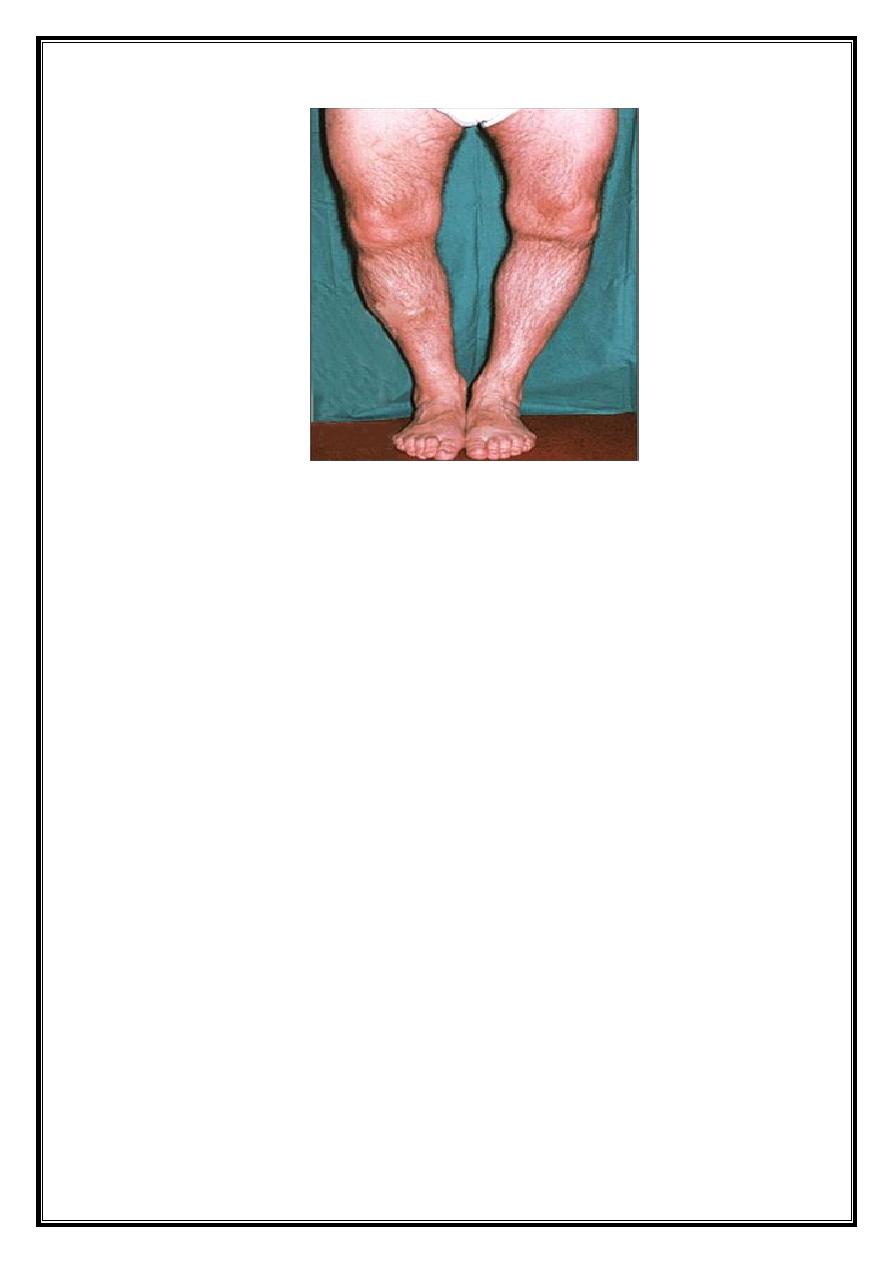
Nutritional rickets: Vitamin D deficiency causes a net
demineralization of bone, resulting in rickets in children and
osteomalacia in adults . Insufficient exposure to daylight and/or
deficiencies in vitamin D consumption occur predominantly in
infants and the elderly. Vitamin D deficiency is more common in
the northern latitudes, because less vitamin D synthesis occurs in
the skin as a result of reduced exposure to ultraviolet light.
9
Renal rickets (renal osteodystrophy): This disorder results from
chronic renal failure and, thus, the decreased ability to form the
active form of the vitamin. 1,25-diOH cholecalciferol (calcitriol)
administration is effective replacement therapy.
Hypoparathyroidism: Lack of parathyroid hormone causes
hypocalcemia and hyperphosphatemia. These patients may be
treated with any form of vitamin D, together with parathyroid
hormone.
Toxicity of vitamin D
Vitamin D is the most toxic of all vitamins. Like all fat-soluble vitamins,
vitamin D can be stored in the body and is only slowly metabolized. High
doses (100,000 IU for weeks or months) can cause loss of appetite,
nausea, thirst, and stupor. Enhanced calcium absorption and bone
resorption results in hypercalcemia, which can lead to deposition of
calcium in many organs, particularly the arteries and kidneys.
10
Vitamin K
The principal role of vitamin K is in the posttranslational modification of
various blood clotting factors, in which it serves as a coenzyme in the
carboxylation of certain glutamic acid residues present in these proteins.
Vitamin K exists in several forms, for example,
a. in plants as phylloquinone (or vitamin K
1
),
b. in intestinal bacterial flora as menaquinone (or vitamin K
2
).
c. For therapy, a synthetic derivative of vitamin K, menadione, is
available.
Function of vitamin K
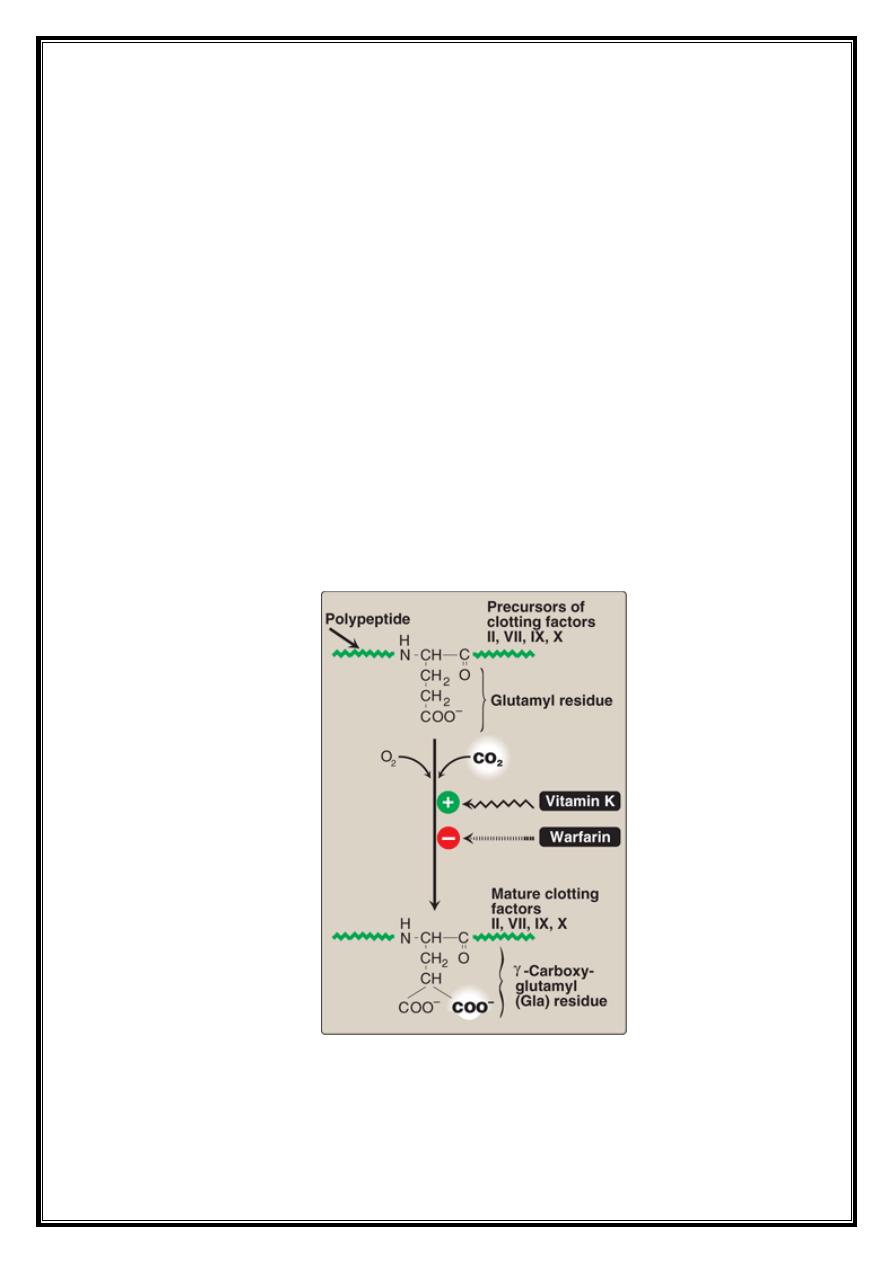
1. Formation of γ-carboxyglutamate (Gla): Vitamin K is required in
the hepatic synthesis of prothrombin and blood clotting factors II,
VII, IX, and X. These proteins are synthesized as inactive
precursor molecules. Formation of the clotting factors requires the
vitamin K–dependent carboxylation of glutamic acid residues
.
Carboxylation of glutamate to form γ-carboxyglutamate (Gla).
11
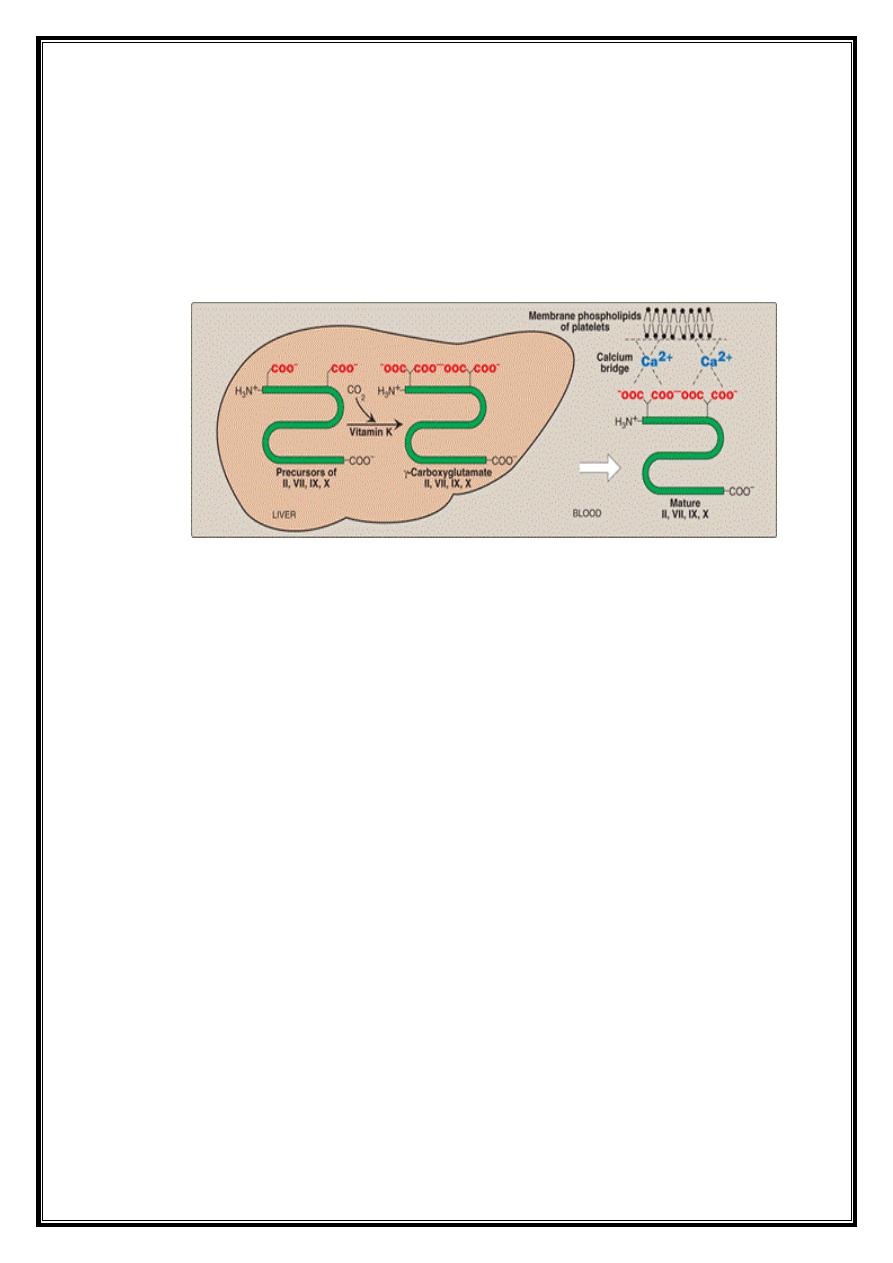
2. Interaction of prothrombin with platelets: The Gla residues of
prothrombin are good chelators of positively charged calcium ions,
The prothrombin–calcium complex is then able to bind to
phospholipids essential for blood clotting on the surface of
platelets. Attachment to the platelet increases the rate at which the
proteolytic conversion of prothrombin to thrombin can occur .
Role of vitamin K in blood coagulation
3. Role of Gla residues in other proteins: Gla is also present in other
proteins (for example, osteocalcin of bone, and in proteins involved
in the degradation of blood clots).
Distribution and requirement of vitamin K
Vitamin K is found in cabbage, cauliflower, spinach, egg yolk, and liver.
There is also extensive synthesis of the vitamin by the bacteria in the gut.
Clinical indications
Deficiency of vitamin K:
A true vitamin K deficiency is unusual because adequate amounts are
generally produced by intestinal bacteria or obtained from the diet. If the
bacterial population in the gut is decreased, for example, by antibiotics,
the amount of endogenously formed vitamin is depressed, and this can
lead to hypoprothrombinemia in the marginally malnourished individual,
for example, a debilitated geriatric patient. This condition may require
supplementation with vitamin K to correct the bleeding tendency.
12
Deficiency of vitamin K in the newborn:
Newborns have sterile intestines and so initially lack the bacteria that
synthesize vitamin K. Because human milk provides only about one fifth
of the daily requirement for vitamin K, it is recommended that all
newborns receive a single intramuscular dose of vitamin K as prophylaxis
against hemorrhagic disease.
Toxicity of vitamin K
Prolonged administration of large doses of vitamin K can produce
hemolytic anemia and jaundice in the infant, due to toxic effects on the
membrane of red blood cells.
Vitamin E
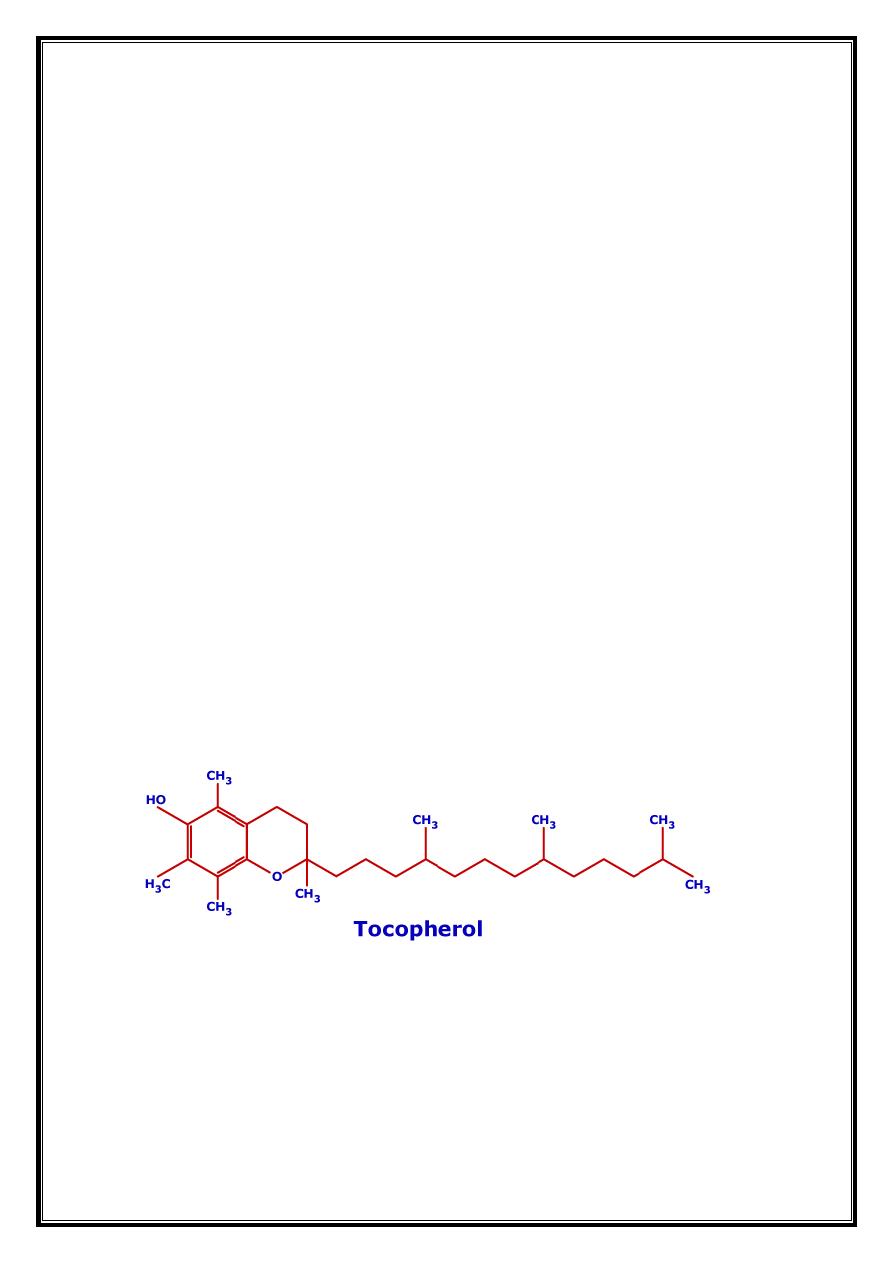
The E vitamins consist of eight naturally occurring tocopherols, of which
α-tocopherol is the most active. The primary function of vitamin E is as
an antioxidant in prevention of the nonenzymic oxidation of cell
components, for example, polyunsaturated fatty acids, by molecular
oxygen and free radicals.
Distribution and requirements of vitamin E
Vegetable oils are rich sources of vitamin E, whereas liver and eggs
contain moderate amounts. The RDA for α-tocopherol is 10 mg for men
and 8 mg for women.
13
Deficiency of vitamin E
Vitamin E deficiency is almost entirely restricted to premature infants.
When observed in adults, it is usually associated with defective lipid
absorption or transport. The signs of human vitamin E deficiency include
sensitivity of erythrocytes to peroxide, and the appearance of abnormal
cellular membranes.
Clinical indications
Vitamin E is not recommended for the prevention of chronic disease,
such as coronary heart disease or cancer. Clinical trials using vitamin E
supplementation have been uniformly disappointing. For example,
subjects in the Alpha-Tocopherol, Beta-Carotene Cancer Prevention
Study trial who received high doses of vitamin E not only lacked
cardiovascular benefit but also had an increased incidence of stroke.
Toxicity of vitamin E
Vitamin E is the least toxic of the fat-soluble vitamins, and no toxicity
has been observed at doses of 300 mg/day.
Populations consuming diets high in fruits and vegetables show decreased
incidence of some chronic diseases. However, clinical trials have failed to
show a definitive benefit from supplements of vitamins A, C, or E;
multivitamins with folic acid; or antioxidant combinations for the
prevention of cancer or cardiovascular disease.
