1
Course: Medical Microbiology
Lecturer: Dr. Weam Saad
Subject: Medical Bacteriology
Bacterial Pathogenesis
Pathogen is a microorganism that is able to produce pathology.
Pathogenicity is the ability of a microorganism to cause disease in the
host for the pathogen, pathogenicity is a manifestation of a host- parasite
interaction.
Obligate pathogenic bacteria: bacteria that live only in host and cause
diseases.
Opportunistic Pathogens Bacteria which cause a disease in the immune-
compromised such as normal flora; Staphylococcus aureus and E. coli can
cause an opportunistic infection.
Determinants of Virulence: the weapons or characteristics that
pathogenic bacteria utilize to produce disease, e.g. toxins, capsules,
enzymes …etc.
Pathogenic Bacteria Virulence Factors
1. Bacterial Adherence and Colonization Factors (Surface Antigens):
Bacterial adherence to portal of entry like: Mucosal Surfaces or attachment
to a eukaryotic cell or tissue surface requires two factors: a receptor and an
adhesin. The receptors are specific carbohydrate or peptide residues on the
eukaryotic cell surface (A complementary molecular binding site on a
surface that binds specific adhesins). The bacterial adhesin is typically a
component of the bacterial cell surface which interacts with the host cell
receptor.
Some adhesins are able to act as antigens and induce specific immune
response against them. And some are used during infections diagnosis like
flagellar H Ag of Salmonella typhi. The following table contains the types
2
of adherence factors are used by pathogenic bacteria for adherence to
surfaces or tissues:
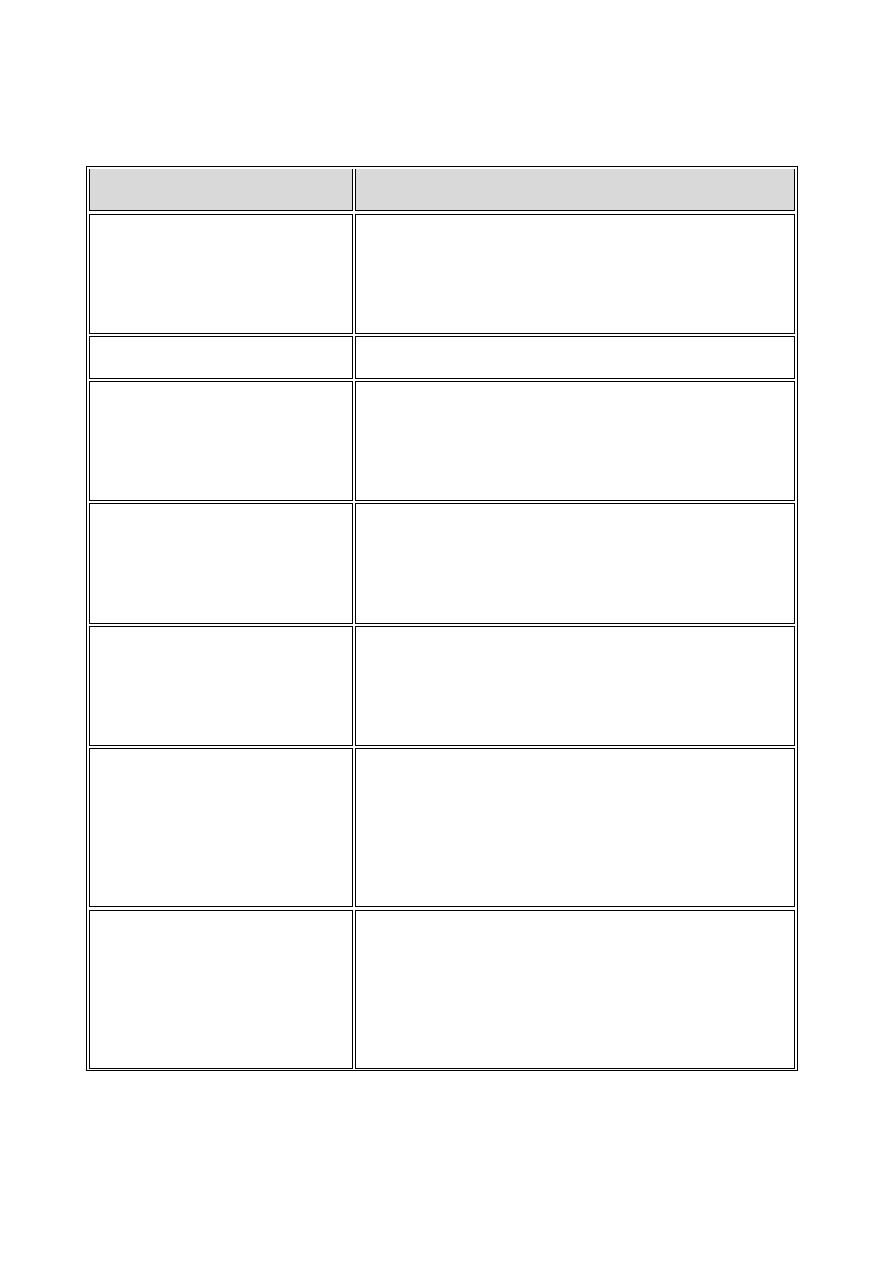
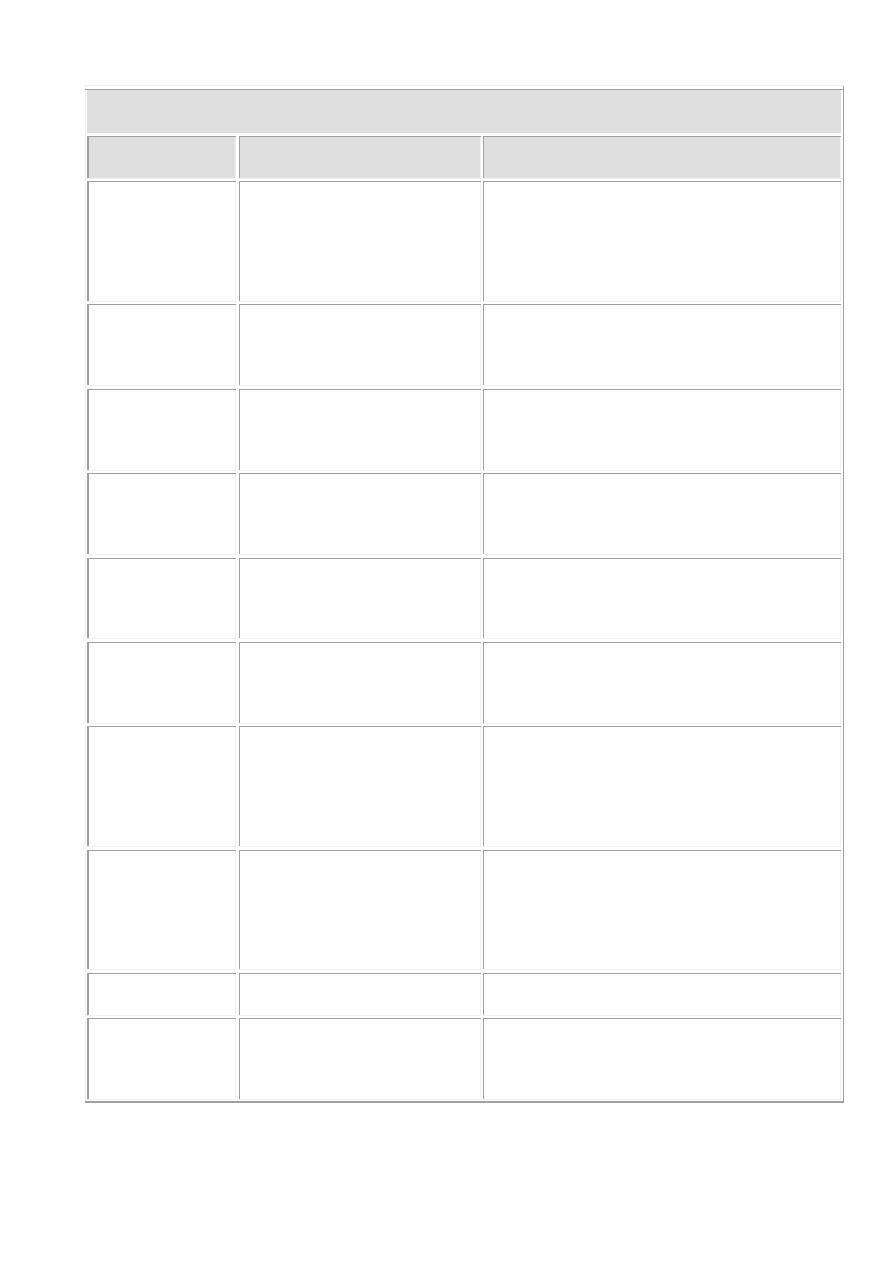
Adherence Factor
Role associated with virulence
1. Fimbriae
Filamentous proteins on the surface of bacterial
cells that may behave as adhesins for specific
adherence
2. Common pili
Same as fimbriae
3. Sex pilus
A specialized pilus that binds mating
procaryotes together for the purpose of DNA
transfer
4. Type 1 fimbriae
Fimbriae in Enterobacteriaceae which bind
specifically to mannose terminated
glycoproteins on eukaryotic cell surfaces
5. Glycocalyx
A layer of exopolysaccharide fibers on the
surface of bacterial cells which may be involved
in adherence to a surface
6. Capsule
A detectable layer of polysaccharide (rarely
polypeptide) on the surface of a bacterial cell
which may mediate specific or nonspecific
attachment
7. Lipopolysaccharide
(LPS)
A distinct cell wall component of the outer
membrane of Gram-negative bacteria with the
potential structural diversity to mediate specific
adherence. Probably functions as an adhesion
3
8. Teichoic acids and
lipoteichoic acids
(LTA)
Cell wall components of Gram-positive bacteria
that may be involved in nonspecific or specific
adherence
9. Biofilm formation
Formation of slimy extracellular matrix
(polysaccharides) produced by some bacteria
for colonization, avoid phagocytosis and resist
antibiotics.
Factors affect adherence:
1) Tissue tropism: some bacteria prefer certain tissues e.g. Streptococcus
mutans is usually found in dental plaques and not on epithelial surfaces of
the tongue.
2) Species specificity: some pathogenic bacteria infect only certain species,
e.g. Neisseria gonorrhoeae infections are limited to humans.
3) Genetic susceptibility: some races are genetically immunized to a
pathogenic bacteria.
2. Bacterial Invasion Factors:
Invasins are proteins that act locally to damage host cells and facilitating the
growth and spread of the pathogen. The damage (break down) to the host as a
result of this invasive activity is a major part of the pathology of an infectious
disease. Also, these invasins can stop immune response activity against the
pathogenic bacteria.
Some bacteria have the ability to survive and multiply inside phagocytic
cells. This ability is considered an important virulence factor and escape
mechanism from the specific immune response. For example: Mycobacterium
tuberculosis, Legionella
pneumophila,
Brucella
abortus,
and Listeria
monocytogenes can remain alive inside phagocytes.

4
Types of Invasins:
1. Spreading Factors (Enzymes)
They are bacterial enzymes that affect the physical properties of tissue matrices
and intercellular spaces, they help in the spread of the pathogen.
1) Hyaluronidase.
It is the original spreading factor produced by Streptococci, Staphylococci, and
Clostridia. The enzyme attacks the interstitial cement (ground substance) of
connective tissue (hyaluronic acid).
2) Collagenase
It is produced by Clostridium perfringens. It breaks down collagen of muscles
and cause gas gangrene.
3) Neuraminidase
It is produced by intestinal pathogens such as Vibrio cholerae and Shigella
dysenteriae. It breaks neuraminic acid the intercellular cement of the epithelial
cells of the intestinal mucosa.
4) Streptokinase and Staphylokinase
They are produced by streptococci and staphylococci. These Kinase enzymes
convert plasminogen to plasmin which digests fibrin and prevents clotting of
the blood. The absence of fibrin in spreading bacterial lesions allows more rapid
diffusion of the infectious bacteria.
5) Enzymes that Cause Hemolysis and/or Leucolysis
These enzymes usually act on the animal cell membrane by forming a pore that
results in cell lysis through enzymatic attack on phospholipids.sometmes thay
are called lecithinases or phospholipases, and if they lyse red blood cells they
are sometimes called hemolysins. Leukocidins, produced by staphylococci and
streptolysin produced by streptococci specifically lyse phagocytes and their
granules (these enzymes are also considered as bacterial exotoxins).

5
6) Phospholipases
They are produced by Clostridium perfringens (i.e., alpha toxin), cause lysis of
phospholipids in cell membranes.
7) Lecithinases
They also produced by Clostridium perfringens, able to destroy lecithin
(phosphatidylcholine) in cell membranes.
8) Hemolysins
They are produced by staphylococci (i.e., alpha toxin), streptococci
(i.e.,streptolysin) and many clostridia, may be channel-forming proteins or
phospholipases or lecithinases that destroy red blood cells and other cells (i.e.,
phagocytes) by lysis.
9) Staphylococcal coagulase
Coagulase, formed by Staphylococcus aureus, it is an enzyme that converts
fibrinogen to fibrin which causes clotting. Coagulase activity is associated with
pathogenic S. aureus and never produced by S. epidermidis. The action of
coagulase is to provide an antigenic disguise if it clotted fibrin on the cell
surface.
10) Extracellular Digestive Enzymes
Heterotrophic bacteria produce a wide variety of extracellular enzymes
including proteases, lipases, nucleases, etc., which have a role in invasion or
pathogenesis. These enzymes have other functions more than bacterial nutrition
or metabolism and help in invasion either directly or indirectly.
2. Toxins:
They are bacterial products that promote bacterial invasion, Toxigenesis is
the ability to produce toxins. Toxic substances, both soluble and cell-associated,
may be transported by blood and lymph and cause cytotoxic effects at tissue
sites remote from the original point of invasion or growth. There are two types
of these toxins:
6
A. Endotoxins
Endotoxin is the LPS layer of Gram-negative bacteria. Endotoxin biological
effects on the host may be lethal because it is released after lysis of bacteria
causing toxic effects include pyrogenicity, leukopenia followed by leukocytosis,
complement activation (alternative pathway), depression in blood pressure
(hypotension), mitogenicity, induction of prostaglandin synthesis, and
hypothermia; cause disseminated intravascular coagulation DIC leading to
thrombosis; inhibits inflammatory responses and kinin system; some patients
suffer from sepsis and lethal shock.
In general it is not good antigen and heat
stable.
Some effects of endotoxin are beneficial to the host. These include:
1. Mitogenic effects on B lymphocytes that increase resistance to viral and
bacterial infections
2. Induction of gamma interferon (IFN-γ) production by T-lymphocytes, which
may enhance the antiviral state, promotes rejection of tumor cells, and activates
macrophages and natural killer cells
3. Activation of the complement cascade with the formation of C3a and C5a
(anaphylotoxin)
4. Induction the production of interleukin-1 by macrophages and interleukin-2
and other mediators by T-lymphocytes.
B. Exotoxins
Exotoxins are bacterial metabolic products; unlike the lipopolysaccharide
endotoxin, the general properties are:
1. Proteins with toxic effects released from viable bacteria.
1. Immunogenic, they are protective antigen due to high molecular weight
and complex composition, induce specific antibodies (called antitoxins),
resulting in complete inhibition of the toxic activity (this immunological
Ag-Ab reaction is called neutralization).
2. Poisonous in low doses (very low concentrations per unit weigh).

7
3. Most of the higher molecular exotoxin proteins are heat labile; while, low
molecular exotoxins are heat-stable peptides.
4. They are produced by both Gram-positive and Gram-negative bacteria.
5. Chemical composition of exotoxins contains mainly two types of
polypeptides; Type A and Type B; type A polypeptides are responsible
for the toxic effect (toxogenic part of the toxin); while B polypeptides are
responsible for delivering the part A to the target cell or tissue. Part B do
not enter target cell. Toxins are different in their composition of both parts
types, some contain (A2B) meaning one Aand two polypeptides of B;
while (2A5B) meaning two A polypeptides and five B polypeptides.
Exotoxins can be grouped into several categories:
1. Neurotoxins like Botulin of Clostridium botulinum.
2. Cytotoxins, like diphtheria toxin of Corynebacterium diphtheriae.
3. Enterotoxins which are responsible of many types of watery diarrhea like
shigatoxin of Shigela sp.
4. Hemolysins, cause blood hemolysis like Streptolysin of Streptococcus
pyogens. Include three types α, β and γ.
5. Erythrogenic toxin which cause bleeding under skin, like Streptococcus
pyogens erythrogenic toxin.
6. Leucocidin cause WBCs lysis like leucocidin of Staphylococcus aureus.
8
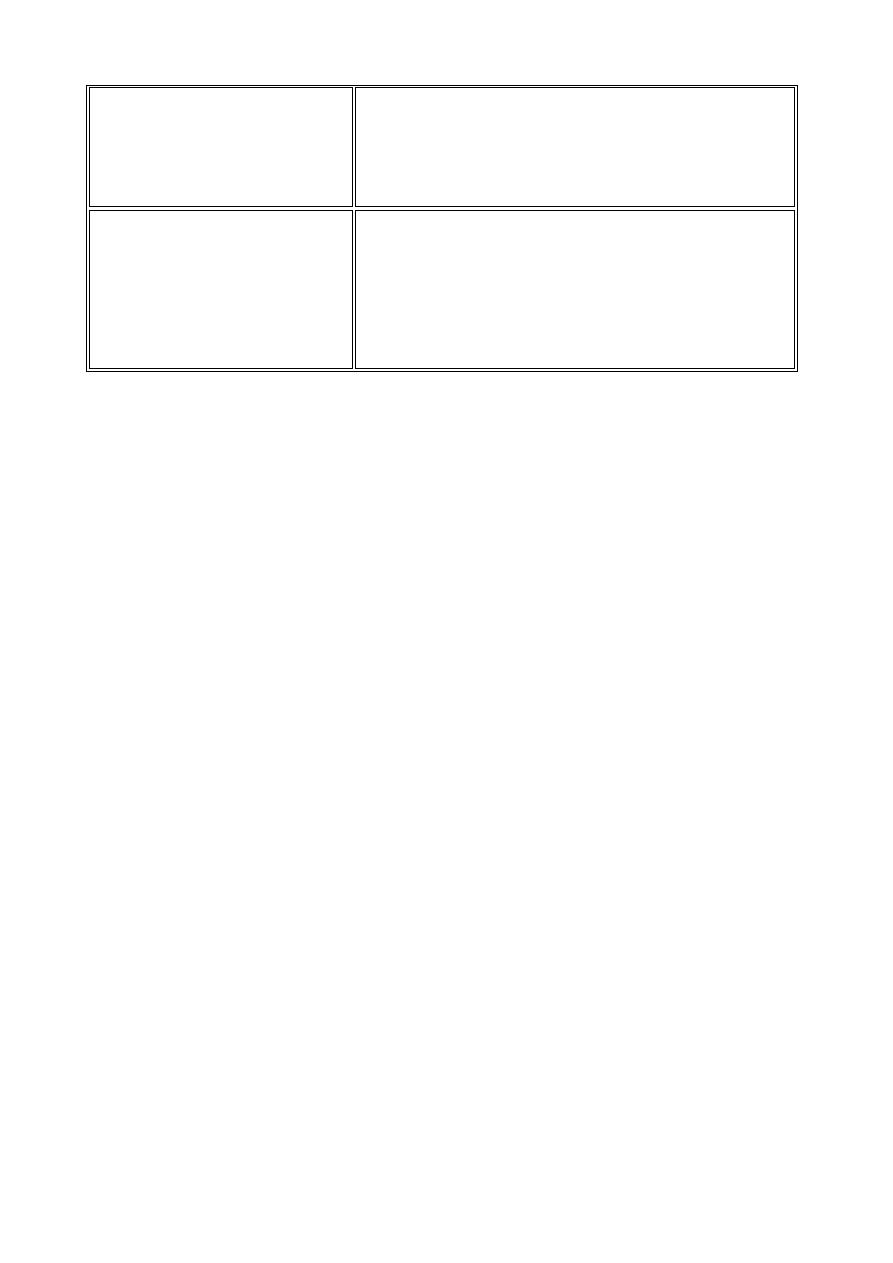
Bacteria Invasins
Invasin
Bacteria
Activity
Hyaluronidase
Streptococci,
staphylococci and
clostridia
Degrades hyaluronic of connective
tissue
Collagenase
Clostridium species
Dissolves collagen framework of
muscles
Neuraminidase
Vibrio cholera
and Shigella dysenteriae
Degrades neuraminic acid of intestinal
mucosa
Coagulase
Staphylococcus aureus
Converts fibrinogen to fibrin which
causes clotting
Kinases
Staphylococci and
Streptococci
Converts plasminogen to plasmin
which digests fibrin
Leukocidin
Staphylococcus aureus
Disrupts neutrophil membranes and
causes discharge of lysosomal granules
Streptolysin
Streptococcus pyogenes
Repels phagocytes and disrupts
phagocyte membrane and causes
discharge of lysosomal granules
Hemolysins
Streptococci,
staphylococci and
clostridia
Phospholipases or lecithinases that
destroy red blood cells (and other
cells) by lysis
Lecithinases
Clostridium perfringens
Destroy lecithin in cell membranes
Phospholipases Clostridium perfringens
Destroy phospholipids in cell
membrane
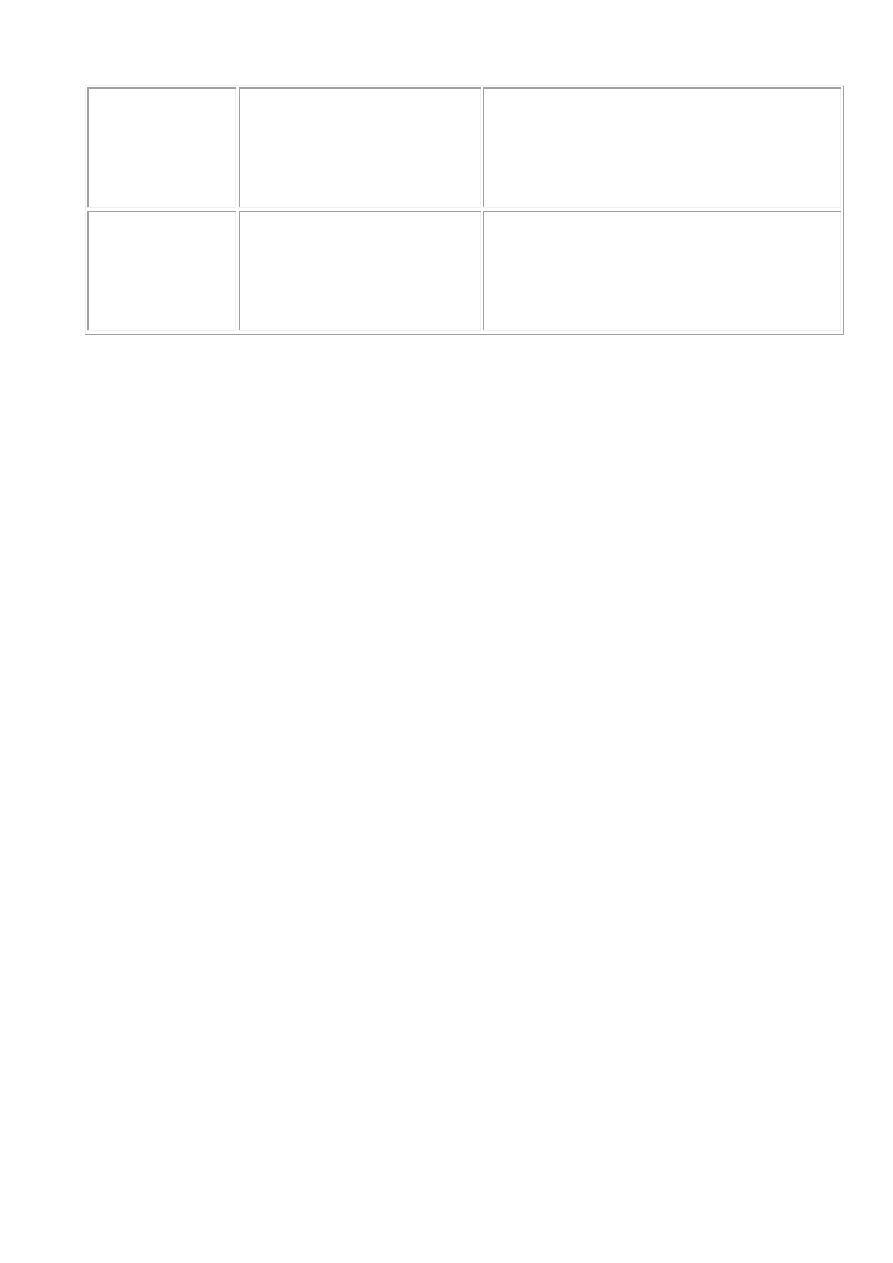
9
Anthrax toxin Bacillus anthracis
One component (EF) is an adenylate
cyclase which causes increased levels
of intracellular cyclic AMP
Pertussis toxin Bordetella pertussis
One toxin component is an adenylate
cyclase that acts locally producing an
increase in intracellular cyclic AMP
10
Pyrogenic Bacteria
These bacteria are pus forming bacteria, they include the following genera:
1. Staphylococci and Streptococci (Gram + cocci).
2. Neisseria (Gram - cocci).
3. Hemophilus (Gram - coccibacilli).
Staphylococci Genus
Staphylococci are Gram-positive spherical bacteria that found in clusters
like grapes. Although more than 20 species of Staphylococcus are described in
Bergey's Manual (2001), only Staphylococcus aureus and Staphylococcus
epidermidis are of medical importance to humans. S. aureus colonizes mainly
the nasal passages and S. epidermidis is normal flora of the skin.
Taxonomically,
the
genus Staphylococcus is
in
the
Bacterial
family Staphylococcaceae.
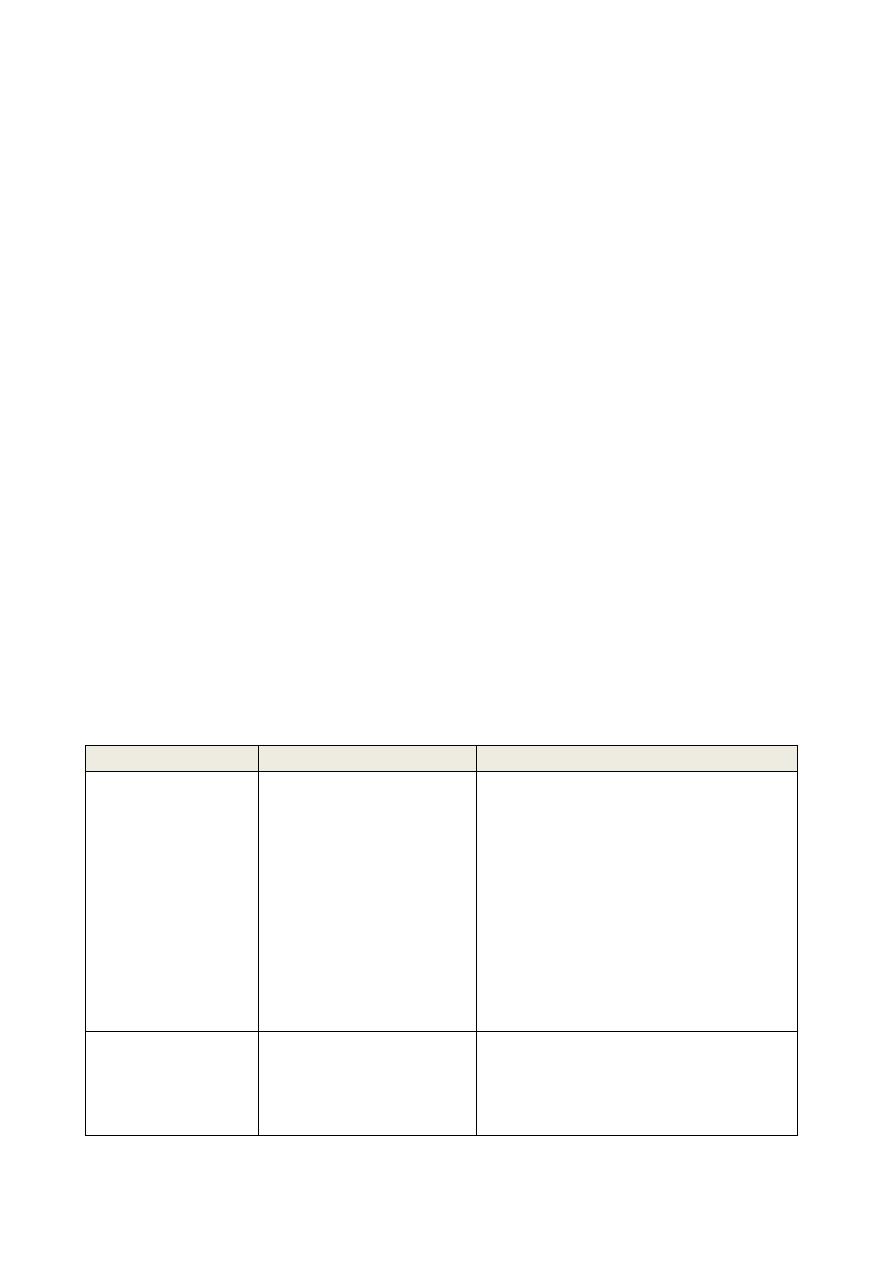
Staphylococcus Species That Affect Humans Most Frequently
Species Parameter
Species
Special Character
Infections
S. aureus
Coagulase-positive;
colonies golden
yellow. Can grow at
45 C ˚ and NaCl 15%
Local purulent
infections: furuncles, carbuncles,
bullous impetigo, wound
infections, sinusitis, otitis media,
mastitis puerperalis, ostitis,
postinfluenza pneumonia, sepsis.
Toxin-caused illnesses: food
poisoning, dermatitis exfoliativa,
toxic shock syndrome
S. epidermidis
Coagulase-negative;
sensitive to
novobiocin
most frequent coagulase negative
Staphylococci pathogen;
opportunist; infection requires
host predisposition;
11
foreign body infections with
discrete clinical symptoms
S. saprophyticus Coagulase-negative;
resistant to
novobiocin
Urinary tract
infections in young women (10–
20%); occasional nonspecific
urethritis in men
Staphylococcus aureus
Gram-positive, cluster-forming coccus
nonmotile, nonsporeforming facultative anaerobe
fermentation of glucose produces mainly lactic acid
ferments mannitol (distinguishes from S. epidermidis)
catalase positive
coagulase positive
golden yellow colony on agar
normal flora of humans found on nasal passages, skin and mucous
membranes
pathogen of humans, causes a wide range of suppurative infections, as
well as food poisoning and toxic shock syndrome
Pathogenesis of S. aureus infections
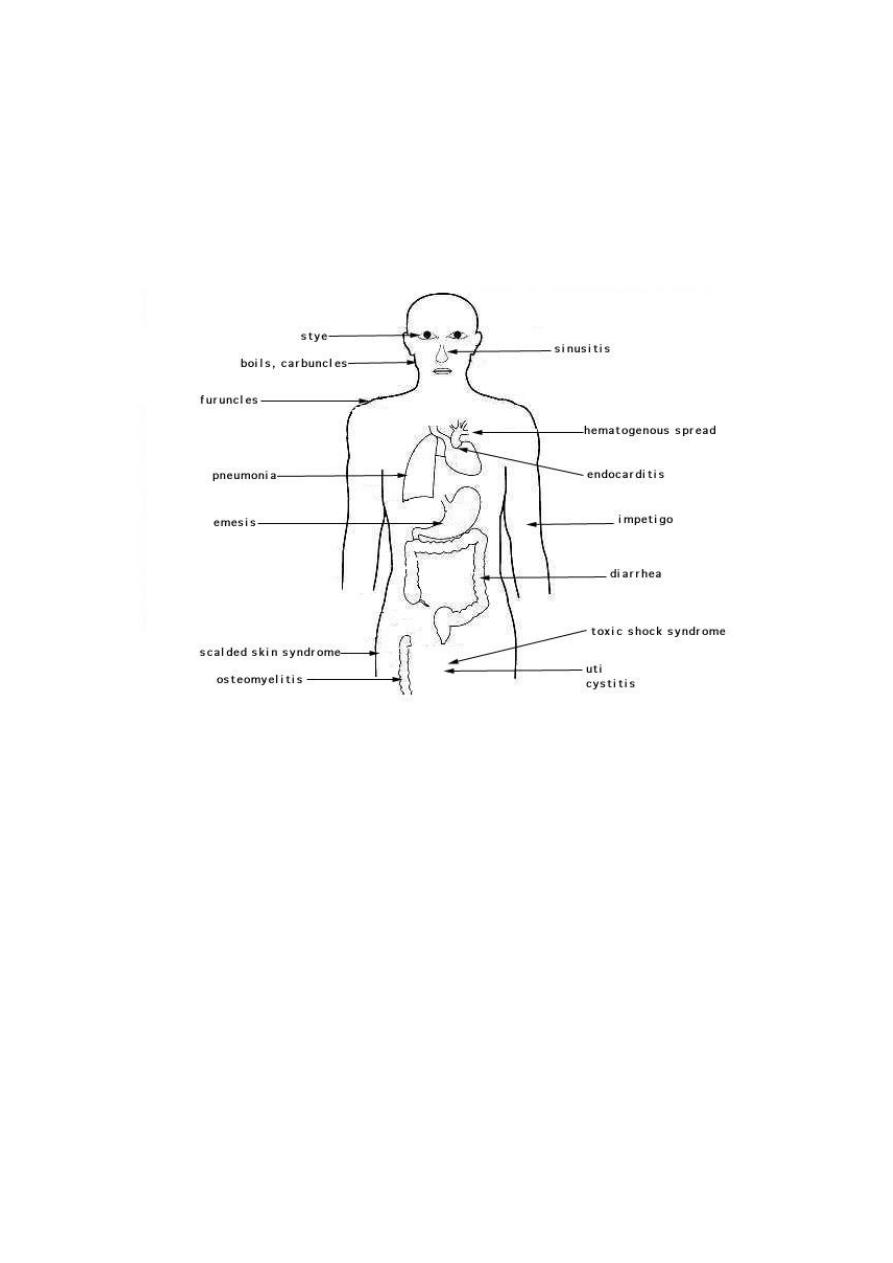
Staphylococcus aureus causes suppurative (pus-forming) infections and
toxinoses in humans. It causes superficial skin lesions such as boils; more
serious infections such as pneumonia, mastitis, meningitis, and urinary tract
infections UTI; and deep infections, such as osteomyelitis and endocarditis.
S. aureus is a major cause of hospital acquired (nosocomial)
infection of surgical wounds and infections associated with contaminated
medical devices. S. aureus causes food poisoning by releasing enterotoxins
into food, and toxic shock syndrome by release of superantigens into the blood
stream.
12
Portals for entry: Staphylococcus produce local infection as a start after
entry. The portal may be a hair follicle, but usually it is a break in the skin,
scratches, trauma or surgical wound. Another portal for entry is the respiratory
tract. Staphylococcal pneumonia is a common complication of influenza.
Sites of infection and diseases caused by Staphylococcus aureus
Adherence to Host Cell Proteins
S. aureus have surface proteins that promote attachment to host proteins
such as laminin and fibronectin that form the extracellular matrix of epithelial
and endothelial surfaces. In addition, most strains express a fibrin/fibrinogen
binding protein (clumping factor) which promotes attachment to blood clots and
traumatized tissue. Most strains of S. aureus express both fibronectin and
fibrinogen-binding proteins. In addition, an adhesin that promotes attachment to
collagen has been found in strains that cause osteomyelitis and septic arthritis.
Interaction with collagen may also be important in promoting bacterial
attachment to damaged tissue where the underlying layers have been exposed.

13
Invasion Factors
The invasion of host tissues by staphylococci involves the production of
a huge amount of invasion factors (extracellular proteins). These proteins are
described below with some possible explanations for their role in invasive
process.
1) Membrane-damaging toxins
1. α-toxin (α -hemolysin): The most effective membrane-damaging toxin
of S. aureus, mainly platelets and monocytes are sensitive to α -toxin.
Susceptible cells have a specific receptor for α -toxin which allows the
toxin to bind then form small pores and cause osmotic lysis.
2. ß-toxin: is a sphingomyelinase which damages membranes rich in this
lipid, usually lyse RBCs. A lysogenic bacteriophage is known to encode
the toxin. Found rare in human isolates.
3. γ-toxin is a very small peptide toxin produced by most strains of S.
aureus. It is also produced by S. epidermidis. The role of γ -toxin in
pathogenisity is unknown.
4. Leukocidin is a multicomponent protein toxin act together to damage
membranes, it is hemolytic, but less than alpha hemolysin. The strains
isolated from severe dermonecrotic lesions produce this toxin, it is an
important factor in necrotizing skin infections.
5. Coagulase and clumping factor: Coagulase is an extracellular protein
which binds to prothrombin in the host to form a complex called
staphylothrombin. It has protease activity and cause conversion of
fibrinogen to fibrin. Coagulase is a marker for identifying S. aureus in the
clinical microbiology laboratory. Helps the bacteria to protect themselves
from phagocytic and immune defenses by causing localized clotting.
6. Staphylokinase: it is a plasminogen activator, this factor lyses fibrin. The
genetic code found in the lysogenic bacteriophages. It causes dissolution
of fibrin clots, hence it is used in medicine to treat patients suffering from
coronary thrombosis. It is bacterial spreading factor.
7. Other extracellular enzymes: S. aureus can produce proteases, a lipase,
a deoxyribonuclease (DNase) and a fatty acid modifying enzyme
(FAME). The first three provide nutrients for the bacteria, and have a

14
minor role in pathogenesis. But, the FAME enzyme is important in
abscesses, where it could modify anti-bacterial lipids and help bacterial
survival.
2) Avoidance of Host Defenses
S. aureus expresses a number of factors that interfere with host defense
mechanisms. This includes both structural and soluble elements of the
bacterium.
1. Capsule
The majority of clinical isolates of S aureus express a surface polysaccharide
of either serotype 5 or 8. Usually called a microcapsule because it can be seen
only by electron microscopy unlike the true capsules of other bacteria. The
function of the capsule is to resist phagocytosis.
2. Protein A
Protein A is a surface protein of S. aureus which binds to IgG molecules by
their Fc region (in the wrong region), which disrupts opsonization and
phagocytosis.
3. Leukocidin
This toxin acts on polymorphonuclear leukocytes (PMNs).
4. Exotoxins
Include several toxic proteins which are responsible for symptoms during
infections:
Enterotoxins and toxic shock syndrome toxin
S. aureus secretes two types of toxin that are superantigens, enterotoxins
(have six types SE-A, B, C, D, E and G), and toxic shock syndrome
toxin (TSST-1). Enterotoxins cause diarrhea and vomiting when ingested and
are responsible for staphylococcal food poisoning and Toxic shock. TSST-1 is
expressed systemically and is the cause of toxic shock syndrome (TSS). When
produced systemically.
Superantigens mode of action is to stimulate T-cells non-specifically
without normal antigenic recognition, see figure below, up to one in five T-cells
will be activated, whereas only 1 in 10,000 are stimulated during the usual
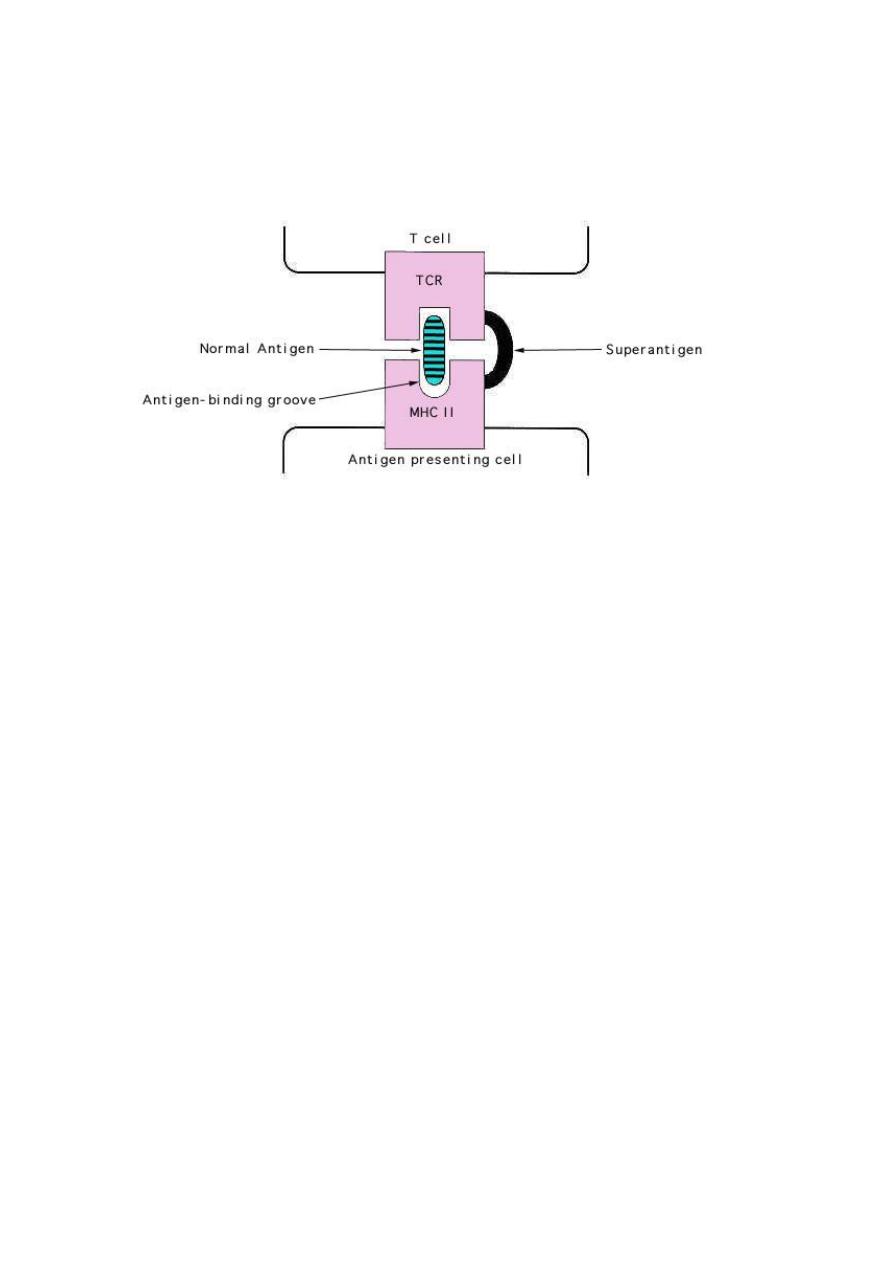
15
antigen presentation. Cytokines are released in large amounts, causing the
symptoms of TSS. Superantigens bind directly to class MHCII major
histocompatibility complexes of antigen-presenting cells.
Superantigens and the non-specific stimulation of T cells.
Exfoliatin toxin (ET)
The exfoliatin toxin, associated with scalded skin syndrome (SSS), causes
separation within the epidermis, between the living layers and the superficial
dead layers. The separation is through the stratum granulosum of the epidermis
leading to the risk of fluid loss and secondary infections.
5. Biofilm formation ability
Biofilm is the slim growing of Staphylococcus aureus as group of bacterial cells
forming layer upon layer of bacterial growth, during colonization process of
infection.
The biofilm matrix components, contain polysaccharides polymer,
protein (teichoic acid), and DNA, they play a major role in pathogenicity
because biofilm help to share nutrients, shield from immune system of hosts and
avoid antibiotics effect.

16
Pathogenic Staphylococcus epidermidis is able to show plastic interaction and
able to colonize catheters devices by forming of biofilm. This ability to form a
biofilm on the surface of a prosthetic device is a significant problem.
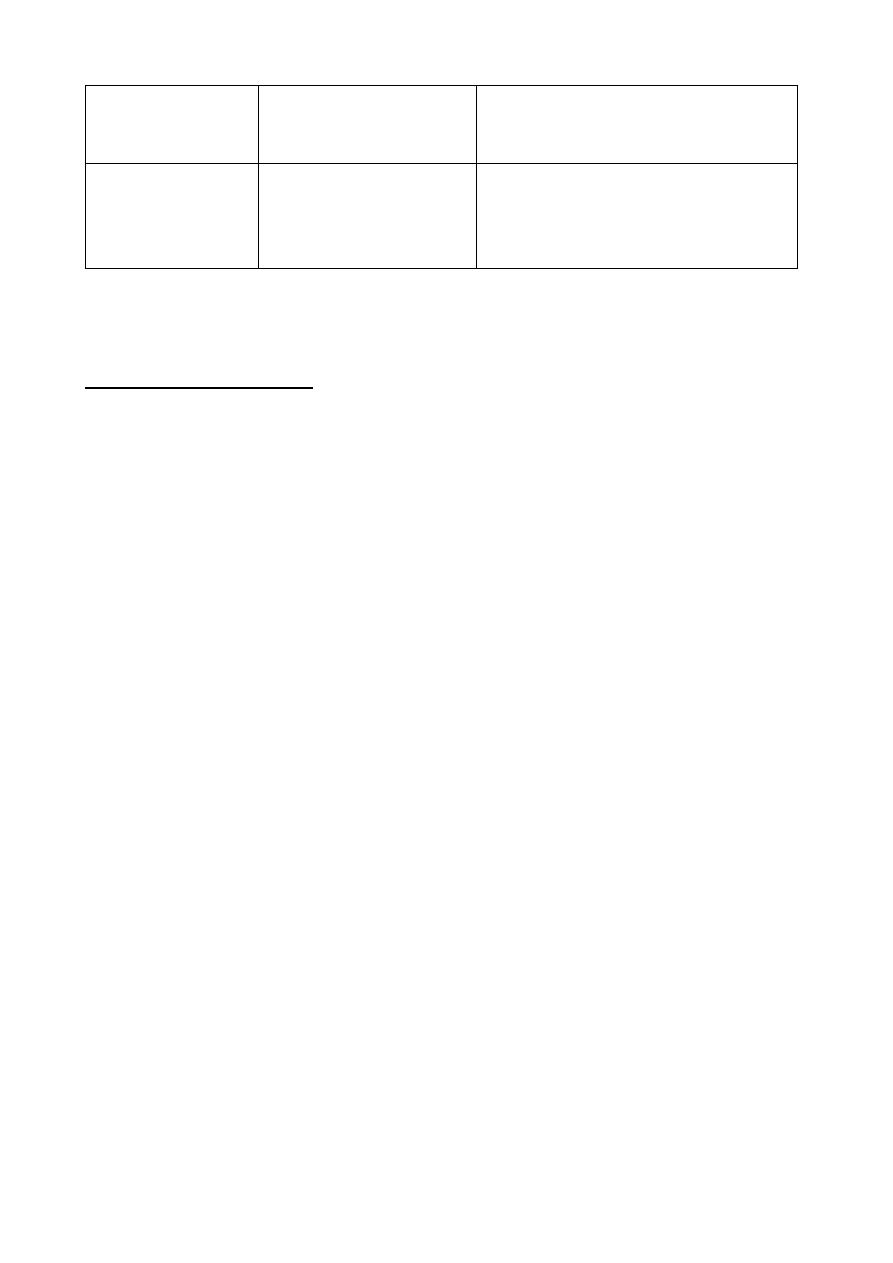
Virulence determinants of Staphylococcus aureus
Resistance of Staphylococci to Antimicrobial Drugs
Hospital strains of S. aureus are usually resistant to many antibiotics
except vancomycin, usually called as MRSA refers to Methicillin
resistant Staphylococcus aureus. Methicillin resistance is widespread and
most methicillin-resistant strains are also multi-antibiotics resistant. The
antibiotics resistance is due to the plasmids (extrachromosomal genes)
associated with resistance ability or by chromosomal mutation.
S. aureus shows resistance to antiseptics and disinfectants, such as
quaternary ammonium compounds, which may aid its survival in the hospital
environment hence these bacteria is a significant problem in the hospital
environment causing nosocomial infection especially in surgical wounds.

17
Host Defense against Staphylococcal Infections
Phagocytosis is the major mechanism against staphylococcal infection. But
they are difficult to be killed after phagocytic engulfment because they
produce catalase which neutralizes oxygen and superoxide and avoid killing
mechanisms inside the phagolysosome.
Specific Antibodies are produced which neutralize toxins and induce
opsonization.
The localized host response to staphylococcal infection is inflammation,
characterized by an elevated temperature at the site, swelling, the accumulation
of pus, and necrosis of tissue. Around the inflammation area, a fibrin clot help
to form pus-filled boil or abscess.
Epidemiology and Control
Staphylococci are widespread human parasites. The main sources of infection
are shedding human lesions, fomites contaminated from such lesions, and the
human respiratory tract and skin. Contact spread of occurs in hospitals, where
the staff and patients carry antibiotic-resistant staphylococci MRSA in their
nose or on the skin.
The areas at highest risk for severe staphylococcal infections in hospitals are
newborn nurseries, intensive care units, operating rooms, and cancer
chemotherapy wards.
Hygiene, and aseptic management of lesions can control the spread of
staphylococci from lesions, ultraviolet irradiation of air have little effect in
prevent staphylococci spreading from carriers.
Treatment
Hospital acquired infection is often caused by antibiotic resistant strains and can
only be treated with vancomycin or Rifampin coupled with a second oral
antistaphylococcal drug sometimes provides long-term suppression and
possibly cure of nasal carriage. Many of the community acquired
Staphylococcal infections are now methicillin resistant and only be treated with
combination therapy using sulfa drugs and minocycline or rifampin.
18
Vaccines
No vaccine is yet available that stimulates active immunity against
staphylococcal infections in humans.
Infections and involved Virulence factors in the pathogenesis
of Staphylococcus aureus
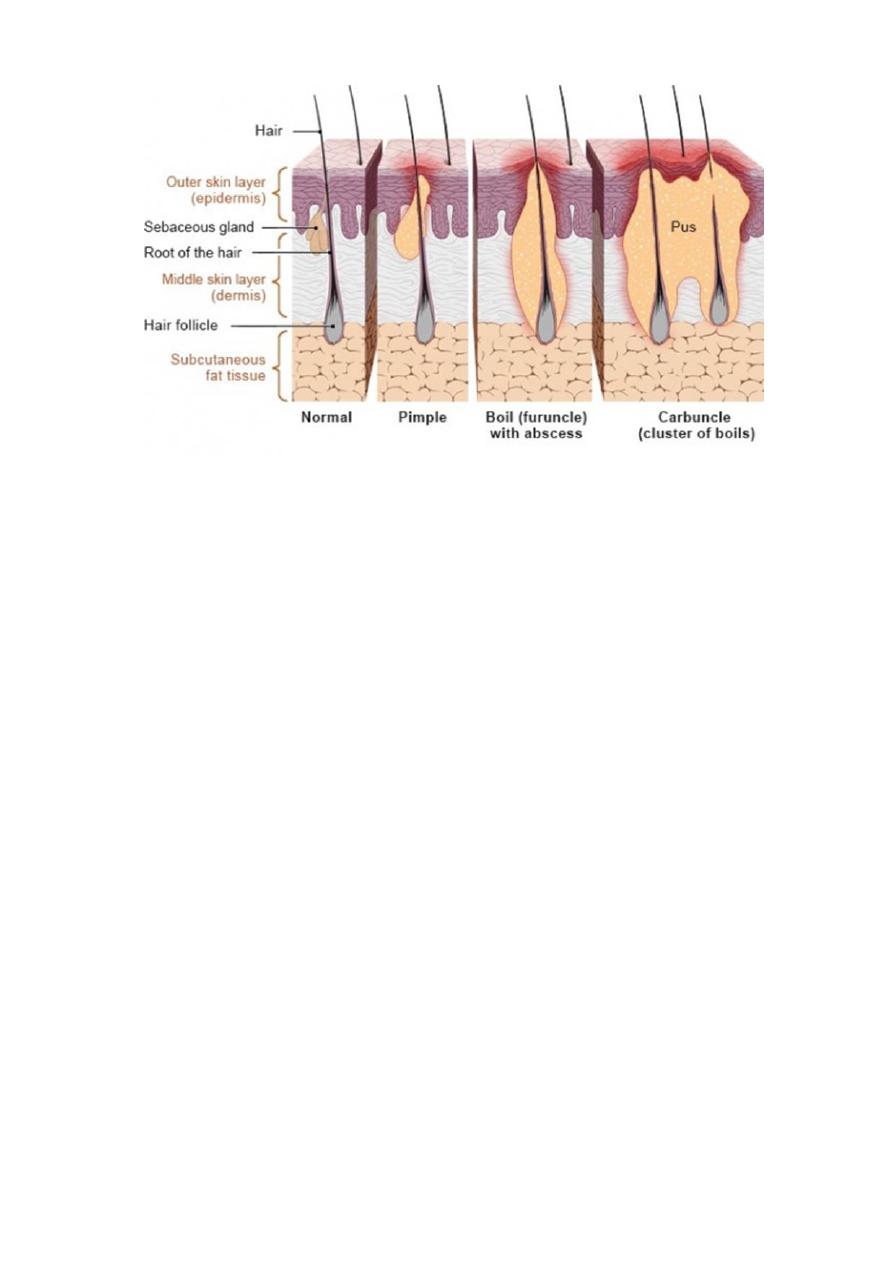
(1) Boils, pimples and carbuncle (folliculitis)
Colonization: cell-bound (protein) adhesins
Invasion: Invasins: staphylokinase
Other extracellular enzymes (proteases, lipases, nucleases, collagenase,
elastase. etc.)
Resistance to phagocytosis: coagulase, leukocidin
Resistance to immune responses: coagulase
Toxigenesis: cytotoxic toxins (hemolysins and leukocidin)
Pathogenesis:
It is a pus-filled bump in the skin that is caused by the bacterial infection. It’s
a bit like a very big yellow pimple, but it’s deeper in the skin and hurts a lot
more.
Boils develop when a hair follicle and the surrounding tissue become infected.
Hair follicles consist of one hair, the root of the hair, a sebaceous gland and a
small muscle that can pull the hair up, making it stand on end. Hair follicle
inflammations are sometimes also referred to as “deep folliculitis” or
“perifolliculitis.”
The infection cause the death of skin tissue inside the boil, creating a pus-filled
space (an abscess). Skin abscesses can develop from boils, but also from other
things like infected insect bites or injections with dirty needles. If several
boils merge into a larger bump, it’s called a carbuncle (a cluster of boils)..
Sometimes boils heal without causing any problems, but it is better to get
medical treatment for quick cure, relieve the pain and prevent complications.
Because sometimes boils develop into carbuncle.
19
(2)
Pneumonia
Colonization: cell-bound (protein) adhesins
Invasins: staphylokinase, hyaluronidase
Other extracellular enzymes (proteases, lipases, nucleases, collagenase,
elastase. etc.)
Resistance to phagocytosis: coagulase, leukocidin, hemolysins,
carotenoids, superoxide dismutase, catalase, growth at low pH
Resistance to immune responses: coagulase, antigenic variation
Toxigenesis: Cytotoxic toxins (hemolysins and leukocidin)
(3)
Food poisoning (emesis or vomiting)
Toxigenesis: Enterotoxins A-G (superantigens).
Pathogenesis:
Staph food poisoning is characterized by a sudden start of nausea, vomiting, and
stomach cramps. Most people also have diarrhea. Symptoms usually develop
within 30 minutes to 8 hours after eating or drinking an item containing Staph
toxin, and last no longer than 1 day. Severe illness is rare. The illness cannot be
passed from one person to another with Fast cure. The enterotoxins are heat
stable and resistant to the action of gut enzymes. Important cause of food
poisoning, enterotoxins are produced when S. aureus grows in carbohydrate and
protein foods. Ingestion of 25 μg of enterotoxin B results in vomiting and

20
diarrhea. The emetic effect of enterotoxin is the result of central nervous system
stimulation (vomiting center) after the toxin acts on neural receptors in the gut.
(4)
Septicemia (invasion of the bloodstream):
Invasins: staphylokinase, hyaluronidase
Other extracellular enzymes (proteases, lipases, nucleases, collagenase,
elastase. etc.)
Resistance to phagocytosis: coagulase, protein A, leukocidin, hemolysins,
carotenoids, superoxide dismutase, catalase, growth at low pH
Resistance to immune responses: coagulase, protein A, antigenic variation
Toxigenesis: cytotoxic toxins (hemolysins and leukocidin)
(5)
Osteomyelitis (invasion of bone)
Colonization: cell-bound (protein) adhesins
Invasins: staphylokinase, hyaluronidase
Other extracellular enzymes (proteases, lipases, nucleases, collagenase,
elastase. etc.)
Resistance to phagocytosis: coagulase, protein A, leukocidin, hemolysins,
carotenoids, superoxide dismutase, catalase, growth at low pH
Resistance to immune responses: coagulase, protein A, antigenic variation
Toxigenesis: cytotoxic toxins (hemolysins and leukocidin)
(6) Toxic shock syndrome
Colonization: cell-bound (protein) adhesins
Resistance to immune responses: coagulase, antigenic variation
Toxigenesis: TSST-1 toxin, Enterotoxins A-G
Pathogenesis:
Staphylococcal toxic shock syndrome (TSS) is a life-threatening illness
characterized by fever, rash (similar to sunburns), hypotension, multi-organ
failure or dysfunction (involving at least 3 or more vital organs), and shock.
Typically syndrome starts with the infection of the palms and soles and
develops after 1-2 weeks from the onset of acute illness. The clinical
syndrome can also include severe myalgia, vomiting, diarrhea, headache, and
neurologic abnormalities. The gene encoding for this toxin found in 20% of
S. aureus isolates including MRSA.
21
(7)
Surgical wound infections
Colonization: cell-bound (protein) adhesins
Invasins: staphylokinase, hyaluronidase
Other extracellular enzymes (proteases, lipases, nucleases, collagenase,
elastase. etc.)
Resistance to phagocytosis: coagulase, protein A, leukocidin, hemolysins,
carotenoids, superoxide dismutase, catalase, growth at low pH
Resistance to immune responses: coagulase, protein A, antigenic variation
Toxigenesis: cytotoxic toxins (hemolysins and leukocidin)
(8)
Scalded skin syndrome (analogous to scarlet fever) (Called SSS)
Colonization: cell-bound (protein) adhesins
Invasins: staphylokinase, hyaluronidase
Other extracellular enzymes (proteases, lipases, nucleases, collagenase,
elastase. etc.)
Resistance to phagocytosis: coagulase, leukocidin, hemolysins
Resistance to immune responses: coagulase, antigenic variation
Toxigenesis: Exfoliative toxins A and B (superantigens)
Pathogenesis:
Exfoliative toxins of S. aureus are two types of proteins of the same molecular
weight and have epidermolytic activity. Exfoliative toxin A is encoded by gene
in a bacteriophage and is heat stable (resists boiling for 20 minutes). Exfoliative
toxin B is carried by plasmid and heat labile. These epidermolytic toxins act by
dissolving the mucopolysaccharide matrix of the epidermis.
Syndrome occurs commonly in newborns typically following an erythematous
cellulitis. Severity of staphylococcal scalded skin syndrome varies from a few
blisters localized to the site of infection to a severe exfoliation affecting almost
the entire body.
Pathogenesis of these toxins by breaking down the desmosomes of epidermal
layer due to protease effect of the exotoxins lead to the separation of the
superficial layer of the epidermis due to cleave desmoglein (which normally
22
holds the granulosum and spinosum layers together), like in the case of the
autoimmune skin disease pemphigus vulgaris.
Diagnostic Laboratory tests:
1) Specimens:
Surface swab for pus or aspirates from abscess, blood, tracheal aspirate or
spinal fluid, are used for culture depending on infection location.
2) Smear:
Staphylococci appear Gram + cocci in clusters in gram stained smears of pus
or sputum; it is not possible to distinguish between S. aureus and S.
eipermidis in smear only.
3) Culture:
On blood agar give typical colonies, on mannitol salt agar only
Staphylococcus aureus are able to ferment mannitol and it is used as
differential media during diagnosis.
4) Catalase Test
5) Coagulase Test
6) Antibiotic sensitivity test (susceptibility testing).
7) Serologic and typing test.
