
Clinical pharmacology
Dr. Hussain Addai aljabery
M.B.Ch.B M.Sc. ( Pharma.)
D.M.R.D F.I.B..M.C ( Radio)
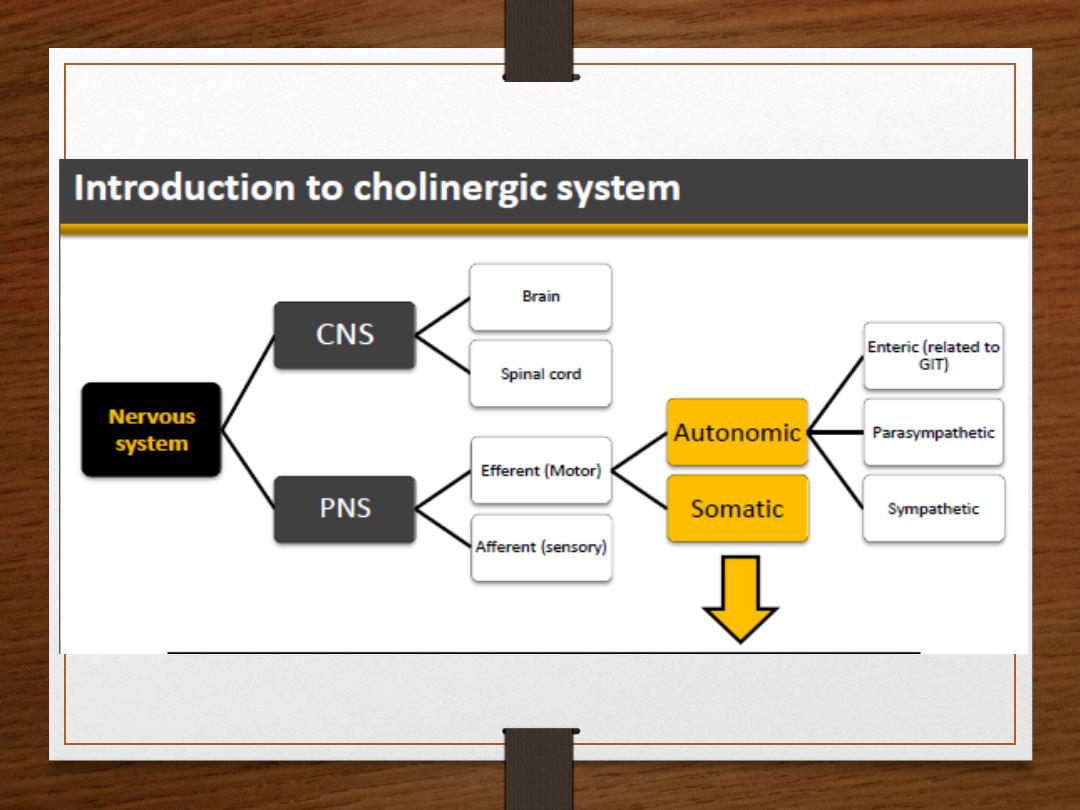
autonomic
PHARMACOLOGY
(cholinergic agonists-
parasympathomimetic )
Direct -acting cholinergic agonists OBJECTIVE:
•To identify the mechanism of action of direct acting acetylcholine receptor stimulants
•To discuss the pharmacokinetic aspects and pharmacodynamics effects of direct
cholinomimetics
•To outline the therapeutic uses and toxicity of direct cholinergic agonists
•
Indirect -acting cholinergic agonists OBJECTIVES:
•
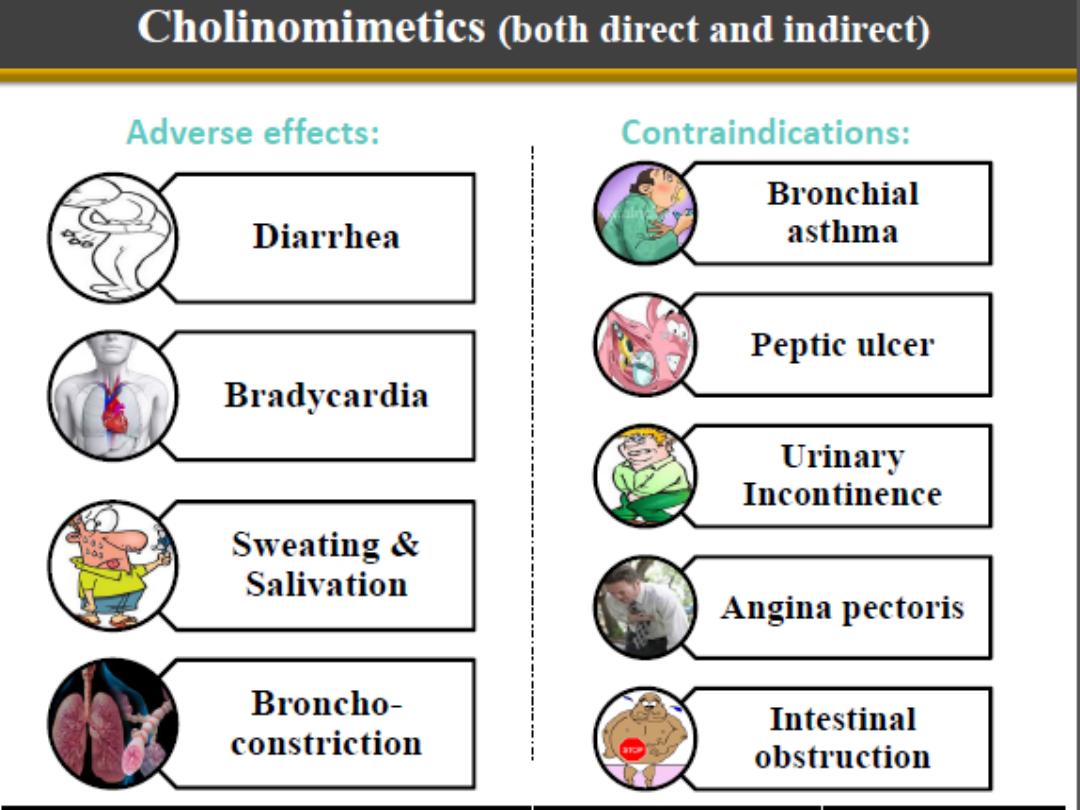
•Classification of indirect acting cholinomimetics
•
• Mechanism of action, kinetics, dynamics and uses of anticholinesterases
•
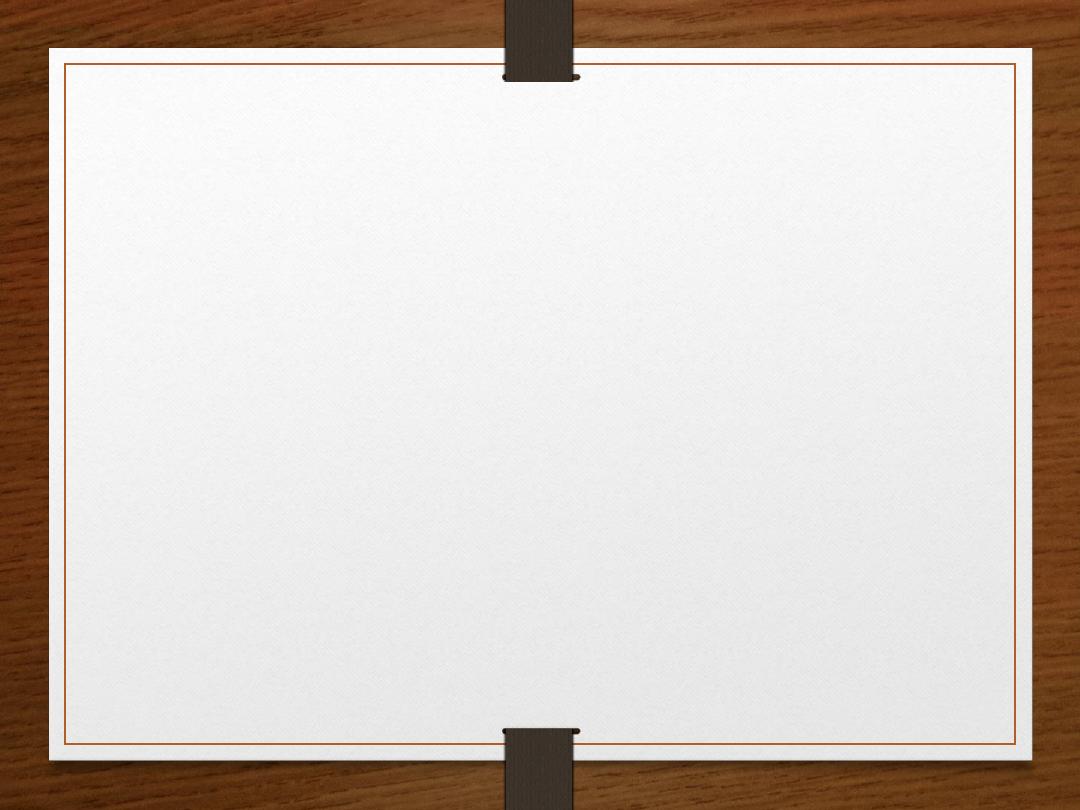
• Adverse effects & contraindications of anticholinesterases
•
• Symptoms and treatment of organophosphates toxicity.
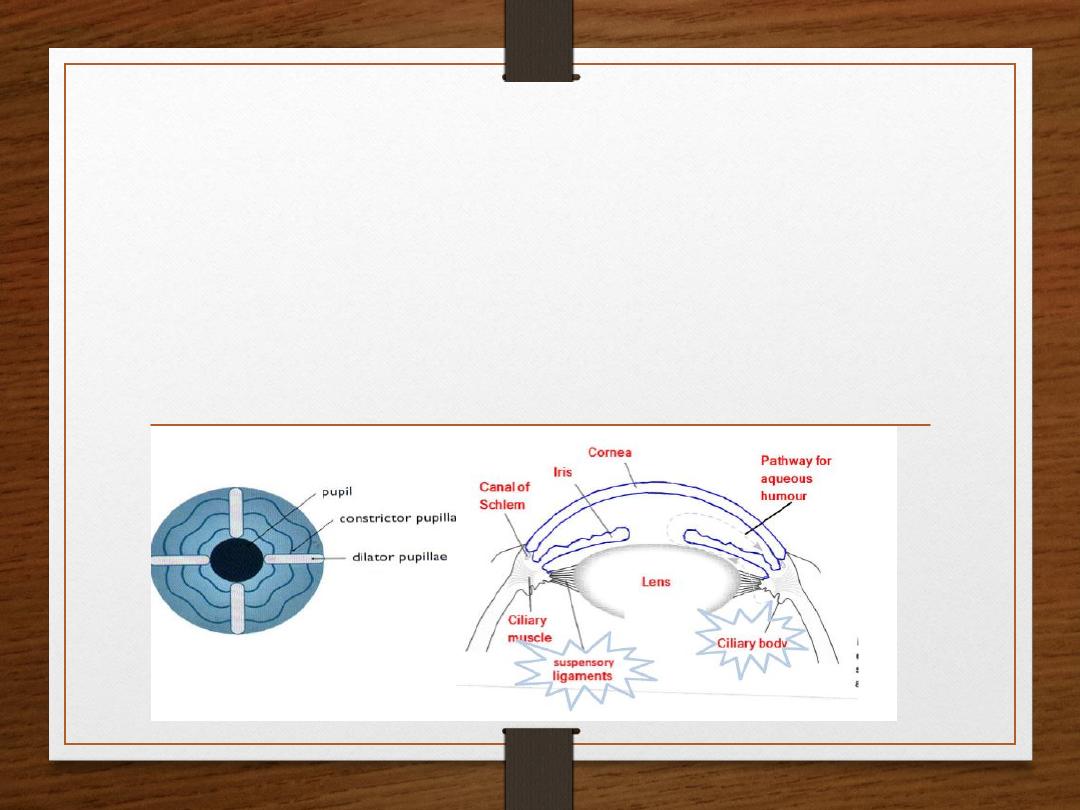
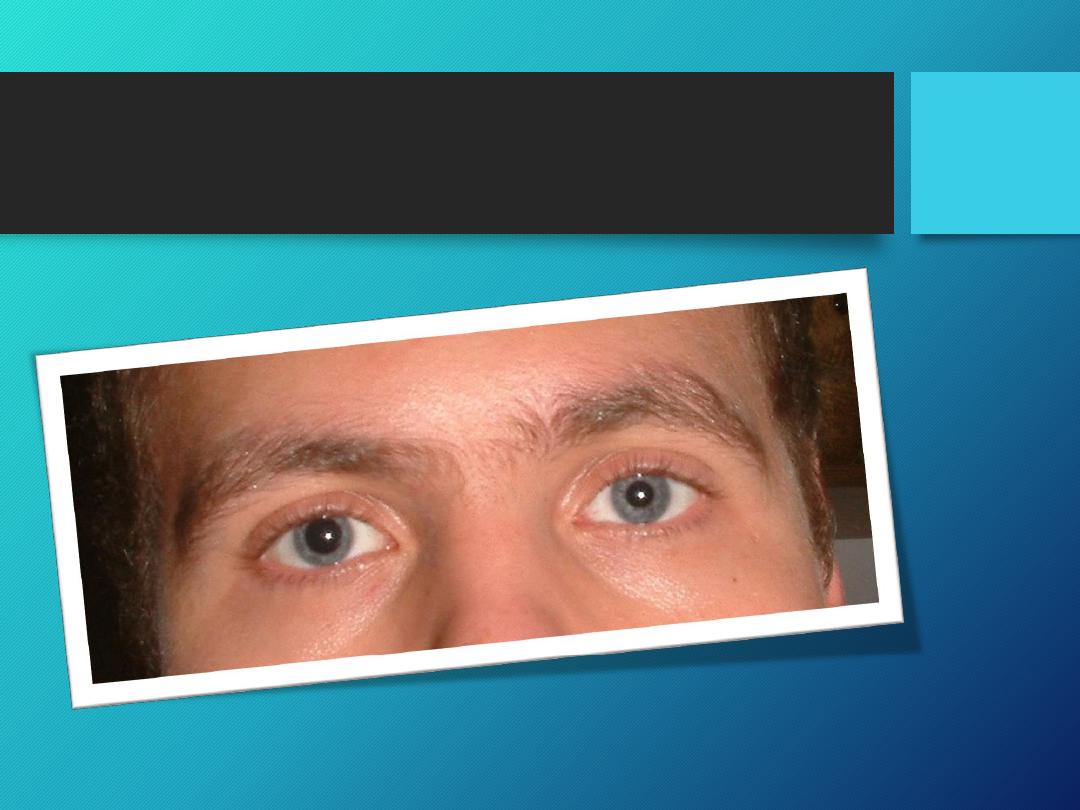
The iris has two muscles that control light intensity:
1. Dilator pupillae, a longitudinal radial muscle which dilates the pupil
(mydriasis) in the dark, to allow as much as possible of light to enter the
eye. It is innervated by sympathetic NS.
2. Constrictor pupillae, a circular muscle which constricts the pupil
(miosis)in places with good lighting.
It is innervated by parasympathetic NS.
Accommodating the ciliary muscle for near vision:
• Parasympathetic activation contracts
the ciliary muscle
.
( when ACh
combines with muscarinic M3 receptor).
• Contraction of ciliary muscle pulls the ciliary body forward & inward ,
relaxing the suspensory ligaments of the lens (lens becomes spherical).
(Contraction of ciliary body = relaxation of the suspensory ligaments , and vice versa).
• The lens bulges more (increased curvature) , this causes a decrease in focal
length.
• This parasympathetic reflex is essential to accommodate for
near vision
.
Constrictor pupillae is important for:
1- Adjusting the pupil in response to change
in light intensity. 2- Regulating the intraocular
pressure.
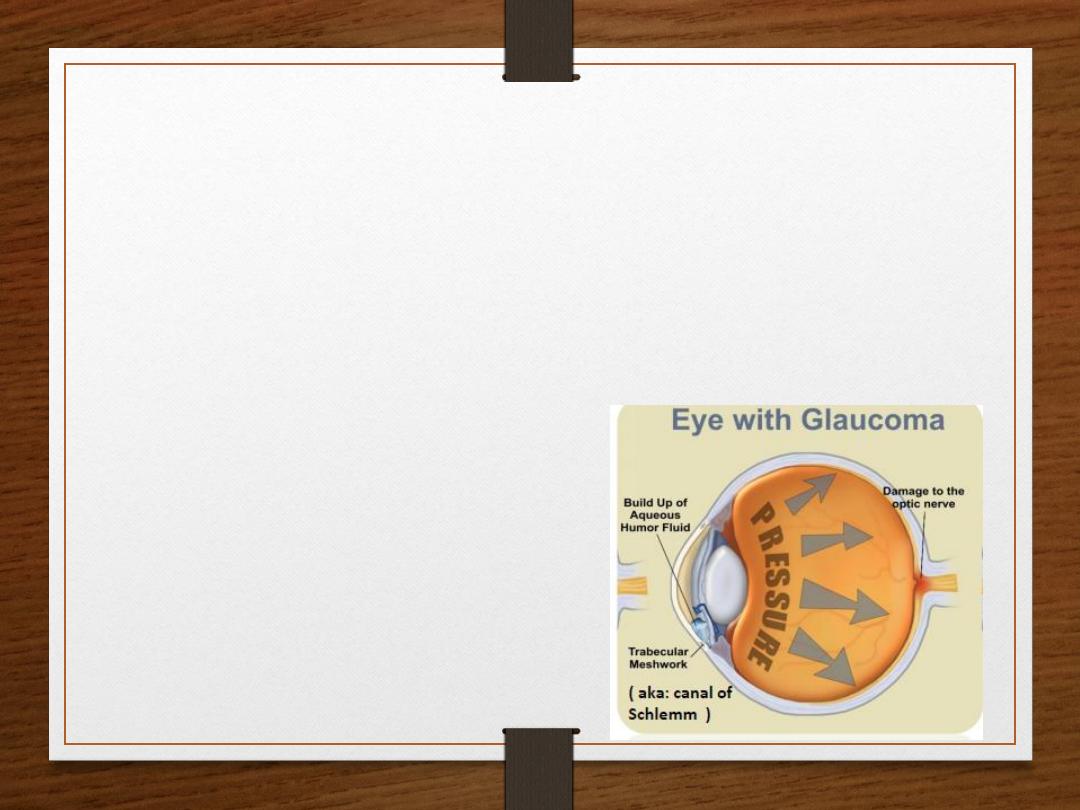
Regulating the intraocular pressure: In the healthy eye:
•Aqueous humour is secreted by the cells of the epithelium
covering the ciliary body.
•Increased tension in the ciliary body removes the Aqueous
humour continuously by drainage into the canal of Schlemm.
•Normal intraocular pressure is 10-15mmHg above atmospheric
pressure.
In some people:
•Dilatation of their pupil will block canal of schlemm, therefore
it impeds drainage of aqueous humour.
•The accumulation of aqueous humour leads to an increase in
intraocular pressure.
• increase IOP may lead to glaucoma, and retinal detachment.
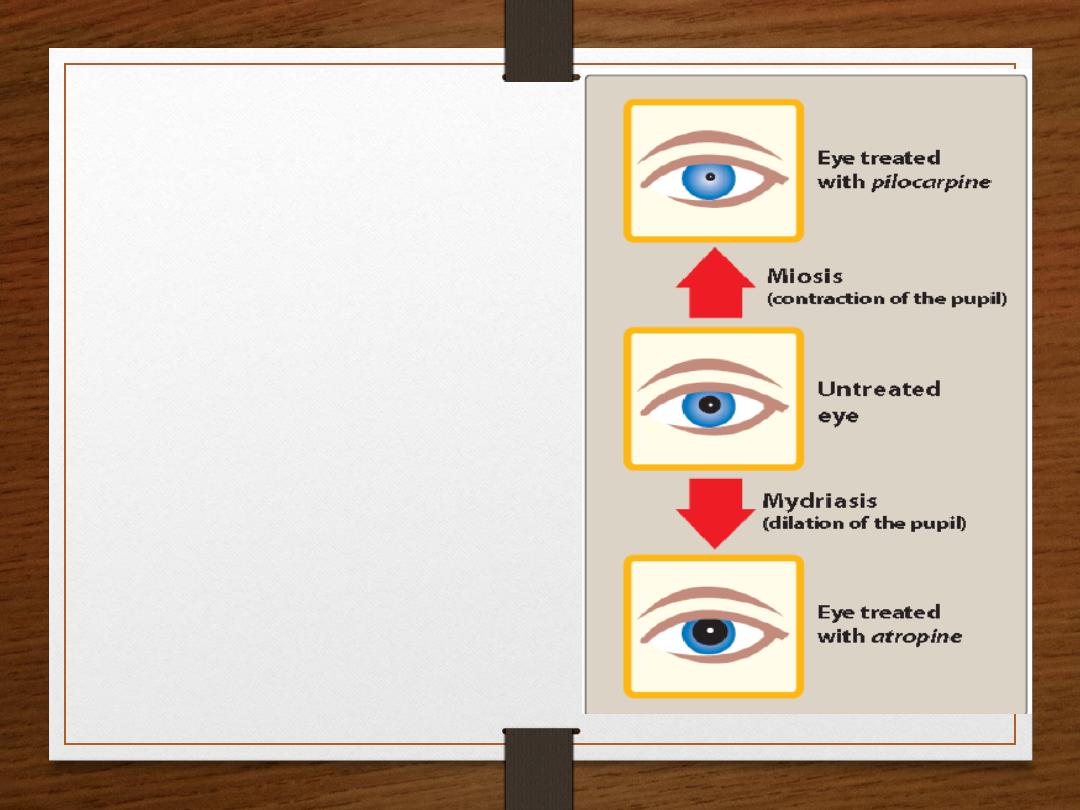
Treatment:
When using cholinergic drugs
(e.g.
pilocarpine
), constrictor pupillae
causes miosis, which contracts the pupil
away from canal of schlemm, leading to
increased filtration of
Aqueous humour.
Thus,
activation of constrictor pupillae
decreases intraocular pressure in patients
with glaucoma.
Overview:
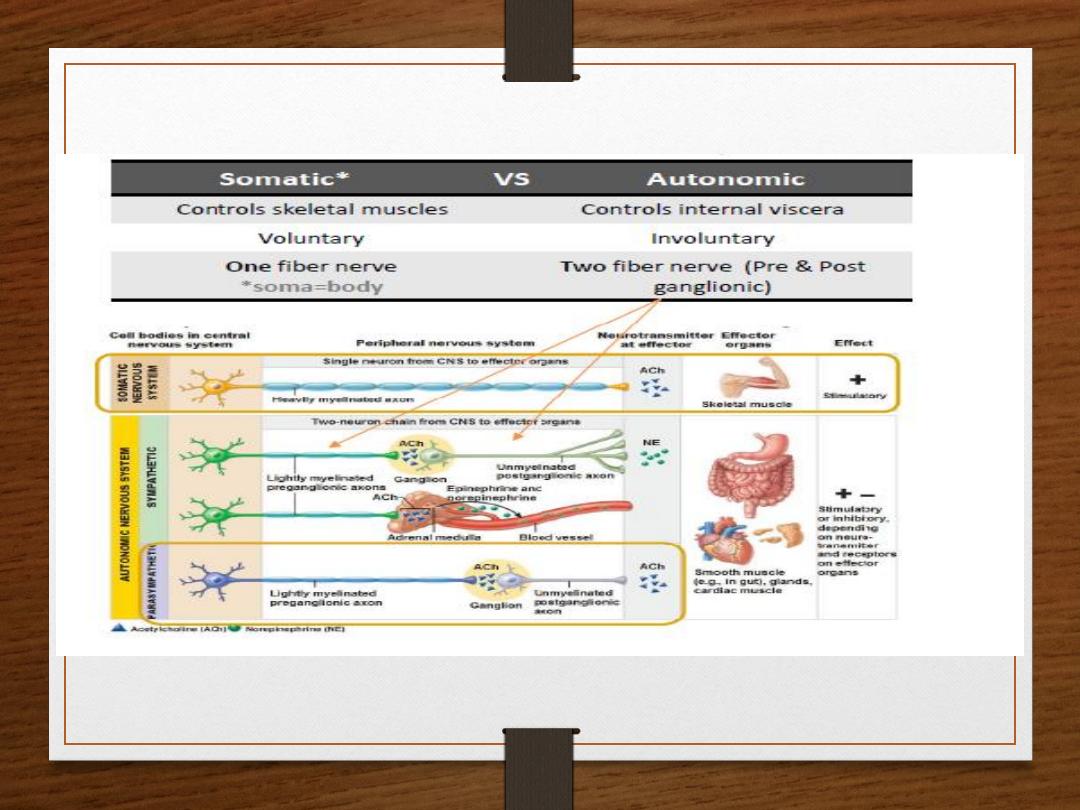
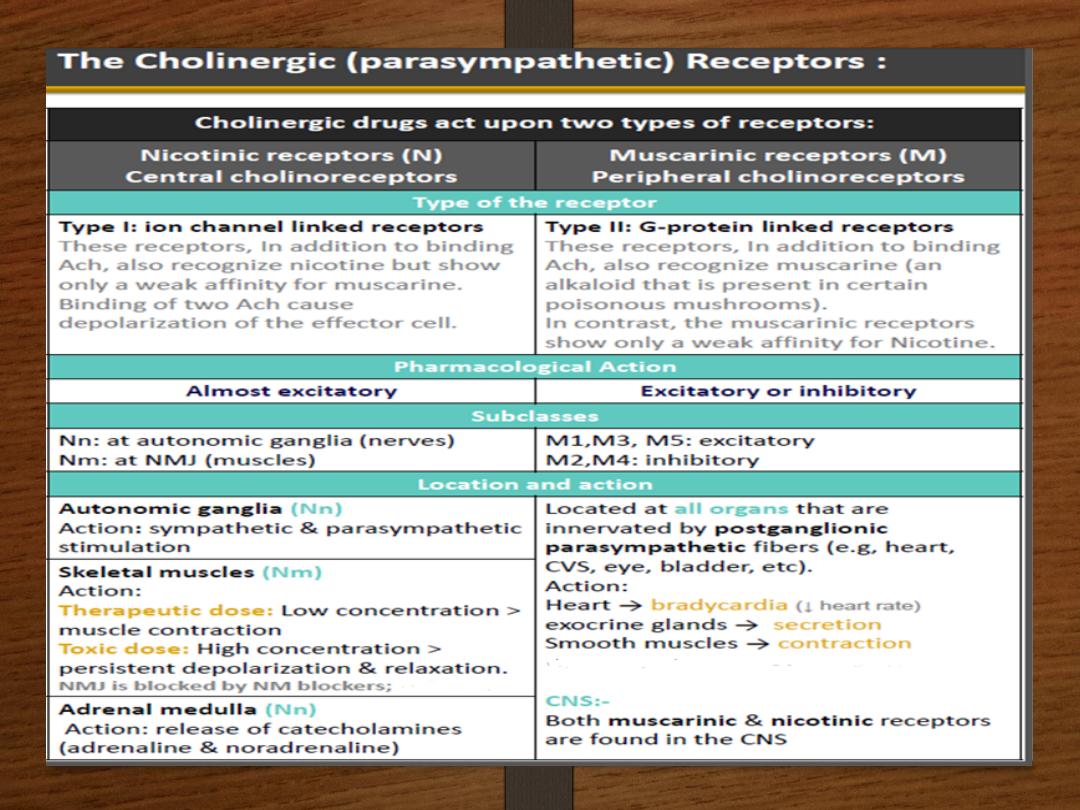
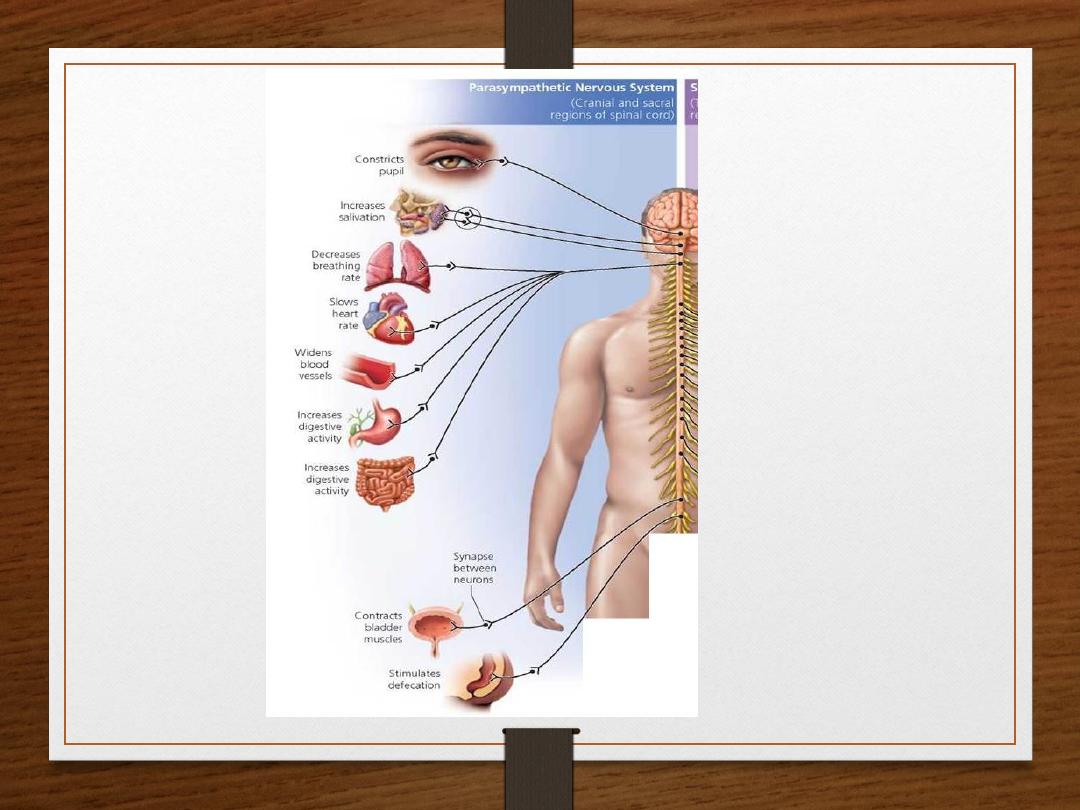
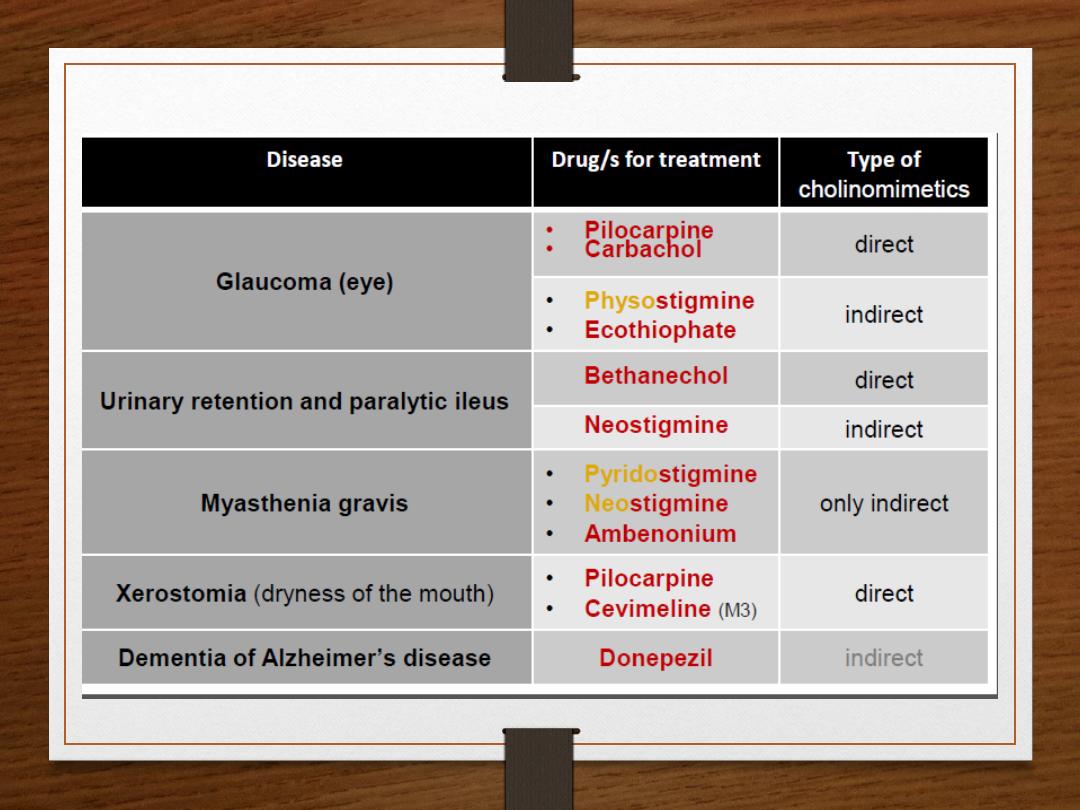
Drugs that affect the ANS are divided into two groups:
1. Cholinergic Drugs which act on muscarinic and nicotinic receptors that are
activated by Ach. (parasympathetic)
2.Adrenergic Drugs which act on adrenergic alpha and beta receptors that are
activated by Norepinephrine or epinephrine. (sympathetic)
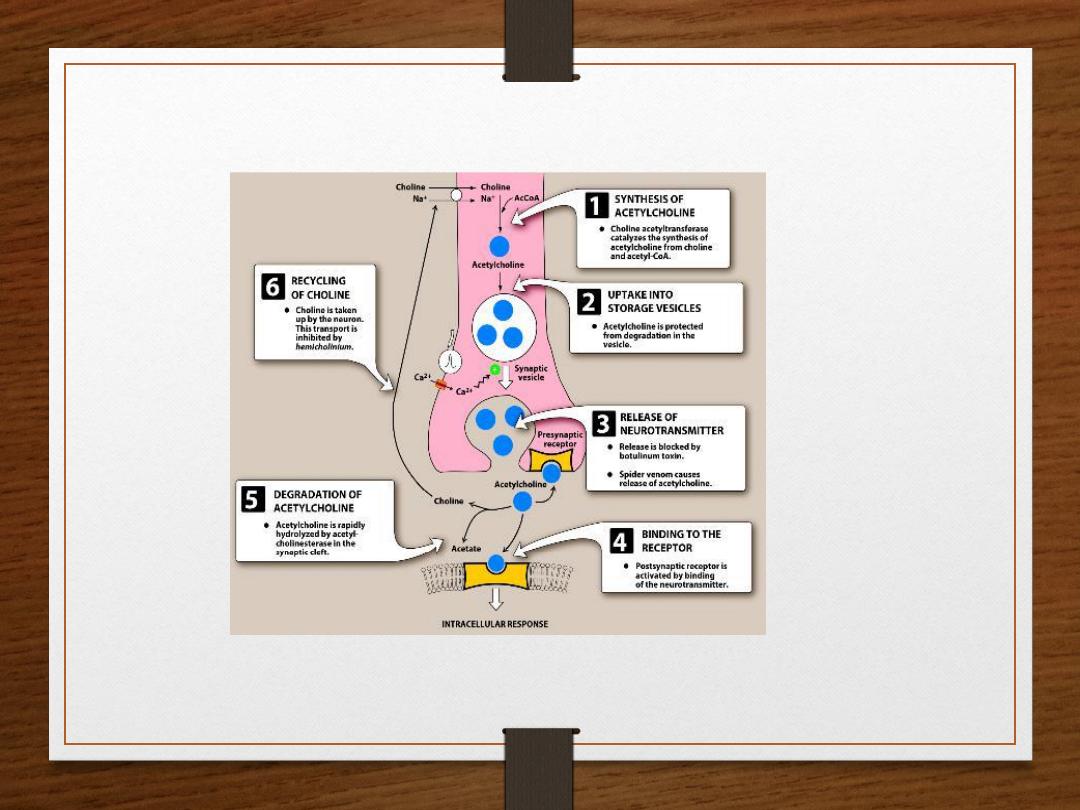
❖The Cholinergic Neuron:
•The neurotransmitter in parasympathetic nervous system (cholinergic system) is
Acetylcholine, and nerves are called cholinergic nerves.
•Neurotransmission at Cholinergic Neurons involves six steps:
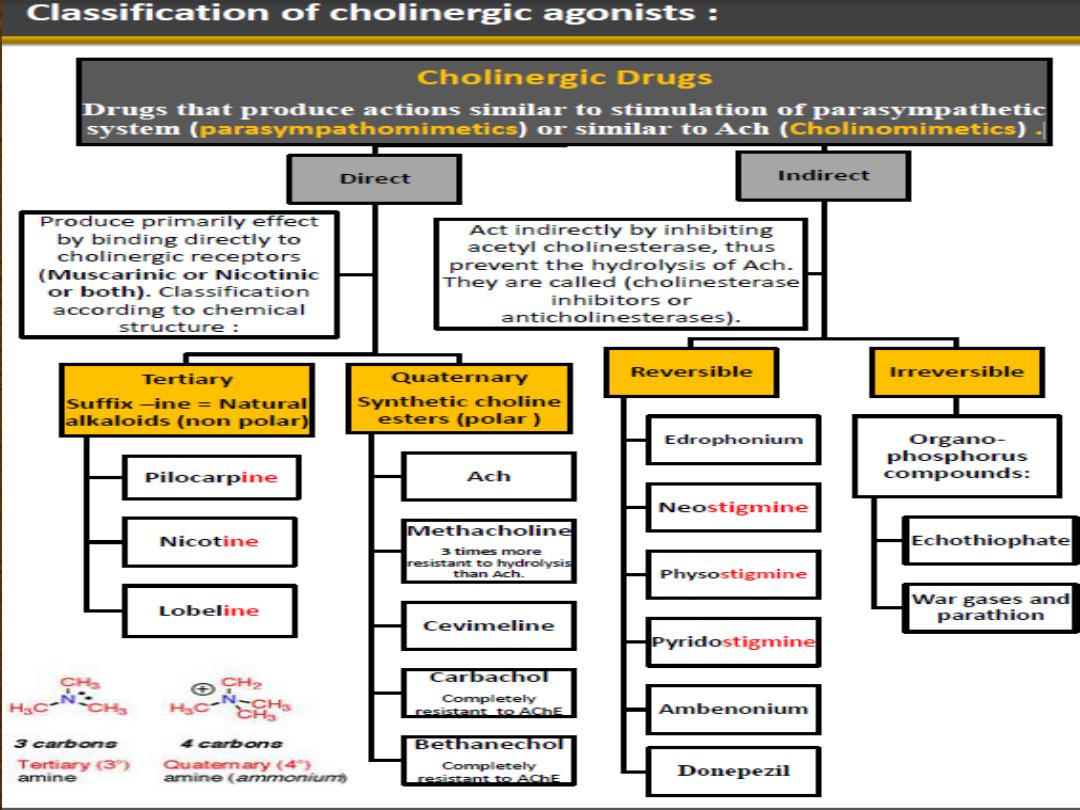
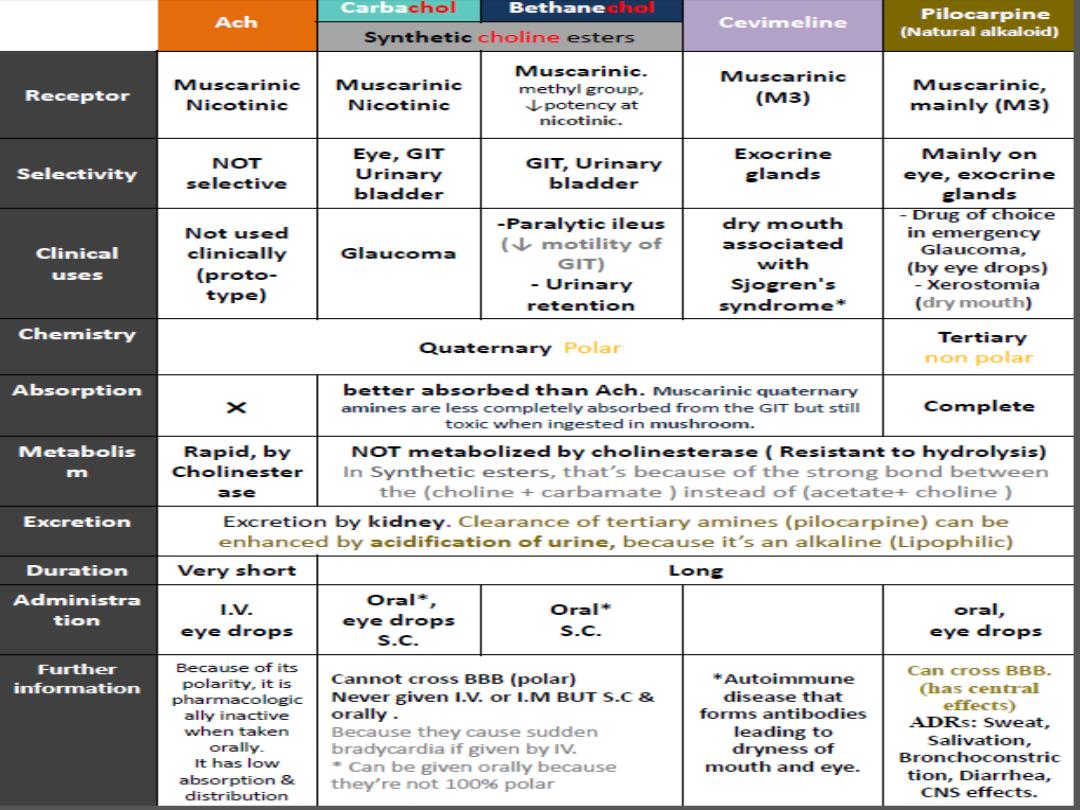
Cholinergic Agonist
•
Acetylcholine
•
Fates
•
Easily hydrolysed in stomach (acid catalysed
hydrolysis)
•
Easily hydrolysed in blood (esterases)
•
No selectivity between receptor types
•
No selectivity between different target organs
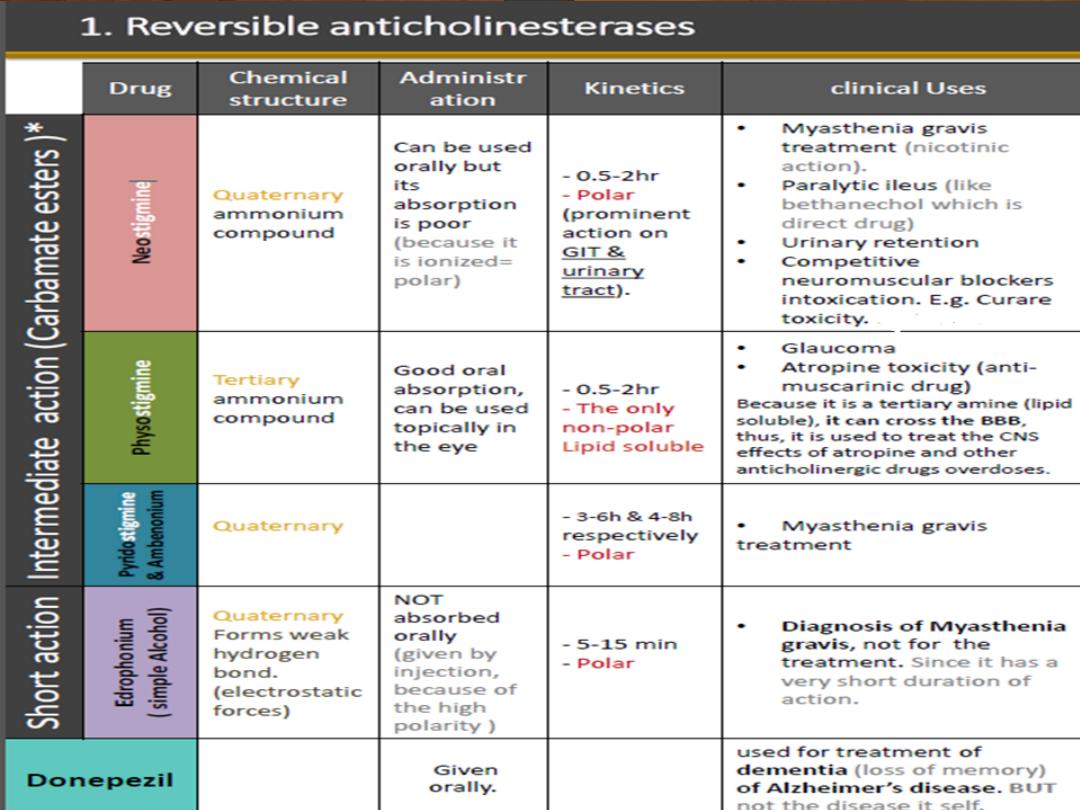
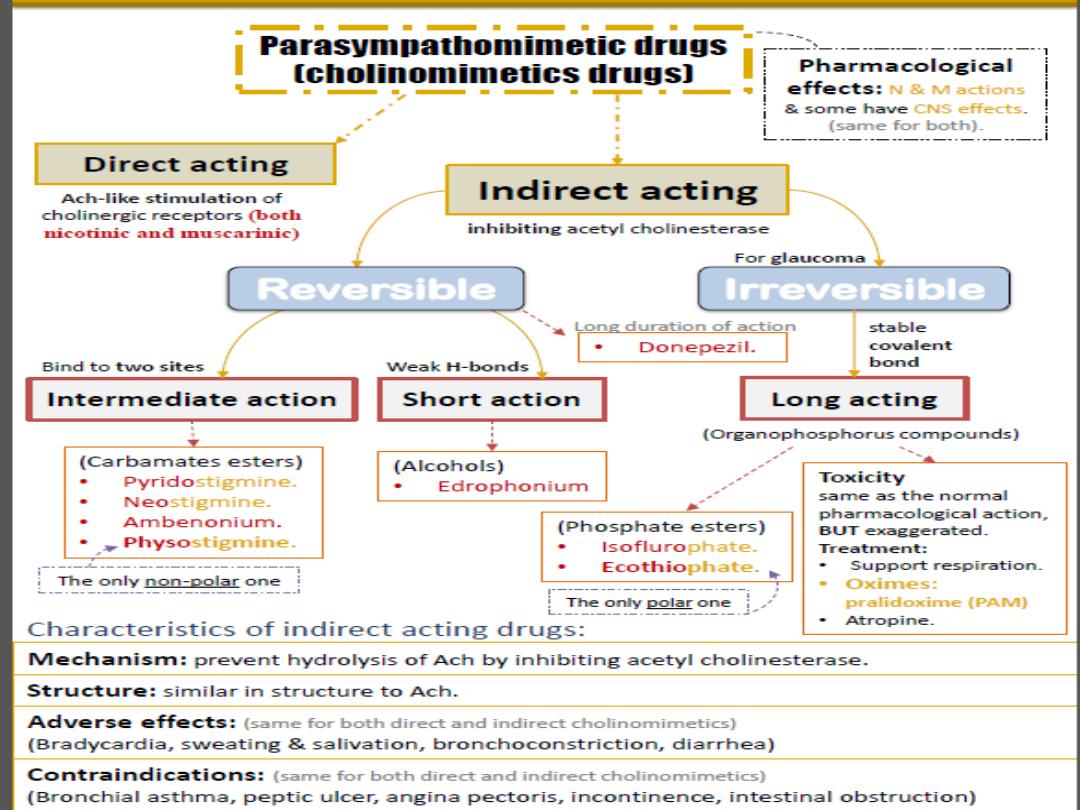
Indirect Cholinomimetics
(Anticholinesterases)
•
Mechanism of action: Anticholinesterases prevent
hydrolysis of Ach by inhibiting acetyl cholinesterase
(inhibit the inhibitor). Those drugs inhibit cholinesterase
by tricking it and combining with it instead of Ach, since
they have similar structure. (any inhibiter for an enzyme
must be similar in structure as the enzyme’s substrate. E.g.
Ach). Thus, they increase Ach concentrations and prolong
its actions at the cholinergic receptors (weather nicotinic or
muscarinic, since they acts on the enzyme present at the
synaptic cleft of both of them).
Pharmacological effects:
•
All Anticholinesterases have muscarinic and nicotinic
actions (N & M actions) , only lipid soluble drugs have
CNS effects which can happened centrally and
peripherally (excitation, convulsion, respiratory failure,
coma). e.g. physostigmine & phosphate ester (except
echothiophate that is polar). Remember: Both direct
and indirect cholinomimetics have pharmacological
actions similar to Ach . (e.g. miosis, bradycardia,
bronchoconstriction, increased motility, secretion of
exocrine glands).
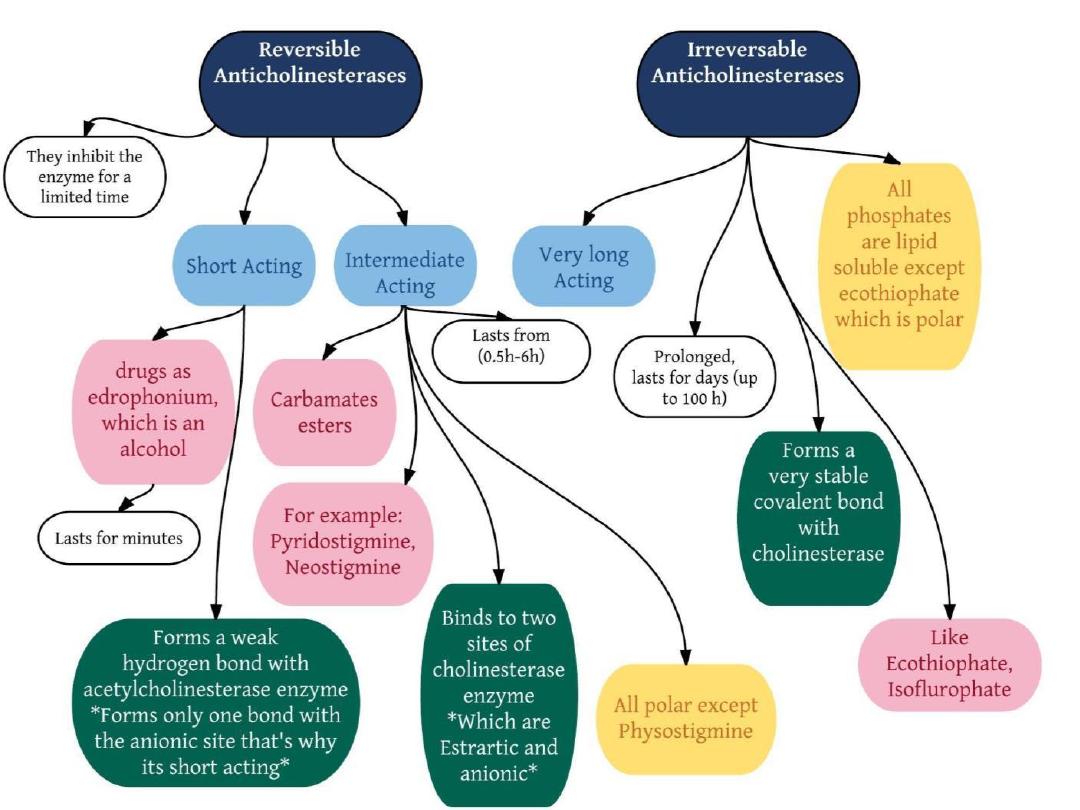
Irreversible anticholinesterases (Long acting)
Organophosphorus compounds E.g. Ecothiophate
Mechanism of action:
•Binds to cholinesterase by strong covalent bond.
•Thus, Hydrolysis by AChE is very slow ‘100 hours’
•Thus, Has a long duration of action.
•Aging* makes bond extremely stable.
•All are highly lipid soluble except ecothiophate.
•well absorbed from the skin, lung, gut & conjunctiva except
ecothiophate (less stable in aqueous solution)
•Used only to treat glaucoma**
* Aging: Long time exposure to organophosphates makes the covalent bond
between the drug and the enzyme stronger. So when a patient is exposed to
it in war gases or insecticide it’s hard to treat him because it’s both
irreversible and time dependent. They can be absorbed through skin,
therefore it is common for farmers to get intoxicated while spraying
insecticides bare footed and without precaution. ** Used rarely due to
adverse effects.. But used safely in glaucoma because it has local effect
when applied by eye drops.
Symptoms of Organophosphates toxicity:
•
intoxication symptoms are the same as the normal
pharmacological actions, BUT exaggerated or in excess amount
•
Severe bradycardia, hypotension.
•
Bronchospasm.
•
Increase GIT motility. Cramps & diarrhea.
•
CNS effects. Cross BBB, because it’s lipid soluble.( Convulsion
,coma & respiratory failure.)
•
Initial twitching of skeletal muscles. Depolarization block
Muscle weakness & paralysis
Treatment of organophosphate toxicity
❖Support respiration.
Since they cause bronchospasm, First and most important
step -before introducing any drug to the patient- is to control the patient’s
airway and provide him with adequate oxygen by artificial respiration.
❖Atropine (to block muscarinic actions & CNS effects).
Atropine has apposing
effects of cholinomimetics.
❖Cholinesterase reactivators
(Oximes
e.g.:
pralidoxime (PAM)
)
• First choice & most effective drugs.
•Acts by regeneration (Re-Activation) of recently inhibited cholinesterase
enzyme, if given before aging.
By doing so, they reduce Ach effects.
Uses:
I.V →
over 15-30 min for organophosphate intoxication (poisoning).
Thanks
